Abstract
Background
The industrial revolution that took place in the United Kingdom (UK) between 1760 and 1830 led to profound social change. Occupational medicine was concerned with the diagnosis, treatment, and prevention of occupational diseases, that is, diseases directly caused by exposure to workplace hazards. A similar pattern of development has occurred globally.
Methods
A review of relevant literature.
Results
The international conceptualization and development of occupational health occurred during the 20th century. A new paradigm for occupational health has emerged that extends the classical focus on what might be termed “health risk management” that is, the focus on workplace hazards and risk to health to include the medical aspects of sickness absence and rehabilitation, the support and management of chronic noncommunicable diseases, and workplace health promotion.
Conclusion
The future strategic direction for occupational health will be informed by a needs analysis and a consideration of where it should be positioned within future healthcare provision. What are the occupational health workforce implications of the vision for occupational health provision? New challenges and new ways of working will necessitate a review of the competence and capacity of the occupational health workforce, with implications for future workforce planning.
Keywords: human resources management, occupational health, occupational medicine, paradigm shift, workforce planning
1. Introduction
This paper examines the evolution that has taken place in occupational medicine and occupational health (OH) from the second half of the 20th century and discusses the paradigm shift in practice that is now faced by OH practitioners. New challenges and new ways of working will necessitate a review of the competence and capacity of the OH workforce, with implications for future workforce planning.
2. Evolution of occupational medicine
The industrial revolution that took place in the UK between 1760 and 1830 led to profound social change, with rapid urbanization associated with squalid living conditions and epidemics of infectious diseases [1]. Working and residential conditions in the 1830s and their effects on adults and children were recorded by Charles Turner Thackrah, regarded as the father of occupational medicine in the UK [2]. Consideration of the health and well-being of workers reflects prevailing social attitudes and tends to lag behind periods of significant industrial change. The UK government gradually introduced legislation to protect the health of workers, in light of the increasing public intolerance of such conditions. Occupational medicine was concerned with the diagnosis, treatment, and prevention of occupational diseases, that is, diseases directly caused by exposure to workplace hazards. A similar pattern of development has occurred globally.
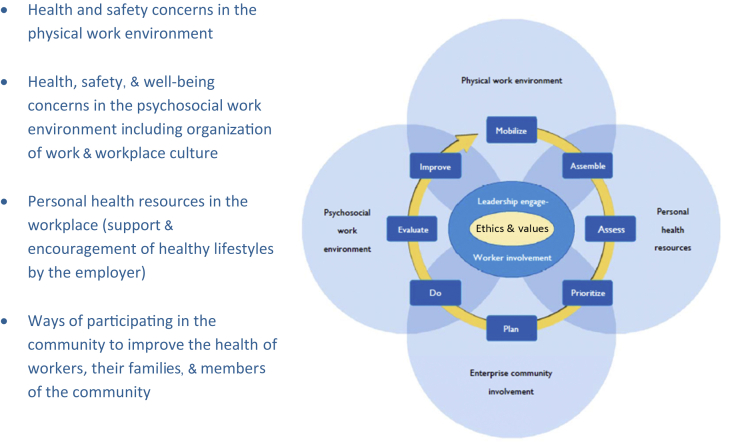
The international conceptualization and development of OH occurred during the 20th century. Key influences were the establishment of the International Commission for Occupational Health, in 1906, and the establishment of the Industrial Labour Organisation, after the Second World War. The International Labour Organisation (ILO) convention 161 (1985) described the components of workplace OH provision [3]. Concepts of OH have developed subsequently, influenced by the World Health Organisation (WHO) definition of health [4]. Health is a positive affirmation of physical, mental, and social well-being, not merely the absence of disease. There has also been the recognition that OH has a positive contribution to make to the performance of enterprises and to the well-being of the communities in which they are based. The WHO Europe concept of health, environment, and safety management in enterprises described comprehensive OH as the long-term maintenance of the working ability of employees, taking into account occupational, environmental, social, and lifestyle determinants of health [5] More recently, the WHO healthy workplace model has portrayed a healthy workplace as “one in which workers and managers collaborate to use a continual improvement process to protect and promote the health, safety and well-being of all workers and the sustainability of the workplace” by considering four discrete, albeit linked, areas [6]. These are: (1) health and safety concerns of the physical work environment; (2) health, safety, and well-being concerns in the psychosocial work environment, including work organization and workplace culture; (3) personal health resources in the workplace (support and encouragement of healthy lifestyles by the employer); and (4) ways of participating in the community to improve the health of workers, their families, and members of the community.
