ABSTRACT
Objective:
The aim of this study was to assess the impact of turmeric cream on the healing of Caesarean wound.
Methods:
This study was done as a randomized double blind trial in three groups of women who had a Caesarean operation. The redness, oedema, ecchymosis, drainage, approximation (REEDA) scale was used to evaluate the wound healing process. The χ2, analysis of variance (ANOVA) and Tukey tests were used for statistical analysis.
Results:
Seven days after the surgery, the averages of REEDA score in the intervention, placebo and control groups were respectively, 0.46, 0.88 and 1.17 (p < 0.001), while on day 14, it was 0.03, 0.22 and 0.36 (p < 0.001), showing a significant statistical difference. Similarly, there was a difference between the intervention and placebo groups in the amount of oedema on the 7th and 14th days after the surgery (respectively, p = 0.066 and p < 0.001). The observed difference between the intervention and control groups in the amount of oedema was statistically significant on the 7 th and 14 th days after the surgery (p < 0.001).
Conclusion:
Turmeric was effective in faster healing of wounds of Caesarean operation. The use of turmeric is suggested to reduce the complications of the wounds from Caesarean section.
Keywords: Caesarean delivery, turmeric, wound healing
RESUMEN
Objetivo:
El objetivo de este estudio fue examinar el impacto de la crema de cúrcuma en la cura de las heridas de cesárea.
Métodos:
Este estudio se realizó como un ensayo doble ciego aleatorio en tres grupos de mujeres que tuvieron operación cesárea. La escala de enrojecimiento, edema, equimosis, drenaje, escala de aproximación (REEDA, siglas en inglés) se utilizó para evaluar el proceso de cicatrización. Para el análisis estadístico se utilizaron la prueba χ 2, el análisis de varianza (ANOVA), y el test de Tukey.
Resultados:
Siete días después de la cirugía, los promedios de puntuación de REEDA en los grupos de intervención, control y placebo fueron 0.46, 0.88 y 1.17 (p < 0.001), respectivamente, mientras que en el día 14, fueron 0.03, 0.22, y 0.36 (p < 0.001), mostrando una diferencia estadística significativa. Asimismo, hubo una diferencia entre los grupos de intervención y placebo en la cantidad de edema en los días 7 y 14 después de la cirugía (p = 0.066 y p < 0.001, respectivamente). La diferencia observada entre el grupo de intervención y control en la cantidad de edema fue estadísticamente significativa en los días 7 y 14 días después de la cirugía (p < 0.001).
Conclusión:
La cúrcuma fue efectiva en la curación más rápida de las heridas de la operación cesárea. Se sugiere el uso de la cúrcuma para reducir las complicaciones de las heridas de la cesárea.
INTRODUCTION
The prevalence of Caesarean section (C-section) has increased in most countries (1–4). It is reported that the prevalence of C-section was 33% in Iran in 1998 (5), 66.5% in Tehran in 2009, 45.6% in Tabriz in 2004 and 66.4% in Shiraz from 2005 to 2006 (6–8). However, the standard level of Caesarean is 15 per cent according to the World Health Organization (4).
The most prevalent complication after C-section is delay or failure of surgical wound healing. Not only does it cause pain, discomfort, increase in the length and cost of hospitalization, it also postpones the emotional relationship between mother and the newborn, causing anxiety in the mother (9, 10). Furthermore, the commonest cause of morbidity after C-section is wound infection (11–12) and its prevalence has been reported to be about 6% in various studies, resulting in interventions such as drainage, debridement and restoration of the wound (7). Sometimes it leads to inguinal hernia (13).
There is no accurate statistical information about the rate of the complications of Caesarean wounds in Iran; however, in some studies, it has been reported that the rate of Caesarean wound infection is about five per cent and the rate of wound disruption about seven per cent (14).
To reduce the Caesarean wound complications and accelerate the wound healing, several suggestions have been presented, including causing the least trauma to tissue, meeting the sterility standards, skin preparation before surgery, using appropriate surgical techniques (14), using prophylactic antibiotic, the observance of hygiene at wound site, and use of analgesics (5). However, these types of treatments are associated with a high rate of recurrence and sometimes they are painful (14).
