Abstract
The amount of lymph node dissection (LD) required during surgical treatment of gastric cancer surgery has been quite controversial. In the 1970s and 1980s, Japanese surgeons developed a doctrine of aggressive preventive gastric cancer surgery that was based on extended (D2) LD volumes. The West has relatively lower incidence rates of gastric cancer, and in Europe and the United States the most common LD volume was D0-1. This eventually caused a scientific conflict between the Eastern and Western schools of surgical thought: Japanese surgeons determinedly used D2 LD in surgical practice, whereas European surgeons insisted on repetitive clinical trials in the European patient population. Today, however, one can observe the results of this complex evolution of views. The D2 LD is regarded as an unambiguous standard of gastric cancer surgical treatment in specialized European centers. Such a consensus of the Eastern and Western surgical schools became possible due to the longstanding scientific and practical search for methods that would help improve the results of gastric cancer surgeries using evidence-based medicine. Today, we can claim that D2 LD could improve the prognosis in European populations of patients with gastric cancer, but only when the surgical quality of LD execution is adequate.
Keywords: Gastric cancer, D2 lymph node dissection, Evidence-based medicine, European patients, Regional lymph nodes
Core tip: The amount of lymph node dissection required during surgical treatment of gastric cancer has been quite controversial. We can now claim that D2 lymph node dissection improves the prognosis in European populations with gastric cancer, but only when the surgical quality of the lymph node dissection execution is adequate.
INTRODUCTION
Radical surgery for malignant tumors traditionally includes mandatory one-piece removal of regional lymph nodes (LNs). This approach was introduced over 100 years ago by an American surgeon, W.S. Halsted, and has been used to determine the extent of surgery in basic sites of neoplasia including tumors in the gastrointestinal tract. Despite its high clinical effectiveness and use as a standard treatment in Asia, extensive D2/D3 lymph node dissection (LD) has not been widely used in gastric cancer (GC) surgery in Europe and the Americas until recently.
Indeed until recently, European clinical recommendations for cancer treatment did not suggest D2 LD as a surgical standard of care[1]. The relevance of this issue is also evident when considering the surgical standard of Western randomized trials on multimodal treatment for GC. The MAGIC trial set the standard for combined treatment of GC in the European Union, and D2 LD was performed in only 42.5% of patients[2]. The US standard multimodal treatment for GC is based on the INT 0116 trial[3] in which an extended LD was performed in only 10% of patients. In a large-scale clinical trial on perioperative chemoradiotherapy effectiveness (the CRITICS trial; ongoing in Europe), the planned extension of LD is more limited than D2[4]. Thus, the issue of standardization in lymphadenectomy extension for GC in Western countries remains relevant.
DEFINITION AND LEVELS OF LYMPHNODAL DISSECTION IN GASTRIC CANCER
Lymphatic efflux from the stomach travels through a complex multidirectional network[5]. Lymph from different sections of the stomach is drained into the para-aortal LN collector through one of four routes: (1) left subdiaphragmatic via the LN in the circulation of the left lower diaphragmatic artery; (2) abdominal via the LN along the left gastric, splenic, and common hepatic arteries and the celiac trunk; (3) upper mesenteric that receives lymph from the subpyloric LNs and runs along the upper mesenteric artery; and (4) retropancreatic, which is associated with LNs of the hepatoduodenal ligament, upper mesenteric vessels and common hepatic artery. Both the left subdiaphragmatic and abdominal routes drain lymph from the upper third of the stomach. The lymphatic efflux from the gastric body drains primarily through the abdominal route, and lymph efflux from the distal stomach drains through abdominal, upper mesenteric and retropancreatic routes[6].
Metastases to regional LNs are diagnosed in 37%-65% of patients with tumors in the gastric corpus, in 44%-80% of patients with tumors in the proximal stomach, and in 50%-59% of patients with tumors in the distal stomach[7,8]. The involvement of regional LNs depends directly on the depth of primary tumor invasion. In intra- and sub-epithelial tumors, regional lymphogenous metastases are diagnosed in 0%-5.5% and 19%-31% of patients, respectively[7,9]. In muscle or subserosal layer invasions, regional LN involvement increases to 30%-62%; in serous membrane tumors, regional LN metastases are found in 74% of patients, and 90%-91% in cases with infiltration of adjacent organs[7].
The first one-piece tissue dissection of regional lymphogenous metastasis during the course of GC surgery was carried out in 1962 by Jinnai et al[10]. Since then, the concept of extended radical LD has become an essential stage in the strategy of GC surgical treatment in Japan. Research in the field of lymph node (LN) topography and extended clinical efficiency formed the basis of the first edition of “General Rules for the Gastric Cancer Study”, which was published in the early 1960s under the auspices of the Japanese Research Society for Gastric Cancer[11]. The first English edition of these guidelines was published in Europe in 1995. Subsequently, research performed by the Japanese Gastric Cancer Association (JGCA) formed the basis for a second English edition based on the Japanese classification of gastric cancer by the JGCA[12] as well as Japanese gastric cancer treatment guidelines[13]. These guidelines describe the following groups of stomach LNs (Table 1, Figure 1).
Table 1.
