Abstract
Purpose
This study reports the characteristics of corneal higher order aberrations (HOAs) in eyes with normal topographic pattern using the Pentacam scheimpflug system.
Methods
In this prospective, observational, comparative study, 165 eyes of 97 patients separated into five groups based on corneal topographic patterns were enrolled. All eyes received a comprehensive ophthalmologic examination including corneal tomographic analysis with the Pentacam system. Keratometry, corneal cylinder, and corneal aberrometric data were recorded and analyzed. Root mean square values (RMS) were calculated for corneal HOAs up to the 6th order, total coma, total trefoil, total spherical aberration, total tetrafoil, and higher order astigmatism. Evaluation of these data to discriminate between the five groups was assessed using the analysis of variance test by Generalized Estimation Equation Linear Model.
Results
Corneal HOAs were found to be significantly higher for Asymmetric Bow Tie and Irregular groups than other groups (p = <0.001). RMS of total coma aberration (, , , ) were significantly greater in the Asymmetric Bow Tie pattern than others, and RMS of total Spherical aberration (, ) was significantly higher in the Irregular pattern than other groups (p = <0.001). The results of our study demonstrate that a tendency toward significant higher values of trefoil, tetrafoil, and higher order astigmatism in Irregular pattern (all p < 0.05). Significantly higher amounts of 3rd order RMS in Asymmetric Bow Tie group and 4th to 6th order RMS in Irregular pattern group were other outcomes of our study (p = <0.001).
Conclusions
Based on results in this study, there were a good correlation between corneal topographic pattern and corneal HOAs in normal eyes. These results indicate that the corneal HOAs values are largely determined by the topographic patterns. A larger sample size would perhaps have been beneficial to yield in more accurate outcomes.
Keywords: Topography pattern, Pentacam, Corneal higher-order aberrations
Introduction
Detection of subtle corneal abnormalities or even normal corneas with potential of postoperative visual complications among refractive surgery candidates is important because sometimes patients complain about poor quality of vision even when their visual acuity is 20/20 postoperatively. However, operating on an undetected keratoconic cornea is a major cause of post refractive surgery ectasia.1
Some studies compared higher order aberrations (HOAs) between keratoconic and normal eyes and reported Keratoconus produces significantly higher levels of ocular and corneal aberrations in comparison to normal eyes.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 Based on results of these studies, HOAs can be used to distinguish early Keratoconus from normal and to grade the severity of Keratoconus.16 Additionally, correlation between corneal topographic indices such as irregularity and keratometry with HOAs was demonstrated in a previous study.17 Another study showed corneal HOAs correlate with topographic patterns.18
The purpose of this study was to compare corneal HOAs, measured with the Pentacam scheimpflug system between normal topographic patterns.
Methods
In this prospective, observational, comparative study, 165 eyes of 97 patients, ranging in age from 20 to 35 years old (59 females/38 males) with normal topographic cornea who were scheduled for refractive surgery in Isfahan Persian Eye Clinic were enrolled. The eyes were divided into five differentiated groups based on corneal topographic patterns. We consider the same sample size for all pattern groups.
Classification of sample groups was based on topographic patterns described by Bogan's and colleagues.19 According to this classification, the color-coded topographic maps were grouped into the following patterns: round, oval, symmetric bow tie, asymmetric bow tie, and irregular.
All participants were asked to stop wearing soft contact lenses for at least one week and rigid gas-permeable contact lenses for at least one month before obtaining measurements. Eyes with any ocular pathology such as dry eye, glaucoma, Keratoconus, retinal diseases, systemic conditions such as connective tissue disorders, and history of ocular surgery were excluded. A complete ocular examination including slit-lamp biomicroscopy, cycloplegic refraction, best spectacle distance visual acuity, intra-ocular pressure and dilated fundus examination, and corneal topographic analysis with the Pentacam system (Oculus Optikgerate, Wetzlar, Germany) was performed.
The Oculus Pentacam HR (OCULUS Optikgerate GmbH, Wetzlar, Germany) is a non-invasive system that can provide measurements of corneal HOAs up to the 10th order of the Zernike polynomials which uses a rotating Scheimpflug camera that takes 100 images with 500 measurement points on the anterior and posterior corneal surfaces over a 180-degree rotation. The elevation data from all these images are combined to form a three-dimensional reconstruction of the corneal structure. After processing all this information, the internal software provides a large number of different calculations. Then the corneal elevation profile was automatically converted into corneal wavefront data.
