Abstract
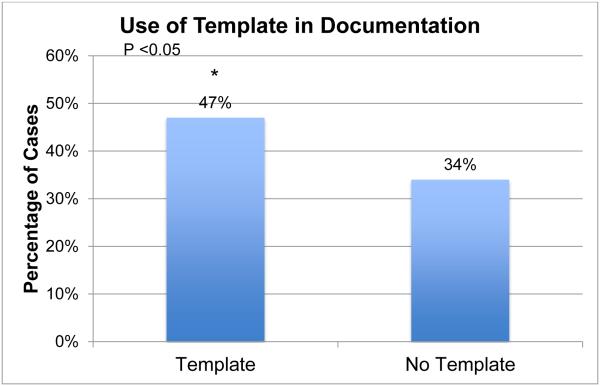
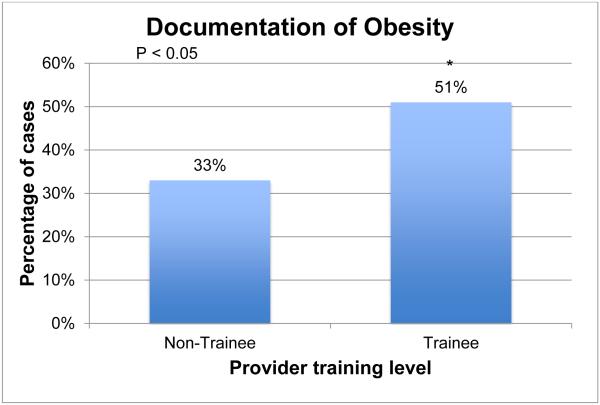
Identification of obesity at well-child care (WCC) examinations is a step towards intervention. Studies have shown suboptimal documentation in primary care clinics that can improve with the use of Electronic Health Records (EHR). This study investigated the impact of a standardized EHR template on documentation of obesity at WCC visits and its impact on physician behavior. A cohort of 585 children with severe early onset obesity (BMI > 99th percentile, age < 6 years) was identified with an electronic algorithm. Complete records of visit notes were reviewed to extract history taking, counseling, and recording of obesity. Use of a standardized EHR template for WCC visits is associated with improvement in rates of documentation of obesity (47 v/s 34%, P < 0.01), without interruption of workflow. Documentation of obesity in the chart improved nutritional (66 v/s 44%, P < 0.001) and physical activity counseling (23 v/s 9%, P < 0.001).
Keywords: severe obesity, documentation, electronic health records, template, pediatric obesity
Background
Obesity remains a major public health concern. The rates of severe childhood obesity continue to rise at an alarming rate1,2, although there is a plateau in the overall rates3. Youth with severe obesity have a much more adverse cardio-metabolic profile with signs of vascular dysfunction and subclinical atherosclerosis as early as 9 years of age4–6, compared to overweight or obese children. Tracking of adiposity from childhood into adult life is much stronger in the severely obese7,8 with concomitant morbidity and premature mortality9–11. Despite the awareness, there is ample evidence on suboptimal clinical documentation of diagnoses and management plan in the medical records in the primary care clinics (PCC)12–16. Finding effective ways to improve documentation and early intervention is especially important for severe childhood obesity due to the aforementioned risk factors.
Timely identification is a crucial step towards intervention. Studies have found better response to lifestyle changes during early childhood compared to adolescence, especially in children with severe obesity17,18. In response, the American Academy of Pediatrics (AAP) revised its childhood obesity prevention and management guidelines for primary care in 200719. Subsequent studies have revealed major gaps in guideline awareness20 and scarce documentation of obesity-related assessment 21. These findings emphasize the need to augment current approaches to increase the uptake.
