Abstract
Intrauterine devices (IUDs) are reliable method for contraception. Although, they are generally regarded as safe, serious consequences may occur in case of uterine perforation or intravesical migration. We present a rare case of a 74 year old lady with a forgotten IUD for 42 years resulting in intravesical migration, formation of vesicovaginal fistula (VVF) without uterine perforation, complete urinary incontinence, recurrent urinary tract infections (UTIs) and a large vesicovaginal calculus.
Keywords: Saf-T-Coil, IUD, Vesicovaginal fistula, Bladder calculus
Background
A 74 year old female described the insidious onset of increasing frequency, urgency, mixed urinary incontinence and suprapubic discomfort over the previous 12 months. During this time she had been treated by her GP for recurrent culture proven Proteus mirabilis UTIs. Following an episode of painless vaginal bleeding 6 months after the initial onset of her urinary symptoms, she was referred to gynecological services for urgent investigation of postmenopausal bleeding.
While with the gynecology department, hysteroscopy and MRI pelvis were performed revealing a vesicovaginal fistula (VVF), bladder and vaginal calculi (Fig. 1). The uterus was empty and appeared normal. Cytology washings of the upper vagina did not reveal any malignant cells. At this point, patient was referred to our urology service for evaluation and management of bladder calculus.
Figure 1.
T2-weighted contrast enhanced MRI pelvis showing Vesicovaginal fistula (VVF) (arrow) and calculi on an axial section (A), Plain X-ray KUB demonstrating a 5.3 cm bladder calculus (B), Large bladder stone on flexible cystoscopy (C) and diagrammatic representation of operative findings (D).
Her past medical history was notable only for a history of COPD. She is an active smoker with a 20 year smoking pack history. She had never undergone any abdominopelvic surgery. She has 3 children who were all delivered via the normal vaginal route without any complications. An intrauterine contraceptive device (IUD) was inserted after the birth of her youngest child 42 years previously which was presumed by the patient to have been expelled spontaneously.
On initial examination she appeared comfortable. Her vital signs were within normal range. Examination of the cardiovascular and respiratory systems was unremarkable. Examination of the abdomen revealed a soft, non-distended abdomen with mild tenderness in the suprapubic area on deep palpation. There were no palpable masses. On pelvic examination she is noted to have a palpable mass in the upper vagina.
Investigations
Baseline blood investigations included a full blood count, renal profile, calcium, phosphate and uric acid levels. She is noted to be anemic with hemoglobin (Hb) of 10.2 g/dL and mean cell volume (MCV) of 74.3 fL. White cell count was within normal range at 6.4 × 103/μL. She has borderline renal impairment with a creatinine (Cr) of 93 μmol/L and eGFR of 51 mL/min. Calcium, phosphate and uric acid levels were all within normal range. Her urine analysis did not show any evidence of active infection.
Plain X-ray KUB revealed a 5.3 cm bladder calculus with no evidence of foreign body (Fig. 1). Flexible cystoscopy confirmed the large bladder calculus in the bladder with a supratrigonal VVF and extension of the calculus into the vaginal fornix and upper vagina (Fig. 1).
Treatment
She underwent rigid cystoscopy with a 23 French rigid cystoscope under general anesthetic. Combined pneumatic and LASER (Holmium: YAG) cystolithotripsy of a large >5 cm intravesical stone was performed with complete fragmentation. A foreign body was identified within the calculus with heavy encrustation. Again, combined approach was employed to completely clear the foreign body of the encrustations, in the bladder as well as in the vagina with exposure of fistulous opening in the bladder (Fig. 2). Foreign body was removed via vaginal route which revealed to be a “Saf-T-Coil” first generation IUD (Fig. 3). Two coils were seen to lie within the bladder, while the rest of it was lying within the vaginal fornix. There was no evidence of vesicouterine connection.
