Abstract
Purpose
To present an overview on ultra-wide-field imaging in diabetic retinopathy.
Methods
A comprehensive search of the pubmed database was performed using the search terms of “ultra-wide-field imaging”, “ultra-wide-field fluorescein angiography” and “diabetic retinopathy”. The relevant original articles were reviewed.
Results
New advances in ultra-wide-field imaging allow for precise measurements of the peripheral retinal lesions. A consistent finding amongst these articles was that ultra-wide-field imaging improved detection of peripheral lesion. There was discordance among the studies, however, on the correlation between peripheral diabetic lesions and diabetic macular edema.
Conclusions
Visualization of the peripheral retina using ultra-wide-field imaging improves diagnosis and classification of diabetic retinopathy. Additional studies are needed to better define the association of peripheral diabetic lesions with diabetic macular edema.
Keywords: Ultra-wide-field imaging, Diabetic retinopathy, Diabetic macular edema, Fluorescein angiography
Introduction
Since the introduction of human flash fundus photography in 1886, significant advances have occurred in the field of fundus imaging. Traditional fundus cameras take the images from the posterior pole (the macula and optic nerve), covering a 20–50 degree of field of view (Fig. 1). This part of fundus is the place for the most important ocular diseases including macular degeneration, glaucoma, and optic neuropathy. In addition, the images obtained from the optic nerve and macula, have been routinely used for the diagnosis, management and follow up of retinal vascular occlusions and diabetic retinopathy. We present a brief review on the utility of the ultra-wide-field imaging in the management of diabetic retinopathy. The relevant articles were extracted following a comprehensive search of the pubmed database using the search terms; “ultra-wide-field imaging”, “ultra-wide-field fluorescein angiography” and “diabetic retinopathy”.
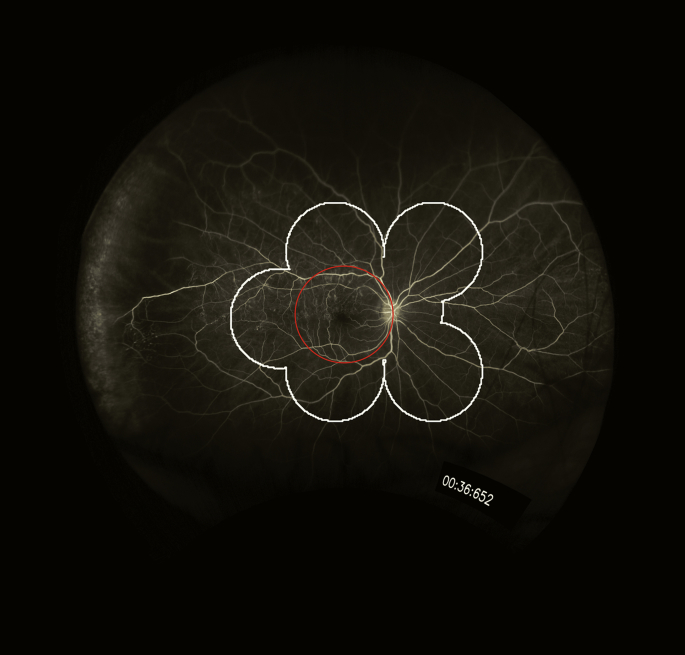
Fig. 1.
Central/axial ultra-wild-field fluorescein angiography image obtained with Optos instrument from a patient with superotemporal branch retinal vein occlusion. Red circle shows a 30° image centered on the macula, the white line delineates the field covered by a montage of 7 field ETDRS image. With a central 30° and 7 field montage image, the areas of non-perfusion in the temporal periphery remain undetected.