Suboptimal documentation of obesity in PCC remains a significant bottleneck in management12–14,22. In a study of 2 clinics with general and specialist pediatricians, only 31% of the visits for patients who were overweight or obese included appropriate documentation13. In the National Hospital and Ambulatory Medical Care Survey of 1155 obese pediatric patients, only 18% (CI 13-23%) of the clinical notes showed accurate documentation of obesity23. This is especially important as patients who have obesity documented as a diagnosis are significantly more likely to have a management plan in the notes in both children and adults23,24.
The availability of Health Information Technology (HIT) is changing this scenario rapidly. HIT tools including Electronic Health Records (EHRs), computerized provider order entry (CPOE) and smart sets (standardized progress notes) are now available for chronic disease management. The use of automatic Body Mass Index (BMI) calculation at the point of care has demonstrated improvement in obesity documentation among both children and adults25–28. Tang et al showed that clinicians using an EHR-based toolset for weight-related documentation and counseling impacted patient lifestyle behaviors on short –term follow-up26. Other HIT tools including computerized alerts, clinical guidelines, order sets, documentation templates, diagnostic tools and clinical workflow tools are also available, that have the potential to make meaningful changes in long-term clinical outcomes. However, a recent systematic review revealed that most studies have focused on calculation, display or plotting of BMI (or BMI percentiles). Few have examined the use of other EHR features in weight-related outcomes in patients 29, and no studies have focused on children with severe early onset obesity.
In the current environment of information overload, it is not yet known which of the available HIT tools will be most effective while avoiding provider fatigue. A systematic review on use of electronic alerts for chronic disease management showed only a modest improvements in care with on-screen point of care reminders30. Use of large scale paradigm shifting changes in EHRs, although available, are fraught with challenges in design and implementation31 and provider engagement32. In one study, providers were found to ignore the flashing screen alerts during their workflow and considered navigating to a different screen for “Smartset” orders for obesity management a burden, although they used well-child care (WCC) visit Smartset regularly32. There is an urgent need to investigate the effects of small steps to optimize physician documentation behavior without disrupting workflow or producing alert fatigue. This study investigates the impact of a standardized electronic WCC visit template, without a specific focus on obesity, on documentation and management of children with severe early onset obesity.
Methods
A standardized electronic template for the documentation of the WCC visits was introduced in the primary care clinic at Boston Children’s Hospital (BCH) in 2012 (Table 1). This template provides automatic population of problem list, medication list, allergies, body measurements, and vital signs into the clinical note. It also provides prompts for age appropriate health topics such as nutrition, physical activity, sleep, elimination, along with other components of WCC like developmental screening, social and family history. The assessment and plan section has prompts related to weight management to be addressed in all children. Each section has pre-defined sentence prompts that are designed to facilitate history taking and documentation. The Electronic Health Records implementation group at BCH has validated the template using the Office for National Coordinator for Health Care Technology EHR certification criteria and meaningful use Stage 2 criteria33. Use of template while documenting a well-child visit is encouraged, but not mandatory.
Table 1.
