Abstract
Rationale
In acute stroke, the volume of salvageable brain tissue is maximal at onset and declines rapidly with time. Prehospital start of clinical trial interventions would enable delivery of neuroprotective agents, such as magnesium sulfate, to stroke patients in the hyperacute period when they are potentially most effective.
Aims
A broad aim of the FAST-MAG study is to develop and validate techniques to perform pivotal trials of neuroprotective therapies for acute stroke in the prehospital setting. In tandem with an accompanying general trial design article, this manuscript provides a detailed overview of several novel prehospital study methods employed in the NIH FAST-MAG Trial.
Design
Multicenter, randomized, double-blinded, placebo-controlled, pivotal clinical trial.
Special Prehospital Procedures Distinctive prehospital methods deployed in FAST-MAG include: identifying likely stroke patients using the Los Angeles Prehospital Stroke Screen; eliciting explicit informed consent from patients or on scene legally authorized representatives via cellphone discussion with off-scene physicians; paramedic rating of pretreatment stroke severity using the Los Angeles Motor Scale; assigning patients to a study arm using blinded, pre-encounter randomization; facilitating continuity of study infusion from the field to the ED by stocking ambulances with study kits including both field and hospital doses; and electronic fax consent signature documentation by geographically separated subjects and enrolling physicians.
Discussion
The suite of prehospital trial methods developed for the FAST-MAG Trial enable enrollment of patients in very early time windows, including the hyperacute, ‘golden hour’ period immediately after stroke onset.
Keywords: ambulance, clinical trial, magnesium, neuroprotection, paramedic, prehospital
Introduction
This paper describes in detail novel, prehospital methods used in the Field Administration of Stroke Therapy –Magnesium (FAST-MAG) Phase 3 Trial. A companion paper describes the rationale and general clinical trial design methodology of the FAST-MAG Phase 3 Trial.
Methods
Prehospital screening
Paramedics screen all transported patients to identify potential study candidates. To identify likely stroke patients for enrollment, the FAST-MAG trial employs a two stage screening process. In the first step, paramedics identify potential patients using a modified version of the Los Angeles Prehospital Stroke Screen (LAPSS). The LAPSS is an 8 item diagnostic inventory that takes 1–2 min to perform, has high sensitivity and specificity, is well validated, and is a standard part of ambulance personnel training worldwide (1). For the FAST-MAG trial, the age exclusion for the LAPSS was changed from age <45 to age <40 years old, creating the modified LAPSS (mLAPSS).
The second stage of the screening process is assessment of the patient by phone by the enrolling physician-investigator, based on paramedic report and discussion with the patient and/or on-scene legally authorized representatives. The lower age limit on the mLAPSS increased the pool of patients eligible for the trial while the physician phone screening provided an additional protection against enrollment of too many stroke- mimicking conditions.
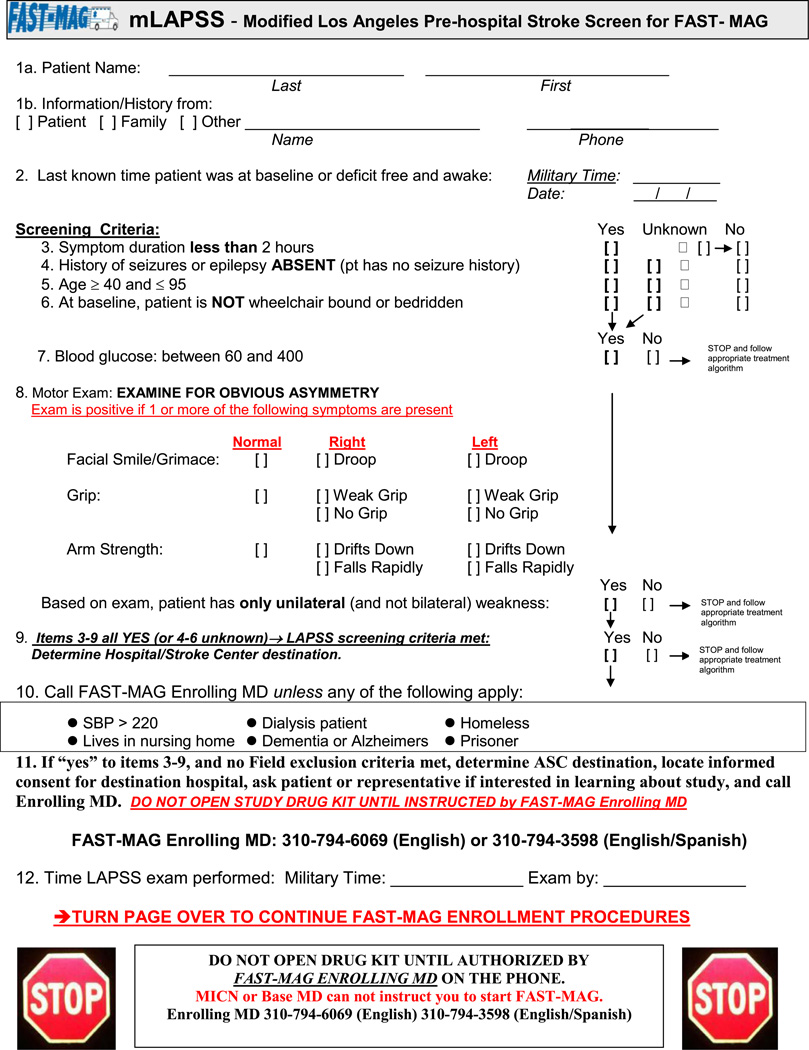
Initially paramedics were instructed to offer the opportunity to learn about the study to all patients meeting study inclusion criteria, with evaluation of all study exclusion criteria left for the phone-enrolling physician-investigator. However, over the course of the study, to reduce the frequency of non-enrollment calls, several exclusion criteria elements were added to paramedic performance. The final paramedic screening form is shown in Fig. 1. In addition to the mLAPSS, the form includes 6 exclusion criteria for paramedics to apply: systolic blood pressure >220, patient on dialysis, history of dementia, patient resident in a nursing home, patient homeless, or patient a prisoner.