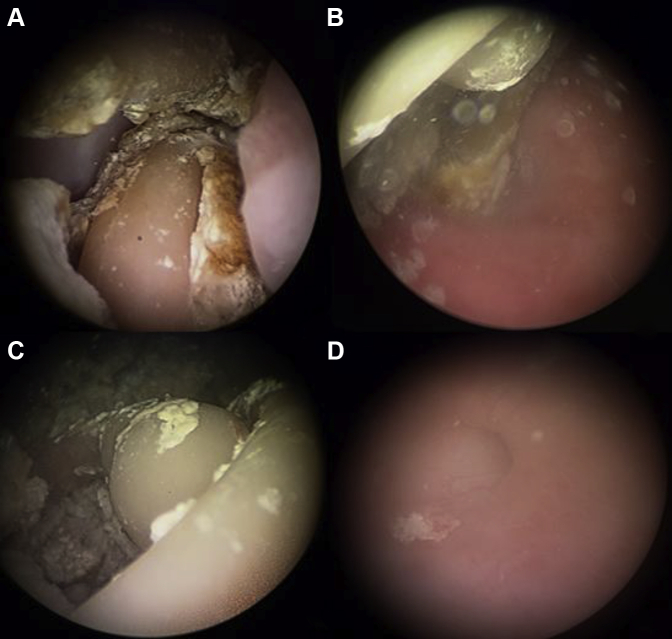
Figure 2.
Heavily encrusted IUD seen after cystolithotripsy (A, B and C) and cystoscopic visualization of fistulous opening after removal of IUD (D).
Figure 3.

Retrieved “Saf-T-Coil”.
Outcome and follow up
A silicone 16 French urethral catheter was placed as form of urinary diversion and patient was referred to gynecology services for management of VVF.
Discussion
VVF is most commonly associated with gynecological surgery in the developed world. The majority of early VVFs occur in association with hysterectomy, while pelvic radiation is the most important cause of delayed fistula formation.
The “Saf-T-Coil” (Julius Schmid Laboratories, Little Falls, New Jersey, USA) IUD was a first generation IUD that entered manufacturing in 1965 and was one of the first inert type plastic IUDs to be commonly used.1 It was also one of the first to adopt the familiar T-shape of IUDs still used today. It was accepted during its time as being generally safe, effective and easy to insert, with low expulsion rates due to its bulky frame. Production was halted in 1982 for economic reasons as newer contraceptive methods gained popularity.
A case report was found involving a migrated “Lippes Loop” with VVF, chronic kidney disease and bladder calculus.2 We have also found two case reports of uterine perforation secondary to a “Saf-T-Coil” IUD; two of these occurred at the time of insertion, while one case presented 30 years post insertion with erosion into the peritoneal cavity and small bowel obstruction.3, 4
Although, intravesical migration of IUD and subsequent calculus formation is extremely uncommon, it can present with voiding symptoms, recurrent UTIs, suprapubic pain and hematuria. Hydronephroureter and pyelonephritis may be present.2
In this case the initiating event may have been migration of IUD eroding supratrigonally in the bladder resulting in vesicovaginal fistula with subsequent encrustation, recurrent UTIs and giant calculus formation. This is perhaps the more likely explanation given the orientation of the IUD within the calculus at time of retrieval.
It is recommended by World Health Organisation (WHO) that dislocated IUDs should be removed because of significant risk of complications.5 Treatment options are different depending on the final location of the migrated IUD. If there is intraperitoneal migration, minimally invasive or an open approach may be employed to deal with the complications as well as to remove the device, whereas in cases of intravesical migration and stone formation, cystolithotripsy of bladder calculus should be done with subsequent removal of IUD.2
Conflict of interest
None.
Acknowledgment
This case report has not been financed by any institution.
References
- 1.Manufacturer halts Saf-T-Coil production. Contracept Technol Update. 1982;3(9):109–110. [PubMed] [Google Scholar]
- 2.Karsmakers R., Weis-Potters A.E., Buijs G., Joustra E.B. Chronic kidney disease after vesico-vaginal stone formation around a migrated intrauterine device. BMJ Case Rep. 2010;2010 doi: 10.1136/bcr.12.2009.2547. pii: bcr1220092547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tacchi D. Uterine perforation by a Saf-T-Coil intrauterine contraceptive device. J Obstet Gynaecol Br Commonw. 1968;75:1176. doi: 10.1111/j.1471-0528.1968.tb02907.x. [DOI] [PubMed] [Google Scholar]
- 4.Brar R., Doddi S., Ramasamy A., Sinha P. A forgotten migrated intrauterine contraceptive device is not always innocent: a case report. Case Rep Med. 2010;2010:3. doi: 10.1155/2010/740642. Article ID 740642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . World Health Organization; Geneva, Switzerland: 1987. Mechanism of Action, Safety and Efficacy of Intrauterine Devices. [PubMed] [Google Scholar]