Researchers have suggested various topical creams such as fusidic acid (15), honey (16, 17), Hypericum perforatum (18), lavender (19) and turmeric for Caesarean wound healing. Turmeric has been one of the oldest medicinal plants used as an anti-inflammatory drug in traditional medicine (20). Turmeric is a herbaceous, perennial plant of the ginger family with curcumin as the effective material of its rhizome (21). Curcumin has numerous properties such as being anti-inflammatory (20–22), antibacterial (23, 24) and antiviral (25) as well as acting as a wound healer (26–29). Curcumin reduces inflammation in damaged tissues by decreasing the activity of enzymes such as cyclooxygenase, lipoxygenase and nitric acid synthase, and inhibiting the production of tumour necrosis factor-alpha (TNF-α) and interleukin (IL)- 1, 2, 6, 8, 12 (30).
Golmakani et al (20) conducted a study in Hazrat Zainab Hospital, Mashhad, to investigate the effect of turmeric cream on episiotomy wound healing in primigravida women. The women were assigned to two groups, namely, intervention group (using turmeric cream) and placebo group. The results indicated that topical application of turmeric cream was effective in episiotomy wound healing (20). In another study conducted by Kundu et al (31), the effect of turmeric poultice was compared with the effect of honey on wound healing. It was concluded that both turmeric rhizome poultice and honey had the same effect on wound healing and both intervention groups (turmeric and honey) had higher rates of tension power and wound shrinkage than the control group, with p < 0.01 (31).
Due to the importance of reducing the complications of Caesarean wound and faster recovery of mothers for taking better care of themselves and the baby, this study was conducted with the aim of investigating the effect of turmeric cream on Caesarean section wound healing.
SUBJECTS AND METHODS
This research is a double blind randomized controlled clinical trial that was conducted on 181 pregnant women referred to Imam Ali Hospital of Amol for a C-section. Based on the pilot study and the sample size formula for comparison of averages, with 95% confidence and 80% power test, the sample size for each group was considered 50 people. Eligible participants were selected by purposeful sampling and were then randomly allocated into one of three groups as the intervention, placebo or control. After the C-section, the advisor gave the coded cream packages to the researchers to apply them (the researchers were blind until the data analysis).
Inclusion and exclusion criteria
Criteria for entering the study included: giving consent to participate in the study, educational level higher than fifth grade of elementary school, gestational age from 37 to 42 full weeks based on the first day of the last period cycle, or sonography. The exclusion criteria were: smoking or drug abuse, known history of confounding diseases of wound healing such as chronic systemic or immune system diseases, consuming medications effective on wound healing such as glucocorticoids, anticoagulants, immunosuppressives, chemotherapy, and obstetric complications such as pre-eclampsia, excessive bleeding and chorioamnionitis, and surgery time of more than 60 minutes for a C-section.
Extraction protocol
A pharmacist prepared the cream. First, using 90% ethanol solution, the essence of chopped turmeric was extracted by a percolation method. Materials were separately prepared in the oil phase and aqueous phase. In the oil phase, stearic acid, cetyl alcohol, triethanolamine were mixed together, and in the aqueous phase, materials such as sodium hydroxide, glycerol, distilled water, methyl paraben and propyl were mixed and turmeric extract was added to them. Both the oil phase and the aqueous phase were heated at 70 °C. When both phases came to this temperature, the aqueous phase was slowly added to the oil phase and was constantly stirred to form a cream. The placebo was prepared using a mixture of Vaseline and a few drops of concentrated hydro-alcoholic extract of turmeric rhizome, in the form of sterile ointment. Then it was packed in sealed tubes with a shape and colour similar to the drug package. A sample of the final product was given to the lab and was cultured to exclude contamination. It was then used in the study.
