Abstract
Examination of the ocular fundus is a critical aspect of the neurological examination. For example, in patients with headache the ocular fundus examination is needed to uncover “red flags” suggestive of secondary etiologies. However, ocular fundus examination is infrequently and poorly performed in clinical practice. Non-mydriatic ocular fundus photography provides an alternative to direct ophthalmoscopy that has been studied as part of the Fundus photography vs. Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) study. Herein, we review the results of the FOTO-ED study with a particular focus on the study's implications for the acute care of patients presenting with headache and focal neurologic deficits. In headache patients, we not only observed optic disc edema and optic disc pallor as would be expected, but also a large number of abnormalities associated with hypertension. Based upon subjects with focal neurological deficits, the FOTO-ED study suggests that the ocular fundus examination may assist with the triage of patients presenting with suspected transient ischemic attack. Continued advances in the ease and portability of non-mydriatic fundus photography will hopefully help to restore ocular fundus examination as a routinely performed component of all neurological examinations.
Keywords: ocular fundus, headache, cerebrovascular disease, direct ophthalmoscopy, emergency
Introduction
The retinal microvasculature shows important changes that are associated with stroke and dementia, and the continued study of retinal microvascular changes may provide deeper insights into the pathophysiology of stroke, dementia, and other neurological conditions, as Cheung et al. have discussed in this issue.[1] Their article highlights the value of fundus photography in the observation and study of retinal microvascular changes and discusses the need to translate the findings from large epidemiological studies to the frontlines of clinical practice. Indeed, the ocular fundus examination is a critical part of the diagnostic toolkit for neurologists because it offers the only window for direct noninvasive visualization of a part of the brain (the optic nerve and retina) and its accompanying microvasculature. In many cases, the ocular fundus may hold the only clue that a patient has a more serious underlying diagnosis (e.g., papilledema is a headache patient). However, ophthalmoscopy, instead of fundus photography, is the primary means used for visualization of the ocular fundus in current clinical practice, and it is underutilized and poorly performed. For example, in two hospitals in Birmingham, United Kingdom, only 25 of 56 inpatients (45%; 95%CI: 32-58%) referred to neurology could recall being examined with an ophthalmoscope whereas 54 (96%; 95%CI: 87-99%) recalled being examined with a stethoscope.[2]
In this article, we review the findings of the Fundus photography vs. Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) study,[3-5] which compared direct ophthalmoscopy to fundus photography in an emergency department (ED) setting, with a particular focus on the study's implications for acute care neurology.[6,7]
Direct ophthalmoscopy vs. non-mydriatic ocular fundus photography
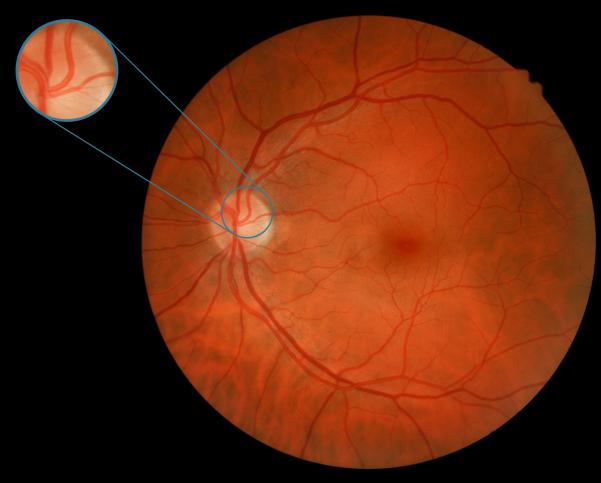
Direct ophthalmoscopes, while portable and commonly mounted on the walls of examination rooms in outpatient clinics and EDs, are very difficult to use and provide an extremely limited view of the ocular fundus (~5°) (Figure). The limitations of the direct ophthalmoscope have an impact not only on non-ophthalmologists, but also on eye care specialists themselves. For example, in dilated patients examined by ophthalmologists with a direct ophthalmoscope the sensitivity for common conditions, such as diabetic and hypertensive retinopathy, falls by about a half.[8] When used without dilation, as is typical in many outpatient and emergency department settings, the field of view and sensitivity fall even further.[9]
Figure.
Normal non-mydriatic ocular fundus photograph with inset showing typical field of view of a direct ophthalmoscope.
