Abstract
Nitrogen dioxide (NO2), a by-product of combustion produced by indoor gas appliances such as cooking stoves, is associated with respiratory symptoms in those with obstructive airways disease. We conducted a three-armed randomized trial to evaluate the efficacy of interventions aimed at reducing indoor NO2 concentrations in homes with unvented gas stoves: (i) replacement of existing gas stove with electric stove; (ii) installation of ventilation hood over existing gas stove; and (iii) placement of air purifiers with high-efficiency particulate air (HEPA) and carbon filters. Home inspection and NO2 monitoring were conducted at 1 week pre-intervention and at 1 week and 3 months post-intervention. Stove replacement resulted in a 51% and 42% decrease in median NO2 concentration at 3 months of follow-up in the kitchen and bedroom, respectively (P = 0.01, P = 0.01); air purifier placement resulted in an immediate decrease in median NO2 concentration in the kitchen (27%, P < 0.01) and bedroom (22%, P = 0.02), but at 3 months, a significant reduction was seen only in the kitchen (20%, P = 0.05). NO2 concentrations in the kitchen and bedroom did not significantly change following ventilation hood installation. Replacing unvented gas stoves with electric stoves or placement of air purifiers with HEPA and carbon filters can decrease indoor NO2 concentrations in urban homes.
Keywords: Indoor air, Nitrogen dioxide, Housing intervention, Urban environment, Gas stove, Air purifier
Introduction
Nitrogen dioxide (NO2), a by-product of combustion, is produced by several sources unique to the indoor environment, including gas stoves and gas heaters. Current evidence suggests that exposure to higher indoor NO2 concentrations leads to symptoms in children with asthma, including chest tightness, shortness of breath, wheeze, cough, nocturnal symptoms, and an increased number of asthma attacks (Belanger et al., 2006; Garrett et al., 1998; Hansel et al., 2008). In addition, we have recently reported that exposure to higher indoor NO2 concentrations is associated with increased respiratory symptoms and risk of COPD exacerbations in former smokers with moderate to severe COPD (Hansel et al., 2013).
Consequently, interventions that are successful at reducing indoor NO2 concentrations may be beneficial to improving respiratory health in patients with obstructive lung diseases. In fact, current guidelines suggest that patients with asthma ‘avoid exposure to gas stoves and appliances that are not vented to the outside (Evidence C)’ and that ‘efficient ventilation, non-polluting cooking stoves, use of flues, and similar interventions are feasible and should be recommended (Evidence B)’ to patients with COPD (Global Strategy for Diagnosis, Management, and Prevention of COPD, 2013; National Heart, Lung, and Blood Institute National Asthma Education and Prevention Program, 2007). Despite these recommendations, very little is known about what home interventions will reduce indoor NO2 concentrations.
In Baltimore City, like many urban communities, unvented gas stoves are common, and the presence of a gas stove in the home is independently associated with higher indoor NO2 concentrations (Hansel et al., 2008). We designed a randomized, three-armed intervention trial to assess whether home interventions targeting unvented gas stoves can decrease indoor NO2 concentrations and whether such interventions are feasible given the characteristics of each approach (Table 1). Homes in Baltimore City with unvented gas stoves were assigned to receive one of the following three interventions: (i) replacement of existing gas stove with an electric stove; (ii) installation of ventilation hood over existing gas stove; and (iii) placement of portable air purifiers in the home. To our knowledge, there have been no randomized trials that examine the impact of interventions focusing on gas stoves on concentrations of indoor NO2 in residential environments.
Table 1.
Characteristics of interventions. Qualitative comparison of each intervention arm (stove replacement, air purifier, and ventilation hood)
| Stove replacement | Air purifier | Ventilation hood | |
|---|---|---|---|
| Equipment costa | $390 | $500 | $65 |
| Installation costa | Professional installation required; $1875 (includes removal of old stove) | Easy to set up, no professional help needed | Professional installation required; $1,900 |
| Operating costa | Cost of electricity to operate stove | Cost of electricity to operate air purifier, cost of replacement air filters; $215 | Cost of electricity to operate hood |
| Adherence | No additional steps needed to derive benefit | Must turn on to derive benefit | Must turn on to derive benefit |
| Maintenance | None required | Replacement of air filters according to manufacturer instructions | None required |
| Target of intervention | Addresses pollution derived from stove use | Addresses multiple potential sources of pollution | Addresses pollution derived from stove use |
The costs listed represent the average cost of the appliances used in this study but may vary depending on make/model purchased. Installation costs may vary depending on home infrastructure.