Data were gathered through a unit selection form (inclusion and exclusion criteria), a form containing demographic information, as well as information about the current pregnancy, the after-surgery information form, the daily drug intake form, and health advice and nutritional tips form. The redness, oedema, ecchymosis, drainage, approximation (REEDA) scale was used for the follow-up of the Caesarean wound condition. In this scale, a score between 0 and 3 is given to the wound based on the redness, oedema, bruising, wound secretion and the interstice between the two edges of the wound. The total point was then calculated. The lower the score, the better the wound condition.
Data gathering scale
The REEDA scale is a valid instrument used to assess wound healing that has been confirmed by Davidson (32). Researcher's performance in completing the REEDA scale was approved by a gynaecologist and the reliability of the questionnaire was determined to be r = 0.9. After surgery and full recovery, the mother was met and an encoded ointment packet was given to her in the intervention and placebo groups. Then the mothers were given full instructions on how to use it. They were instructed to wash their hands and clean the wound location the day after the surgery, and rub some gel on the suture area so that it covers the location, and leave it uncovered for 15 minutes. This had to be continued twice a day (12 ± 2 hours) up to 14 days. They were also asked to fill in the checklist related to the instructions. All of the above were examined in the control group but nothing was used on the incision location.
The condition of the wound healing was assessed based on the REEDA scale by one of the co-researchers on the first, seventh and fourteenth days after a C-section. At the time of the assessment, the mother was in the supine position. Nutrition is one of the effective factors in recovery and wound scar. Although it is not possible to accurately control it, in a follow-up period, the number of meals containing milk and dairy, meat, fruits and vegetables was relatively controlled. It should be mentioned that all the participants received the normal medications such as analgesic and antibiotic after C-section.
A gynaecologist with 25 years of experience performed all the surgeries on the participants. The average length of the Caesarean wound was less than 10 cm in all patients. All received injectable antibiotic as prophylaxis (2g cephazoline) and 25 mg of intramuscular pethidine for pain relief after the surgery.
After data collection, coding was done and data were analysed using SPSS software, version 16. For data analysis, descriptive analysis, analysis of variance (ANOVA), χ2 and Tukey were used with the p-value ≤ 0.05.
RESULTS
Initially, 181 people entered the study; however, according to the exclusion criteria, several of them were excluded and at the end, 55 mothers were allocated to the intervention group, 54 to the placebo group and 53 patients to the control group. There was no significant difference between the three groups in terms of demographic features such as age, educational level, employment, husband's occupation and educational level, adequacy of income, residency, regular exercise and pregnancy characteristics such as prenatal care [p > 0.05] (Table 1).
Table 1. Demographic and obstetric characteristics of study group.
| Variable | Drug group n (%) |
Placebo group n (%) |
Control group n (%) |
Test Chi-squared |
|---|---|---|---|---|
| Mother's educational level | ||||
| Primary school | 5 (8.2) | 4 (6.5) | 3 (5.4) | |
