Abstract
Purpose
To report a case of cytomegalovirus (CMV) retinitis in an immunocompetent adult patient.
Methods
A 61-year-old woman with proven CMV retinitis and no evidence of HIV or other underlying immunodeficiencies was referred.
Results
She was referred with history of recent right eye visual loss. In fundus examination, she had signs of retinal vasculitis. After initial examination, she was found to have CMV retinitis documented by polymerase chain reaction (PCR) analysis of vitreous sample. She had neither underlying risk factor in any assessed work-up nor any concomitant disease in 10 months follow-up. She received intravitreal ganciclovir with good response to treatment.
Conclusion
Ophthalmologists should take into account infectious causes of retinal vasculitis before approaching anti-inflammatory or anti-VEGF therapy.
Keywords: Cytomegalovirus, Immunocompetency, Retinitis
Introduction
Most cases of Cytomegalovirus (CMV) retinitis are reported in acquired immunodeficiency syndrome (AIDS) patients.1 It can also affect other immunocompromised patients.1 Few cases are reported in healthy individuals.1 Here we present a documented case of CMV retinitis in an otherwise healthy patient.
Case report
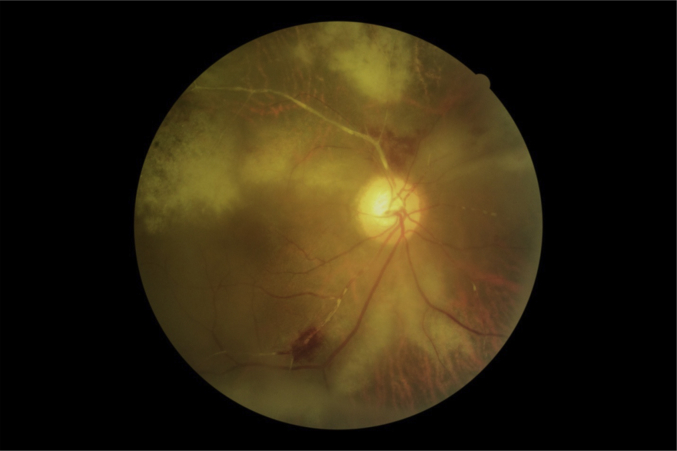
A 61-year-old woman was referred to our clinic with a 1-month history of decreased vision in her right eye. Her best corrected visual acuity was 4/20 in her right eye and hand motion in the left eye. Examination of her right eye revealed fine keratic precipitates, +1 aqueous cells, mild vitritis, patches of hemorrhagic retinitis with vessel segmentation, and perivascular sheathing along arcades with extension to fovea (Fig. 1). There were few pigments in vitreous. In the left eye, the patient had an old standing inferior rhegmatogenous retinal detachment (RRD) (Figs. 2 and 3), optic disc pallor and occluded vessels. Six months before her referral to our hospital, she had received three injections of intravitreal bevacizumab (IVB) in her left eye with diagnosis of branch retinal vein occlusion (BRVO). She had no history of systemic or ocular disease nor any drug consumption.
Fig. 1.
CMV retinitis (OD) at baseline.
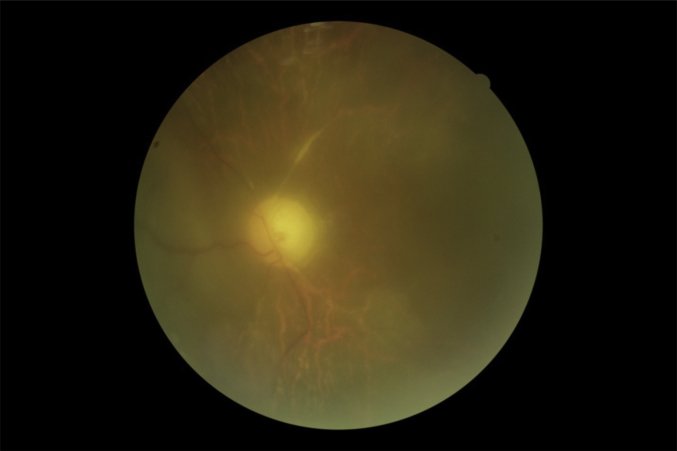
Fig. 2.