The lymphatic system of the stomach[12]
| LN groups | LN topography |
| №1 | Right paracardiac LNs |
| №2 | Left paracardiac LNs |
| №3 | LNs along the lesser curvature |
| №4sa | LNs along the short gastric vessels |
| №4sb | LNs along the left gastroepiploic vessels |
| №4d | LNs along the right gastroepiploic vessels |
| №5 | Suprapyloric LNs |
| №6 | Infrapyloric LNs |
| №7 | LNs along the left gastric artery |
| №8а | LNs along the common hepatic artery (anterosuperior group) |
| №9 | LNs at the celiac trunk |
| №10 | LNs at the splenic hilum |
| №11р | LNs along the proximal splenic artery |
| №11d | LNs along the distal splenic artery |
| №12a | LNs in the hepatoduodenal ligament (along the hepatic artery) |
| №12b | LNs in the hepatoduodenal ligament (along the bile duct) |
| №12р | LNs in the hepatoduodenal ligament (behind the portal vein) |
| №13 | Retro-pancreaticoduodenal LNs |
| №14а | LNs along the superior mesenteric artery |
| №14v | LNs along the superior mesenteric vein |
| №15 | LNs along the middle colic vessels |
| №16 | Para-aortic LNs |
| №17 | LNs on the anterior surface of the pancreatic head |
| №18 | LNs along the inferior margin of the pancreas |
| №19 | Infradiaphragmatic LNs |
| №20 | LNs in the esophageal hiatus of the diaphragm |
LNs: Lymph nodes.
Figure 1.
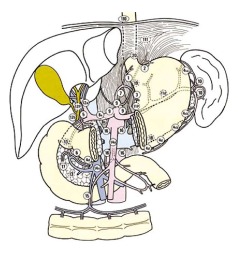
Topography of stomach lymph node groups[12].
According to the classification of gastric cancer by the JGCA (1998)[12], the stomach lymphatic system consists of three LN compartments. Each of these is a temporary barrier that prevents tumor cells from entering the lymphatic system. Grouping stomach lymph collectors into compartments created the basis for determining the gradation of category “N” at staging and a theoretical basis for the extension of LD according to tumor site as reported in the following table (Table 2)[12]. The LN groups 12b, p and above are classified as N3 - in the given classification-this is equivalent to distant metastases.
Table 2.
Lymph node groups (compartments 1-3) by location of tumor
| Location lymph node station | LMU/MUL MLU/UML | LD/L | LM/M/ML | MU/UM | U | E+ |
| No. 1 rt paracardial | 1 | 2 | 1 | 1 | 1 | |
| No. 2 lt paracardial | 1 | M | 3 | 1 | 1 | |
| No. 3 lesser curvature | 1 | 1 | 1 | 1 | 1 | |
| No. 4sa short gastric | 1 | M | 3 | 1 | 1 | |
| No. 4sb lt gastroepiploic | 1 | 3 | 1 | 1 | 1 | |
| No. 4d rt gastroepiploic | 1 | 1 | 1 | 1 | 2 | |
| No. 5 suprapyloric | 1 | 1 | 1 | 1 | 3 | |
| No. 6 infrapyloric | 1 | 1 | 1 | 1 | 3 | |
| No. 7 lt gastric artery | 2 | 2 | 2 | 2 | 2 | |
| No. 8a ant comm hepatic | 2 | 2 | 2 | 2 | 2 | |
| No. 8b post comm hepatic | 3 | 3 | 3 | 3 | 3 | |
| No. 9 celiac artery | 2 | 2 | 2 | 2 | 2 | |
| No. 10 splenic hilum | 2 | M | 3 | 2 | 2 | |
| No. 11p proximal splenic | 2 | 2 | 2 | 2 | 2 | |
| No. 11d distal splenic | 2 | M | 3 | 2 | 2 | |
| No. 12a lt hepatoduodenal | 2 | 2 | 2 | 2 | 3 | |
| No. 12b,p post hepatoduod | 3 | 3 | 3 | 3 | 3 | |
| No. 13 retropancreatic | 3 | 3 | 3 | M | M | |
| No. 14v sup mesenteric v. | 2 | 2 | 3 | 3 | M | |
| No. 14a sup mesenteric a. | M | M | M | M | M | |
| No. 15 middle colic | M | M | M | M | M | |
| No. 16a1 aortic hiatus | M | M | M | M | M | |
| No. 16a2,b1 paraaortic, middle | 3 | 3 | 3 | 3 | 3 | |
| No. 16b2 paraaortic, caudal | M | M | M | M | M | |
| No. 17 ant pancreatic | M | M | M | M | M | |
| No. 18 inf pancreatic | M | M | M | M | M | |
| No. 19 infradiaphragmatic | 3 | M | M | 3 | 3 | 2 |
| No. 20 esophageal hiatus | 3 | M | M | 3 | 3 | 1 |
| No. 110 lower paraesophag | M | M | M | M | M | 3 |
| No. 111 supradiaphragmatic | M | M | M | M | M | 3 |
| No. 112 post mediastinal | M | M | M | M | M | 3 |
M: Lymph nodes regarded as distant metastasis.
Of note, in the last version of tumor-node-metastasis (TNM) classification introduced by the Union for International Cancer Control (UICC)[14], category “N” is determined not by the topography but rather by the number of affected regional LNs. Accordingly, in the last version of JGCA guidelines (2011)[13], the extension of nodal dissection is defined according to the extension of gastric resection as reported in the following figures.