In the current study, the Pentacam software version 6.02r10 was used. All measurements were obtained by an experienced operator using same system and procedure. The patient was asked to blink and then look at the fixation target before each measurement. The examiner adjusted the joystick until appropriate alignment of the scan center on the center of pupil was achieved. The system automatically took 100 images of the cornea within the two-second period. Scans not meeting acceptable criteria (blinks during the scan or other artifacts) according to the Pentacam software indications were repeated. Only measurements with an “ok” reading were included.
The study was approved by the Ethics Committee of Iran University of Medical Sciences, and all experiments conformed to the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants after explaining the purpose of the study.
Statistical analysis
Corneal higher order aberrations were compared for normal topographic pattern groups. The following data were compared between the study groups mean keratometry, corneal astigmatism, and root-mean–square (RMS) of the corneal wavefront. From the 10 order Zernike coefficients measured by the instrument, the following RMS groups were examined: total higher order (all terms included in the third, fourth, fifth, and sixth order); total coma (including , , , and ); vertical coma (); total trefoil (including , , , and ); total spherical aberration (including and ); total tetrafoil (including , , , and ); and higher order astigmatism (including , , , and ). All Zernike coefficients and RMS values were calculated for a pupil diameter of 6.0 mm.
Statistical analysis was performed using the software SPSS version 17.0 for Windows (SPSS, Chicago, IL, USA). All data were expressed as mean ± standard deviation. Normality of all data samples was checked by means of the Kolmogorov–Smirnov test. In this study, the correlation between eyes was low in RMS of HOAs (r = 0.156), so data from both eyes was analyzed. For analysis of variance to comparison between groups, General Linear Model Test was used. P values less than 0.05 were considered statistically significant.
Results
This study included 165 eyes from 97 subjects. Thirty-three eyes in each group were evaluated and analyzed. The demographics data of all groups studied are presented in Table 1.
Table 1.
The demographics data, mean keratometry, and corneal astigmatism in all study groups.
| Round | Oval | Symmetric bow tie | Asymmetric bow tie | Irregular | |
|---|---|---|---|---|---|
| Subject/Eyes | 17/33 | 21/33 | 21/33 | 18/33 | 19/33 |
| Age (mean ± SD) | 26.76 ± 3.26 | 26.39 ± 1.48 | 26.88 ± 1.92 | 27.85 ± 2.22 | 27.69 ± 2.81 |
| Sex (male/female) | 7/11 | 9/12 | 9/12 | 4/14 | 9/10 |
| Mean k | 44.33 ± 1.56 | 43.89 ± 0.97 | 43.25 ± 1.22 | 43.93 ± 1.30 | 43.77 ± 0.94 |
| Corneal astigmatism | 0.573 ± 0.26 | 0.973 ± 0.382 | 2.58 ± 0.82 | 1.69 ± 0.75 | 0.594 ± 0.49 |
According to the qualitative classification system of normal corneal topography based on the Bogan's et al.’s study, we included 33 eyes in each pattern group. There were no statistically significant differences among any of pattern groups for age and sex. The mean k and corneal astigmatism for all eyes was 43.83 ± 1.25 (range 40.1–46.6) and 1.28 ± 0.957 (range 0.0–4.70), respectively. Although there were statistically significant differences in mean keratometric power between groups (p = 0.002), the correlation between K mean and pattern was not significant (p = 0.146).
Corneal astigmatism was 0.573 ± 0.26 D for Round, 0.973 ± 0.382 D for Oval, 2.58 ± 0.82 D for Symmetric Bow Tie, 1.69 ± 0.75 D for Asymmetric Bow Tie, and 0.594 ± 0.49 D for Irregular pattern (Table 1). There were statistically significant differences in mean corneal astigmatism values between topographic pattern groups (p < 0.001). Mean corneal astigmatism in Symmetric and Asymmetric Bow Tie groups was significantly higher than other groups. The difference between Irregular and Round was not significant (p = 0.920). There was a significant correlation between corneal astigmatism and pattern (p < 0.001).