Left eye fundus view showing disc pallor and occluded vessels.
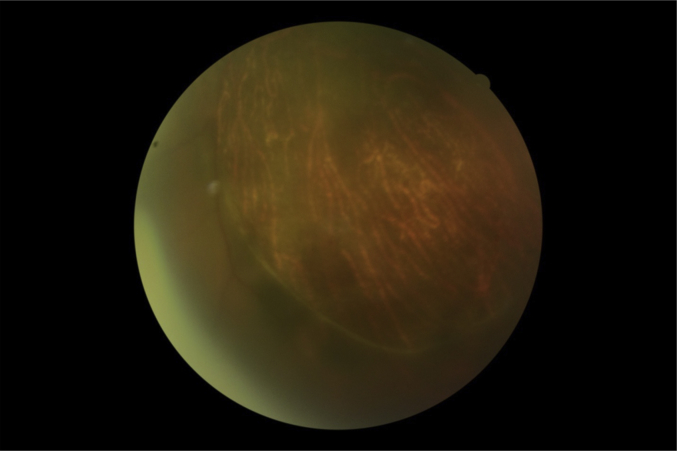
Fig. 3.
Left eye inferior detachment.
She had been visited by other ophthalmologists and was supposed to have retinal vaso-occlusive disease. Major neck vessels were evaluated by doppler sonography to rule out embolic obstruction of retinal vessels. The vessels were normal. They consulted us for continuing treatment with IVB injection.
Because of atypical feature of fundus, we suspected other etiologies of retinal vasculitis. Complete Blood Count (CBC), Erythrocyte Sedimentation Rate (ESR), Venereal Disease Research Laboratory (VDRL), Fluorescent Treponemal Antibody Absorption (FTA-ABS), Purified Protein Derivative (PPD), Anti Nuclear Antibodies (ANA), Rheumatoid Factor (RF), Antiphospholipid, Anti Converting Enzyme (ACE), chest X-ray, anti-HIV antibody, and PCR of vitreous sample for CMV, Herpes Simplex Virus (HSV), Varicella Zoster Virus (VZV) were the laboratory tests requested. They were all normal except for a high concentration of CMV DNA in vitreous PCR (7,000,000 copy/ml) (QS-RGQ kit by Qiagen company, Germany). PCR was negative for HSV and VZV DNA. Patient's CD4 count was also normal (950 cells/mm3). We requested an infectious and internal specialist consultation with suspicion of an underlying immunodeficiency, malignancy, or rheumatologic disorder (especially behcet's disease), but all the work-ups including pathergy test and HLA-B51 were negative.
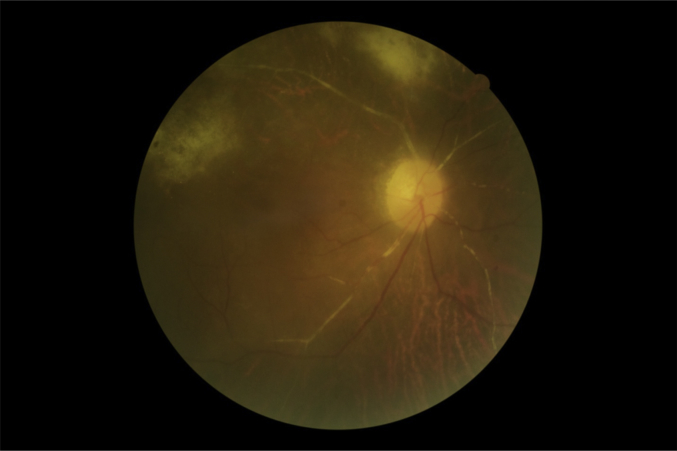
We administered intravitreal ganciclovir (2 mg) twice per week as the loading dose for 2 weeks and then once per week. Also oral valganciclovir (900 mg, BID) was prescribed. After 4 sessions of injection, the patient had substantial subjective improvement in VA. Her BCVA improved to 8/20, and patches of retinitis began to fade from the macula (Fig. 4). We continued weekly injections for 2 months until resolution of retinitis.