During distal subtotal gastrectomy, the lymph node dissection levels are as follows: (1) D0: LD in a volume less than D1; (2) D1: №1, 3, 4sb, 4d, 5, 6, 7; (3) D1 +: D1 plus №8a, 9; and (4) D2: D1 plus №8a, 9, 11p, 12a (Figure 2).
Figure 2.
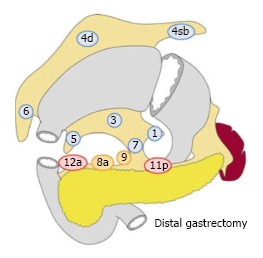
Lymph node dissection levels in distal subtotal gastrectomy[13].
In gastrectomy, the LD levels are as follows: (1) D0: LD in a volume less than D1; (2) D1: №1-7; (3) D1 +: D1 plus №8a, 9, 11p; and (4) D2: D1 plus №8a, 9, 10, 11p, 11d, 12a (Figure 3).
Figure 3.
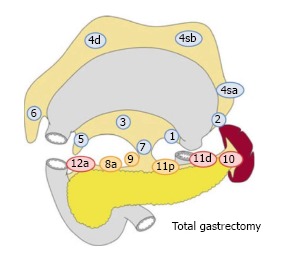
Lymph node dissection levels in gastrectomy[13].
Levels of LD in proximal subtotal gastrectomy: (1) D0: LD in a volume less than D1; (2) D1: №1, 2, 3a, 4sa, 4sb, 7; and (3) D1 +: D1 plus №8a, 9, 11p (Figure 4).
Figure 4.
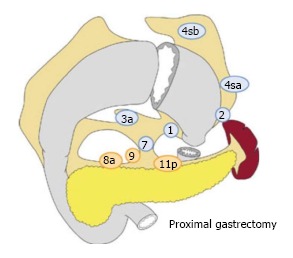
Lymph node dissection levels in proximal subtotal gastrectomy[13].
LD extended beyond these definitions are classified as D2 +. Their effectiveness remains controversial; therefore, they are currently not recommended for routine use in clinical practice[13].
Gastric cancer classification by JGCA (1998) has demonstrated its high efficiency in several clinical studies[5,15,16]. LN staging based on topography laid the grounds for JGCA’s classification. These are considered anatomical in contrast to the rather mechanistic quantitative approach of the UICC classification. This allows for consideration of disease propagation and for more accurate prognosis. In support of this thesis, the correlated survival of patients with lesions of various LN groups has been studied patients with the same number of regional lymphogenous metastases, survival differed depending on the LN collectors in which lesions were located[17]. Thus, localization as well as the quantity of metastatically-affected regional LNs has a probable prognostic value. According to Y. Noguchi[18], in N0, LN lesion groups 1-6 (N1 according JGCA), LN lesion groups 7-12 (N2), and LN groups 13-16 (N3), the 5-year survival rate was 85%, 60%, 25% and 11%, respectively.
A significant advantage of the second JGCA gastric cancer classification in terms of practical application is its direct link with the volume of LD based on the staging principle of lymphogenous metastasis. Of note, the Japanese classification uses the term “regional lymph node”. This is defined not only by the lymph node topography, but also by the site of the primary tumor in the stomach; the UICC classification does not provide this differentiation.
Another obvious advantage of the classification offered by JGCA[12] lies in the possibility of extrapolating data about the regional LN condition into the UICC classification. The reverse conversion is not possible; therefore, it is not possible to conduct a comparative analysis of retrospective studies in a different series.
Western pathologists and surgeons criticize the Japanese GC classification mainly because of its complexity and also because precision mapping is laborious in practice. However, the Eastern and Western GC classifications are finally approaching each other. This tendency can be observed in the latest edition of the TNM UICC classification and the latest editions of the JCGA gastric cancer treatment guidelines[13,14].
DEBATE ON THE EXTENT OF LYMPHNODAL DISSECTION: EASTERN VS WESTERN POSITION
Results of a retrospective analysis of LD D2 were first published in Japan in 1970 by Mine et al[19]. The authors reported a slight increase in the survival rate among patients with pN0 and a probable increase in the 5-year survival rate from 10% to 21% in the group pN+. Similar results were reported in a study by Kodama et al[20], who indicated an increase in the 5-year survival rate from 33% to 58% in the entire group of patients.
In the 1970s and 1980s, Japanese surgeons developed a doctrine of aggressive preventive GC surgery based on the extended (D2) and super-extended (D3) LD volumes[21]. Concurrently, in Europe and the United States, the most common LD volume was D0-1. Due to the relatively lower GC incidence rates in the West, European and American surgeons continued to reframe the ideology and master the techniques of extended interventions in GC cases until the end of the 1990s. This eventually caused a scientific conflict between the Eastern and Western schools of surgical thought. Japanese surgeons used D2 LD in surgical practice, whereas European surgeons insisted on repetitive clinical trials in the European patient population. They reasoned that certain biological differences in GC were present in the “Eastern” type[22].