| Junior high school | 29 (47.5) | 25 (40.3) | 25 (44.6) | p = 0.96 |
| High school | 21 (34.4) | 26 (41.9) | 23 (41.1) | |
| University graduate | 6 (9.8) | 7 (11.3) | 5 (8.9) | |
| Total | 61 (100) | 62 (100) | 56 (100) | |
| Father's educational level | ||||
| Primary school | 8 (13.1) | 2 (3.2) | 9 (15.5) | p = 0.16 |
| Junior high school | 21 (31.4) | 31 (50) | 19 (32.8) | |
| High school | 24 (39.2) | 18 (29) | 20 (34.5) | |
| University graduate | 8 (13.1) | 11 (17.7) | 10 (17.2) | |
| Total | 61 (100) | 62 (100) | 58 (100) | |
| Mother's occupational status | ||||
| Housewife | 52 (85.2) | 57 (91.9) | 49 (86) | p = 0.46 |
| Employee | 9 (14.8) | 5 (8.1) | 8 (14) | |
| Total | 57 (100) | 62 (100) | 61 (100) | |
| Father's occupational status | ||||
| Self-employed | 10 (16.4) | 9 (14.5) | 11 (19.6) | p = 0.9 |
| Employed | 20 (32.8) | 23 (37.1) | 21 (37.5) | |
| Occasional worker | 31 (50.8) | 30 (48.4) | 24 (42.9) | |
| Total | 61 (100) | 62 (100) | 56 (100) | |
| Family income | ||||
| Below poverty line | 16 (26.2) | 16 (25.8) | 12 (20.7) | p = 0.73 |
| Above poverty line | 45 (73.8) | 46 (74.2) | 46 (79.3) | |
| Total | 61 (100) | 62 (100) | 58 (100) | |
| Area of residence | ||||
| City | 36 (59) | 34 (54) | 28 (57.1) | p = 0.89 |
| Village | 25 (41) | 28 (45.2) | 21 (42.9) | |
| Total | 62 (100) | 62 (100) | 49 (100) | |
| Exercise | ||||
| Yes | 17 (28.3) | 14 (22.6) | 12 (20.7) | p = 0.59 |
| No | 43 (71.7) | 48 (77.4) | 46 (79.3) | |
| Total | 60 (100) | 62 (100) | 58 (100) | |
| Mean ± SD | Mean ± SD | Mean ± SD | ANOVA | |
| Age (year) | 25.95 ± 4.9 | 26.54 ± 6.30 | 26.87 ± 5.96 | p = 0.23 |
| Number of pregnancies | 1.62 ± 0.7 | 1.51 ± 0.65 | 1.85 ± 0.79 | p = 0.33 |
| Number of prenatal care visits | 8.93 ± 1.93 | 8.90 ± 1.45 | 9.3 ± 1.65 | p = 0.23 |
Among the participants, 34.2% underwent C-section due to an emergency condition, while 63.8% had elective C-section. In 75% of cases, plastic sutures and in 25%, intermittent sutures were used. There was no significant difference between the groups in the use of antibiotics, that is, 85% of them were regularly taking them. Ninety per cent stated that they washed their hands and dried the wound location before using the gel. Ninety-two per cent claimed that they consumed milk, meat, fruits, vegetables and whole grains every day. Most of the women who participated in the study (82.5%) had begun their normal activity 10 days after the surgery. Therefore, there was no significant difference between the three groups in term of the factors affecting wound healing.
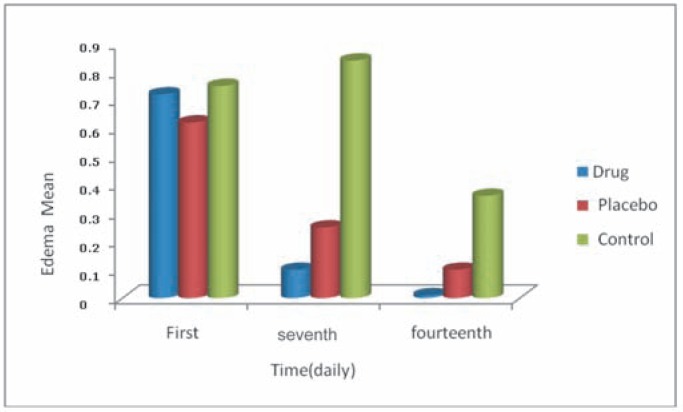
A Tukey test was employed to find the differences between the groups with regard to wound oedema. Findings of the study indicated that wound oedema score in the intervention and placebo groups on the 7th and 14th day after C-section was statistically different (p = 0.066, p < 0.001). A similar result was found between the intervention and control groups (p < 0.001) [Fig. 1]. But in terms of the other REEDA criteria, namely, redness, bruising, wound exudation and interstice, no significant differences were found among groups on the 7th and 14th days after C-section. However, the average scores of redness and exudation in the intervention group were less than those of the other two groups. There was no discharge in any members of the intervention group on the 14th day.
Fig. 1. Average oedema in the three groups: drug (intervention), control and placebo on the first, seventh and fourteenth days after Caesarean section.