Single-field versus wide-field imaging
Single-field fundus photography has been used to detect retinal and optic nerve disease whose primary site of involvement is the posterior pole. The advantages of single-field fundus photography are largely related to convenience to the patient, requiring less time, less light exposure, and in many cases no need for mydriasis. A report by the American Academy of Ophthalmology in 2004 noted that there is a sufficient level of evidence to suggest single-field fundus photography as a screening tool for diabetic retinopathy to identify patients with retinopathy for referral for ophthalmic evaluation and management.1 Non-mydriatic retinal photographs have been shown to allow easy, reliable and reproducible imaging of the optic nerve and retina in non-ophthalmologic settings such as the emergency department.2
Wide-field images can be obtained by three methods; creating montage images, using a special lens with a traditional fundus camera and using a specially-designed wide-angle camera. Montage image, that is a combination of 30-degree images, visualizes about 75 degrees of retina. Early Treatment Diabetic Retinopathy Study (ETDRS) group introduced the stereoscopic color fundus photography in 7 standard fields as the gold standard for the detection and classification of diabetic retinopathy.3 Although 7-field photography is a reliable method for assessment of diabetic retinopathy, it is a time-consuming examination requiring skilled photographers and pharmacological pupil dilation. Consequently, other modalities including 2-field 45° retinal photographs (1 macular-centered field and 1 disc/nasal field), and non-mydriatic cameras were evaluated as user-friendly alternatives to standard 7-filed imaging.4
Pomerantzeff developed the first wide-angle camera system, known as the Equator-Plus camera, in 1975. He used a contact lens and fiber optic scleral transillumination to take fundus images up to 148°.5 The Staurenghi lens is a contact lens system that provides a 5-fold increase (150°) in the fundus fields of view. Clarity Medical Systems introduced the Retcam contact imaging system that gives a maximum field of view of 130°. This technology utilizes a portable camera with a fiberoptic cable light source connected to a computer and is particularly useful for the imaging of pediatric patients.
The Heidelberg Spectralis non-contact ultra-wide-field module offers a wide-field of view of 120° with a scanning laser ophthalmoscopy. Optos (Optos, Dunfermline, United Kingdom) introduced retinal imaging with non-contact scanning laser technology to take the ultra-wide field images. The 200° field of view of the Optos images covers 82% of the retinal surface (compared to 15% for the 45° images). A recent study comparing these two systems showed that on a single non-steered image, the Optos covers a significantly larger total retinal surface area. The Optos images show a wider view of the retina temporally and nasally, however, the Heidelberg Spectralis images show the superior and inferior retinal vasculature more peripherally and overall, the images from Spectralis system seemed to have less peripheral distortion.6 These initial comparative studies were performed using the Optos 200Tx and not with the newer Optos California device which purports to provide better visualization of the inferior and superior periphery as well as new software for stereographic projection to address peripheral distortion.
Ultra-wide-filed versus montage ultra-wide-field imaging
Despite a wide field of view achieved by the Optos optomap images, a small but important part of the peripheral retina may be obscured in the axial images, particularly in the vertical meridian as noted previously. This may be due to the inherent limitation in the imaging of the peripheral retina, obscuration by the lids or pupil, or a combination thereof. Consequently, Optos developed a special software to combine the axial images with those obtained with steering to different gazes. This montage image covers the entire field of the retina (Fig. 2). Using this software, Singer et al7 evaluated the extent of the peripheral retinal vasculature in normal fluorescein angiography (FA) images and provided the normative data as a potential reference for future studies. They found significant difference in distance from the optic disc to the periphery based on the quadrant (with temporal being larger than inferior being larger than superior being larger than nasal) and age (shorter in older individuals). The stereographic projection software is also able to address the problem of the peripheral non-linear warp and difference in the size of the measurements in relation to the angle of view. Thus, the lesion areas can be calculated in anatomically correct physical units.8
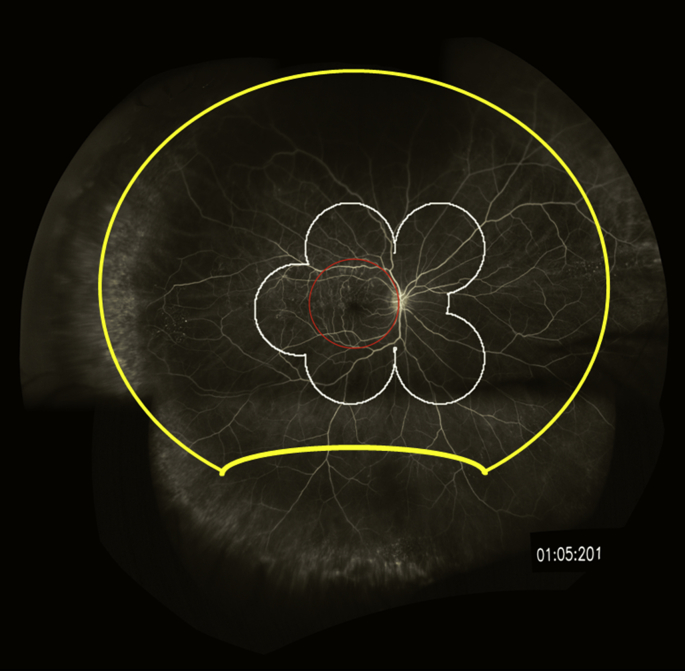
Fig. 2.