One of the most significant publications from that time was a study of a European population of patients with GC by Pacelli et al[23]. The authors reported a probable increase in the 5-year survival rate from 30% (D1, LD) to 49% (D2, 3 LD) for patients with stage III GC and from 50% to 65% in the entire group of patients.
Similar results were obtained by a group of German surgeons supervised by Siewert et al[24] during the course of a prospective multicentric trial of nearly 2500 patients. A probable increase in the survival rate was reported in patients with stages II-IIIA GC. However, in patients with pN2 (TNM UICC) or with extensive tumor invasion of the gastric serosa, D2 LD was not associated with increased survival.
Over time, researchers increasingly noted the low credibility of non-randomized studies. The results of the first randomized trials published by Dent et al[25] and Robertson et al[26] featured high rates of postoperative complications and mortality. However, the results did not provide high levels of credibility because of the small numbers of patients enrolled. The first large-scale randomized multicentric study of the efficacy of D2 LD in a population of European patients with GC was carried out in the 1990s.
This study, known as the Dutch trial[27], involved 1078 randomized patients and was organized by the Dutch Gastric Cancer Group. At the same time, the British MRS (Medical Research Society) carried out its own trial[28] with 400 randomized patients. The first results of these studies were preliminarily published in 1997 at the Second International Gastric Cancer Congress (IGCC) in Munich. However, the necessity of compliance with the full volume of D2 LD dramatically increased the frequency of splenectomies (up to 37% in the Dutch study and up to 65% in the British) and resections of the pancreas (30% in the Dutch study and 56% in the British) in all groups. These studies showed a dramatic increase in the number of postoperative complications after D2 LD (from 25% after performing D0-1 in the control group up to 43% in the Dutch trial and from 28% to 46% in the British trial). They also showed an increase in the postoperative mortality rate (from 4% to 10% in the Dutch trial and from 6.5% to 13% in the British trial)[27,28]. In the Eastern Asian series however, the rate of postoperative complications was 17%-21%[29,30]. The postoperative mortality rate after D2 LD in Eastern clinics was also significantly lower than in Europe-less than 2% in the Japanese nationwide registry[31] and less than 1%[30] or even zero[29] in specialized centers.
After a 5-year follow-up of European randomized studies, the expected increase in survival of D2 LD group was not achieved; the 5-year survival in the Dutch trial was 45% in group D1 LD and 47% in group D2 LD. In the British trial, it was 35% in group D1 LD and 33% in group D2 LD[32,33] (Figure 5).
Figure 5.
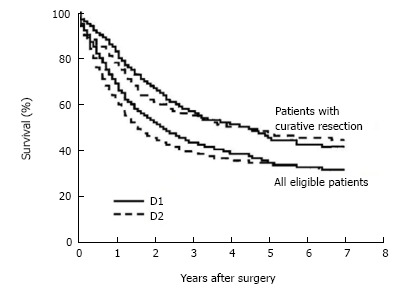
Patient survival in the Dutch trial[32].
Thus, the European oncology society preliminarily concluded that the extended LD volumes used in European GC patients were ineffective. This was based on evidence-based medicine and relied on the results of the two major Western randomized trials. However, a detailed analysis of this study and all potential reasons for the lack of a positive result were shown at the 1999 IGCC in Seoul. The summary of this analysis was later published in the New England Journal of Medicine[34]. Despite a good design and detailed statistical analysis, the study had some serious shortcomings that made the results ambiguous. These included:
The large number of participating surgical centers (about 80 clinics), which resulted in surgeons obtaining an insufficient amount of practical experience in the surgical procedures required for the study. For instance, some surgeons performed fewer than 5 D2 LD surgeries per year. This not only potentially affected the level of postoperative complications and mortality, but also led to a reduction in LN removal in the course of D2 LD and consequently to a reduction in radical surgeries[34].
There was a lack of surgery standardization (there were no clear criteria for splenectomy or spleen-saving dissection of the 10th LN group, instrumental or manual anastomosis, etc.).
Conversely, surgeons participating in the randomized trial in Taiwan performed a minimum of 80 D2 LD surgeries before the study began. The results of that study revealed a possible increase in survival rates when extended volumes of LD were performed[35].
The median number of LNs removed is an important indicator of LD quality. Significant geographic fluctuations of this indicator in the performance of D2 LD have now been established. There are diametrically polar indicators in European randomized trials. In the British study, the median number of removed LNs was 17[28]; in the Dutch study, the number was 30[32]. There were 25-26 LNs removed in the Western retrospective studies[36,37] and 54 LNs removed in Japanese specialized centers[30]. The minimum adequate number of LNs to be removed in gastric cancer surgeries-according to the requirements of TNM UICC (2009)[14]-is 15. This level of LD was provided in 86%[36] to 95%[37] of patients in the Western retrospective studies and in 100% of patients in the Japanese studies[30]. According to Siewert et al[24], the efficiency of LD execution can meet the standards of D2 only when a minimum of 26 LNs are removed.