Fig. 1.
Screening form for paramedic use to identify potential study candidates.
Paramedics offer the opportunity to learn about the study to all patients meeting mLAPSS inclusion criteria and the 6 straightforward exclusion criteria. The suggested script for paramedics to use is: ‘It looks like you may be having a stroke. You may qualify for a study evaluating an experimental drug for strokes. If you would like more information about the study, we will call the study doctor who will explain the study and the consent form as you read it. While on the phone, we will be providing usual care and getting you ready for transport to the hospital. Would you like me to call the study doctor?’ If the patient or their on-scene representative answers in the affirmative, the paramedic calls the appropriate English- or Spanish-speaking physician enolling line number. The paramedic gives a brief report to the responding physician and then hands the cellular phone to the patient or representative to talk directly with the enrolling physician while the paramedic is released to continue with standard prehospital care.
Prehospital consent
Explicit informed consent
The great preponderance of patients in FAST-MAG are enrolled using explicit, written, informed consent procedures. The consent process is a refinement of that employed in the FAST-MAG Pilot Trial (2). Explicit consent conversations are conducted by an off-site enrolling physician-investigator speaking by cellular phone with the consent provider, in parallel to paramedic delivery of on-site care. Consent conversations are conducted in a language in which the consent provider is fluent, either English or Spanish. At all times, up to 4 English-speaking and up to 4 Spanish –speaking enrolling physician investigators are on call to respond immediately to potential enrollment calls from paramedics in the field. Paramedics are provided with a single phone number for the English-speaking enrolling line and a single phone number for the Spanish-speaking enrolling line. Via a voice-over-internet protocol simultaneous ring system, the enrolling line calls are directed simultaneously to all 4 potentially available physician-enrolling investigators (3). The first physician to answer the call is connected immediately with the paramedic. In every 7–10 day period, one of the on-call physicians is the designated first-responder, expected to answer each call as fast as possible. The remaining physicians are back-up responders, ready to pick-up any call not immediately answered by the designated physician, in case the first-responder physician is in an area with poor cell phone connectivity or is otherwise unavailable to respond promptly to the call. The central enrolling investigator panel of 4 English-speaking and 4 Spanish-speaking physicians performs all enrollments in the trial across all 315 enrolling ambulances from 40 EMS agencies, traveling to 60 receiving hospital Emergency Departments.
The consent provider is the patient if he or she is competent or the patient’s on-scene legally authorized representative if the patient is not competent. Each ambulance carries the English and Spanish consent forms approved by the individual Institutional Review Boards of the 4 to 5 receiving hospitals to which it travels most frequently (total of 8–10 consent forms per ambulance). When a patient or his or her representative indicates they wish to learn more about the study, the paramedic hands them the appropriate English or Spanish language consent form approved by the patient’s destination hospital. The paramedic also hands the individual a cellular phone already connected to the enrolling physician.