A montage ultra-wild-field fluorescein angiography of a central/axial image with images steered inferiorly, temporally and nasally, from the same patient shown in Fig. 1. Yellow line shows the border of the central/axial image. The montage allows more detailed evaluation of the peripheral vasculature in all steered quadrants.
Ultra-wide-field imaging in diabetic retinopathy
Visualization of the peripheral retina using ultra-wide-field imaging has led to new era in the assessment of diabetic retinopathy. Several studies evaluated the utility of the ultra-wide-field imaging in grading diabetic retinopathy. Price et al9 compared diabetic retinopathy severity grading between Optomap ultra-wide-field images and an ETDRS seven-standard field view. Although severity grades were identical in 85% of the images and within one severity level in 100% of the images, 19% of the images were assigned a higher retinopathy level in the ultra-wide-field view compared to the ETDRS seven-field view. Similarly, Weiss et al10 showed 3.9 times more non-perfusion, 1.9 times more neovascularization, and 3.8 times more panretinal photocoagulation scars in the ultra-wide-field FA images view compared to the 7-standard field ETDRS images. They reported that ultra-wide-field FA demonstrated retinal pathology (including non-perfusion and neovascularization) not evident in a 7-standard field overly in 10% of eyes. Talks et al11 showed that Optomap ultra-wide-field images detected approximately 30% more peripheral neovascularization than standard two-field imaging in patients referred from a UK diabetic retinopathy screening service. Silva et al12 reported that diabetic retinopathy severity differs in 20% of eyes when comparing ultra-wild-field imaging and ETDRS 7-standard field images. They showed that the additional peripheral lesions identified by ultra-wild-field images resulted in a more severe assessment of diabetic retinopathy (DR) in 10% of eyes than was suggested by the lesions within the ETDRS fields. Silva et al13 evaluated the ultra-wild-field images to correlate the diabetic retinopathy progression with the predominantly peripheral lesions. Predominantly peripheral lesions were defined as hemorrhages, microaneurysms, venous beading, intraretinal microvascular abnormalities, and new vessels elsewhere with more than 50% of the graded lesion located outside the ETDRS field in each of the 5 extended fields. They found that the presence and increasing extent of predominantly peripheral lesions were associated with increased risk of progression of the diabetic retinopathy (i.e. a 4.7-fold increased risk for progression to proliferative diabetic retinopathy) over 4 years, independent of baseline diabetic retinopathy severity and HbA1c levels.
Recent studies assessed the role of ultra-wide-field FA imaging in eyes with diabetic macular edema. Wessel et al14 reported a significant correlation between diabetic macular edema and peripheral retinal ischemia in the ultra-wide-field FA images. They found that eyes with retinal ischemia had 3.75 times increased odds of having macular edema compared with those without retinal ischemia. Patel et al15 reported a correlation between recalcitrant diabetic macular edema with larger areas of retinal non-perfusion in ultra-wide-field FA and greater severity of diabetic retinopathy. Sim et al16 evaluated the association between peripheral retinal ischemia in ultra-wide-field FA images and central ischemia in diabetic retinopathy. They observed moderate correlations between the peripheral ischemic index and foveal avascular zone area, and between the peripheral leakage index and foveal avascular zone area. Oliver and Schwartz17 observed an association of late peripheral vessel leakage in ultra-wide-field FA images with focal diabetic macular edema. In contrast to the above-mentioned studies, Silva et al18 did not find an association between clinically significant diabetic macular edema and non-perfusion area and non-perfusion index. They also assessed the association of predominantly peripheral lesions in ultra-wide-field FA images of eyes with diabetic retinopathy and severity of diabetic retinopathy. Presence of predominantly peripheral lesions was associated with increased non-perfusion area and non-perfusion index.
Few studies evaluated ultra-wide-field FA-guided targeted laser photocoagulation of the peripheral non-perfusion in eyes with diabetic retinopathy. Reddy et al19 reported 2 patients with proliferative diabetic retinopathy in which targeted retinal photocoagulation resulted in regression of retinal neovascularization. Muqit et al20 assessed the effect of single-session targeted laser photocoagulation guided by ultra-wide-field FA in 28 eyes. At 24 weeks, complete disease regression was found in 37% and additional panretinal laser photocoagulation was planned for active proliferative diabetic retinopathy in 30%.