Selected obesity-related elements included in the well-child visit note template
| Age Appropriate Health Topics |
|---|
| Nutrition |
| Drinks _ % Milk |
| Drinks 2-3 glasses of milk/day? _ |
| Drinks>1 glass of juice or soda/day? _ |
| Eating fruits and vegetables? _ |
| Physical activity |
| Exercise outside of school? _ |
| Sleep |
| Regular bedtime? _ |
| TV in bedroom? _ |
| Elimination |
| Caregiver concerns: _ |
| Fully toilet trained? _ |
| Enuresis or encopresis? _ |
| Physical Examination |
| Height, weight, BMI (%’ile)1 |
| Impression And Plan |
| Routine Health Maintenance |
| Growth_ |
| Healthy nutrition and activity counseling?_ |
| Active Problems |
| Childhood Obesity (BMI 95-100 percentile)2 |
Imports automatically into the note
If previously added to the patient’s problem list, will import automatically into the note
Population
We reviewed the health records of children between the ages of 2-19 years with 2 or more documented BMI measurements > 99th percentile before their 6th birthday. Severe obesity was defined as BMI percentile > 99th for age, as these readings are automatically calculated and displayed in the EHR (Power Chart, Cerner Corp, Kansas City, MO), with no provision to display the current CDC definition for severe obesity of BMI > 120% of 95th percentile34. Records were identified using an electronic algorithm incorporating structured data (height, weight, diagnoses codes, medication list etc.) and unstructured data (free-text clinical notes) between 2007 and 2013. The algorithm excluded children with pathogenic causes of obesity including primary endocrinopathy or neoplasm. Children with prolonged steroid use (> 14 days or, 3 separate courses with a total of 28 days in the 6 months prior to the measurement) were also excluded. This algorithm was designed and validated for the Electronic Health Records and Genomics (eMERGE) Study sponsored by NHGRI (details in supplement). The algorithm was used to extract data for children seen throughout the hospital, and the subset of children visiting the primary care center for WCC visit were selected for this study. A total of 585 unique children with severe early onset obesity were seen in the PCC between 2007-13. Of these, 311 children had at least one WCC visit documented in 2009-14. We chose to review notes after 2009, to allow for the implementation of the AAP guidelines on management of childhood obesity19. Data was extracted from the most recent WCC visit. The group was divided into the visits where the standardized template was used (n = 137, 2013-14) and those where it was not used (n =174, 2009-14) based on the structure of the note.
Definitions
Body mass index (BMI) was calculated using the height and weight obtained on the same day using the formula BMI = [weight in (kg)]/ [height (m)] 2. BMI percentile was based on CDC 2000 growth curves developed by National Center for Health Statistics (www.cdc.gov/growthcharts). The EHR automatically calculated BMI upon entry of height and weight during well-child visits. Height, weight, BMI percentiles are available at the point of care along with blood pressure, heart rate and temperature on the initial EHR screen for the visit. Documentation of overweight or obese was defined as the inclusion of the key words: “overweight”, “obese”, or “obesity”, “weight gain” in the clinical note. Documentation also included the use of obesity-related ICD-9 codes for the visit (codes 278.00, 278.0, 278.01, 278.02, 278.1, 2, 3, 783.1, 259.8, V85.54, V77.8). Presence of standardized data fields in the clinical note was used to identify the template. Nutritional history, history of intake of sugary drinks, physical activity and screen time were identified by the presence of a brief description of each field in the clinical note. Nutritional counseling was defined as any recommendation to reduce the intake of highly refined or processed foods (e.g. sugary drinks, fast food) or increase intake of healthful foods (vegetables, healthy fats). Physical activity counseling was defined as any recommendation to increase physical activity, whether via sports, daily exercise, gym classes or other activities. Screen time counseling was defined as any recommendation to reduce the amount of time spent in front of a screen (TV, computer, or electronics). Training level was dichotomized as non-trainees (attending physicians, or other providers) and trainees (resident physician or fellow). The Institutional Review Board at BCH approved the study. Due to the nature of the data extraction, a waiver of informed consent was obtained. All data extraction was validated by dual extraction by two investigators (VT and FL) with a concordance rate > 80%.
Statistical analysis
Univariate analysis was performed using χ2 tests. A p-value < 0.05 was considered significant. Multivariate logistic regression analysis was performed to examine the association between use of the template and documentation of obesity while adjusting for age, gender, nutritional, physical activity and screen time history, in addition to training level. We also examined this association using a multi-level mixed logistic regression model while adjusting for provider as the clustering variable. Statistical analyses were performed using STATA v.12 (Statacorp LP, College Station, TX).
Results
Table 2 displays selected baseline characteristics of the cohort of children seen at the visits studied. A total of 311 unique patients attending WCC visit at the PCC were included in the study. The gender distribution showed a predominance of males (63%). Forty seven percent of children were African American and 40% of Hispanic ethnicity, reflecting the patient population seen at the PCC. Attending physicians evaluated 62% of the patients compared to 38% resident physician or fellows in training.