Methods
Homes were recruited between June 2009 and March 2011 in partnership with the Baltimore City Health Department’s Healthy Homes Inspections and Health (HHIH) Services Program, which aims to reduce home-based factors that are major sources of health hazards and chronic health issues. Contact information of interested individuals receiving services from HHIH was forwarded to Johns Hopkins study staff, and individuals were contacted via telephone to determine whether their home was appropriate for randomization to assess the impact of home interventions on indoor NO2 concentration. Preliminary eligibility was based on the following inclusion criteria: (i) the presence of unvented gas stove (combination cooktop and oven, fueled by gas, which is not ventilated with either a vented range hood or an overhead kitchen exhaust fan) and (ii) home occupant and home owner willing to provide informed consent. If eligible based on the telephone screening evaluation, homes were visited by a member of the study team for further evaluation and home assessment. In addition to the above criteria, homes were eligible if interventions were feasible based on home assessment, including sufficient electric service and structural design that did not prohibit interventions. Homes were ineligible if the home owner or home occupant planned to change residences within the study period or if there were foster children residing in the home. The study was reviewed and approved by the Johns Hopkins Medical Institutional Review Board. Written consent was obtained from the home owner.
Randomization
Randomization into one of the following three interventions was performed using block randomization by season. In our previous studies in Baltimore City, the NO2 concentration was 16 ppb higher in homes with a gas stove compared with those without (Hansel et al., 2008). Using these data, sample size was calculated with an estimated 82% power to detect NO2 changes in a similar magnitude pre- and post-intervention. Given the uncertainty of the ability of the air purifier to reduce NO2 concentrations, and estimated only moderate compliance with air purifier use, a 1:1:2 (stove replacement: ventilation hood: air purifier) randomization scheme was employed to ensure a larger sample of homes receiving the air purifier.
Stove replacement: Existing gas stoves were removed and replaced with stoves with electric resistance coils [including models from Roper™ (La Fayette, GA, USA), Maytag® (Benton Harbor, MI, USA), and Whirlpool® (Benton Harbor, MI, USA)] and convection and self-cleaning electric ovens. A general contractor was hired to install the stoves according to the manufacturer’s guidelines.
Ventilation hood: Range hoods [BROAN® (Hartford, WI, USA) Range Hood model numbers 433611, 403001, or 423001] with ventilation fans to the outdoors and secure seal to minimize energy loss were installed over existing gas stoves. The manufacturer lists the flow rates for the models used as 160–220 cubic feet per minute. A general contractor was hired to install the ventilation hoods according to the manufacturer’s guidelines.
Air purifier placement: Two ENERGY STAR® efficient air purifiers containing HEPA and activated carbon filters (Austin HealthMate®, Austin Air: Buffalo, NY, USA), which can adsorb gases including NO2 (Rubel et al., 1995), were placed in the home. Manufacturer-provided flow rates are 75, 200, and 400 cubic feet per minute on the low, medium, and high settings, respectively. Participants were encouraged to use the air purifiers on the high setting. The filter has a life expectancy of 5 years and was therefore not changed during the study period. One air purifier was placed in the kitchen and the other in the main bedroom.
Household inspection
All participants that were determined to be eligible based on the initial home assessment visit had home inspections and air quality assessment at baseline (1 or 2-weeks pre-intervention) and at 1 week and 3 months post-intervention. At the baseline visit, trained study staff completed a comprehensive home inspection with a focus on heating and cooling mechanisms, dryer type, and type of stove. At each follow-up visit, a briefer home inspection was completed that documented use of heating and cooling systems, the presence of smoking during the visit, and if the home had been assigned to the air purifier intervention, whether or not the air purifier was in use during the visit.
Environmental monitoring
Indoor air monitoring by trained technicians was completed over 7 days at each monitoring period. Week-long integrated NO2 samples were collected using a passive sampler (Ogawa badge) loaded with filters coated with triethanolamine (TEA) placed in the kitchen and main bedroom (Palmes et al., 1976). The median limit of detection (LOD) was 2.03 ppb. All analytical batches included 10% field and laboratory blanks and duplicates.
To evaluate the relationship between ambient and indoor NO2 concentrations, weekly ambient NO2 concentrations from the Baltimore City EPA monitoring station #24-510-0040 were collected. All homes were located within 6 miles of the monitoring site.
Statistical analysis
We compared continuous variables using Student’s two-tailed t-test or the Kruskal–Wallis test, as appropriate. We determined differences for categorical variables by Pearson’s chi-square or Fisher’s exact test, as appropriate. Post-intervention NO2 concentrations were compared with baseline concentrations using the Wilcoxon–Mann–Whitney test. Log-transformed ambient and corresponding indoor NO2 concentrations were compared for each baseline, 1-week, and 3-month monitoring period using Pearson’s correlation. Subsequently, to evaluate the impact of season on effectiveness of interventions at reducing indoor NO2 concentrations, the change in NO2 concentration following intervention (at 1 week and 3 months) in homes that had their baseline visit during the Baltimore heating season (November 1–March 1, Baltimore Gas and Electric) was compared with those in the non-heating season using the Wilcoxon–Mann–Whitney test. Similar comparisons were made in homes that had gas furnaces vs. those without, and in homes with gas dryers vs. those without. All analyses were performed with Stata-SE version 12.0 (StataCorp, College Station, TX, USA). A two-tailed P-value < 0.05 was used to detect statistically significant differences.