Non-mydriatic ocular fundus photography offers a promising alterative to direct ophthalmoscopy by allowing wide-field (45°) photographs of the ocular fundus to be taken without pharmacologic dilation of the pupils with relative ease, even after only limited training (Figure).[3] In contrast to direct ophthalmoscopy, non-mydriatic fundus photography increases sensitivity (as well as specificity and inter-examination agreement) for diabetic retinopathy even among ophthalmologists using indirect ophthalmoscopy.[10,11]
Non-mydriatic ocular fundus photography in the emergency department
Failure to correctly examine the ocular fundus can have life-threatening consequences, particularly in the ED, and the FOTO-ED study hypothesized that non-mydriatic ocular fundus photography would be feasible and improve diagnosis in the ED. The main goal of the FOTO-ED study was to compare non-mydriatic fundus photography to direct ophthalmoscopy.[3-5]
The first phase of the FOTO-ED evaluated the routine clinical use of direct ophthalmoscopy by ED physicians, whereas the second phase evaluated the routine use of non-mydriatic ocular fundus photography as interpreted by the ED physicians. In both phases, all patients had non-mydriatic ocular fundus photographs obtained. The FOTO-ED study included adult patients presenting to a university ED with headaches, focal neurologic deficits, diastolic blood pressure (DBP) ≥120 mmHg, and/or acute visual changes. Photographs of the posterior pole of the ocular fundus (optic disc, macula, and major retinal vessels) were obtained from both eyes of enrolled patients at presentation by trained nurse practitioners or a medical student using a commercially available, Food and Drug Administration–approved, non-mydriatic ocular fundus camera (Kowa nonmyd-D series cameras; Kowa Optimed, Inc., Torrance, CA). Throughout the FOTO-ED study, relevant ocular fundus abnormalities were defined as optic disc edema, isolated intraocular hemorrhage, grade III/IV hypertensive retinopathy retinal vascular occlusion, and optic disc pallor.
FOTO-ED: Phase I – Only Direct Ophthalmoscopy Available to Emergency Physicians
In the first phase of the FOTO-ED study,[3,4] 350 patients were enrolled. The median age of patients was 44.5 years (interquartile range [IQR] 31–59 years), and 220 (63%) were women. Two hundred twenty-eight (65%) had headache, 100 (29%) had focal neurologic symptoms, 92 (26%) had acute visual changes, and 21 (6%) had DBP ≥120 mmHg (note that patients were allowed to have more than one presenting complaint). The performance of ED physicians and their findings on direct ophthalmoscopy were prospectively recorded, with the physicians unaware of the photography results.
Forty-four of the 350 patients had relevant ocular findings (13%; 95% CI: 9–17%) identified on non-mydriatic fundus photographs by the neuro-ophthalmologist reviewing the images. These included 13 cases of optic nerve edema, 13 cases of intraocular hemorrhages, 10 cases of hypertensive retinopathy (grade III or IV), 4 cases of arterial vascular occlusion, and 4 cases of optic nerve pallor. The ED physicians only examined 48/350 (14%) of the enrolled patients and personally identified none of the relevant findings. Eleven of the 44 relevant abnormalities were known before the patients’ presentation to the ED. Of the remaining 33 findings, 6 were found during ophthalmology consultations obtained by the ED. However, the remaining 27 patients’ abnormalities were not identified, which means that 82% (95% CI: 65–93%) of the findings unknown at the time of ED presentation were missed by routine ED care.
For each photography session, the nurse practitioner rated the ease and speed and patients rated the ease, speed, and comfort of non-mydriatic ocular funds photography on a 10-point Likert scale (10 best). Mean scores for each scale were 8.7 or better suggesting the technique was well liked by both staff and patients. The quality of the photographs was of some diagnostic value for 97% of enrolled patients. Median photography time was 1.9 minutes (IQR: 1.3–2.9), a very tiny sliver of the many hours these patients spent in the ED on average.
The results of the first phase of the FOTO-ED study confirmed that direct ophthalmoscopy was infrequently and poorly performed in the ED and showed that non-mydriatic fundus photography was a feasible alternative to direct ophthalmoscopy.
FOTO-ED: Phase II – Fundus Photography Provided to Emergency Physicians
Three hundred fifty-four patients were enrolled in phase II of the FOTO-ED study.[5] The second cohort of patients was similar to that enrolled in the first phase in terms of age, sex, and complaint distribution: median age 45.9 years (IQR: 33–57), 251 (71%) were women, 206 patients (58%) had headache, 123 (35%) had focal neurologic symptoms, 56 (16%) had acute visual changes, and 21 (6%) had DBP ≥120 mm Hg (again note that patients were allowed to have more than 1 presenting complaint). Thirty-five patients (10%; 95% CI: 7%–13%) had relevant findings identified by neuro-ophthalmologist review of the photographs, including 6 patients with disc edema, 6 with grade III/IV hypertensive retinopathy, 7 with isolated intraocular hemorrhages, 15 with optic disc pallor, and 1 with a retinal vascular occlusion.