The average frequency of metastatic lesions in LNs of group №10th (LNs of the splenic hilum) in various tumor sites in the stomach is 8.8%. Metastatic lesions in these LNs are likely to worsen the prognosis[38]. The application of splenectomy on principle including for LN dissection of the 10th group was not effective in patients with GC until recently. A small study conducted in Korea by Yu et al[39] demonstrated a tendency toward increased survival after splenectomy; however, this result was not statistically significant. A meta-analysis conducted in 2009 by Yang et al[40] also confirmed an increase in the 5-year survival rate of patients with GC after splenectomy. According to other authors[38], unless the tumor has invaded the spleen, splenectomy is necessary only in case of LN lesions in group №4sa. Therefore, despite the fact that LN dissection of the 10th group is regulated by the JGCA guidelines (2011)[13], the role of splenectomy as a standard stage of D2 LD remains controversial. The answer to this question will likely be clarified soon after the publication of the results of a large randomized trial investigating the efficacy of splenectomy in Japanese patients with cancer of the upper third of the stomach (JCOG 0110 that began in Japan in 2002)[41].
Despite the previous pessimistic results, Hartgrink et al[42] conducted a second analysis of the “Dutch material” in 2001. They found a significant increase in survival in group D2 LD, especially in patients with metastases in LNs of the first stage of metastasis (N1 by JGCA). After 15 years of observation of patients during the Dutch trial, no significant difference in survival between groups under observation has not been noted. However, when the most controversial group of patients with splenectomies and resection of the pancreatic gland was excluded from the analysis, the 15-year survival rate increased dramatically from 22% in D1 LD to 35% in D2 LD (P = 0.006)[43] (Figure 6).
Figure 6.
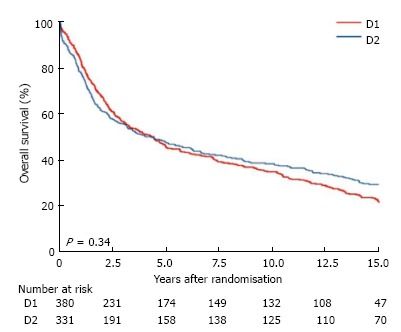
Survival of patients in the Dutch trial after a 15-year observation[43].
In 2013, the results of meta-analysis obtained by 12 randomized controlled major European trials on LD D2 effectiveness were published. These clearly proved the thesis concerning an increased risk of postoperative complications with D2 LD and the possible increase in survival only in the group that did not have splenectomy and resection of the pancreatic gland[44]. Therefore, in the latest European oncology guidelines, D2 LD is the standard surgical procedure but only in highly specialized centers with extensive experience in such surgeries as well as postoperative care[45].
According to the Japanese guidelines on the gastric cancer treatment issued by JGCA (2011)[13], the algorithm of surgical treatment in patients with GC is as follows (Figure 7).
Figure 7.
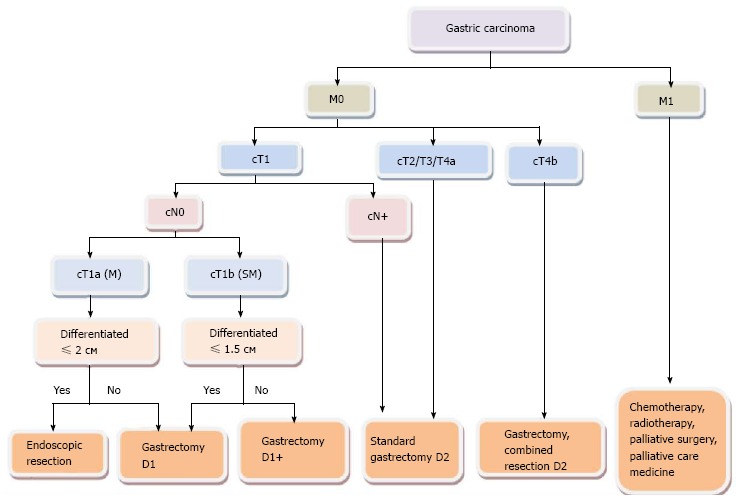
Algorithm of surgical treatment of patients with gastric cancer according to the guidelines provided by Japanese Gastric Cancer Association (2011)[13].
The amount of LD required during surgical treatment of gastric cancer surgery has been quite controversial. Today, however, in light of evidence-based medicine, one can observe the results of this complex evolution of views: D2 LD is considered an unambiguous standard of GC surgical treatment in specialized centers according to national recommendations in Germany[46], the United Kingdom[47] and Italy[48] as well as mutual recommendations of the European Society of Medical Oncologists, Surgical Oncologists and Radiation Therapists (ESMO-ESSO-ESTRO)[45]. Such a consensus of the Eastern and Western surgical schools became possible due to the longstanding scientific and practical search for methods that would help improve the results of GC surgeries using evidence-based medicine[49]. In Western surgical terminology, D2 LD is now called a standard volume of intervention, whereas D2 + LD is an extended operation.
This debate into the effectiveness of extended (D2 + LD) interventions in GC cases remains open. A well-known clinical study conducted by Sasako et al[34] did not demonstrate an increase in survival after D2 + para-aortic LD for patients with resectable GC. However, many recent studies have demonstrated the possibility of increased survival after the application of extended LD in a selected group of patients with a high risk of metastasis in LNs of the N°16 station[50,51].
Furthermore, the effectiveness of laparoscopic D2 LD in GC cases remains undetermined. Today, clinical research is underway in the KLASS-2 trial, which aims to determine the effectiveness of such interventions. The impact of interventions with D1 +, D2 and D2 + LD on the risk of intraperitoneal progression of GC after surgery[6] remains unknown.