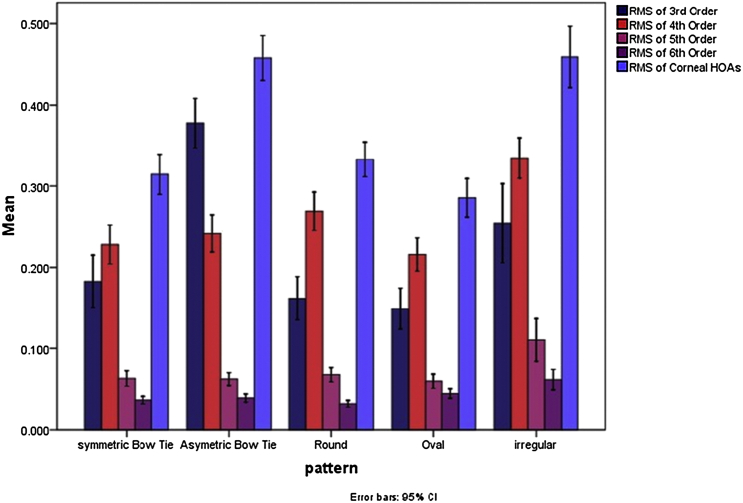
Root-mean–square (RMS) wavefront error values for the higher order (third through sixth order) aberrations were calculated for each study group (Table 2 and Fig. 1).
Table 2.
Root mean square values for the higher order (third through sixth order) aberrations in each study group.
| RMS of 3rd order | RMS of 4th order | RMS of 5th order | RMS of 6th order | |
|---|---|---|---|---|
| Round | 0.162 ± 0.076 | 0.269 ± 0.066 | 0.068 ± 0.025 | 0.032 ± 0.012 |
| Oval | 0.149 ± 0.072 | 0.216 ± 0.058 | 0.0596 ± 0.025 | 0.044 ± 0.017 |
| Symmetrical bow tie | 0.183 ± 0.091 | 0.228 ± 0.067 | 0.063 ± 0.027 | 0.036 ± 0.013 |
| Asymmetrical bow tie | 0.378 ± 0.086 | 0.242 ± 0.064 | 0.062 ± 0.022 | 0.039 ± 0.014 |
| Irregular | 0.254 ± 0.137 | 0.335 ± 0.070 | 0.110 ± 0.074 | 0.062 ± 0.035 |
| Total eyes | 0.225 ± 0.127 | 0.258 ± 0.077 | 0.072 ± 0.044 | 0.043 ± 0.022 |
Root mean square (RMS).
Fig. 1.
Root mean square values for the higher order (third through sixth order) aberrations in each study group.
For the 3rd order RMS, statistically significant differences were found between Asymmetric Bow Tie with others (p < 0.001) and between Irregular pattern compared to other groups (p < 0.05). Regarding the 4th order RMS, statistically significant differences among groups were found between Irregular and others and between Round with Oval (p = 0.02) and Symmetric Bow Tie (p = 0.039). RMS of 5th and 6th order was significantly higher in Irregular pattern group than others (p < 0.001). Also there were significant differences between oval with Round (p < 0.001) and Symmetric Bow Tie (p = 0.021) patterns for RMS of 6th order.
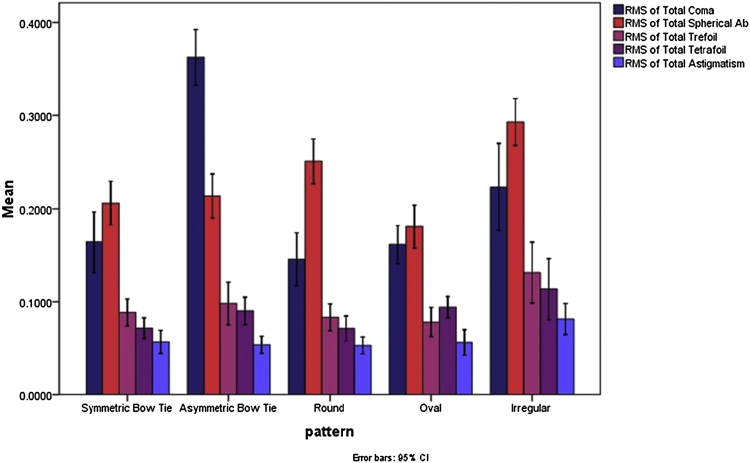
On the other hand, we calculated RMS for higher order total corneal aberrations, total trefoil, total coma, vertical coma, total tetrafoil, total higher order spherical aberration (SA), and total higher order astigmatism (Table 3 and Fig. 2).