At the core of the model is the need to secure the engagement of the workforce via effective leadership, and the promotion of workplace culture and values that underpin health and well-being (Fig. 1). There is now a body of evidence showing the relationship between workplace health and well-being, worker engagement, resilience, and productivity [7]. Thus, OH may be promoted as contributing much more than the prevention of occupational diseases and illnesses; there is a strong business case to be made in terms of the productivity of organizations as well as the public health of communities.
Fig. 1.
World Health Organisation healthy workplace model.
Note. From: World Health Organisation (WHO). 5 Keys to Healthy Workplaces. WHO global model for action [Internet]. Geneva (Switzerland): WHO. 2011 [cited 2015 Feb 25]. Available from: http://www.who.int/occupational_health/5_keys_EN_web.pdf?ua=1. Copyright 2011, WHO.
A new paradigm for OH has emerged that extends the classical focus on what might be termed “health risk management”—that is, the focus on workplace hazards and risk to health—to include the medical aspects of sickness absence and rehabilitation, the support and management of chronic noncommunicable diseases, and workplace health promotion. The importance of sickness absence as a global health measure has been highlighted by Kivimaki et al [8] in the Whitehall II studies. A report from the Organisation for Economic Cooperation and Development on sickness, disability, and work [9] has shown that long-term sickness absence is high in many member countries of the Organisation for Economic Cooperation and Development, and this is linked to disability inflow rates. The report identified a need to produce guidance for health professionals to maximize health outcomes and minimize inappropriate sick leave. The importance of incentives for employers to provide work environments that strengthen, rather than compromise, physical and mental health of workers was emphasized. In the UK, a review of sickness absence recorded that, every year, 140 million working days are lost to sickness absence [10]. Although most people return to work after a short period of absence, approximately 300,000 people fall out of work and claim health-related state benefits. Worklessness is associated with significant personal and financial cost. It has also been recognized that the longer someone is out of work, the harder it becomes to return to work. Consequently, the authors recommended the creation of a new type of service, available to people absent from work because of illness, which would provide an in-depth assessment of physical and/or mental health. This would form the basis for bespoke advice on how to return to work. It is anticipated that the service would be provided by appropriately skilled occupational therapists, physiotherapists, general practitioners, and nurses, as well as by OH professionals. There is a strong evidence base to support vocational rehabilitation, with particular emphasis on common health problems, such as mild to moderate musculoskeletal, mental health, and cardiorespiratory conditions [11]. These conditions account for two-thirds of long-term sickness absence. A key feature of vocational rehabilitation, which should influence future healthcare planning and commissioning, is that clinical treatment alone has little impact on work outcomes. Effective vocational rehabilitation depends on work-focused healthcare and accommodating workplaces, thus highlighting the role of OH practitioners in future integrated healthcare pathways.