CONCLUSION
The data show that D2 LD can improve the prognosis in European GC patients, but only when the surgical quality of LD execution is adequate. As part of the 10th IGCC in 2013 in Verona, Italy, the former president of the European Society of Surgical Oncology, Professor C. van de Velde, noted in his expert lecture that “the only way to improve the efficiency of surgical treatment of gastric cancer in Europe is to place patients in specialized surgical centers, provide training so that individual surgeons could specialize on the issue of LD D2 and an objective and permanent audit on quality of lymphadenectomy in each surgical center”.
Footnotes
Conflict-of-interest statement: No conflict of interest.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: January 18, 2016
First decision: February 22, 2016
Article in press: April 18, 2016
P- Reviewer: Gu GL, Inokuchi M, Park WS S- Editor: Gong ZM L- Editor: A E- Editor: Lu YJ
References
- 1.Okines A, Verheij M, Allum W, Cunningham D, Cervantes A; ESMO Guidelines Working Group. Gastric cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21 Suppl 5:v50–v54. doi: 10.1093/annonc/mdq164. [DOI] [PubMed] [Google Scholar]
- 2.Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, Scarffe JH, Lofts FJ, Falk SJ, Iveson TJ, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20. doi: 10.1056/NEJMoa055531. [DOI] [PubMed] [Google Scholar]
- 3.Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC, Stemmermann GN, Haller DG, Ajani JA, Gunderson LL, Jessup JM, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345:725–730. doi: 10.1056/NEJMoa010187. [DOI] [PubMed] [Google Scholar]
- 4.Dutch Colorectal Cancer Group. Randomized phase III trial of adjuvant chemotherapy or chemoradiotherapy in resectable gastric cancer (CRITICS). In: ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US) Available from: https://clinicaltrials.gov/ct2/show/NCT00407186 NLM Identifier: NCT00407186.
- 5.Maruyama K, Gunvén P, Okabayashi K, Sasako M, Kinoshita T. Lymph node metastases of gastric cancer. General pattern in 1931 patients. Ann Surg. 1989;210:596–602. doi: 10.1097/00000658-198911000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Manzoni G, Roviello F, Siquini W. Surgery in the multimodal management of gastric cancer. Milan: Springer-Verlag Italia; 2012. p. 266. [Google Scholar]
- 7.Di Leo A, Marrelli D, Roviello F, Bernini M, Minicozzi A, Giacopuzzi S, Pedrazzani C, Baiocchi LG, de Manzoni G. Lymph node involvement in gastric cancer for different tumor sites and T stage: Italian Research Group for Gastric Cancer (IRGGC) experience. J Gastrointest Surg. 2007;11:1146–1153. doi: 10.1007/s11605-006-0062-2. [DOI] [PubMed] [Google Scholar]
- 8.Shen KH, Wu CW, Lo SS, Hsieh MC, Hsia CY, Chiang SC, Lui WY. Factors correlated with number of metastatic lymph nodes in gastric cancer. Am J Gastroenterol. 1999;94:104–108. doi: 10.1111/j.1572-0241.1999.00779.x. [DOI] [PubMed] [Google Scholar]
- 9.Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, Kato Y. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–225. doi: 10.1007/pl00011720. [DOI] [PubMed] [Google Scholar]
- 10.Jinnai D, Tanaka S. Technique of extended radical operation for gastric cancer. Geka Chiryo. 1962;7:316–324. [Google Scholar]
- 11.Japanese Research Society for Gastric Cancer. The general rules for gastric cancer study. Jpn J Surg. 1963;16:121–123. [Google Scholar]
- 12.Japanese Gastric Cancer Association. Japanese Classification of Gastric Carcinoma - 2nd English Edition. Gastric Cancer. 1998;1:10–24. doi: 10.1007/s101209800016. [DOI] [PubMed] [Google Scholar]
- 13.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3) Gastric Cancer. 2011;14:113–123. doi: 10.1007/s10120-011-0042-4. [DOI] [PubMed] [Google Scholar]
- 14.Sobin LH, Gospodarowicz MK, Wittekind Ch. TNM classification of malignant tumors. 7th ed. UK: Blackwell Publishing; 2010. p. 310. [Google Scholar]
- 15.de Manzoni G, Verlato G, di Leo A, Guglielmi A, Laterza E, Ricci F, Cordiano C. Perigastric lymph node metastases in gastric cancer: comparison of different staging systems. Gastric Cancer. 1999;2:201–205. doi: 10.1007/s101200050063. [DOI] [PubMed] [Google Scholar]
- 16.Maruyama K, Sasako M, Kinoshita T, Sano T, Katai H. Surgical treatment for gastric cancer: the Japanese approach. Semin Oncol. 1996;23:360–368. [PubMed] [Google Scholar]