The physician completes study eligibility screening by confirming inclusion criteria and assessing for exclusion criteria, answers any questions the consent provider has regarding the study, and assesses the competence of the consent provider based on the individual’s ability to restate key study procedures, risks, and what to do if they wish to discontinue participation. If the patient or their legally authorized representative agrees to participate in the trial, the consent provider signs the consent form in the field. Once the form is signed, the enrolling physician-investigator authorizes the paramedics to begin study agent infusion. Upon arrival at the Emergency Department, the paramedics hand the signed consent form and paramedic-completed study forms to the Emergency Department (ED) bedside clincal nurse. When the responding study coordinator arrives shortly thereafter at the ED, the study coordinator faxes to the enrolling physician-investigator the consent form with the consent provider signature. The enrolling physician-investigator then co-signs the consent form (as the consent elicitor) and faxes it back to the study coordinator. The study coordinator places the double-signed consent form in the study record and provides copies to the patient and to the official medical record.
Exception from explicit informed consent
A small proportion of patients are enrolled in the FAST-MAG Trial under Federal regulations authorizing exception from informed consent (EFIC) for research performed in emergency circumstances. This method of enrollment was added to the trial after launch to increase enrollment rates. Its use is confined to patients who are not competent to provide self-consent and who do not have on scene with them a legally authorized representative (LAR) to provide proxy consent, but who do have on scene with them an informant who knows the patient well (KPW). In the United States, state law determines who can serve as a LAR to provide proxy consent for research. As all FAST-MAG sites are in California, California state law governs the trial and specifies as potential LARs the following categories of individuals: a spouse, a registered domestic partner, a parent, an adult child, a sibling, an agent identified in an Advance Health Care Directive, or a legal conservator or guardian. Sometimes a patient rendered noncompetent by their stroke will have on scene with them an individual who knows them well enough to provide medical history regarding whether they meet study inclusion or exclusion criteria, but who is not legally authorized in California to provide proxy consent research. Such KPW individuals may include a grandparent, an uncle or aunt, an adult grandchild, an adult nephew or niece, an unregistered domestic partner, or a close friend.
In order to be able to enroll such patients, the FAST-MAG trial implemented the processes of community consultation and public disclosure required by EFIC regulations for hospitals in Los Angeles County. A community advisory panel was constituted with representatives from the Southern California Stroke Association, the American Stroke/Heart Association, the American Association for Retired Persons, the National Association for the Advancement of Colored People, and National Hispanic Coalition for the Elderly. Public meetings were held in catchment areas of the participating receiving hospitals, a total of 45 meetings attended by 2069 individuals. Information about EFIC enrolling in the study was also disseminated to the public by print, radio, and television reports, community stroke education lectures, and the internet. Enrolling under EFIC was approved by 36 hospital sites and the Los Angeles EMS Agency.
Prehospital randomization process
To streamline study procedures in the field, the study uses blinded pre-encounter randomization (BPER). In BPER, the study kit to be used for the next-to-be-enrolled patient is identified prior to patient encounter and forward-positioned in the ambulance for immediate use. Each ambulance is stocked with one study kit at a time, containing the next allocation in its permuted block sequence. When an ambulance uses a study kit, the study coordinator assigned to that fire station restocks the vehicle within 24 h with its next assigned kit. The use of BPER means that paramedics do not have to choose between ‘A’ and ‘B’ kits in the potentially chaotic prehospital environment. Once authorized to begin the study infusion, they can simply immediately access the only study kit currently stocked in the vehicle. (After BPER implementation in FAST-MAG, another group independently developed a similar approach with the alternative label ‘step-forward randomization.’ (4))
Prehospital randomization statistical analysis
BPER randomization in the field permits the permuted block randomization schedule to be stratified by ambulance. This ambulance-level stratification deters potential confounding by heterogeneity in patient type and prehospital care processes across different participating EMS systems, which can be important factors related to outcome.