Many industrialized countries are facing the challenges of an aging population and workforce. In the United States of America, it is projected that by 2020, 25% workforce will be aged ≥ 55 years [12]. In Europe, it is predicted that a combination of reducing birth rates and rising life expectancy will halve the ratio between people of working age and people over the age of 65 years by 2060 [13]. Asia too will have to address this phenomenon. Japan is considered the World's oldest country, and by 2040, it is predicted to have the highest median age of its population. In addition, China, Hong Kong, and Singapore are reported to be aging the fastest among the countries of the region. In absolute numbers, China and India have the largest older populations. From a public health perspective, this will be associated with an increase in the percentage of the population with noncommunicable diseases. Developed economies are experiencing a rise in healthcare expenditure for chronic diseases, such as cancer and cardiovascular disease, and Japan is reported to allocate 36% of government spending on its healthcare provision [14]. WHO has developed an active aging policy framework [15]. Active aging is defined as the process of optimizing opportunities for health, participation, and security in order to enhance quality of life as people age. Work is recognized as an important component of active aging, and WHO has stated that, throughout the world, if more people would enjoy opportunities for dignified work (properly remunerated in adequate environments, protected against workplace hazards) earlier in life, people would reach old age able to participate in the workplace. The workplace and OH has an important role, therefore, in promoting the health and well-being of workers, via the adoption of the WHO healthy workplace model, and in becoming part of mainstream healthcare for the purposes of treating and supporting people with noncommunicable diseases. “WHO considers workplace health programs as one of the best-buy options for prevention and control of non-communicable diseases and for mental health. Such programs can help achieving the WHO objective of reducing the avoidable deaths of NCDs and the burden of mental ill health and to protect and promote health at the workplace as stipulated in the Global Plan of Action on Workers' health 2008–2017” [16].
3. Strategic direction—Occupational health to workplace health and well-being
The future strategic direction for OH will be informed by a needs analysis and a consideration of where it should be positioned within future healthcare provision. The WHO Global Plan of Action [17] asserts that the health of workers is determined not only by occupational hazards, but also by social and individual factors, and access to health services. It raises concern that there are major gaps between and within countries in the exposure of workers and local communities to occupational hazards and their access to OH services. The function of OH services has been to protect workers from workplace hazards. These may lead to workplace injuries, cancer, and hearing loss, as well as respiratory, musculoskeletal, cardiovascular, reproductive, neurological, skin, and mental ill health disorders [18]. Globally, exposures to carcinogens are estimated to cause 8% lung cancer, the most frequent cause of cancer. Occupational exposures to airborne particulates probably cause 12% of deaths due to chronic obstructive pulmonary disease. There are also deaths due to silicosis, asbestos-related diseases, and pneumoconiosis. However, in high-income countries, morbidity due to conditions such as low back pain and common mental health disorders has become the focus of OH services. The growing evidence of the global impact of mental illnesses is demonstrated by the finding that five of the 10 leading causes of disability, worldwide, are mental health problems [19]. Mental illness is considered to be as relevant in low-income countries as in wealthy ones, cutting across age, gender, and social strata. The workplace has been identified as a key setting for addressing the rising incidence and prevalence of mental ill health. The workplace is an appropriate environment in which to raise awareness of mental health and to use good mental health practice to influence attitudes toward mental ill health. The WHO/ILO document ‘Mental Health and Work’ [19] provides examples of mental health workplace initiatives from the UK, the USA, Canada, Spain, Italy, and Finland.
With regard to the strategy for prevention of occupational ill health, the ILO has referred to a new paradigm of prevention, focusing on occupational diseases and not only on occupational injuries [20]. The “hidden epidemic” of occupational disease comprises the established diseases, such as the pneumoconioses and asbestos-related diseases, in addition to emerging conditions. Technological, social, and organizational changes in the workplace, as well as rapid globalization, have seen the emergence of new risks and challenges. Musculoskeletal and mental health disorders will require new approaches to stem the increasing incidence. There will be a need for better data to inform prevention strategies. Challenges to be overcome in this regard include: (1) the lack of knowledge and experience in diagnosis, recognition, and reporting occupational diseases; (2) inclusion of small- and medium-sized enterprises in national reporting schemes; (3) changing working populations as a result of migration; and (4) the long latency of occupational diseases.
Further analysis of the global burden of disease reveals that the incidence and prevalence of noncommunicable diseases pose the greatest challenge to both public and OH. Thus, future OH practice will be based on a holistic biopsychosocial approach to the promotion of health, well-being, and work ability.