Results
Two hundred and eighty-one home occupants expressed interest in the study, 39 of which failed the telephone screening [no longer interested (n = 21), did not want electric stove (n = 15), lived in apartment without landlord consent (n = 2), and already had electric stove (n = 1)]. Of the remaining 242 homes, 47 did not have a home assessment due to scheduling difficulties. One hundred and ninety-five homes underwent home assessments to determine eligibility. Fifty-seven of these homes did not meet eligibility because the stove was located too far from the exterior wall, and placing a ventilation hood to the outdoors was not feasible given the budget and capability of the general contractor. Thirty additional homes did not meet eligibility due to reasons including electrical limitations (n = 7), landlord objection (n = 4), lack of space for ventilation hood (n = 4), and an additional eight homes lost interest in the study prior to randomization. One hundred homes were randomized, of which 78 homes received an intervention, with 17 homes receiving an electric stove, 15 homes receiving ventilation hood, and 46 homes receiving air purifiers. Twenty-two homes did not receive intervention, mainly due to difficulty contacting the home owner to arrange for intervention or home owner dissatisfaction with randomization results (Figure 1). These homes did not have the baseline visit and thus did not undergo the home inspection.
Fig. 1.
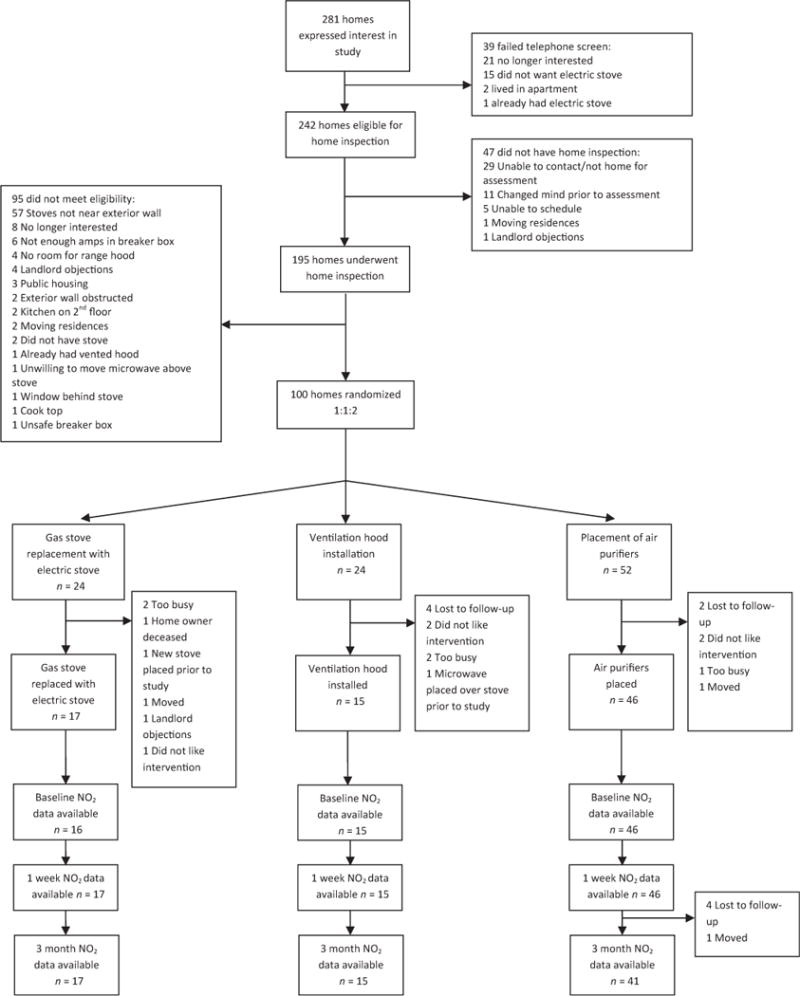
Flow diagram of study outlining home assessment, randomization into study branches, and follow-up of 3 months (NO2 = nitrogen dioxide)
Of the 78 homes receiving intervention, the majority of participants owned their home (89%), were African American (91%), and had a greater than high school education (56%). Less than half of home owners were employed, and home owners randomized to receive a ventilation hood were less likely to be employed (Table 2). The majority of homes had other gas appliances, including 91% with natural gas burning furnaces and 39% with gas-fueled clothes dryers. One quarter (25%) of homes had continuous pilot lights in their gas stoves. Approximately 30% of homes had any smoking in the home, and when present, overall smoking was low with the mean number of cigarettes smoked indoors per day of 2.9 ± 6.8 cigarettes. The median baseline NO2 concentration was 17.9 ppb (range 3.2, 71.4), and 13.1 ppb (range 3.4, 41.8) in the kitchen and bedroom, respectively (difference between the kitchen and bedroom P-value < 0.01). Although homes receiving a ventilation hood tended to have lower baseline kitchen NO2 concentrations, there was no statistical difference in baseline NO2 concentrations between groups (Table 2).