However, stratifying randomization by ambulance means that randomization is not stratified by acute care hospital, as is commonly done in hospital-based acute stroke trials. To investigate the potential impact of hospital variation with different approaches to ambulance stratification, we performed a simulation study prior to trial launch. Based on actual data from the Los Angeles EMS system showing the distribution of hospitals served by emergency vehicles, we simulated the randomization for the FAST-MAG study using the following input parameters: 313 emergency vehicles, up to 69 receiving hospitals, each vehicle delivering patients to 3 to 4 hospitals, an average of 11·6 patients randomized per vehicle, and randomization block sizes of 2 and 4. Stochastic variation was added to each sample and repeated 200 times. We computed maximum hospital-level imbalances in treatment group assignment at each hospital over all simulations and produced summary statistics by hospitals that enrolled <10, 10–20, and >20 patients (Supporting Information Table S1). As expected, the frequency of treatment group imbalances was smaller for a blocksize of 2 than 4. Using a blocksize of 2 and stratifying by emergency vehicle, treatment group balance at the hospital-level was generally well maintained. In the most common scenario of hospitals enrolling more than 20 patients, the maximum imbalance of 8 patients did not occur at all with a blocksize of 2; and at hospitals enrolling 10–20 patients, the maximum imbalance of 6 occurred at only 8%.
Treatment – prehospital and prehospital to hospital transition
The prehospital loading dose is administered through fixed-lumen size tubing (Rely-A-Flow tubing, I Flow Corp; ICU tubing, MedSpec, Inc). Use of electronic infusion pumps is not a standard element of paramedic scope of practice in the United States. The controlled gravity infusion system ensures administration at a preset rate, without requiring paramedics to set an electronic pump, count drops, or adjust roller clamps or an aperture dial. The active arm prehospital dose bag is prepared as 4·44 grams of Magnesium Sulfate in 60 ml of normal saline, allowing 6 ml for priming and 54 ml for administration. The fixed lumen size was selected so that when the intravenous bag is placed at the height above the patient standard in rescue ambulances, the infusion rate is 216 ml/h.
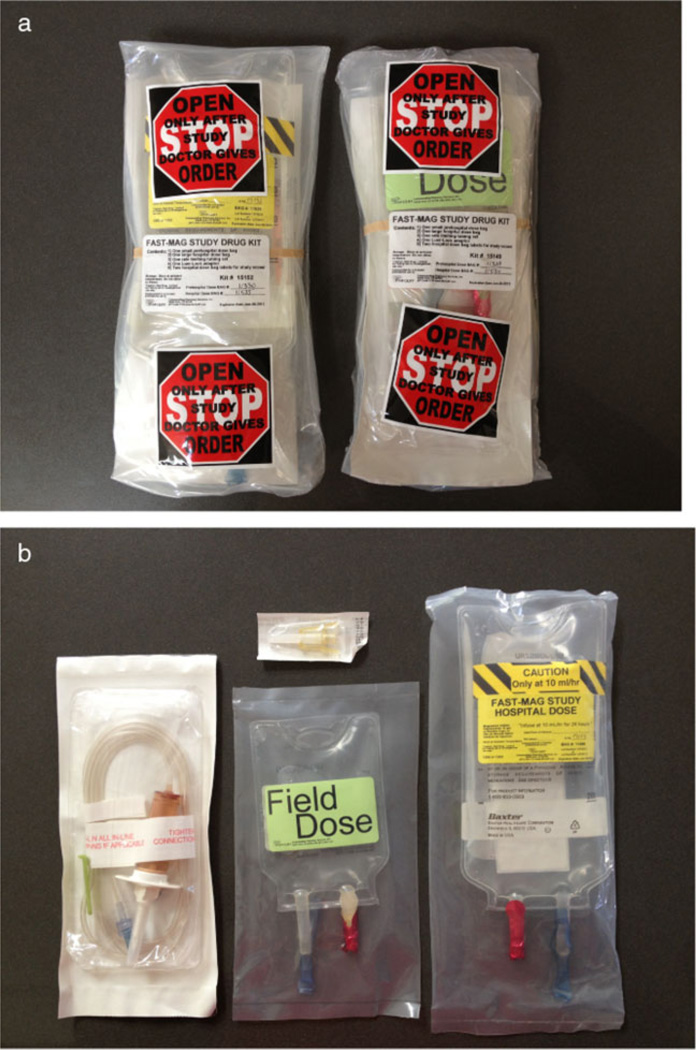
To ensure the immediate availability in the ED of the maintenance infusion to be started at the completion of the 15 min loading dose, each ambulance is stocked with a shrink wrapped study kit that contains the premixed maintenance dose bag in addition to the premixed field loading dose bag and its gravity set tubing (Fig. 2). The field dose bag is smaller (50 cc) and labeled with different wording and colors than the maintenance, hospital dose bag. Enrolling physicians instruct paramedics to ‘Please hang the small, green, field dose bag, and hand the large, yellow, hospital dose bag to the receiving nurse in the ED.’ The receiving ED nurse begins the ambulance-delivered maintenance infusion using a standard infusion pump, as soon as the loading dose is completed.