Future directions
Future researches may further elucidate the association of peripheral diabetic lesions with the stage of diabetic retinopathy and macular edema. The relationship between the presence and extent peripheral non-perfusion with different types of diabetic macular edema (focal versus diffuse and acute versus chronic) may also be a topic of further study. This is especially important for the eyes with chronic persistent macular edema. Varying results have been reported after laser photocoagulation of the ischemic area in eyes with retinal vein occlusion and diabetic retinopathy.19, 20, 21, 22 Additional well-designed studies are needed to show the role of ultra-wide-field-guided peripheral laser photocoagulation in diabetic macular edema.
Automated detection of diabetic retinopathy using standard fundus photography has been evaluated before with high sensitivity and specificity for posterior lesions.23 Future studies may focus on the automated detection of the peripheral lesions on the ultra-wide-field images as well.
Ultra-wild-field imaging improves the detection of the peripheral diabetic retinopathy lesions. Diabetic Retinopathy Research Network protocol AA aims to evaluate the association of the peripheral findings on ultra-wide-field color and FA images with the progression of the diabetic retinopathy.24 The study results are expected to be available in 2020.
Footnotes
Financial interest: Dr. Sadda is a consultant for Carl Zeiss Meditec, Optos, Allergan, Genentech, Alcon, Novartis and Roche. He receives research funding from Carl Zeiss Meditec, Optos, Allergan and Genentech. He also receives honoraria from Carl Zeiss Meditec, Optos and Allergan. Other authors have no financial interest.
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Williams G.A., Scott I.U., Haller J.A., Maguire A.M., Marcus D., McDonald H.R. Single-field fundus photography for diabetic retinopathy screening: a report by the American Academy of Ophthalmology. Ophthalmology. 2004;111:1055–1062. doi: 10.1016/j.ophtha.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Early Treatment Diabetic Retinopathy Study Research Group Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification. ETDRS report no. 10. Ophthalmology. 1991;98:786–806. [PubMed] [Google Scholar]
- 3.Pérez M.A., Bruce B.B., Newman N.J., Biousse V. The use of retinal photography in nonophthalmic settings and its potential for neurology. Neurologist. 2012;18:350–355. doi: 10.1097/NRL.0b013e318272f7d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoenfeld E.R., Greene J.M., Wu S.Y., O'Leary E., Forte F., Leske M.C. Recruiting participants for community-based research: the diabetic retinopathy awareness program. Ann Epidemiol. 2000;10:432–440. doi: 10.1016/s1047-2797(00)00067-3. [DOI] [PubMed] [Google Scholar]
- 5.Pomerantzeff O. Equator-plus camera. Invest Ophthalmol. 1975;14:401–406. [PubMed] [Google Scholar]
- 6.MT1 Witmer, Parlitsis G., Patel S., Kiss S. Comparison of ultra-widefield fluorescein angiography with the Heidelberg Spectralis(®) noncontact ultra-widefield module versus the Optos(®) Optomap(®) Clin Ophthalmol. 2013;7:389–394. doi: 10.2147/OPTH.S41731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singer M., Sagong M., van Hemert J., Kuehlewein L., Bell D., Sadda S.R. Ultra-widefield imaging of the peripheral retinal vasculature in normal subjects. Ophthalmology. 2016;123(5):1053–1059. doi: 10.1016/j.ophtha.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 8.Tan C.S., Chew M.C., van Hemert J., Singer M.A., Bell D., Sadda S.R. Measuring the precise area of peripheral retinal non-perfusion using ultra-widefield imaging and its correlation with the ischaemic index. Br J Ophthalmol. 2016;100:235–239. doi: 10.1136/bjophthalmol-2015-306652. [DOI] [PubMed] [Google Scholar]