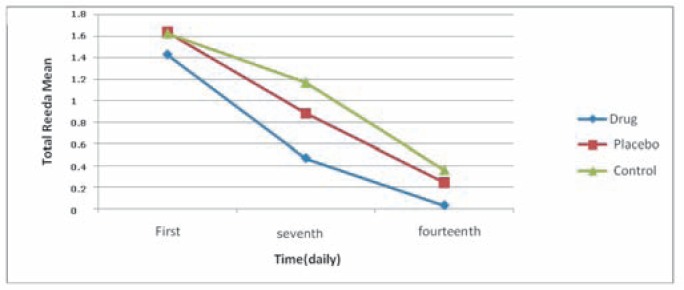
Comparison of the total scores of the five variables of the REEDA scale showed that the REEDA score in the group receiving the drug was different from the score of the placebo group (p = 0.049) and the score of the control group (p = 0.07), and the difference was statistically significant. But there was not a significant difference between the placebo group and the control group. Furthermore, the results showed that the total REEDA score among the three groups was statistically significant on the fourteenth day after C-section. Thus, statistical difference was significant between the intervention and placebo groups (p = 0.027) as well as the intervention and control groups (p = 0.003). However, there was no significant difference between the placebo group and the control group (Tukey test for comparison between two groups) . The use of ANOVA test for comparing the three groups together in terms of total REEDA score showed the statistical differences was significant on the 7th and 14th days [p < 0.001] (Table 2, Fig. 2).
Table 2. Total REEDA scores in the study groups on the first, seventh and fourteenth days.
| Tumeric group (M ± SD) |
Placebo group (M ± SD) |
Control group (M ± SD) |
p-value | |
|---|---|---|---|---|
|
First day Total REEDA |
1.43 ±0.69 | 1.64 ±1 | 1.63 ±0.5 | NS |
|
7th day Total REEDA |
0.47. ±0.57 | 0.88 ±1 | 1.17±1.14 | p = 0.001 |
|
14th day Total REEDA |
0.03 ±0.18 | 0.24 ±0.58 | 0.36 ±0.48 | p = 0.001 |
REEDA – redness, oedema, ecchymosis, drainage, approximation; M ± SD – mean ± standard deviation; NS – non-significant
Fig. 2. Total REEDA (redness, oedema, ecchymosis, drainage, approximation) mean score among the three groups on the first, seventh and fourteenth days.
DISCUSSION
The results of this study showed that turmeric extract was effective in the wound healing process after C-section and reduced oedema, wound inflammation and wound healing time. Evaluation of the criteria of the REEDA tool on the scar location of the C-section showed that the score for wound oedema in the intervention group was significantly less than the wound oedema score of the placebo group on the 7th day after surgery (p = 0.066). Significant differences were observed between the intervention and placebo groups. Moreover, the difference between the intervention group and the control group was statistically significant on the 7th and 14th days. Similarly, in a study conducted by Golmakani et al, it was found that there was a significant difference between the intervention and placebo groups on the 7th and 14th days after the C-section (20). The results of the study also showed there was no exudation from the wound of the participants in any of the groups on the 14th day after the Caesarean section.
Kundu et al (31), in a study conducted on animals, observed on the 14th day after the injury that the surface of the wound in the intervention group (using turmeric on the wound) was pink, wet and without exudates and the surface was not covered with floccule, but the control group had moist exudative wound and the surface was covered with dense floccule. Microscopy of the wound sample revealed that the mean score of vessel formation – epithelialization and the formation of collagen, elastin and reticulum – in the control group was less than the intervention group on the 14th day (31).
Research has shown that within two days after C-section, 20 mediators were identified including IL- 12, 10, 6, 4, 2, 1, TNF-α and prostaglandin E2 from the wound exudate that can be effective in inflammation and wound pain (33). Turmeric inhibits the activity of cyclooxygenase 2 (Cox2), lipoxygenase, and the inducible nitric oxide synthase (iNOS) enzyme. It also reduces the production of IL- 12, 10, 6, 4, 2, 1, TNF-α and the inflammatory cytokines (34, 35). It has been reported that the anti-inflammatory effects of oral administration of turmeric is similar to the effect of hydrocortisone in the short term (6).