Table 2.
Home owner and housing characteristics. Descriptive data of participants and details of home and housing structure by total study population and by study arm (stove replacement, air purifier, and ventilation hood)
| All homes (n = 78) | Stove replacement (n = 17) | Air purifier (n = 46) | Ventilation hood (n = 15) | |
|---|---|---|---|---|
| Home owner characteristics | ||||
| African American race, n (%) | 71 (91.0) | 16 (94.1) | 42 (91.3) | 13 (86.7) |
| Full- or part-time employment, n (%)* | 29 (37.2) | 7 (41.2) | 19 (41.4) | 3 (20.0) |
| >High school education, n (%) | 44 (56.4) | 8 (53.3) | 28 (60.9) | 8 (53.3) |
| Age, mean (SD) | 53.5 (13.8) | 52.0 (12.0) | 51.5 (15.0) | 59.0 (10.3) |
| Housing characteristics | ||||
| Reporting any smoking in home, n (%) | 21 (27.3) | 5 (29.4) | 11 (24.4) | 5 (33.3) |
| Owner occupied, n (%) | 69 (88.5) | 15 (88.2) | 40 (87.0) | 14 (93.3) |
| Row house, n (%) | 67 (85.9) | 13 (76.5) | 41 (89.1) | 13 (86.7) |
| Central air conditioning, n (%) | 17 (21.8) | 4 (23.5) | 11 (23.9) | 2 (13.3) |
| Natural gas furnace, n (%) | 71 (91.0) | 15 (88.2) | 42 (91.3) | 14 (93.3) |
| Gas dryer, n (%) | 30 (38.5) | 5 (29.4) | 19 (41.3) | 6 (40.0) |
| Continuous pilot light on stove, n (%) | 19 (24.7) | 5 (29.4) | 11 (24.4) | 3 (20.0) |
| [NO2] in kitchen at baseline (ppb), median (range) | 17.9 (3.2, 85.3) | 19.7 (9.2, 70.2) | 19.2 (6.8, 85.3) | 12.2 (3.2, 53.3) |
| [NO2] in bedroom at baseline (ppb), median (range) | 13.1 (3.4, 41.8) | 16.9 (6.9, 41.8) | 12.4 (3.4, 35.1) | 13.1 (5.3, 39.2) |
NO2, nitrogen dioxide; ppb, parts per billion.
P-value < 0.05.
At 1 week following the intervention, replacement of a gas stove with an electric stove resulted in a 44% decrease in the median kitchen NO2 concentration, and 69% percent of homes receiving this intervention had a decrease in kitchen NO2 concentrations. At 3 months post-intervention, replacement of a gas stove with an electric stove resulted in a 51% decrease in the median kitchen NO2 concentration (Figure 2), and 88% percent of homes had a decrease in NO2 concentrations (Table S1). In the bedroom, replacement of a gas stove with an electric stove resulted in a 31% decrease in median NO2 at 1 week and a 42% decrease in median NO2 concentration at 3 months (Figure 3). Three-quarters (75%) of homes had a decrease in NO2 concentration at 3 months (Table S1).
Fig. 2.

NO2 concentrations by study arm: kitchen. Displays median kitchen NO2 concentration for each study arm (stove replacement, air purifier, and ventilation hood) at baseline, 1-week, and 3-month follow-up. (NO2 = nitrogen dioxide, ppb = parts per billion)
Fig. 3.
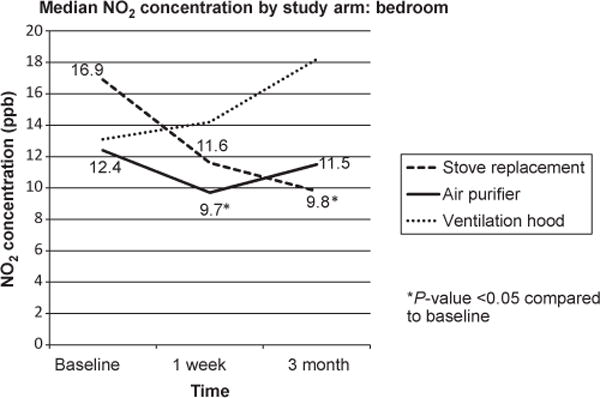
NO2 concentrations by study arm: bedroom. Displays median bedroom NO2 concentration for each study arm (stove replacement, air purifier, and ventilation hood) at baseline, 1-week, and 3-month follow-up. (NO2 = nitrogen dioxide, ppb = parts per billion)
Placement of air purifiers with HEPA and carbon filters resulted in a 27% decrease in median kitchen NO2 concentration at 1 week, and 76% of homes receiving the air purifiers had a decrease in NO2 concentration. At 3 months post-intervention, placement of air purifiers resulted in a 19% decrease in kitchen median NO2 concentration (Figure 2) and two-thirds (66%) of homes had a decrease in kitchen NO2 concentration (Table S1). In the bedroom, placement of air purifiers resulted in a 23% decrease in median NO2 at 1 week, but NO2 concentrations were not significantly different from baseline at 3 months of follow-up (Figure 3). 61% and 54% of homes had a decrease in NO2 concentrations in the bedroom at 1 week and 3 months of follow-up, respectively (Table S1). The majority (85%) of homes in the air purifier intervention arm had the kitchen air purifier turned on during home inspection at the 3-month follow-up visit.