The strategic implication of the paradigm shift from a “labor approach” to a “public health approach” is that there will be a move away from a consideration of OH toward a focus on worker's health [21]. This means that OH practitioners will be concerned with not only employed workers, that is, those under some form of employment contract, but also self-employed and informal workers. Interventions will extend to families and communities, and will not be restricted to actions at the workplace. The promotion and maintenance of health and well-being will involve a consideration of all health determinants and will not be restricted to work-related health issues. Importantly, the health of workers will not be seen as only the responsibility of employers, but also of the wider stakeholder group, including health, work, and environment authorities; insurance companies; and other healthcare practitioners. An example might be in addressing stress at work. Many companies have now developed health and well-being strategies that encourage healthy behaviors at work and at home, and promote participation in physical activity challenges. Use is made of activity-tracking devices that are able to download data to mobile phones. The outputs may be used for both motivational purposes and construction of organizational risk profiles. Improvements in the profiles may attract lower insurance premiums for companies. Social media may be used to develop online communities and to facilitate activity challenges. This will redefine the remit and roles of OH practitioners and may necessitate searching for a new term to describe the role and function of the discipline.
4. Developing the OH workforce
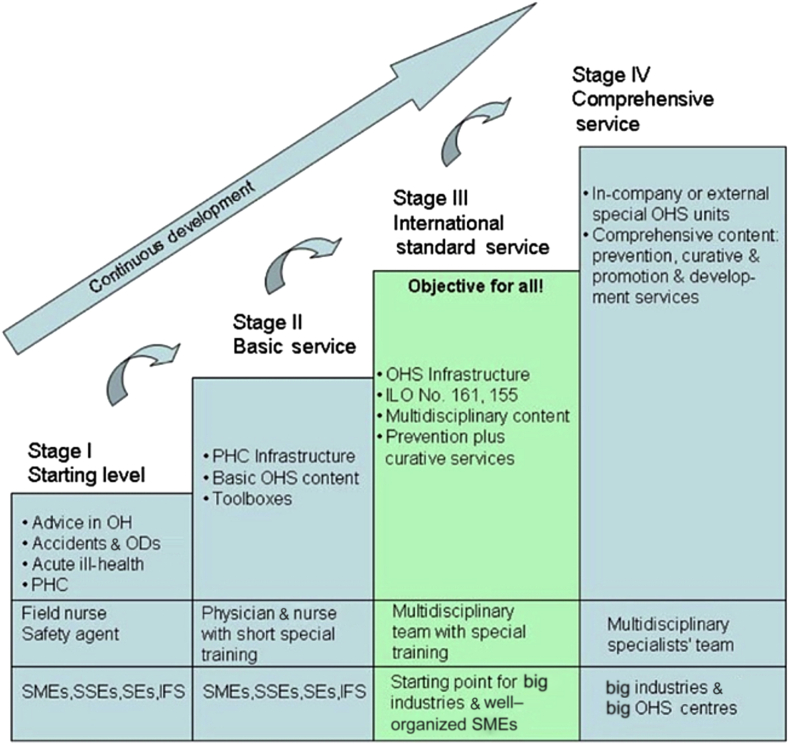
In 2005, WHO, ILO, and the International Commission on Occupational Health jointly launched the Basic Occupational Health Services initiative, with the aim to provide OH globally at some level to all working people. The Basic Occupational Health Services are for the protection of people's health at work; promotion of health, well-being, and work ability; as well as prevention of ill health and accidents. They are underpinned by the Alma Ata principles [22]. Rantanen [23] developed the original Basic Occupational Health Services concept into a four-stage model of increasingly advanced services (Fig. 2), providing for more complex needs by progressively skilled and experienced OH providers. This model is grounded in primary care delivery systems. Increasing development and sophistication of OH services, as might be found in large multinational organizations, have sufficient resources to employ specialist and expert OH practitioners. Such services will be expected to demonstrate a return on investment for the employing organizations, which should include not only measures of worker productivity, but also the value added to the local communities and healthcare systems.
Fig. 2.
Stepwise development of occupational health services.
Note. From: J. Rantanen, Basic occupational health services, 3rd ed, p. 8 [Internet]. Helsinki (Finland): Finnish Institute of Occupational Health, 2007 [cited 2015 Apr 04]. Available from: http://www.ttl.fi/en/publications/Electronic_publications/Documents/BOHS3Edition28Sept2007_3_.pdf. Copyright 2007, Finnish Institute of Occupational Health. Reproduced with permission.