Fig. 2.
Photos of FAST-MAG study kit carried in each ambulance. (a) Front and back views of the FAST-MAG study kit. (b) Contents of an opened kit. Each shrink-wrapped kit includes one rate controlled gravity set and Luer lock for administration of the prehospital dose, one 50 ml loading dose bag containing premixed study agent or placebo (prehospital dose, green label), and one 250 ml maintenance dose bag containing premixed study agent or placebo (in-hospital dose, yellow label).
Receiving hospital notification of incoming enrollment
Several notifications occur immediately upon enrollment to ensure the receiving hospital is ready to continue the study protocol in patients arriving by ambulance. Immediately after completing the enrollment call with a patient, the field enrolling MD calls the receiving hospital ED and speaks to the receiving hospital Emergency Department Attending, giving a report of the enrollment and reviewing study procedures. Generally all the emergency medicine physicians and the neurology physicians on staff at a receiving hospital are serving as study investigators, so this call also serves as notification of hospital study investigators of the enrollment. If the ED attending on duty is not a study investigator, the enrolling physician-investigator will also call the site Principal Investigator to notify him or her of the enrollment. The ED Principal Investigator or their designee then proceeds directly to the receiving hospital ED or calls the receiving hospital ED and further reviews FAST-MAG study procedures and individual aspects of case-specific clinical care with the attending ED physician.
After discussing the enrollment with the receiving attending physician, the enrolling physician-investigator next calls the on-call site study coordinator. Two study coordinators are on call at all times to respond to study enrollments, one for the Northern and one for the Southern portions of the Los Angeles and Orange County region. After being notified of an enrollment in their area by an enrolling physician-investigator, the on-call study coordinator immediately calls the receiving hospital ED charge nurse, informs him or her of the imminent arrival of a FAST-MAG patient, and reviews study procedures with ED nursing staff. The on-call study coordinator then proceeds directly to the receiving hospital ED to assist with implementation of study procedures.
In parallel with these special study notification processes, paramedics also report patient enrollment to their base station and the receiving hospital ED, using standard ambulance prehospital communication channels (cellphones, ambulance radios, and/or computer notification systems).
Regional organization and central study coordination
Like many prehospital studies (5–8), FAST-MAG is being performed within a large Emergency Medical Services region, with participation of as many receiving facilities as possible. This geographic concentration provides economies of scale in reaching a wide population and training paramedics efficiently, but requires the extension of a research framework to some EMS Provider Agencies and to some community hospitals that have little or no intrinsic research infrastructure. To accomplish this outreach, the FAST-MAG Clinical Coordinating Center has 15 study coordinators (generally research nurses) who work fulltime for the trial. Each study coordinator is assigned ~18 primary fire stations and 4 primary hospitals. The study coordinators are responsible for all training of paramedics at their assigned stations. At the study hospitals, the study coordinators assist the site Principal Investigators with Institutional Review Board approvals and correspondence, and train clinical nursing staff in the ED and inpatient units in study procedures. For hospitals that did not have a Federalwide Assurance (FWA) prior to the FAST-MAG study, the study coordinator also assists the facility in applying for a FWA.
Paramedic education
FAST-MAG study procedures are being implemented by over 3000 paramedics in the Los Angeles and Orange County regions. A continuous paramedic education program is being delivered throughout the study period by the investigators and study coordinators. Paramedics new to the system undergo a 1–2 h formal lecture in stroke pathophysiology and identification, patient screening, study drug administration, and additional study procedures, employing materials modified from those developed and successfully employed in the LAPSS prospective validation study (1). After initial training, knowledge of study procedures is refreshed by frequent fire station visits by study coordinators and a paramedic peer educator, providing opportunistic update training every 3–6 months; and by training video segments included in the mandatory annual countywide paramedic training program. In addition, a trial bimonthly newsletter includes tips and lessons for paramedics from trial experience.
Assessing stroke severity
Pretreatment stroke deficit severity is the dominant predictor of outcome in acute stroke and an essential baseline variable to measure in any treatment trial. However, the standard measure of deficit severity used in traditional trials, the NIH Stroke Scale (NIHSS), is too long for use in the field and cannot be used as a baseline assessment when performed in the ED, as enrolled patients have already been receiving, and possibly responding to, study agent by the time of ED assessment. To rate pretreatment stroke deficit severity, FAST-MAG is using the Los Angeles Motor Scale, a 0–5 point rating of motor deficit severity derived directly from the face, arm, and grip weakness exam section of the LAPSS. When performing the LAPSS, paramedics also automatically perform the LAMS. Though simple and rapid, the LAMS is a useful assessment of stroke deficit severity, correlating well with concurrent NIHSS scores, and predicting final three month disability, activity of daily living, neurologic deficit outcomes, and presence of large vessel occlusion, nearly as well as the full NIHSS (9,10).