NO2 concentrations in the kitchen and bedroom did not significantly change following ventilation hood installation (n = 15): (kitchen: median NO2 at baseline = 12.2 ppb; median NO2 at 1 week = 25.5 ppb, P-value compared with baseline = 0.14; median NO2 at 3 months = 24.7 ppb, P-value compared with baseline = 0.11 and bedroom: median NO2 at baseline = 13.1 ppb; median NO2 at 1 week = 14.2 ppb, P-value compared with baseline = 0.68; median NO2 at 3 months = 18.2 ppb, P-value compared with baseline = 0.18) (Table S2).
Kitchen NO2 concentrations at 1 week were significantly different between the intervention arms (P-value = 0.04). In addition, there was a statistically significant difference in kitchen NO2 concentrations between each intervention arm at 3 months of follow-up (P-value < 0.01). Bedroom NO2 concentrations at 1 week were not significantly different between the intervention arms; there was a statistically significant difference in bedroom NO2 concentrations between each intervention arm at 3 months of follow-up (P-value = 0.03; Table S2).
Median ambient NO2 concentrations were 28.8, 29.8, and 28.9 ppb at baseline, 1 week, and 3 months, respectively. There was no statistically significant difference in ambient NO2 concentrations across study visits for both the entire cohort and by study arm and no significant difference between study arms at each time period (Table S3). Furthermore, there was no statistically significant correlation between ambient NO2 and indoor NO2 concentrations at any visit across study arms (data not shown).
Because over 90% of our study homes had gas furnaces, it is difficult to determine whether the presence of a gas furnace modified the effect of our interventions. However, there was no statistically significant difference in the change in NO2 concentrations (1-week baseline; 3-month baseline) between homes with natural gas heat and homes without, for each intervention group (all P > 0.05). Similarly, 38.5% of study homes had a gas dryer, and there was no statistically significant difference in the change in NO2 concentrations between homes with a gas dryer and homes without, for each intervention group (all P > 0.05). While 13 homes in our study reported use of a space heater, all were electric and thus did not likely contribute to indoor NO2 concentrations (data not shown).
Homes with stoves that had continuous pilot lights had higher baseline concentrations of NO2 in both the kitchen and bedroom (kitchen: 27.1 vs. 14.8 ppb, P < 0.01; bedroom: 18.1 vs. 11.7 ppb, P < 0.01) compared with those with auto-ignite pilot lights. Subsequently, interventions, including stove replacement and placement of air purifiers, tended to be associated with a greater reduction in median NO2 concentrations in homes with stoves with continuous pilot lights (Table S4).
Eighteen (23%) of homes had their baseline visit during the heating season of November 1–March 31. There were no statistically significant differences in the change in indoor NO2 concentration at 1 week and 3 months of follow-up between homes with baseline visits in the heating vs. non-heating season (all P > 0.05).
Discussion
To our knowledge, this is the first randomized intervention study focusing on gas stoves as the primary target of remediation of indoor NO2 concentrations and shows that in-home interventions targeting gas stoves can reduce NO2 concentrations in urban homes. Specifically, replacing unvented gas stoves with electric stoves reduced NO2 concentrations by 51% and 42% in the kitchen and bedroom, respectively, indicating that stove replacement may impact NO2 concentrations beyond the kitchen. Further, these reductions in NO2 concentrations were observed despite the majority of homes having other gas-powered appliances such as gas furnaces and clothes dryers. In addition, placement of air purifiers with HEPA and carbon filters in the home results in a nearly 27% decrease in median kitchen NO2 concentrations immediately (1 week after placement), and reductions are maintained at 3 months following intervention. These results show that simple home interventions may reduce indoor NO2 concentrations and the results of this study can be used to guide future intervention studies assessing the health benefits of NO2 exposure reduction.
We have previously shown that the presence of a gas stove was the largest contributor to indoor NO2 concentrations in Baltimore homes, even in homes with a gas furnace (Hansel et al., 2008). This finding may be partly explained by Baltimore City building codes that specify ventilation requirements for furnaces, but do not require venting range hoods or other kitchen ventilation for gas cooking appliances. Furthermore, a recent study utilizing a simulation model suggests that 60% of homes using gas stoves without adequate ventilation will have NO2 concentrations that exceed national health-based standards (Logue et al., 2013). Accordingly, replacing gas stoves with electric stoves was associated with the largest drop in indoor NO2 concentrations. Furthermore, NO2 concentrations were also decreased in the bedroom, indicating that replacing the predominant source of NO2 may have a benefit throughout the home, not only the kitchen. The placement of an electric stove was associated with an initial $300–500 cost of the stove, plus the expense of installation. Although the increased cost of electricity may be an issue for lower income households, there are minimal potential additional costs once the stove is installed. Further, the efficacy of this intervention is not dependent on behavior or adherence (e.g., turning on the ventilation hood or air purifier).