IFS, informal sector; ILO, International Labour Organisation; OD, occupational disease; OHS, occupational health service; PHC, primary health care; SE, self-employed; SME, small and medium-sized workplace; SSE, small enterprise.
This is consistent with the WHO's work on extending access to the most essential health interventions and services for workers' health [17]. This includes: (1) enabling primary care centers to deliver preventive, curative, and rehabilitation people-centered care according to the specific health needs of working people, particularly those who do not have access to OH services; (2) strengthening the specialized OH services (multidisciplinary and basic), and improving their link to primary care centers and the rest of the health systems; (3) stimulating international efforts to build human resource capacities for workers' health, in both primary care and OH specialists.
What are the OH workforce implications of the vision for OH provision? The WHO Global Strategy on Occupational Health for All: The Way to Health at Work [24] has set out objectives and actions that include the development of human resources for OH. OH is described as a broad expert activity that utilizes the basic knowledge of other disciplines, such as medicine, chemistry, physics, toxicology, physiology, psychology, and safety technology. At the time of publication (1994), it was considered that many of the industrialized countries had trained a sufficient number of occupational medical experts to provide one physician per 2,000–3,000 workers and about one nurse per 1,000–2,000 workers (with a wide range of variation). However, the training of specialists other than medical experts for the multidisciplinary OH team was less systematically organized in most countries. Special curricula for occupational hygiene were available in six European countries and in the United States and Canada. WHO had defined the profile of the occupational hygienist on the basis of defined areas of knowledge, in an effort to promote international harmonization of training curricula. Training of physiotherapists specialized in OH was also available in some countries, while the special training of occupational psychologists was said to be rare. In many Western European countries, the training of safety engineers was reported to be well organized. The universal shortage of both expert resources and training in developing and newly industrialized countries was highlighted. Three main reasons were suggested to explain this. (1) A lack of effective legislation and a lack of requests from authorities and employers meant that there was little stimulus of employment opportunities for such experts. (2) In the absence of a stimulus, vocational training institutions and universities had not organized and developed curricula for the training of experts in OH. (3) In some instances where training was available, it was oriented to clinical occupational medicine only, which, although important, did not address the needs for expertise in a multiprofessional preventive workplace-oriented OH service.
Objective 3 of the more recent WHO Global Plan of Action 2008–2017 is concerned with the improvement of the performance of and access to OH services. Among other things, the capacity of a sufficient and competent workforce is a key requisite. Suggested measures include further postgraduate training in relevant disciplines, building capacity for the provision of basic OH services, incorporating workers' health in primary healthcare training, creating incentives for attracting and retaining human resources for workers' health, and the establishment of networks of services and professional associations. There is a recognition of the need for supranational leadership and leverage to provide the necessary stimulus for building human and institutional capacities.
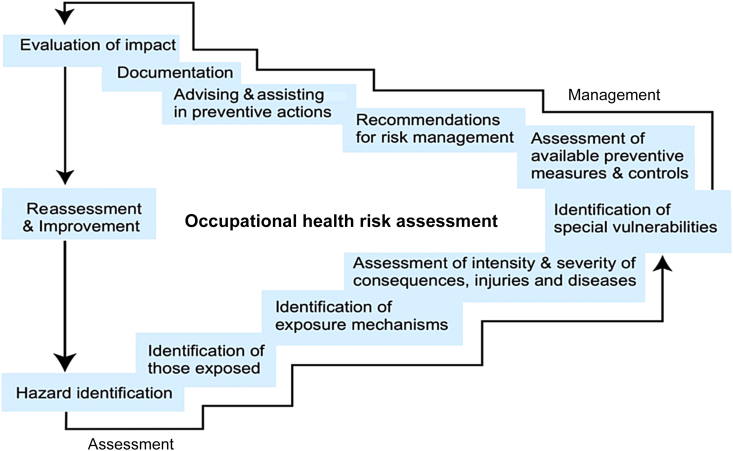
Although many reports and recommendations identify that a multiprofessional approach is desired or essential, and many identify who may be included in this approach, few reports identify the actual make-up of an OH team, or offer a process on how to determine the make-up or numbers to meet the need of a workforce. This might be approached by looking at multiprofessional interventions with regard to the new OH paradigm. With regard to health risk management, it is internationally recognized that multiprofessional teams are key to a successful OH service [25], but owners and managers of businesses must also understand the need to address risk assessment and how to commission evidence-based, quality-assured OH and safety teams who deliver cost-effective services. In Switzerland, a postgraduate training program in OH has been designed such that the core OH elements are delivered to a combination of occupational physicians, health and safety officers, and business managers, before teaching profession-specific modules. The compilation of a multiprofessional team should be based on risk assessments of the needs of the workforce. A risk assessment cycle of assessment, management, and review (Fig. 3) is an example of a framework that might be used to inform the composition of an OH and safety team. The virtuous circle of assessment of workforce hazards and risk and management actions to implement preventative actions highlights the competencies required of the team [26].