Fig. 4.
Fundus (OD) view after 4sessions of intravitreal gancyclovir in 2 weeks.
Patient was offered RD surgery on her left eye, but she refused to do it. Ten months after treatment, she had no new sign of CMV reactivation.
Discussion
CMV infection is common worldwide. It is estimated that 40–100% of people are seropositive until the 4th decade of life.2 Following primary infection virus spreads hematogenously and can infect the retina.3 CMV retinitis is the most common opportunistic viral infection in HIV patients.4 It occurs usually as CD4 count decreases below 50/mm3.4 It is also seen in immunocompromised patients like lymphoma, acute leukemia, and organ transplantation patients.5
It is quite unlikely to encounter CMV retinitis in immunocompetent patients. There are few reports of CMV retinitis in otherwise healthy patients. Gupta S et al6 reported nine cases that were immunocompetent at the time of diagnosis. Alaa Radwan et al5 also reported 2 cases of CMV retinitis that were immunocompetent. In most reports, patients were limited to those who had undergone intravitreal injection of corticosteroids.7, 8, 9, 10, 11 The cause is attributed to the local immunosuppression caused by intraocular injection.1, 12
We have followed our patient for more than 10 months and performed all the necessary laboratory tests, and no predisposing factor was found.
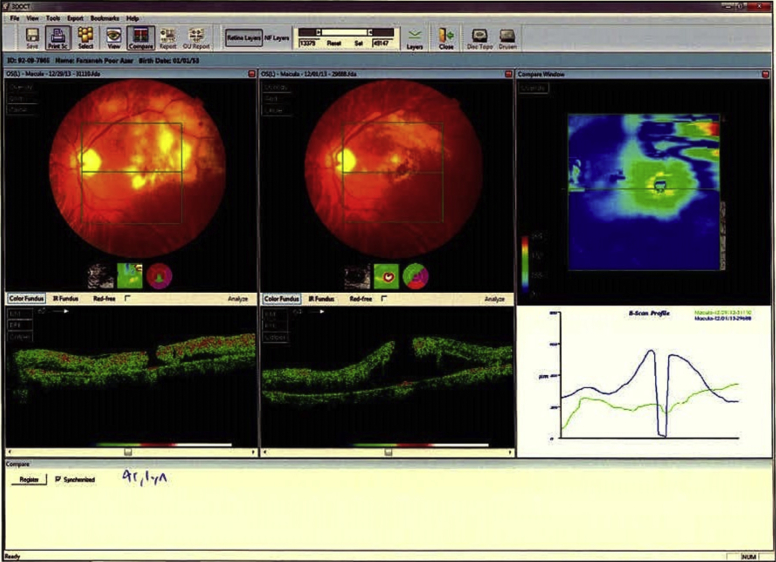
We did not perform diagnostic sampling of the left eye vitreous, but fundus occluded vessels (Fig. 2) and OCT picture of this eye before her referral to our hospital (Fig. 5) may propose prior CMV retinitis in the left eye that has lead to RRD. Retinal detachment may occur in up to 24% of CMV retinitis patients.13
Fig. 5.
OCT of patient's left eye 6 months before involvement of right eye.