We also found a significant decrease in NO2 concentrations with the use of air purifiers with HEPA and carbon filters. Activated carbon filters in home air purification devices can adsorb NO2 (Rubel et al., 1995). Our results support our previous post hoc analysis of a home intervention study showing decreased indoor NO2 concentrations at 6 months of follow-up in homes outfitted with an air purifier with HEPA and carbon filter (Rusher et al., 2008). However, in the current study, sustained reduction in NO2 concentrations was only observed in the kitchen; bedroom NO2 concentrations at 3 months were no longer statistically different from baseline. As inspector-documented compliance was assessed only in the kitchen and not in the bedroom, we do not know whether or not the lack of improvement in bedroom NO2 was due to lack of use of the air purifier in that location. Documented adherence to air purifier use was relatively high in this study (85% of kitchen air purifiers being turned on when home inspection occurred at 3 months), and prior research by our group has shown that even modest adherence (59%) to air purifier use can result in a decrease in indoor particulate matter (PM) concentrations and improved respiratory health in children with asthma (Butz et al., 2011). Given the previous studies showing the efficacy of air purifiers in reducing PM, air purifiers may be an attractive option for decreasing concentrations of multiple pollutants within the home, if PM reduction is also a goal. Furthermore, air purifiers may also target other potential sources of NO2 in the home, not just stoves, and may be considered if additional sources of NO2 are thought to be a major contributor to indoor NO2 concentrations. Costs of air purifiers can be high, with additional ongoing costs required for replacement of filters and the energy cost of running the air purifiers.
Ventilation hood installation did not significantly reduce indoor NO2 concentrations in our study, and there was a trend toward higher NO2 concentrations in follow-up visits, although not statistically significant. The reason for the lack of efficacy of ventilation hoods is uncertain. Home inspection visits did not necessarily occur at times when stoves were in use to allow for inspector-documented adherence, and we did not ask participants to track ventilation hood use; thus, it is unclear if the lack of efficacy is due primarily to lack of use of the hoods. There may also have been changes in cooking behaviors that were unaccounted for. In addition, the overall function and ability of the ventilation hood to clear NO2 remains largely unknown. Research by Singer et al. suggests that ventilation hoods have measured maximum airflows that are approximately 70% of reported manufacturer values (Singer et al., 2012). In addition, in studies of carbon dioxide, the capture efficiency (fraction of generated pollutants that are captured by range hood) varies highly among ventilation hood models and depends on location of burner use (front vs. back burners); models with high capture efficiency are often prohibitively loud for use in a residential environment (Delp and Singer, 2012). These studies, some of which are conducted in a controlled laboratory environment, highlight the potential variability in effectiveness of ventilation hoods, which would only be exacerbated when used in a real world, residential environment. It is also important to note that broad implementation of this intervention would be difficult in Baltimore homes as housing structure and kitchen design often made installation of ventilation hoods complex and costly, limiting the number of homes available for the intervention in our study.
Previously, only a few studies have examined the impact of modifying the indoor environment to decrease indoor concentrations of NO2. In their non-randomized study of three apartment buildings in California, Noris et al. reported a decrease in indoor NO2 in apartments receiving a variety of retrofits aimed at improving overall indoor air quality (Noris et al., 2013). The remainder of studies have focused primarily on the replacement of unvented gas heaters, two of which were conducted in schools. A randomized, double-blinded crossover study replacing unflued gas heaters with vented heaters in classrooms in Australia showed that classrooms with unflued gas heaters had concentrations of NO2 that were nearly double those in intervention classrooms (31.6 ppb vs. 17.5 ppb). The higher concentration of NO2 in non-intervention classrooms was associated with increased report of cough and wheeze among students (Marks et al., 2010). Similarly, Pilotto et al. replaced unflued gas heaters in eighteen public schools in Australia with flued gas heaters or electric heaters. Mean NO2 concentrations post-intervention were 15.5 ppb in the classrooms receiving new heaters compared with 47 ppb in control classrooms. Frequency of asthma symptoms was lower in children with asthma in class-rooms receiving the intervention (Pilotto et al., 2004). A home intervention study in New Zealand showed that homes receiving more efficient heating devices (heat pumps, wood pellet burner, or high capacity flued gas heater) in place of unflued gas heaters had lower NO2 concentrations than control homes. This decrease was associated with a reduction in asthma symptoms and healthcare utilization in children with asthma living in intervention homes. Symptom improvement occurred even though NO2 concentrations were moderate low (4.5 ppb in intervention homes, 8.4 ppb in control homes) (Howden-Chapman et al., 2008).