- 17.Isozaki H, Okajima K, Kawashima Y, Yamada S, Nakata E, Nishimura J, Ichinona T. Prognostic value of the number of metastatic lymph nodes in gastric cancer with radical surgery. J Surg Oncol. 1993;53:247–251. doi: 10.1002/jso.2930530412. [DOI] [PubMed] [Google Scholar]
- 18.Noguchi Y, Imada T, Matsumoto A, Coit DG, Brennan MF. Radical surgery for gastric cancer. A review of the Japanese experience. Cancer. 1989;64:2053–2062. doi: 10.1002/1097-0142(19891115)64:10<2053::aid-cncr2820641014>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 19.Mine M, Majima S, Harada M, Etani S. End results of gastrectomy for gastric cancer: effect of extensive lymph node dissection. Surgery. 1970;68:753–758. [PubMed] [Google Scholar]
- 20.Kodama Y, Sugimachi K, Soejima K, Matsusaka T, Inokuchi K. Evaluation of extensive lymph node dissection for carcinoma of the stomach. World J Surg. 1981;5:241–248. doi: 10.1007/BF01658301. [DOI] [PubMed] [Google Scholar]
- 21.Maeta M, Yamashiro H, Saito H, Katano K, Kondo A, Tsujitani S, Ikeguchi M, Kaibara N. A prospective pilot study of extended (D3) and superextended para-aortic lymphadenectomy (D4) in patients with T3 or T4 gastric cancer managed by total gastrectomy. Surgery. 1999;125:325–331. [PubMed] [Google Scholar]
- 22.Jatzko G, Pertl A, Jagoditsch M. Chirurgische therapie und ergebnisse beim magenfrühkarzinom. Chir Gastroenterol. 1999;15:223–226. [Google Scholar]
- 23.Pacelli F, Doglietto GB, Bellantone R, Alfieri S, Sgadari A, Crucitti F. Extensive versus limited lymph node dissection for gastric cancer: a comparative study of 320 patients. Br J Surg. 1993;80:1153–1156. doi: 10.1002/bjs.1800800930. [DOI] [PubMed] [Google Scholar]
- 24.Siewert JR, Böttcher K, Roder JD, Busch R, Hermanek P, Meyer HJ. Prognostic relevance of systematic lymph node dissection in gastric carcinoma. German Gastric Carcinoma Study Group. Br J Surg. 1993;80:1015–1018. doi: 10.1002/bjs.1800800829. [DOI] [PubMed] [Google Scholar]
- 25.Dent DM, Madden MV, Price SK. Randomized comparison of R1 and R2 gastrectomy for gastric carcinoma. Br J Surg. 1988;75:110–112. doi: 10.1002/bjs.1800750206. [DOI] [PubMed] [Google Scholar]
- 26.Robertson CS, Chung SC, Woods SD, Griffin SM, Raimes SA, Lau JT, Li AK. A prospective randomized trial comparing R1 subtotal gastrectomy with R3 total gastrectomy for antral cancer. Ann Surg. 1994;220:176–182. doi: 10.1097/00000658-199408000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, van Elk P, Obertop H, Gouma DJ, Taat CW. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet. 1995;345:745–748. doi: 10.1016/s0140-6736(95)90637-1. [DOI] [PubMed] [Google Scholar]
- 28.Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, Cook P. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. The Surgical Cooperative Group. Lancet. 1996;347:995–999. doi: 10.1016/s0140-6736(96)90144-0. [DOI] [PubMed] [Google Scholar]
- 29.Wu CW, Hsiung CA, Lo SS, Hsieh MC, Shia LT, Whang-Peng J. Randomized clinical trial of morbidity after D1 and D3 surgery for gastric cancer. Br J Surg. 2004;91:283–287. doi: 10.1002/bjs.4433. [DOI] [PubMed] [Google Scholar]
- 30.Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, Tsujinaka T, Kinoshita T, Arai K, Yamamura Y, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy--Japan Clinical Oncology Group study 9501. J Clin Oncol. 2004;22:2767–2773. doi: 10.1200/JCO.2004.10.184. [DOI] [PubMed] [Google Scholar]
- 31.Fujii M, Sasaki J, Nakajima T. State of the art in the treatment of gastric cancer: from the 71st Japanese Gastric Cancer Congress. Gastric Cancer. 1999;2:151–157. doi: 10.1007/s101200050039. [DOI] [PubMed] [Google Scholar]
- 32.Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ, Welvaart K, Songun I, Meyer S, Plukker JT, Van Elk P, Obertop H, et al. Extended lymph-node dissection for gastric cancer. N Engl J Med. 1999;340:908–914. doi: 10.1056/NEJM199903253401202. [DOI] [PubMed] [Google Scholar]
- 33.Cuschieri A, Weeden S, Fielding J, Bancewicz J, Craven J, Joypaul V, Sydes M, Fayers P. Patient survival after D1 and D2 resections for gastric cancer: long-term results of the MRC randomized surgical trial. Surgical Co-operative Group. Br J Cancer. 1999;79:1522–1530. doi: 10.1038/sj.bjc.6690243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sasako M, Sano T, Yamamoto S, Kurokawa Y, Nashimoto A, Kurita A, Hiratsuka M, Tsujinaka T, Kinoshita T, Arai K, et al. D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med. 2008;359:453–462. doi: 10.1056/NEJMoa0707035. [DOI] [PubMed] [Google Scholar]