Discussion
In addition to testing magnesium sulfate specifically, developing and validating general methods to perform pivotal trials of neuroprotective treatments in the prehospital setting is a central broad aim of the NIH FAST-MAG trial. The distinctive prehospital methods developed for FAST-MAG include procedures for stroke identification (LAPSS), informed consent elicitation (physician cellphone discussion), rating of stroke severity (LAMS), randomized assignment to a study arm (blinded, pre-encounter randomization), field study agent infusion (gravity controlled tubing), continuous field to ED drug administration (ambulance stocking of study kit containing both field and hospital doses), and consent signature documentation (electronic fax of consent papers to and from receiving hospital). These approaches are designed to enable FAST-MAG to be: (a) the first prehospital pivotal pharmacologic stroke trial; (b) the first stroke treatment trial to enroll a substantial cohort of patients in the ‘golden hour,’ the initial 60 min after onset; (c) the first prehospital pivotal trial for any condition to employ physician cellphone elicitation of explicit informed consent; and (d) the first pharmacologic neuroprotective trial to deliver study agent in advance of recanalization therapy, potentially permitting more brain tissue to still be salvageable when reperfusion is achieved.
Supplementary Material
Footnotes
Conflicts of Interest: None declared.
Additional Supporting Information may be found in the online version of this article at the publisher’s web-site:
Table S1 Projected frequencies of hospital-level imbalance in treatment assignments for different ambulance-based stratified randomization parameters.
References
- 1.Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles Prehospital Stroke Screen (LAPSS) Stroke. 2000;31:71–76. doi: 10.1161/01.str.31.1.71. [DOI] [PubMed] [Google Scholar]
- 2.Saver JL, Kidwell C, Eckstein M, Ovbiagele B, Starkman S. Physician-investigator phone elicitation of consent in the field: a novel method to obtain explicit informed consent for prehospital clinical research. Prehosp Emerg Care. 2006;10:182–185. doi: 10.1080/10903120500541035. [DOI] [PubMed] [Google Scholar]
- 3.Sanossian N, Starkman S, Liebeskind DS, et al. Simultaneous ring voice-over-internet phone system enables rapid physician elicitation of explicit informed consent in prehospital stroke treatment trials. Cerebrovasc Dis. 2009;28:539–544. doi: 10.1159/000247596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao W, Ciolino J, Palesch Y. Step-forward randomization in multicenter emergency treatment clinical trials. Acad Emerg Med. 2010;17:659–665. doi: 10.1111/j.1553-2712.2010.00746.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Longstreth WT, Jr, Fahrenbruch CE, Olsufka M, Walsh TR, Copass MK, Cobb LA. Randomized clinical trial of magnesium, diazepam, or both after out-of-hospital cardiac arrest. Neurology. 2002;59:506–514. doi: 10.1212/wnl.59.4.506. [DOI] [PubMed] [Google Scholar]
- 6.Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. JAMA. 2000;283:783–790. doi: 10.1001/jama.283.6.783. [DOI] [PubMed] [Google Scholar]
- 7.Alldredge BK, Gelb AM, Isaacs SM, et al. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med. 2001;345:631–637. doi: 10.1056/NEJMoa002141. [DOI] [PubMed] [Google Scholar]
- 8.Aufderheide TP, Nichol G, Rea TD, et al. A trial of an impedance threshold device in out-of-hospital cardiac arrest. N Engl J Med. 2011;365:798–806. doi: 10.1056/NEJMoa1010821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Llanes JN, Kidwell CS, Starkman S, Leary MC, Eckstein M, Saver JL. The Los Angeles Motor Scale (LAMS): a new measure to characterize stroke severity in the field. Prehosp Emerg Care. 2004;8:46–50. doi: 10.1080/312703002806. [DOI] [PubMed] [Google Scholar]
- 10.Nazliel B, Starkman S, Liebeskind DS, et al. A brief prehospital stroke severity scale identifies ischemic stroke patients harboring persisting large arterial occlusions. Stroke. 2008;39:2264–2267. doi: 10.1161/STROKEAHA.107.508127. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.