Our baseline NO2 concentrations were on average slightly higher than that reported in the homes in Howden-Chapman et al’s. study, but lower than in our previous Baltimore City studies (30 ppb) (Hansel et al., 2008). Furthermore, our reduction in NO2 concentrations achieved with replacement of a gas stove for electric stove, or placement of air purifiers with carbon filters, although modest, was similar to the degree of NO2 reduction seen by gas heater interventions in the previous studies. Although it is possible that the observed percentage of homes that had a decrease in NO2 could be attributable to natural temporal variability in NO2 in a home without intervention, the statistically significant decrease in median NO2 in the stove and air purifier intervention arms compared with the ventilation hood group suggests that these reductions were not due to chance alone. Importantly, reductions in NO2 concentrations of a similar magnitude as those in this study have been linked with measureable health improvements in patients with asthma, suggesting that home interventions targeting gas stoves may result in reductions in NO2 concentrations adequate to improve respiratory health in susceptible individuals.
Concentration of indoor NO2 is impacted by many factors, including occupant behaviors, air exchange rates in the home, and ambient NO2 concentrations (Schwab et al., 1994; Spengler et al., 1996). In our study homes, the correlation between ambient NO2 and indoor NO2 was not statistically significant, and thus, ambient NO2 likely does not confound the relationship between the interventions and follow-up indoor NO2 concentrations. Although the majority of homes in our sample were row houses and thus have similar construction characteristics, we did not measure home volumes or air exchange rates. Similarly, cooking frequency and duration was not measured, nor was use of the ventilation hood and bedroom air purifier. The lack of these measurements makes it difficult to account for the myriad of factors that impact NO2 concentrations within a home. However, this study was designed to evaluate the overall efficacy of home interventions in real world, inner-city homes with typical appliance use. The changes in indoor NO2 that were found in our study are reflective of how these interventions perform in homes without coaching or instruction to change daily activity patterns, and the magnitude of benefit of these interventions depends on each home’s unique characteristics and occupant behavior patterns. Finally, our findings reflect the performance of these interventions in our study sample in Baltimore City and thus may not be generalizable to communities that differ from our study population.
In summary, we found that in homes with unvented gas stoves, replacing gas stoves with electric stoves or placing air purifiers with carbon filters reduces indoor NO2 concentrations within 1 week and up to 3 months following intervention. Replacing the gas stove with an electric stove results in the greatest reduction in median NO2 concentrations. Understanding the health benefit of reducing indoor NO2 concentrations is an important next step in providing much needed information about the health effects of modifying the indoor environment. Such information is needed to continue to inform guideline development and provide tangible data to healthcare providers seeking to counsel patients with respiratory disease on exposures in their home environment.
Supplementary Material
Table S1 Percentage of homes at each sampling visit with a decrease in median indoor NO2 following intervention.
Table S2 Median indoor NO2 by location, study arm, and sampling visit.
Table S3 Median ambient NO2 by study arm and sampling visit.
Table S4 Median change in NO2 (ppb) by pilot light.
Practical Implications.
Several combustion sources unique to the residential indoor environment, including gas stoves, produce nitrogen dioxide (NO2), and higher NO2 concentrations, are associated with worse respiratory morbidity in people with obstructive lung disease. A handful of studies have modified the indoor environment by replacing unvented gas heaters; this study, to our knowledge, is the first randomized study to target unvented gas stoves. The results of this study show that simple home interventions, including replacement of an unvented gas stove with an electric stove or placement of HEPA air purifiers with carbon filters, can significantly decrease indoor NO2 concentrations.
Acknowledgments
This study was made possible by funding from United States Department of Housing and Urban Development Grant #FR-5200-N-01A. We would like to thank Sarah Norman, Genevieve Birkby, and all of the staff of the Baltimore City Healthy Homes team. We are grateful to Austin Air® for the donation of the HealthMate® air purifiers used in the study. This work was supported by grants from the NIEHS (ES015781, ES015903, ES018176, R01ES022607) and the EPA (RD83451001).