According to the study results, the total score of the REEDA scale of the intervention group was significantly lower when compared with the total scores of the placebo and control groups (Tukey test for comparison between two groups). This finding was consistent with the result of Golmakani et al (20). Also, in their study, Ungphaiboon et al showed that the use of turmeric soap solution in patients with AIDS ulcers increased the wound healing process (25). In contrast, López-Jornet et al conducted a study to investigate the effect of turmeric cream on wound healing caused by laser (carbon dioxide) in an animal model. In terms of wound recovery, the intervention group had a significant favourable difference with the two other groups on the 7th day, but on the 14th day, there were no statistically significant differences between the groups (24). This result is not consistent with the present study.
The curcumin in turmeric has anti-inflammatory (20– 22), antibacterial (23, 24) and antiviral (25) properties and is effective in wound healing (26–28). Transforming growth factor beta-1 (TGFβ) increases the rate of appearance of fibronectin and collagen, leading to an increase in the rate of the formation of granulation tissue. The curcumin in alcoholic extract of turmeric regulates TGFβ and nitric oxide level in damaged tissue and also leads to better regulation of the formation of granulation tissue and better guidance of growth factors in the wound (29).
Comparison of wound healing scores in this study indicates that the speed of wound healing with the drug in the first seven days was twice more than the placebo group and thrice more than the control group. In other words, the rate of wound healing in the group using turmeric ointment is more than the two other groups. This finding is consistent with the study of Sidhu et al (26). In their study on an animal model, they showed that wounds treated with curcumin healed faster than the wounds from animals that were not treated with curcumin. Jagetia et al and Kundu et al also found similar results (23, 31).
Treatment with curcumin reduces the duration of wound healing, improves collagen replacement, and increases vascular density and fibroblasts in wounds for overall improvement in wound healing. Curcumin has also been shown to have beneficial effect as a pro-angiogenic agent in wound healing by inducing TGFβ, which induces both angiogenesis and accumulation of extracellular matrix, which continues through the remodelling phase of wound repair (29).
Of the strengths of this study, compared to other studies, we can mention the existence of the three study groups, the appropriate number of samples, and performance of C-section by a single surgeon. The inability to accurately assess the status of Caesarean wound healing by biopsy was one of the limitations of this study.
CONCLUSION
With regard to the positive effects of turmeric on the speed of Caesarean wound healing and the fact that no adverse effects were reported from the use of the ointment in mothers, it is recommended that this drug be used for promotion of Caesarean wound healing in women in the postpartum period.
ACKNOWLEDGMENT
We sincerely appreciate the Research Deputy of the Islamic Azad University of Sari, the Surgery Ward staff of Imam Ali Hospital, Ms Mona Eski and Ms Vahide Aghapoor and all other personnel who helped us conduct this study. We also thank all participants, without whom the completion of this study would not be possible.
REFERENCES
- 1.Villar J, Valladares E, Wojdyla D, Zavaleta N, Carroli G, Velazoo A, et al. Cesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006;367:1819–1829. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 2.Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2006. Natl Vital Stat Rep. 2007;56:1–18. [PubMed] [Google Scholar]