Table 2.
Selected Characteristics of the Study cohort
| Patient Characteristics | Number of visits (%) N= 311 |
|---|---|
| Age 2-5 years 6-10 years |
147 (47.2) 164 (52.7) |
| Gender Male Female |
195 (62.7) 116 (37.2) |
| Race Caucasian African American Other Asian Not reported |
19 (6.1) 145 (46.6) 112 (36.0) 6 (1.9) 29 (9.3) |
| Ethnicity Hispanic/Latino Not Hispanic/Latino |
128 (41.1) 183 (58.8) |
| Provider Characteristics | |
| Level of Training Trainee Non-trainee |
118 (37.9) 193 (62.0) |
Use of template was associated with a higher rate of documentation of obesity (Figure 1, p= 0.015). A detailed history on nutrition was noted in the charts often, not influencing documentation of obesity (p = 0.26). However, physicians who noted a history of physical activity (p <0.001), intake of sugary drinks (p = 0.016), and screen time (p = 0.015) were more likely to document obesity. Trainee physicians were more likely to document obesity in the chart compared to non-trainees (Figure 2, p= 0.002). The relationship between use of template and documentation of obesity remained when multivariate logistic regression was used (p < 0.001) adjusting for age, gender, nutritional, physical activity, screen time history and training level of the physician with or without clustering for the provider (Table 3). As over 80% of the children were from race/ethnic minorities (Table 2), we elected not to include this variable in the model. When obesity was documented in the note, the probability of offering counseling for nutrition (p < 0.001), physical activity (p = 0.001), and a follow-up (p= 0.002) visit were much higher (Table 3). The small samples for screen-time counseling limit evaluation.
Figure 1.
Effect of use of template on documentation of obesity
Figure 2.
Association between training level and documentation of obesity
Table 3.
Association between obesity-related behavior history, counseling and documentation of obesity
|
Documentation of
Obesity n=124 (%) |
No Documentation of
Obesity n = 187 (%) |
P-value
(univariate analysis) |
P-value
(logistic regression) |
|
|---|---|---|---|---|
| Template use | 65 (52) | 72 (38) | 0.01 | 0.03 |
| Nutrition documentation1 |
122 (98) | 181(98) | 0.38 | 0.98 |
| Detailed nutrition history2 |
75 (60) | 101 (54) | 0.26 | - |
| Physical activity history | 31 (27) | 14 (11) | <0.001 | <0.001 |
| Sugary drinks history | 82 (66) | 98 (52) | 0.01 | - |
| Fast food history3 | 19 (20) | 14 (12) | 0.13 | - |
| Screen time history3 | 11 (9) | 5 (2) | 0.01 | 0.29 |
| Nutritional counseling | 82 (66) | 82 (44) | <0.001 | - |
| Physical activity counseling |
28 (23) | 17 (9) | <0.001 | - |
| Screen time counseling3 | 19 (15) | 17 (9) | 0.09 | - |
| Trainee | 60 (48) | 58 (31) | <0.001 | 0.03 |
| Follow-up | 29 (23) | 19 (10) | <0.001 | - |
Minimum documentation only for the automatic EHR prompts.
Detailed free-text description of the nutritional history.
Assessment based on the free-text description.
Discussion
Accurate documentation of diagnoses is critically important in the management of chronic health conditions. This is being increasingly recognized as an important benchmark in improving patient care assisted by the nationwide emphasis on EHRs and ICD-10 diagnoses codes. The implementation of ICD-10-Clinical Management /Procedure Coding System (ICD-10-CM/PCS) will require organizations to capture detailed information at the point of care. Since ICD-10-CM/PCS provides increased specificity in its code sets, clinical documentation to support the specificity will be imperative. This can be facilitated through the effective use of EHR templates. Our study suggests that use of a standardized EHR template for WCC visit, without a special emphasis on obesity, in PCC improves documentation of diagnosis and management plan in children with severe early onset obesity.