- 35.Wu CW, Hsiung CA, Lo SS, Hsieh MC, Chen JH, Li AF, Lui WY, Whang-Peng J. Nodal dissection for patients with gastric cancer: a randomised controlled trial. Lancet Oncol. 2006;7:309–315. doi: 10.1016/S1470-2045(06)70623-4. [DOI] [PubMed] [Google Scholar]
- 36.Smith BR, Stabile BE. Aggressive D2 lymphadenectomy is required for accurate pathologic staging of gastric adenocarcinoma. Am Surg. 2006;72:849–852. [PubMed] [Google Scholar]
- 37.de Manzoni G, Verlato G, Guglielmi A, Laterza E, Genna M, Cordiano C. Prognostic significance of lymph node dissection in gastric cancer. Br J Surg. 1996;83:1604–1607. doi: 10.1002/bjs.1800831137. [DOI] [PubMed] [Google Scholar]
- 38.Chen XL, Yang K, Zhang WH, Chen XZ, Zhang B, Chen ZX, Chen JP, Zhou ZG, Hu JK. Metastasis, risk factors and prognostic significance of splenic hilar lymph nodes in gastric adenocarcinoma. PLoS ONE. 2014;9:e99650. doi: 10.1371/journal.pone.0099650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yu W, Choi GS, Chung HY. Randomized clinical trial of splenectomy versus splenic preservation in patients with proximal gastric cancer. Br J Surg. 2006;93:559–563. doi: 10.1002/bjs.5353. [DOI] [PubMed] [Google Scholar]
- 40.Yang K, Chen XZ, Hu JK, Zhang B, Chen ZX, Chen JP. Effectiveness and safety of splenectomy for gastric carcinoma: a meta-analysis. World J Gastroenterol. 2009;15:5352–5359. doi: 10.3748/wjg.15.5352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sano T, Yamamoto S, Sasako M; Japan Clinical Oncology Group Study LCOG 0110-MF. Randomized controlled trial to evaluate splenectomy in total gastrectomy for proximal gastric carcinoma: Japan clinical oncology group study JCOG 0110-MF. Jpn J Clin Oncol. 2002;32:363–364. doi: 10.1093/jjco/hyf085. [DOI] [PubMed] [Google Scholar]
- 42.Hartgrink HH, van de Velde CJH; On behalf of the Dutch Gastric Cancer Group. Update of the Dutch D1 vs D2 gastric cancer trial. The 4th International Gastric Cancer Congress;; April 29-May 2; Knoxville, TN. 2001. [Google Scholar]
- 43.Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ. Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol. 2010;11:439–449. doi: 10.1016/S1470-2045(10)70070-X. [DOI] [PubMed] [Google Scholar]
- 44.Jiang L, Yang KH, Guan QL, Zhao P, Chen Y, Tian JH. Survival and recurrence free benefits with different lymphadenectomy for resectable gastric cancer: a meta-analysis. J Surg Oncol. 2013;107:807–814. doi: 10.1002/jso.23325. [DOI] [PubMed] [Google Scholar]
- 45.Waddell T, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D. Gastric cancer: ESMO-ESSO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24 Suppl 6:vi57–vi63. doi: 10.1093/annonc/mdt344. [DOI] [PubMed] [Google Scholar]
- 46.Meyer HJ, Hölscher AH, Lordick F, Messmann H, Mönig S, Schumacher C, Stahl M, Wilke H, Möhler M. [Current S3 guidelines on surgical treatment of gastric carcinoma] Chirurg. 2012;83:31–37. doi: 10.1007/s00104-011-2149-x. [DOI] [PubMed] [Google Scholar]
- 47.Allum WH, Blazeby JM, Griffin SM, Cunningham D, Jankowski JA, Wong R; Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland, the British Society of Gastroenterology and the British Association of Surgical Oncology. Guidelines for the management of oesophageal and gastric cancer. Gut. 2011;60:1449–1472. doi: 10.1136/gut.2010.228254. [DOI] [PubMed] [Google Scholar]
- 48.De Manzoni G, Baiocchi GL, Framarini M, De Giuli M, D’Ugo D, Marchet A, Nitti D, Marrelli D, Morgagni P, Rinnovati A, et al. The SIC-GIRCG 2013 Consensus Conference on Gastric Cancer. Updates Surg. 2014;66:1–6. doi: 10.1007/s13304-014-0248-1. [DOI] [PubMed] [Google Scholar]
- 49.Verlato G, Giacopuzzi S, Bencivenga M, Morgagni P, De Manzoni G. Problems faced by evidence-based medicine in evaluating lymphadenectomy for gastric cancer. World J Gastroenterol. 2014;20:12883–12891. doi: 10.3748/wjg.v20.i36.12883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roviello F, Pedrazzani C, Marrelli D, Di Leo A, Caruso S, Giacopuzzi S, Corso G, de Manzoni G. Super-extended (D3) lymphadenectomy in advanced gastric cancer. Eur J Surg Oncol. 2010;36:439–446. doi: 10.1016/j.ejso.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 51.de Manzoni G, Di Leo A, Roviello F, Marrelli D, Giacopuzzi S, Minicozzi AM, Verlato G. Tumor site and perigastric nodal status are the most important predictors of para-aortic nodal involvement in advanced gastric cancer. Ann Surg Oncol. 2011;18:2273–2280. doi: 10.1245/s10434-010-1547-5. [DOI] [PubMed] [Google Scholar]