Compared to the first phase where the ED physicians only examined 14% of the patients by direct ophthalmoscopy, the ED physicians in the second phase reviewed the photographs of 239/354 patients (68%) and reported that the photographs were helpful in their evaluation of 125 patients (35%; 95%CI: 30%–41%). Whereas they had not personally identified any of the relevant findings in the first phase, the ED physicians identified 16 of the 35 relevant findings (46%) during their review of the fundus photographs in the second phase (absolute difference: 46%; 95% CI: 29% to 62%; p<0.001). These results were particularly remarkable given that the ED physicians had not received any additional training. The results also emphasized that ocular fundus photography often assisted with ED care even when the photographs were normal (e.g., the absence of papilledema in a patient with possible cerebrospinal fluid shunt malfunction).
Implications of the FOTO-ED study for neurological emergencies
Two subgroups of patients enrolled in the FOTO-ED study offer notable insights into the clinical care of two important neurological emergencies: headache and cerebrovascular disease.
Headache
Headache is the fourth most common chief complaint overall in the ED and the most common neurological complaint.[12] We evaluated the ocular fundus findings in 497 patients presenting to the ED with headache (inclusive of the 434 patients with headache in the FOTO-ED studies).[6] A remarkable number of these patients presenting with headache, 42 (8.5%; 95%CI: 6%–11%) had relevant abnormalities of their ocular fundus: 12 had disc edema, 9 had optic nerve pallor, 6 had grade III/IV hypertensive retinopathy, and 15 had isolated retinal hemorrhages. Thirty (71%) of these abnormalities were among patients with an isolated complaint of headache, and among the 34 patients with abnormal ocular fundi who had brain imaging, 14 (41%) had normal imaging studies. These findings emphasize that examination of the ocular fundus remains relevant regardless of whether there are other “red flags” in the patients’ presentation and even in in the current era of neuroimaging.
Several patient features were independently associated with an increased likelihood of abnormalities: body mass index ≥35 kg/m2 (odds ratio [OR]: 2.3, p=0.02), younger age (OR: 0.7 per 10 year increase, p=0.02), and higher mean arterial blood pressure (OR: 1.3 per 10 mmHg increase, p=0.003). Furthermore, each of these risk factors were associated with one or more of the specific ocular fundus findings: younger age (OR 3.2 per 10 year age decrease, p=0.002) and BMI ≥35 kg/m2 (OR 1.3, p=0.045) with optic disc edema; higher mean arterial pressure (OR 1.5 per 10 mmHg increase, p=0.0002) with intraocular hemorrhage or grade III/IV hypertensive retinopathy; and BMI ≥35 kg/m2 (OR 1.5, p=0.03) with optic disc pallor.
The finding of more fundus abnormalities in younger headache patients suggests that the presence of ocular fundus abnormalities are important in identifying a key subset of younger patients with secondary headaches since secondary headaches are generally more common in older individuals. A finding of optic disc edema or optic disc pallor in a patient with headache is most concerning for disorders of intracranial pressure or compression of the anterior visual pathways, and either should prompt an urgent evaluation for the underlying etiology in a patient without a known cause.
However, remarkably, the largest group of ocular fundus abnormalities detected in patients with headache was isolated retinal hemorrhages (36%), which based upon other evidence are most likely attributable to systemic hypertension.[13,14] When these hemorrhages are combined with the 14% of patients with grade III/IV hypertensive retinopathy, it appears that about half of the relevant ocular fundus abnormalities occurring in headache patients presenting to the ED are attributable to elevated blood pressure. This suggestion initially appears to be in conflict with large, well-conducted, population-based studies and the consensus of the International Headache Society that no association exists between mild to moderate hypertension and headache.[15,16] However, headache is a common presenting symptom of hypertensive urgency and other studies have associated more severe hypertension with headache suggesting that this is not a coincidence in the ED setting.[17] Neurologists who evaluate headache patients should be mindful of the potential that hypertension may be a relevant factor, particularly in the ED or other acute setting, since hypertension is treatable and may not only result in a improvement for the patients’ presenting problem but address an important cause of morbidity and mortality.