- 3.Black C, Kaye JA, Jick H. Cesarean delivery in the United Kingdom: time trends in the general practice research database. Obstet Gynecol. 2005;106:151–155. doi: 10.1097/01.AOG.0000160429.22836.c0. [DOI] [PubMed] [Google Scholar]
- 4.Gary CF, Gant NF, Leveno KJ, Gilstrap LC, Hauth JC, Wenstrom KD. Williams obstetrics. New York: McGraw-Hill; 2005. pp. 823–829. [Google Scholar]
- 5.Moghareh Abed L, Goharian V, Ghanei M, Adibi P, Goharian A. Cesarean section rate and its indications in I.R. of Iran in 1998. Hakim Res J. 2000;2:147–154. [Google Scholar]
- 6.Mukhopadhyay A, Basu N, Ghatak N, Gujral PK. Anti-inflammatory and irritant activities of curcumin analogues in rats. Agents Actions. 1982;12:508–515. doi: 10.1007/BF01965935. [DOI] [PubMed] [Google Scholar]
- 7.Mohamadbeigi A, Mohammad Salehi N. Modeling of associated factors that affect the method of pregnancy termination. Iran J Obstet Gynecol Infertil. 2009;12:17–24. [Google Scholar]
- 8.Buggy D. Can anaesthetic management influence surgical-wound healing? Lancet. 2000;356:355–357. doi: 10.1016/S0140-6736(00)02523-X. [DOI] [PubMed] [Google Scholar]
- 9.Phuapradit W, Saropala N. Topical application of honey in treatment of abdominal wound disruption. Aust N Z J Obstet Gynaecol. 1992;32:381–384. doi: 10.1111/j.1479-828x.1992.tb02861.x. [DOI] [PubMed] [Google Scholar]
- 10.Anderson ER, Gates S. Techniques and materials for closure of the abdominal wall in Cesarean section. Cochrane Database Syst Rev. 2004;(4):CD004663–CD004663. doi: 10.1002/14651858.CD004663.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Veisi F, Zangeneh M, Malekkhosravi S, Rezavand N, Hemiari K, Rezaei M. Subcutaneous vicryl suture covering efficacy on wound complications after Cesarean section. J Kermanshah Univ Med Sci. 2011;15:157–164. [Google Scholar]
- 12.Humburg J, Holzgreve W, Hoesli I. Negative pressure wound therapy in post-cesarean superficial wound disruption: a report of 3 cases. Wounds. 2006;18:166–169. [Google Scholar]
- 13.Nasrollahi SH, Radnia N, Ghafele-Bashi M. Comparison of wound disruption between three methods: closure of subcutaneous with polyglycolic versus closure of subcutaneous with plain and non-closure after cesarean section. Sci J Hamdan Univ Med Sci. 2007;14:35–39. [Google Scholar]
- 14.Kossi J, Vaha-Kreula M, Peltonen J, Risteli J, Laato M. Effect of sucrose on collagen metabolism in keloid, hypertrophic scar, and granulation tissue fibroblast cultures. World J Surg. 2001;25:142–146. doi: 10.1007/s002680020038. [DOI] [PubMed] [Google Scholar]
- 15.Pradhan GB, Agrawal J. Comparative study of post operative wound infection following emergency lower segment Caesarean section with and without the topical use of fusidic acid. Nepal Med Coll J. 2009;11:189–191. [PubMed] [Google Scholar]
- 16.Shirvani MA, Nikpour M, Azadbakht M, Banihosseini SZ, Zanjani R. The effect of honey gel on cesarean incision pain: a triple blind clinical trial. Afr J Pharm Pharmacol. 2013;7:19–24. [Google Scholar]
- 17.Al-Waili NS, Saloom KY. Effects of topical honey on postoperative wound infections due to gram positive and gram negative bacteria following Cesarean section and hysterectomies. Eur J Med Res. 1999;4:126–130. [PubMed] [Google Scholar]
- 18.Samadi S, Khadivzadeh T, Emami A, Moosavi NS, Tafaghodi M, Behnam HR. The effect of Hypericum perforatum on the wound healing and scar of Cesarean. J Altern Complement Med. 2010;16:113–117. doi: 10.1089/acm.2009.0317. [DOI] [PubMed] [Google Scholar]
- 19.Khadivzadeh T, Molkizadeh M, Rakhshandeh M, Khajedaloui M. The impact of lavender cream on episiotomy pain and wound healing in primiparous women. J Mashhad Sch Nurs Midwifery. 2009;9:19–24. [Google Scholar]