Health Information technology has the potential to improve the quality of care, reduce the cost associated with delivering health care, and engage patients and families in innovative ways 35. Rao et al have suggested several ways in which EHRs can be used in chronic disease management and transition of care. These include supporting providers in tracking, coordinating, and managing tasks for high-risk individuals; helping ensure patient safety through electronic prescribing and drug interaction alerts; and improving self-management through methods such as secure messaging, data and information exchange, and patient portals36.
Many Smart sets and clinical decision support algorithms are being developed as features of EHRs to facilitate management of chronic conditions. Co et al reported a multi-center cluster randomized trial evaluating the effectiveness of use of clinical reminders to assess symptoms of ADHD along with availability of an ADHD progress note template with structured data fields. They reported a 20% increase in follow-up visits for ADHD (OR 1.9) and improved clinical documentation37. Talmi et al reported that incorporation of the developmental screening template along with electronic referral system resulted in improved documentation of developmental screening in the chart with improved rates for referral to Early Intervention and subsequent follow-up visits38.
Childhood obesity is now recognized as a chronic disease that can follow similar models for management. The High Five for Kids study reported 1-year outcomes of BMI and other obesity related behaviors from a multi-site randomized control trial after a comprehensive intervention with enhancements of the EHR that incorporates templates, printable materials, electronic reminders and comprehensive billing codes39. Additionally, the study included a comprehensive training of clinical and administrative staff in behavioral interventions. The trial showed a small, non-significant change in BMI in the intervention group (p = 0.15), although there was a significant improvement in the television and video-viewing behavior (p = 0.001). However, as this study did not have a factorial design, it is difficult to interpret the effectiveness of each intervention39. Rattay et al reported a comprehensive overhaul of the EHR for system-level changes based on the chronic care model. Their system modification includes provision of automated BMI measurements, mandatory completion of growth assessment fields, along with alerts for the high BMI. Providers seeing the alerts are directed to a practice alert smart set to facilitate orders and referrals for evaluation and management of comorbidities associated with overweight. Structured fields and “smart phrases’ help in documentation of motivational interviewing. The challenges in implementation included resource allocation, and difficulties in acceptance by the clinical and office staff31. A Cochrane systematic review on the use of point of care computer reminders suggested that more research is necessary to identify design and conceptual features that can help physicians adopt recommended pediatric obesity screening and preventive guidelines30.
However, paradigm-shifting changes in electronic medical records are fraught with problems of provider acceptance. Dryden et al report analysis of in-depth, qualitative interviews of pediatric physicians at a primary care network where an electronic support tool for management of obesity was introduced. This report highlights the challenges faced by providers in adopting such guidelines. The majority of providers did not feel that the supports worked. The automated reminders were noted to be associated with alert fatigue, perception of inefficiency and inappropriate or inconsistent. The use of obesity smart set was found to be superfluous, interfere with workflow and the ability of providers to engage with patients resulting in abandoning the use in short time. The study also notes that most providers found the well-visit smart set helpful and used it regularly32.
In an era where the primary care physician carry the responsibility of managing several conditions requiring chronic care model such as ADHD, asthma, developmental screening, obesity and others, availability of electronic support tools for each condition may not be the right answer for the time strapped practicing clinician. Based on the data on improved documentation of obesity and care plan in our study, we propose that a broad general template that guides clinicians rather than imposing additional clicks and navigation of multiple screens presents an opportunity for use of HIT without interfering with workflow. Additionally, implementation of a generic template coupled with an orderset that allows physicians to make choices based on the patient needs provides flexibility while facilitating care. The documentation of the trainees was far better than those of non-trainees similar to that in a prior study40. Although this could be due to better familiarity of the trainees with HIT, it may also reflect the role of the proximity of the education received by trainees. We propose that provision of resources for continued education about care guidelines, and assistance in documenting motivational interviewing31 are more likely to persuade providers to use available electronic tools rather than redirecting resources towards decision support tools that involve additional screens and clicks.