Cerebrovascular disease
Another area where non-mydriatic ocular fundus photography may be valuable for neurological care in the ED is to assist with the risk stratification of patients presenting with suspected transient ischemic attack (TIA) or stroke. As discussed by Cheung et al. in this issue, it is known that retinal microvascular abnormalities are strongly associated with the long-term risk of stroke, but the value of ocular fundus examination remains less clear in the prediction of short-term events (e.g., stroke within the first few weeks or months after a TIA presentation).[18] However, ocular fundus abnormalities may represent underlying cerebrovascular injury in patients presenting with neurological symptoms. If so, acute microvascular fundus abnormalities would have a role analogous to that of diffusion weighted magnetic resonance imaging (DWI) abnormalities in determining the presence of acute cerebral ischemia.[19]
In the FOTO-ED study, 257 patients had the presenting complaint of focal neurologic deficits,[7] of whom 81 (32%) had cerebrovascular disease (CVD) and 144 (56%; 95%CI: 50-62%) had retinal microvascular abnormalities. Controlling for the commonly used ABCD2 score and diffusion weighted imaging (DWI) abnormalities, a certain severity of focal and general retinal arteriolar narrowing increased the odds of clinically diagnosed CVD vs. an alternative cause of the focal neurologic symptom by 5.5 and 2.6 times, respectively.
Notably, when examining the patients with TIA vs. non-CVD diagnoses based on masked neurologist review (i.e., excluding the patients with stroke), the presence of retinal microvascular findings significantly improved the discrimination of TIA vs. non-CVD after controlling for the ABCD2 score. If these findings bear out in larger studies, fundus photography could provide valuable assistance in the difficult task of separating TIAs from their mimics in the acute setting. Indeed, based on these early results, we have initiated a federally-funded, multi-hospital prospective cohort study designed to further evaluate these findings and to determine whether ocular fundus abnormalities are valuable for acute risk assessment in patients presenting with suspected TIA and minor stroke.
Conclusions
There are significant challenges to the adequate, consistent examination of the ocular fundus with direct ophthalmoscopy that non-mydriatic ocular fundus photography helps to overcome. However, one particular concern with fundus photography is the price of the camera (about $20,000 to $25,000) compared to a direct ophthalmoscope ($100-$500). However, the high risk of poor patient outcomes with associated medico-legal actions,[2,20] the ease with which digital images can be shared with experts via telemedicine when diagnostic uncertainty exists,[21] and the difficulty of improving direct ophthalmoscopy education (another topic addressed in this issue[22]) to a level where ophthalmoscopy would be sensitive enough in frontline clinical care[23,24] suggest the benefits already outweigh the monetary costs, particularly in settings, such as an ED or a large outpatient clinic, where the camera can be shared among multiple providers. Furthermore, more portable and less expensive devices are already in development, and as adoption increases, it is likely that prices will continue to go down.
These increasingly portable devices will also allow us to evaluate patients who are too ill or too young to sit at the camera, and many of these devices can also capture video for the assessment of dynamic phenomena (e.g., spontaneous venous pulsations). Ongoing scientific and technological progress in imaging science and engineering will ultimately lead us to an ideal “digital ophthalmoscope” that will hopefully be in the little black bag of every neurologist.
Acknowledgements
This research was supported in part by an unrestricted departmental grant (Department of Ophthalmology) from Research to Prevent Blindness, Inc., New York, and by NIH/NEI core grant P30-EY006360 (Department of Ophthalmology). Dr. Bruce receives research support from the NIH/NEI (K23-EY019341) and NIH/NINDS (R01-NS089694).
Footnotes
The authors have no relevant conflicts of interest.