- 9.Price L.D., Au S., Chong N.V. Optomap ultrawide field imaging identifies additional retinal abnormalities in patients with diabetic retinopathy. Clin Ophthalmol. 2015;9:527–531. doi: 10.2147/OPTH.S79448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wessel M.M., Aaker G.D., Parlitsis G., Cho M., D'Amico D.J., Kiss S. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 2012;32:785–791. doi: 10.1097/IAE.0b013e3182278b64. [DOI] [PubMed] [Google Scholar]
- 11.Talks S.J., Manjunath V., Steel D.H., Peto T., Taylor R. New vessels detected on wide-field imaging compared to two-field and seven-field imaging: implications for diabetic retinopathy screening image analysis. Br J Ophthalmol. 2015;99:1606–1609. doi: 10.1136/bjophthalmol-2015-306719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silva P.S., Cavallerano J.D., Sun J.K., Soliman A.Z., Aiello L.M., Aiello L.P. Peripheral lesions identified by mydriatic ultrawide field imaging: distribution and potential impact on diabetic retinopathy severity. Ophthalmology. 2013;120:2587–2595. doi: 10.1016/j.ophtha.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Silva P.S., Cavallerano J.D., Haddad N.M. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 2015;122:949–956. doi: 10.1016/j.ophtha.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Wessel M.M., Nair N., Aaker G.D., Ehrlich J.R., D'Amico D.J., Kiss S. Peripheral retinal ischaemia, as evaluated by ultra-widefield fluorescein angiography, is associated with diabetic macular oedema. Br J Ophthalmol. 2012;96:694–698. doi: 10.1136/bjophthalmol-2011-300774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patel R.D., Messner L.V., Teitelbaum B., Michel K.A., Hariprasad S.M. Characterization of ischemic index using ultra-widefield fluorescein angiography in patients with focal and diffuse recalcitrant diabetic macular edema. Am J Ophthalmol. 2013;155 doi: 10.1016/j.ajo.2013.01.007. 1038–1044.e2. [DOI] [PubMed] [Google Scholar]
- 16.Sim D.A., Keane P.A., Rajendram R. Patterns of peripheral retinal and central macula ischemia in diabetic retinopathy as evaluated by ultra-widefield fluorescein angiography. Am J Ophthalmol. 2014;158 doi: 10.1016/j.ajo.2014.03.009. 144–153.e1. [DOI] [PubMed] [Google Scholar]
- 17.Oliver S.C., Schwartz S.D. Peripheral vessel leakage (PVL): a new angiographic finding in diabetic retinopathy identified with ultra wide-field fluorescein angiography. Semin Ophthalmol. 2010;25:27–33. doi: 10.3109/08820538.2010.481239. [DOI] [PubMed] [Google Scholar]
- 18.Silva P.S., Dela Cruz A.J., Ledesma M.G. Diabetic retinopathy severity and peripheral lesions are associated with nonperfusion on ultrawide field angiography. Ophthalmology. 2015;122:2465–2472. doi: 10.1016/j.ophtha.2015.07.034. [DOI] [PubMed] [Google Scholar]
- 19.Reddy S., Hu A., Schwartz S.D. Ultra wide field fluorescein angiography guided targeted retinal photocoagulation (TRP) Semin Ophthalmol. 2009;24:9–14. doi: 10.1080/08820530802519899. [DOI] [PubMed] [Google Scholar]
- 20.Muqit M.M., Marcellino G.R., Henson D.B. Optos-guided pattern scan laser (Pascal)-targeted retinal photocoagulation in proliferative diabetic retinopathy. Acta Ophthalmol. 2013;91:251–258. doi: 10.1111/j.1755-3768.2011.02307.x. [DOI] [PubMed] [Google Scholar]
- 21.Spaide R.F. Prospective study of peripheral panretinal photocoagulation of areas of nonperfusion in centralretinal vein occlusion. Retina. 2013;33:56–62. doi: 10.1097/IAE.0b013e3182641875. [DOI] [PubMed] [Google Scholar]
- 22.Singer M.A., Tan C.S., Surapaneni K.R., Sadda S.R. Targeted photocoagulation of peripheral ischemia to treat rebound edema. Clin Ophthalmol. 2015;9:337–341. doi: 10.2147/OPTH.S75842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mookiah M.R., Acharya U.R., Chua C.K., Lim C.M., Ng E.Y., Laude A. Computer-aided diagnosis of diabetic retinopathy: a review. Comput Biol Med. 2013;43:2136–2155. doi: 10.1016/j.compbiomed.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 24.Diabetic Retinopathy Clinical Research Network. Peripheral diabetic retinopathy (DR) lesions on ultrawide-field fundus images and risk of DR worsening over time. DRCRnet Web site. Available at: http://drcrnet.jaeb.org/Studies.aspx?RecID=239. Accessed 24.03.16.