Footnotes
Supporting Information
Additional Supporting Information may be found in the online version of this article:
References
- Belanger K, Gent JF, Triche EW, Bracken MB, Leaderer BP. Association of indoor nitrogen dioxide exposure with respiratory symptoms in children with asthma. Am J Respir Crit Care Med. 2006;173:297–303. doi: 10.1164/rccm.200408-1123OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butz AM, Matsui EC, Breysse P, Curtin-Brosnan J, Eggleston P, Diette G, Williams D, Yuan J, Bernert JT, Rand C. A randomized trial of air cleaners and a health coach to improve indoor air quality for inner-city children with asthma and secondhand smoke exposure. Arch Pediatr Adolesc Med. 2011;165:741–748. doi: 10.1001/archpediatrics.2011.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delp WW, Singer BC. Performance assessment of U.S. residential cooking exhaust hoods. Environ Sci Technol. 2012;46:6167–6173. doi: 10.1021/es3001079. Epub 2012 May 17. [DOI] [PubMed] [Google Scholar]
- Garrett MH, Hooper MA, Hooper BM, Abramson MJ. Respiratory symptoms in children and indoor exposure to nitrogen dioxide and gas stoves. Am J Respir Crit Care Med. 1998;158:891–895. doi: 10.1164/ajrccm.158.3.9701084. [DOI] [PubMed] [Google Scholar]
- Global Strategy for Diagnosis Management Prevention of COPD. 2013 [Google Scholar]
- Hansel NN, Breysse PN, McCormack MC, Matsui EC, Curtin-Brosnan J, Williams DL, Moore JL, Cuhran JL, Diette GB. A longitudinal study of indoor nitrogen dioxide levels and respiratory symptoms in inner-city children with asthma. Environ Health Perspect. 2008;116:1428–1432. doi: 10.1289/ehp.11349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansel NN, McCormack MC, Belli A, Matsui EC, Peng RD, Aloe C, Paulin L, Williams DL, Diette GB, Breysse PN. In-home air pollution is linked to respiratory morbidity in former smokers with COPD. Am J Respir Crit Care Med. 2013;187:1085–1090. doi: 10.1164/rccm.201211-1987OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howden-Chapman P, Pierse N, Nicholls S, Gillespie-Bennett J, Viggers H, Cunningham M, Phipps R, Boulic M, Fjallstrom P, Free S, Chapman R, Lloyd B, Wickens K, Shields D, Baker M, Cunningham C, Woodward A, Bullen C, Crane J. Effects of improved home heating on asthma in community dwelling children: randomised controlled trial. BMJ. 2008;337:a1411. doi: 10.1136/bmj.a1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logue JM, Klepeis NE, Lobscheid AB, Singer BC. Pollutant exposures from natural gas cooking burners: a simulation-based assessment for Southern California. Environ Health Perspect. 2013 doi: 10.1289/ehp.1306673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks GB, Ezz W, Aust N, Toelle BG, Xuan W, Belousova E, Cosgrove C, Jalaludin B, Smith WT. Respiratory health effects of exposure to low-NOx unflued gas heaters in the classroom: a double-blind, cluster-randomized, crossover study. Environ Health Perspect. 2010;118:1476–1482. doi: 10.1289/ehp.1002186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Heart, Lung, and Blood Institute National Asthma Education and Prevention Program; 2007. National Heart Lung and Blood Institute National Asthma Education and Prevention Program. [Google Scholar]
- Noris F, Adamkiewicz G, Delp W, Hotchi T, Russell M, Singer B, Spears M, Vermeer K, Fisk W. Indoor environmental quality benefits of apartment energy retrofits. Build Environ. 2013;68:170–178. [Google Scholar]
- Palmes ED, Gunnison AF, DiMattio J, Tomczyk C. Personal sampler for nitrogen dioxide. Am Ind Hyg Assoc J. 1976;37:570–577. doi: 10.1080/0002889768507522. [DOI] [PubMed] [Google Scholar]
- Pilotto LS, Nitschke M, Smith BJ, Pisaniello D, Ruffin RE, McElroy HJ, Martin J, Hiller JE. Randomized controlled trial of unflued gas heater replacement on respiratory health of asthmatic schoolchildren. Int J Epidemiol. 2004;33:208–214. doi: 10.1093/ije/dyh018. [DOI] [PubMed] [Google Scholar]
- Rubel AM, Stewart ML, Stencel JM. Activated carbon for control of nitrogen oxide emissions. J Mater Res. 1995;10:562–567. [Google Scholar]
- Rusher RR, Hansel NN, Breysse PN. In-home use of air purifiers and indoor nitrogen dioxide levels. Am J Respir Crit Care Med. 2008:A555. [abstract] [Google Scholar]
- Schwab M, McDermott A, Spengler JD, Samet JM, Lambert WE. Seasonal and yearly patterns of indoor nitrogen dioxide levels: data from Albuquerque, New Mexico. Indoor Air. 1994;4:8–22. doi: 10.1111/j.1600-0668.1994.t01-3-00003.x. [DOI] [Google Scholar]
- Singer BC, Delp WW, Apte MG, Price PN. Performance of installed cooking exhaust devices. Indoor Air. 2012;22:224–234. doi: 10.1111/j.1600-0668.2011.00756.x. [DOI] [PubMed] [Google Scholar]
- Spengler JD, Schwab M, McDermott A, Lambert WE, Samet JM. Nitrogen dioxide and respiratory illness in children Part IV: effects of housing and meteorologic factors on indoor nitrogen dioxide concentrations. Res Rep Health Eff Inst. 1996;58:1–29. discussion 31–6. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Percentage of homes at each sampling visit with a decrease in median indoor NO2 following intervention.
Table S2 Median indoor NO2 by location, study arm, and sampling visit.
Table S3 Median ambient NO2 by study arm and sampling visit.
Table S4 Median change in NO2 (ppb) by pilot light.