References
- 1.Cheung CY, Chen C, Wong TY. Ocular fundus photography as a tool to study stroke and dementia. Semin Neurol. doi: 10.1055/s-0035-1563570. In press. [DOI] [PubMed] [Google Scholar]
- 2.Nicholl DJ, Yap CP, Cahill V, et al. The TOS study: can we use our patients to help improve clinical assessment? J R Coll Physicians Edinb. 2012;42:306–310. doi: 10.4997/JRCPE.2012.405. [DOI] [PubMed] [Google Scholar]
- 3.Bruce BB, Lamirel C, Biousse V, et al. Feasibility of nonmydriatic ocular fundus photography in the emergency department: Phase I of the FOTO-ED study. Acad Emerg Med. 2011;18:928–933. doi: 10.1111/j.1553-2712.2011.01147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bruce BB, Lamirel C, Wright DW, et al. Nonmydriatic ocular fundus photography in the emergency department. N Engl J Med. 2011;364:387–389. doi: 10.1056/NEJMc1009733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bruce BB, Thulasi P, Fraser CL, et al. Diagnostic accuracy and use of nonmydriatic ocular fundus photography by emergency physicians: phase II of the FOTO-ED study. Ann Emerg Med. 2013;62:28–33. e21. doi: 10.1016/j.annemergmed.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thulasi P, Fraser CL, Biousse V, et al. Nonmydriatic ocular fundus photography among headache patients in an emergency department. Neurology. 2013;80:432–437. doi: 10.1212/WNL.0b013e31827f0f20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vuong LN, Thulasi P, Biousse V, et al. Ocular fundus photography of patients with focal neurologic deficits in an emergency department. Neurology. doi: 10.1212/WNL.0000000000001759. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benbassat J, Polak BC, Javitt JC. Objectives of teaching direct ophthalmoscopy to medical students. Acta Ophthalmol. 2012;90:503–507. doi: 10.1111/j.1755-3768.2011.02221.x. [DOI] [PubMed] [Google Scholar]
- 9.Carlsson AM, ten Hove MW, Stockl F. Direct ophthalmoscopic examination of the eyes: does a mydriatic agent help with diagnosis? Can Fam Physician. 2006;52:958–959. [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed J, Ward TP, Bursell SE, et al. The sensitivity and specificity of nonmydriatic digital stereoscopic retinal imaging in detecting diabetic retinopathy. Diabetes Care. 2006;29:2205–2209. doi: 10.2337/dc06-0295. [DOI] [PubMed] [Google Scholar]
- 11.Lin DY, Blumenkranz MS, Brothers RJ, et al. The sensitivity and specificity of single-field nonmydriatic monochromatic digital fundus photography with remote image interpretation for diabetic retinopathy screening: a comparison with ophthalmoscopy and standardized mydriatic color photography. Am J Ophthalmol. 2002;134:204–213. doi: 10.1016/s0002-9394(02)01522-2. [DOI] [PubMed] [Google Scholar]
- 12.Pitts SR, Niska RW, Xu J, et al. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008:1–38. [PubMed] [Google Scholar]
- 13.Bruce BB, Lamirel C, Wright DW, et al. Blood pressure threshold for abnormal ocular fundus findings is lower than expected. Hypertension. 2012;59:e8–9. doi: 10.1161/HYPERTENSIONAHA.111.187781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henderson AD, Bruce BB, Newman NJ, et al. Hypertension-related eye abnormalities and the risk of stroke. Rev Neurol Dis. 2011;8:1–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Hagen K, Stovner LJ, Vatten L, et al. Blood pressure and risk of headache: a prospective study of 22 685 adults in Norway. J Neurol Neurosurg Psychiatry. 2002;72:463–466. doi: 10.1136/jnnp.72.4.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Headache Classification Committee of the International Headache Society The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 17.Gupta VK. Systemic hypertension, headache, and ocular hemodynamics: a new hypothesis. MedGenMed. 2006;8:63. [PMC free article] [PubMed] [Google Scholar]
- 18.Baker ML, Hand PJ, Wang JJ, et al. Retinal signs and stroke: revisiting the link between the eye and brain. Stroke. 2008;39:1371–1379. doi: 10.1161/STROKEAHA.107.496091. [DOI] [PubMed] [Google Scholar]
- 19.Easton JD, Saver JL, Albers GW, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276–2293. doi: 10.1161/STROKEAHA.108.192218. [DOI] [PubMed] [Google Scholar]
- 20.Schliep v. Providence Yakima Med. Ctr. Wash. App. 2005 [Anonymous] [Google Scholar]
- 21.Lamirel C, Bruce BB, Wright DW, et al. Nonmydriatic digital ocular fundus photography on the iPhone 3G: the FOTO-ED study. Arch Ophthalmol. 2012;130:939–940. doi: 10.1001/archophthalmol.2011.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mackay DD, Garza PS. Ocular fundus photography as an educational tool. Semin Neurol. doi: 10.1055/s-0035-1563572. In press. [DOI] [PubMed] [Google Scholar]
- 23.Kelly LP, Garza PS, Bruce BB, et al. Teaching ophthalmoscopy to medical students (the TOTeMS study). Am J Ophthalmol. 2013;156:1056–1061. e1010. doi: 10.1016/j.ajo.2013.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mackay DD, Garza PS, Bruce BB, et al. Teaching ophthalmoscopy to medical students (TOTeMS) II: A one-year retention study. Am J Ophthalmol. 2014;157:747–748. doi: 10.1016/j.ajo.2013.12.013. [DOI] [PubMed] [Google Scholar]