Table 3.
Root mean square value for the higher order corneal aberrations (HOA) in each study group.
| RMS of total trefoil | RMS of total coma | RMS of total spherical | RMS of total tetrafoil | RMS of total higher order astigmatism | HOA RMS | |
|---|---|---|---|---|---|---|
| Round | 0.0833 ± 0.040 | 0.145 ± 0.080 | 0.2509 ± 0.067 | 0.0713 ± 0.037 | 0.0533 ± 0.025 | 0.333 ± 0.061 |
| Oval | 0.0782 ± 0.044 | 0.161 ± 0.058 | 0.1806 ± 0.065 | 0.0940 ± 0.032 | 0.0565 ± 0.038 | 0.285 ± 0.067 |
| Symmetrical bow tie | 0.0886 ± 0.040 | 0.164 ± 0.092 | 0.2059 ± 0.066 | 0.0717 ± 0.031 | 0.0570 ± 0.034 | 0.314 ± 0.070 |
| Asymmetrical bow tie | 0.0982 ± 0.064 | 0.363 ± 0.084 | 0.2138 ± 0.066 | 0.0901 ± 0.041 | 0.0540 ± 0.025 | 0.458 ± 0.078 |
| Irregular | 0.1311 ± 0.091 | 0.223 ± 0.132 | 0.2929 ± 0.070 | 0.1135 ± 0.091 | 0.0815 ± 0.046 | 0.459 ± 0.106 |
| Total eyes | 0.0959 ± 0.061 | 0.211 ± 0.122 | 0.2888 ± 0.077 | 0.0882 ± 0.053 | 0.0605 ± 0.036 | 0.3699 ± 0.107 |
Fig. 2.
Root mean square value for the higher order corneal aberrations in each study group.
RMS of total corneal HOAs were found to be significantly higher in the Asymmetric Bow Tie and Irregular pattern groups than others (p < 0.001), but the differences between these two groups was not significant (p = 0.969).
RMS of total coma (especially vertical coma) was significantly higher in the Asymmetric Bow Tie pattern group. RMS of total spherical aberration was significantly higher in the Irregular pattern than in the other groups. Regarding the other group, only the difference between Round and Oval was significant (p = 0.001). RMS of total Astigmatism was significantly higher in the Irregular pattern than in the other groups. The results showed that RMS of trefoil aberrations was significantly higher in Irregular groups compared to other patterns. The differences between Oval and Asymmetric Bow Tie was borderline significant (p = 0.046). Additionally, RMS of total tetrafoil was only significantly higher in Irregular group in comparison to Round and Symmetric Bow Tie pattern. Also differences between Oval with Round (p = 0.002) and Symmetric Bow Tie (p = 0.012) patterns were significant.
The regression between pattern and RMS of HOAs (p = 0.047), total coma (p = 0.02), total SA (p = 0.001), total trefoil (p = 0.05), total tetrafoil (p = 0.003), and total astigmatism (p = 0.01) were significant.
Discussion
The importance of detecting and measuring corneal higher order aberrations is not only essential for Keratoconus evaluation but also before refractive surgery to identify corneas at risk of ectasia and/or to predict HOAs condition postoperatively regarding a corneal pattern.
This study reports the characteristics of corneal HOAs in eyes with normal topographic pattern based on Bogan's classification system. To the best of our knowledge, it is the first to investigate (compare) the corneal HOAs in normal topographic patterns.
Some studies showed that different higher order aberration components increase with the aging process, so we selected patients in the age range of 20–35 years old.20 The relationship between topographic patterns and corneal astigmatism and between topographic pattern and HOAs were established in previous studies.17, 19 These findings were confirmed in our study. According to Kim et al.’s study, the Symmetric and Asymmetric Bow Tie patterns were distributed toward greater amounts of corneal astigmatism.21 These results indicate that the topographic patterns are largely determined by the corneal astigmatic values.
Previous studies have compared ocular and corneal HOAs between normal and keratoconic eyes and have reported that aberrations (especially coma-like aberrations) are significantly higher in keratoconic eyes compared to normal eyes. Additionally, they have concluded that the earliest manifestation of corneal Asymmetric in Keratoconus is vertical.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16
This tendency was also observed in corneas with Asymmetric Bow Tie pattern in our study. In the current study, we found coma-like aberrations were significantly greater in the Asymmetric Bow Tie pattern than in the other groups (Fig. 2).