Our retrospective study is limited by a small sample size and the observational study design, which has the potential for uncontrolled confounding. It is possible that documentation does not reflect the actual encounter and conversations between the provider and the family. However, based on the uptake of the WCC template and the use of obesity order-set, it can be concluded that this can serve as an important first step in improving the documentation that will be required with the implementation of ICD-10. Continued training of providers in standards of care and motivational interviewing with prompts or “smart phrases” to guide them through the process, document readiness for change with easy access to visual materials to communicate weight issues may prove helpful. We reviewed notes recorded between 2009-14. It is possible that temporal changes in obesity management can influence documentation. However, we excluded notes prior to 2009 to allow for the implementation lag of the updated AAP guidelines published in 200719. Additionally, over 80% of the notes without template were recorded between 2013-14 giving us confidence that the template was indeed responsible for the improvement in documentation.
Conclusions
Our data suggests that use of a standardized EHR template improves documentation of childhood obesity. A generalized template can be created easily without access to specialized resources by most EHRs. It provides an easy way to guide clinicians in care of chronic condition without creating alert fatigue and disruption of workflow. Trainees are more likely to document childhood obesity, regardless of template use. Physician behavior for counseling appears to be positively influenced by documentation of obesity.
Supplementary Material
Acknowledgements
We would like to thank Dean Reede, Dr. Shelia Nutt, Dr. Melissa Wu, and the staff at Project Success in the Office of Diversity and Community Inclusion at Harvard Medical School.
Funding Sources: This work was supported in part by NIH T32DK007699 (VVT).
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
Contributor’s Statement:
Vidhu V. Thaker: Dr. Thaker conceptualized and designed the study, carried out the initial analyses, drafted the initial manuscript, and approved the final manuscript as submitted.
Felix Lee: Mr. Lee participated in study design, performed data extraction, participated in data analyses, and approved the final manuscript as submitted.
Clement J. Bottino: Dr. Bottino participated in conceptualization and study design, reviewed and approved the manuscript as submitted.
Cassandra L. Perry: Ms. Perry is part of eMERGE Consortium- Boston Childrens Hospital: Funded by NHGRI, the resources of this working group were used in generating the list of patients to be studied. She has reviewed and approved the manuscript.
Ingrid A. Holm: Dr. Holm is the Principal Investigator of eMERGE Consortium – Boston Children's Hospital: Funded by NHGRI, the resources of this working group were used in generating the list of patients to be studied. She also reviewed and approved the manuscript.
Joel N. Hirschhorn: Dr. Hirschhorn provided the resources for conduct of the study, reviewed and approved the manuscript as submitted.
Stavroula K. Osganian: Dr. Osganian provided mentorship for the study, facilitated analyses, reviewed and approved the manuscript as submitted.