Most reports of successful treatment were in HIV positive or immunocompromised patients. Induction and maintenance therapy with intravenous ganciclovir, foscarnet and cidofovir is efficacious but systemic side effects limit their use. Oral valganciclovir is also effective with considerably less side effects. Intravitreal injection of ganciclovir or cidofovir is an effective alternative treatment that can bypass systemic side effects with the same efficacy as systemic drugs. If recovery of the patient's immune system is not possible, anti-CMV therapy should be continued.14, 15
Footnotes
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Radwan Alaa, Metzinger Jamie Lynne. Cytomegalovirus retinitis in immunocompetent patients: case reports and literature review. Ocul Immunol Inflamm. 2013;21:324–328. doi: 10.3109/09273948.2013.786095. [DOI] [PubMed] [Google Scholar]
- 2.Krech U. Complement-fixing antibodies against cytomegalovirus in different parts of the world. Bull World Health Organ. 1973;49:103–106. [PMC free article] [PubMed] [Google Scholar]
- 3.Lopez-Contreras J., Ris J., Domingo P. Disseminated cytomegalovirus infection in an immunocompetent adult successfully treated with ganciclovir. Scand J Infect Dis. 1995;27:523–525. doi: 10.3109/00365549509047059. [DOI] [PubMed] [Google Scholar]
- 4.Jabs D.A. Ocular manifestations of HIV infection. Trans Am Ophthalmol Soc. 1995;93:62383. [PMC free article] [PubMed] [Google Scholar]
- 5.Carlstrom G. Virologic studies on cytomegalic inclusion disease. Acta Paediatr Scand. 1965;54:17–22. doi: 10.1111/j.1651-2227.1965.tb06341.x. [DOI] [PubMed] [Google Scholar]
- 6.Gupta Seema, Vemulakonda G.A. Cytomegalovirus retinitis in the absence of AIDS. Can J Ophthalmol. APRIL 2013;48 doi: 10.1016/j.jcjo.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Miyamoto K., Hiroshiba N., Tsujikawa A. In vivo demonstration of increased leukocyte entrapment in retinal microcirculation of diabetic rats. Invest Ophthalmol Vis Sci. 1998;39:2190–2194. [PubMed] [Google Scholar]
- 8.Saidel M.A., Berreen J., Margolis T.P. Cytomegalovirus retinitis after intravitreous triamcinolone in an immunocompetent patient. Am J Ophthalmol. 2005;140:1141–1143. doi: 10.1016/j.ajo.2005.06.058. [DOI] [PubMed] [Google Scholar]
- 9.Vertes D., Snyers B., De Potter P. Cytomegalovirus retinitis after low-dose intravitreous triamcinolone acetonide in an immunocompetent patient: a warning for the widespread use of intravitreous corticosteroids. Int Ophthalmol. 2010;30:595–597. doi: 10.1007/s10792-010-9404-x. [DOI] [PubMed] [Google Scholar]
- 10.Delyfer M.N., Rougier M.B., Hubschman J.P. Cytomegalovirus retinitis following intravitreal injection of triamcinolone: report of two cases. Acta Ophthalmol Scand. 2007;85:681–683. doi: 10.1111/j.1600-0420.2007.00915.x. [DOI] [PubMed] [Google Scholar]
- 11.Sekiryu T., Iida T., Kaneko H. Cytomegalovirus retinitis after intravitreal triamcinolone acetonide in an immunocompetent patient. Jpn J Ophthalmol. 2008;52:414–416. doi: 10.1007/s10384-008-0576-0. [DOI] [PubMed] [Google Scholar]
- 12.Britt W. Manifestations of human cytomegalovirus infection: proposed mechanisms of acute and chronic disease. Curr Top Microbiol Immunol. 2008;325:417–470. doi: 10.1007/978-3-540-77349-8_23. [DOI] [PubMed] [Google Scholar]
- 13.Wong John X., Wong Elizabeth P., Teoh Stephen C. BMC Ophthalmol. 2014;14:150. doi: 10.1186/1471-2415-14-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henderly D.E., Freeman W.R., Causey D.M., Rao N.A. Cytomegalovirus retinitis and response to therapy with ganciclovir. Ophthalmology. 1987;94:425–434. doi: 10.1016/s0161-6420(87)33454-2. [DOI] [PubMed] [Google Scholar]
- 15.Lowance D., Neumayer H.H., Legendre C.M. Valacyclovir for the prevention of cytomegalovirus disease after renal transplantation. N Engl J Med. 1999;340:1462–1470. doi: 10.1056/NEJM199905133401903. International Valacyclovir Cytomegalovirus Prophylaxis Transplantation Study Group. [DOI] [PubMed] [Google Scholar]