We also found that RMS of total spherical aberration was significantly higher in the Irregular pattern than other groups. Differences between Round and Oval was significant (p < 0.001). There were not significant differences in SA between other groups (Fig. 1).
Based on Feizi et al.’s study, trefoil and tetrafoil aberrations were not significantly different between Keratoconus and normal eyes. They concluded vertical and horizontal tetrafoil were not significantly correlated with any topographic parameters.17 But the results of our study demonstrate that a tendency toward significant higher values of trefoil and tetrafoil in Irregular pattern. A probable reason for this difference is poor reliability of Pentacam for measuring these particular aberrations.22, 23, 24, 25 Based on previous studies, the Pentacam system exhibited excellent (reasonable) repeatability and reliability for a number of anterior corneal HOAs such as coma and SA; however, for certain aberrations with higher azimuthal frequencies such as trefoil and tetrafoil exhibited poor reliability.25
Significantly higher amounts of 3rd order RMS in the Asymmetric Bow Tie group and 4th to 6th order RMS in the Irregular pattern group were other outcomes of our study (Fig. 1).
The ability to obtain detailed information about the normal corneal topography and their relation to HOAs and visual function offer the promise of improved understanding of corneal surface abnormalities, and better predict visual outcomes of refractive surgery.
Previous studies showed coma and SA typically exhibit the highest magnitude in normal population,26, 27 and some other reported corneal refractive surgery induced optical changes in the HOAs, especially SA and coma.28 It has been established that these corneal aberrations have a more negative impact on visual acuity.29 A strong correlation between visual symptoms and ocular aberrations, such as monocular diplopia with coma and starburst and glare with SA, were established in investigations.28
Having the ability to treat Irregularity in corneal shape correlated with a specific symptomatic HOAs will improve the efficacy and safety of corneal refractive surgery and may reduce the aberrations responsible for the patient's symptoms. Therefore, detection of characteristics of HOAs is important and can be useful in this regard.
Based on results in this study, there was a good correlation between corneal topographic pattern and corneal HOAs in normal eyes. This evidence allowed our research group to develop some hypothesis such as characteristics of corneal HOAs may be predicted from corneal topography patterns or corneal topography pattern can be used as a good predictor of corneal HOAs. For example, an ophthalmologist might predict that an eye with Irregular pattern would probably have higher Spherical aberration, and since Spherical aberration increased post refractive surgery, this eye may have the potential complication related to SA postoperatively such as glare. However, the topographic pattern may not be accurate enough to determine the special aberration value for interpretation.
It is clear from these data that all of the corneal higher order aberrations (3rd order and above) were higher in Asymmetric Bow Tie and Irregular pattern groups. Further quantitative studies of corneal topography should provide more detailed information defining the distinction between normal and pathologic corneas, and the topographic characteristics of normal corneas in various refractive states.
There are several limitations to this study. We evaluated only corneal HOAs because anterior corneal surface is probably the most important refractive interface of the eye due to the large difference in refractive index between air and cornea. This implies that the major source of HOAs is the anterior surface of the cornea. However, because of the compensation generated by the internal aberration, ocular aberration values are more effective on visual function. Future studies should investigate the relationship between corneal topographic parameters and both corneal and ocular HOAs pre- and post refractive surgery in eyes with different refractive status. Another limitation of the present study is that the reliability of corneal wavefront measurements provided by the Pentacam system was not checked simultaneously. More investigations with a larger sample size after solving the reliability problems of this device or by using another validated system would perhaps have been beneficial to yield in a more accurate outcome.
Acknowledgments
We thank the Research Assistant of Rehabilitation College of Iran University of Medical Sciences for funding support.