References
- 1.Skinner A, Skelton J. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr. 2014;168(6):561–566. doi: 10.1001/jamapediatrics.2014.21. [DOI] [PubMed] [Google Scholar]
- 2.Lo JC, Chandra M, Sinaiko A, et al. Severe obesity in children: prevalence, persistence and relation to hypertension. Int J Pediatr Endocrinol. 2014;2014(1):3. doi: 10.1186/1687-9856-2014-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Sun C, Cheung M, Viikari JSA, Dwyer T. Childhood Adiposity, Adult Adiposity, and Cardiovascular Risk Factors. N Engl J Med. 2011;365(20):1876–1885. doi: 10.1056/NEJMoa1010112. RO. [DOI] [PubMed] [Google Scholar]
- 5.Michalsky MP, Inge TH, Simmons M, et al. Cardiovascular Risk Factors in Severely Obese Adolescents: The Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) Study. JAMA Pediatr. 2015 Mar; doi: 10.1001/jamapediatrics.2014.3690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(1):12–17.e2. doi: 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 7.Singh AS, Mulder C, Twisk JWR, van Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474–488. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 8.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005;115(1):22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 9.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362(6):485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Juonala M, Magnussen CG, Berenson GS, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365(20):1876–1885. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- 11.Morrison JA, Friedman LA, Gray-McGuire C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: the Princeton Lipid Research Clinics Follow-up Study. Pediatrics. 2007;120(2):340–345. doi: 10.1542/peds.2006-1699. [DOI] [PubMed] [Google Scholar]
- 12.O’Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114(2):e154–e159. doi: 10.1542/peds.114.2.e154. [DOI] [PubMed] [Google Scholar]
- 13.Riley MR, Bass NM, Rosenthal P, Merriman RB. Underdiagnosis of pediatric obesity and underscreening for fatty liver disease and metabolic syndrome by pediatricians and pediatric subspecialists. J Pediatr. 2005;147(6):839–842. doi: 10.1016/j.jpeds.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 14.Melamed OC, Nakar S, Vinker S. Suboptimal identification of obesity by family physicians. Am J Manag Care. 2009;15(9):619–624. [PubMed] [Google Scholar]
- 15.Cook S, Weitzman M, Auinger P, Barlow SE. Screening and counseling associated with obesity diagnosis in a national survey of ambulatory pediatric visits. Pediatrics. 2005;116(1):112–116. doi: 10.1542/peds.2004-1517. [DOI] [PubMed] [Google Scholar]
- 16.Mabry IR, Clark SJ, Kemper A, Fraser K, Kileny S, Cabana MD. Variation in establishing a diagnosis of obesity in children. Clin Pediatr (Phila) 2005;44(3):221–227. doi: 10.1177/000992280504400305. [DOI] [PubMed] [Google Scholar]
- 17.Danielsson P, Kowalski J, Ekblom Ö , Marcus C. Response of severely obese children and adolescents to behavioral treatment. Arch Pediatr Adolesc Med. 2012;166(12):1103–1108. doi: 10.1001/2013.jamapediatrics.319. [DOI] [PubMed] [Google Scholar]
- 18.Knop C, Singer V, Uysal Y, Schaefer A, Wolters B, Reinehr T. Extremely obese children respond better than extremely obese adolescents to lifestyle interventions. Pediatr Obes. 2013 Dec; doi: 10.1111/j.2047-6310.2013.00212.x. [DOI] [PubMed] [Google Scholar]
- 19.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 20.Rhodes ET, Ebbeling CB, Meyers AF, et al. Pediatric obesity management: variation by specialty and awareness of guidelines. Clin Pediatr (Phila) 2007;46(6):491–504. doi: 10.1177/0009922806298704. [DOI] [PubMed] [Google Scholar]
- 21.Sharifi M, Rifas-Shiman SL, Marshall R, et al. Evaluating the implementation of expert committee recommendations for obesity assessment. Clin Pediatr (Phila) 2013;52(2):131–138. doi: 10.1177/0009922812471712. [DOI] [PubMed] [Google Scholar]
- 22.Ruser CB, Sanders L, Brescia GR, et al. Identification and management of overweight and obesity by internal medicine residents. J Gen Intern Med. 2005;20(12):1139–1141. doi: 10.1111/j.1525-1497.2005.0263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel AI, Madsen KA, Maselli JH, Cabana MD, Stafford RS, Hersh AL. Underdiagnosis of pediatric obesity during outpatient preventive care visits. Acad Pediatr. 2010;10(6):405–409. doi: 10.1016/j.acap.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bardia A, Holtan SG, Slezak JM, Thompson WG. Diagnosis of obesity by primary care physicians and impact on obesity management. Mayo Clin Proc. 2007;82(8):927–932. doi: 10.4065/82.8.927. [DOI] [PubMed] [Google Scholar]