- 20.Golmakani N, Motlagh ER, Tara F, Assili J, Shakeri MT. The effects of turmeric (Curcuma longa L) ointment on healing of episiotomy site in primiparous women. Iran J Obstet Gynecol Infertil. 2009;11:29–38. [Google Scholar]
- 21.Fallah Huseini H, Zahmatkash M, Haghighi M. A review on pharmacological effects of Curcuma longa L (turmeric) J Med Plants. 2010;1:1–15. [Google Scholar]
- 22.Kohli K, Ali J, Ansari M, Raheman Z. Curcumin: a natural antiinflammatory agent. Indian J Pharmacol. 2005;37:141–147. [Google Scholar]
- 23.Jagetia GC, Rajanikant GK. Acceleration of wound repair by curcumin in the excision wound of mice exposed to different doses of fractionated γ radiation. Int Wound J. 2012;9:76–92. doi: 10.1111/j.1742-481X.2011.00848.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.López-Jornet P, Camacho-Alonso F, Jiménez-Torres MJ, Orduña-Domingo A, Gómez-Garcia F. Topical curcumin for the healing of carbon dioxide laser skin wounds in mice. Photomed Laser Surg. 2011;29:809–814. doi: 10.1089/pho.2011.3004. [DOI] [PubMed] [Google Scholar]
- 25.Ungphaiboon S, Supavita T, Singchangchai P, Sungkarak S, Rattanasuwan P, Itharat A. Study on antioxidant and antimicrobial activities of turmeric clear liquid soap for wound treatment of HIV patients. Songklanakarin J Sci Technol. 2005;27:269–578. [Google Scholar]
- 26.Sidhu GS, Mani H, Gaddipati JP, Singh AK, Seth P, Banaudha KK, et al. Curcumin enhances wound healing in streptozotocin induced diabetic rats and genetically diabetic mice. Wound Repair Regen. 1999;7:362–374. doi: 10.1046/j.1524-475x.1999.00362.x. [DOI] [PubMed] [Google Scholar]
- 27.Mani H, Sidhu GS, Kumari R, Gaddipati JP, Seth P, Maheshwari RK. Curcumin differentially regulates TGF-beta1, its receptors and nitric oxide synthase during impaired wound healing. Biofactors. 2002;16:29–43. doi: 10.1002/biof.5520160104. [DOI] [PubMed] [Google Scholar]
- 28.Maheshwari RK, Singh AK, Gaddipati J, Srimal RC. Multiple biological activities of curcumin: a short review. Life Sci. 2006;78:2081–2087. doi: 10.1016/j.lfs.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 29.Thangapazham RL, Sharma A, Maheshwari RK. Beneficial role of curcumin in skin disease. Adv Exp Med Bio. 2007;595:343–357. doi: 10.1007/978-0-387-46401-5_15. [DOI] [PubMed] [Google Scholar]
- 30.Attarpour Yazdi MM. Antibacterial activity of Curcuma longa extract against bacteria isolated from infected burn wounds. Planta Med. 2009;75:PJ156–PJ156. [Google Scholar]
- 31.Kundu S, Biswas TK, Das P, Kumar S, De DK. Turmeric (Curcuma longa) rhizome paste and honey show similar wound healing potential: a preclinical study in rabbits. Int J Low Extrem Wounds. 2005;4:205–213. doi: 10.1177/1534734605281674. [DOI] [PubMed] [Google Scholar]
- 32.Davidson NS. REEDA: Evaluating postpartum healing. J Nurse Midwifery. 1974;19:6–8. [PubMed] [Google Scholar]
- 33.Carvalho B, Clark DJ, Angst MS. Local and systemic release of cytokines, nerve growth factor, prostaglandin E2, and substance P in incisional wounds and serum following Cesarean delivery. J Pain. 2008;9:650–657. doi: 10.1016/j.jpain.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 34.Kang BY, Song YJ, Kim K, Choe YK, Hwang SY, Kim TS. Curcumin inhibits Th1 cytokine profile in CD4+ T cells by suppressing interleukin-12 production macrophages. Br J Pharmacol. 1999;128:380–384. doi: 10.1038/sj.bjp.0702803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Biswas SK, McClure D, Jimenez LA, Megson IL, Rahman I. Curcumin induces glutathione biosynthesis and inhibits NF-κB activation and interleukin-8 release in alveolar epithelial cells: mechanism of free radical scavenging activity. Antioxid Redox Signal. 2005;7:32–41. doi: 10.1089/ars.2005.7.32. [DOI] [PubMed] [Google Scholar]