Footnotes
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Seiler T., Quurke A.W. Iatrogenic keratectasia after LASIK in a case of forme fruste keratoconus. J Cataract Refract Surg. 1998 Jul;24:1007–1009. doi: 10.1016/s0886-3350(98)80057-6. [DOI] [PubMed] [Google Scholar]
- 2.Maeda N., Fujikado T., Kuroda T. Wavefront aberrations measured with Hartmann-Shack sensor in patients with keratoconus. Ophthalmology. 2002 Nov;109:1996–2003. doi: 10.1016/s0161-6420(02)01279-4. [DOI] [PubMed] [Google Scholar]
- 3.Jafri B., Li X., Yang H., Rabinowitz Y.S. Higher order wavefront aberrations and topography in early and suspected keratoconus. J Refract Surg Thorofare NJ. 2007 Oct;23:774–781. doi: 10.3928/1081-597X-20071001-06. 1995. [DOI] [PubMed] [Google Scholar]
- 4.Shah S., Naroo S., Hosking S. Nidek OPD-scan analysis of normal, keratoconic, and penetrating keratoplasty eyes. J Refract Surg Thorofare NJ. 2003 Apr;19:S255–S259. doi: 10.3928/1081-597X-20030302-18. 1995. [DOI] [PubMed] [Google Scholar]
- 5.Barbero S., Marcos S., Merayo-Lloves J., Moreno-Barriuso E. Validation of the estimation of corneal aberrations from videokeratography in keratoconus. J Refract Surg Thorofare NJ. 2002 Jun;18:263–270. doi: 10.3928/1081-597X-20020501-09. 1995. [DOI] [PubMed] [Google Scholar]
- 6.Gobbe M., Guillon M. Corneal wavefront aberration measurements to detect keratoconus patients. Contact Lens Anterior Eye J Br Contact Lens Assoc. 2005 Jun;28:57–66. doi: 10.1016/j.clae.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Jinabhai A., Radhakrishnan H., O'Donnell C. Visual acuity and ocular aberrations with different rigid gas permeable lens fittings in keratoconus. Eye Contact Lens. 2010 Jul;36:233–237. doi: 10.1097/ICL.0b013e3181e52dd1. [DOI] [PubMed] [Google Scholar]
- 8.Kosaki R., Maeda N., Bessho K. Magnitude and orientation of Zernike terms in patients with keratoconus. Invest Ophthalmol Vis Sci. 2007 Jul;48:3062–3068. doi: 10.1167/iovs.06-1285. [DOI] [PubMed] [Google Scholar]
- 9.Lim L., Wei R.H., Chan W.K., Tan D.T.H. Evaluation of higher order ocular aberrations in patients with keratoconus. J Refract Surg Thorofare NJ. 2007 Oct;23:825–828. doi: 10.3928/1081-597X-20071001-13. 1995. [DOI] [PubMed] [Google Scholar]
- 10.Nakagawa T., Maeda N., Kosaki R. Higher-order aberrations due to the posterior corneal surface in patients with keratoconus. Invest Ophthalmol Vis Sci. 2009 Jun;50:2660–2665. doi: 10.1167/iovs.08-2754. [DOI] [PubMed] [Google Scholar]
- 11.Schwiegerling J., Greivenkamp J.E. Using corneal height maps and polynomial decomposition to determine corneal aberrations. Optom Vis Sci Off Publ Am Acad Optom. 1997 Nov;74:906–916. doi: 10.1097/00006324-199711000-00024. [DOI] [PubMed] [Google Scholar]
- 12.Gordon-Shaag A., Millodot M., Ifrah R., Shneor E. Aberrations and topography in normal, keratoconus-suspect, and keratoconic eyes. Optom Vis Sci Off Publ Am Acad Optom. 2012 Apr;89:411–418. doi: 10.1097/OPX.0b013e318249d727. [DOI] [PubMed] [Google Scholar]
- 13.Bühren J., Kühne C., Kohnen T. Defining subclinical keratoconus using corneal first-surface higher-order aberrations. Am J Ophthalmol. 2007 Mar;143:381–389. doi: 10.1016/j.ajo.2006.11.062. [DOI] [PubMed] [Google Scholar]
- 14.Nilforoushan M.-R., Speaker M., Marmor M. Comparative evaluation of refractive surgery candidates with Placido topography, Orbscan II, Pentacam, and wavefront analysis. J Cataract Refract Surg. 2008 Apr;34:623–631. doi: 10.1016/j.jcrs.2007.11.054. [DOI] [PubMed] [Google Scholar]