- 25.Keehbauch J, Miguel GS, Drapiza L, Pepe J, Bogue R, Smith-Dixon A. Increased documentation and management of pediatric obesity following implementation of an EMR upgrade and education. Clin Pediatr (Phila) 2012;51(1):31–38. doi: 10.1177/0009922811417293. [DOI] [PubMed] [Google Scholar]
- 26.Tang JW, Kushner RF, Cameron KA, Hicks B, Cooper AJ, Baker DW. Electronic tools to assist with identification and counseling for overweight patients: a randomized controlled trial. J Gen Intern Med. 2012;27(8):933–939. doi: 10.1007/s11606-012-2022-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schriefer SP, Landis SE, Turbow DJ, Patch SC. Effect of a computerized body mass index prompt on diagnosis and treatment of adult obesity. Fam Med. 2009;41(7):502–507. [PubMed] [Google Scholar]
- 28.Bordowitz R, Morland K, Reich D. The use of an electronic medical record to improve documentation and treatment of obesity. Fam Med. 2007;39(4):274–279. [PubMed] [Google Scholar]
- 29.Baer HJ, Karson AS, Soukup JR, Williams DH, Bates DW. Documentation and diagnosis of overweight and obesity in electronic health records of adult primary care patients. JAMA Intern Med. 2013;173(17):1648–1652. doi: 10.1001/jamainternmed.2013.7815. [DOI] [PubMed] [Google Scholar]
- 30.Shojania KG, Jennings A, Mayhew A, Ramsay CR, Eccles MP, Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane database Syst Rev. 2009;3:CD001096. doi: 10.1002/14651858.CD001096.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rattay KT, Ramakrishnan M, Atkinson A, Gilson M, Drayton V. Use of an electronic medical record system to support primary care recommendations to prevent, identify, and manage childhood obesity. Pediatrics. 2009;123(Suppl):S100–S107. doi: 10.1542/peds.2008-1755J. May 2007. [DOI] [PubMed] [Google Scholar]
- 32.Dryden EM, Hardin J, McDonald J, Taveras EM, Hacker K. Provider perspectives on electronic decision supports for obesity prevention. Clin Pediatr (Phila) 2012;51(5):490–497. doi: 10.1177/0009922812436549. [DOI] [PubMed] [Google Scholar]
- 33.Department of Health and Human Services Health Information Technology: Standards, Implementation Specifications, and Certification Criteria for Electronic Health Record Technology, 2014 Edition; Revisions to the Permanent Certification Program for Health Information Technology. 2012 https://www.federalregister.gov/articles/2012/09/04/2012-20982/health-information-technology-standards-implementation-specifications-and-certification-criteria-for. Published September 4, 2012. Accessed September 1, 2015. [PubMed]
- 34.Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index – for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90(4):1314–1320. doi: 10.3945/ajcn.2009.28335. [DOI] [PubMed] [Google Scholar]
- 35.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care--a national survey of physicians. N Engl J Med. 2008;359(1):50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- 36.Rao S, Brammer C, McKethan A, Buntin MB. Health information technology: transforming chronic disease management and care transitions. Prim Care. 2012;39(2):327–344. doi: 10.1016/j.pop.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 37.Co JPT, Johnson SA, Poon EG, et al. Electronic health record decision support and quality of care for children with ADHD. Pediatrics. 2010;126(2):239–246. doi: 10.1542/peds.2009-0710. [DOI] [PubMed] [Google Scholar]
- 38.Talmi A, Bunik M, Asherin R, et al. Improving Developmental Screening Documentation and Referral Completion. Pediatrics. 2014 Sep; doi: 10.1542/peds.2012-1151. [DOI] [PubMed] [Google Scholar]
- 39.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Arch Pediatr Adolesc Med. 2011;165(8):714–722. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hillman JB, Corathers SD, Wilson SE. Pediatricians and screening for obesity with body mass index: does level of training matter? Public Health Rep. 2009;124(4):561–567. doi: 10.1177/003335490912400413. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.