- 15.Schlegel Z., Hoang-Xuan T., Gatinel D. Comparison of and correlation between anterior and posterior corneal elevation maps in normal eyes and keratoconus-suspect eyes. J Cataract Refract Surg. 2008 May;34:789–795. doi: 10.1016/j.jcrs.2007.12.036. [DOI] [PubMed] [Google Scholar]
- 16.Alió J.L., Shabayek M.H. Corneal higher order aberrations: a method to grade keratoconus. J Refract Surg Thorofare NJ. 2006 Jun;22:539–545. doi: 10.3928/1081-597X-20060601-05. 1995. [DOI] [PubMed] [Google Scholar]
- 17.Feizi S., Einollahi B., Raminkhoo A., Salehirad S. Correlation between corneal topographic indices and higher-order aberrations in keratoconus. J Ophthalmic Vis Res. 2013 Apr;8:113–118. [PMC free article] [PubMed] [Google Scholar]
- 18.McCormick G.J., Porter J., Cox I.G., MacRae S. Higher-order aberrations in eyes with irregular corneas after laser refractive surgery. Ophthalmology. 2005 Oct;112:1699–1709. doi: 10.1016/j.ophtha.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 19.Bogan S.J., Waring G.O., Ibrahim O. Classification of normal corneal topography based on computer-assisted videokeratography. Arch Ophthalmol Chic Ill. 1990 Jul;108:945–949. doi: 10.1001/archopht.1990.01070090047037. 1960. [DOI] [PubMed] [Google Scholar]
- 20.Hashemi H., Khabazkhoob M., Jafarzadehpur E. Higher order aberrations in a normal adult population. J Curr Ophthalmol. 2015 Sep;27:115–124. doi: 10.1016/j.joco.2015.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim H.C., Chang S.D. Relationship between topographic patterns and corneal astigmatism in Korean adults. Korean J Ophthalmol KJO. 2003 Dec;17:91–96. doi: 10.3341/kjo.2003.17.2.91. [DOI] [PubMed] [Google Scholar]
- 22.He J.C., Watanabe R., Gwiazda J. The accuracy of three optical systems in measuring corneal wavefront aberrations. Invest Ophthalmol Vis Sci. 2006 May 1;47(13) 562–562. [Google Scholar]
- 23.Sideroudi H., Labiris G., Giarmoulakis A. Repeatability, reliability and reproducibility of posterior curvature and wavefront aberrations in keratoconic and cross-linked corneas. Clin Exp Optom. 2013 Nov;96:547–556. doi: 10.1111/cxo.12044. [DOI] [PubMed] [Google Scholar]
- 24.Piñero D.P., Saenz González C., Alió J.L. Intraobserver and interobserver repeatability of curvature and aberrometric measurements of the posterior corneal surface in normal eyes using Scheimpflug photography. J Cataract Refract Surg. 2009 Jan;35:113–120. doi: 10.1016/j.jcrs.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 25.Read S.A., Collins M.J., Iskander D.R., Davis B.A. Corneal topography with Scheimpflug imaging and videokeratography: comparative study of normal eyes. J Cataract Refract Surg. 2009 Jun;35:1072–1081. doi: 10.1016/j.jcrs.2009.01.020. [DOI] [PubMed] [Google Scholar]
- 26.Artal P., Guirao A., Berrio E., Williams D.R. Compensation of corneal aberrations by the internal optics in the human eye. J Vis. 2001;1:1–8. doi: 10.1167/1.1.1. [DOI] [PubMed] [Google Scholar]
- 27.Wang L., Dai E., Koch D.D., Nathoo A. Optical aberrations of the human anterior cornea. J Cataract Refract Surg. 2003 Aug;29:1514–1521. doi: 10.1016/s0886-3350(03)00467-x. [DOI] [PubMed] [Google Scholar]
- 28.Chalita M.R., Xu M., Krueger R.R. Correlation of aberrations with visual symptoms using wavefront analysis in eyes after laser in situ keratomileusis. J Refract Surg Thorofare NJ. 2003 Dec;19:S682–S686. doi: 10.3928/1081-597X-20031101-13. 1995. [DOI] [PubMed] [Google Scholar]
- 29.Applegate R.A., Sarver E.J., Khemsara V. Are all aberrations equal? J Refract Surg Thorofare NJ. 2002 Oct;18:S556–S562. doi: 10.3928/1081-597X-20020901-12. 1995. [DOI] [PubMed] [Google Scholar]