Fig. 3.
Risk assessment–risk management cycle.
Note. From: J Rantanen, Basic occupational health services [Internet]. 2007 [cited 2015 Apr 04]. Available from: http://www.ttl.fi/en/publications/Electronic_publications/Documents/BOHS3Edition28Sept2007_3_.pdf. Copyright 2007, Finnish Institute of Occupational Health. Reproduced with permission.
In the EU, despite the Occupational Health Services Convention recommendation [3] that OH services should be multidisciplinary, development of the multiprofessional model was reported to be limited to the UK, Spain, and the Nordic countries [27]. For many of the other EU countries, the role of the occupational physician in the delivery of OH is paramount, and an occupational physician is often the only practitioner considered necessary or available.
With respect to attendance management and rehabilitation, a systematic review found that early access to OH and a multiprofessional approach were the two key factors for supporting return to work [28]. A number of reports highlight the need to include an OH philosophy into all healthcare practitioners' encounters with people, to ensure that work is considered as an outcome measure in interventions for those of working age. This would establish a broad-based vocational rehabilitation workforce, of which OH practitioners were only a part. There is an obvious challenge to developing a multidisciplinary approach to the management of chronic noncommunicable disease. The cost of utilizing several professionals, where previously only one had the responsibility for delivering care, is a potential barrier to the new paradigm. Where a team of practitioners addressing both physical and psychological illness and human resource professionals address work, home, and social life and emphasize the worker's responsibility and role in their rehabilitation, a long-term success rate and even reversal of chronic problems should demonstrate qualitative and quantitative returns on investment [29].
A fully integrated OH model of care should include health promotion initiatives, insurance benefits (to include gym membership and other healthcare offers, short- and long-term incapacity, compensation, and case management provision), OH and safety engagement, and employee assistance programs [30]. In addition, specialists aligned with work (architects and design engineers, toxicologists, case managers, and legal and union representatives) are sometimes engaged in an OH communication group. Models of workplace health and well-being, such as the Business in the Community Workwell model [31], demonstrate the clinical and nonclinical influences on workplace well-being. In this model, there is a need for availability and competencies of human resources for promoting good physical and mental health, good work, good relationships, and good support. Thus, the wider OH team, in this case, would include the additional specialists already mentioned, experts in human factors, practitioners in personnel and organizational development, health educationalists, and the multiprofessional stakeholders in the provision of comprehensive workplace health support.
5. Building OH workforce capacity
Initiatives for capacity building are not new. A methodology for planning the development of human resources in environmental and OH was piloted in several countries between 1994 and 1996 [32]. The context was a recommendation from the WHO Office of Occupational Health for countries to develop a national program or plan that included a strategy to ensure the required staffing. The objectives of the planning process were: (1) to identify the development and needs of human resources; (2) to maximize resources and improve interagency coordination; (3) to generate funds for capacity building; and (4) to establish policies and infrastructure to maintain human resources.
The three components of the development of human resources are planning, production, and management. Planning is concerned with the number and type of personnel needed (in short, medium, and long terms), production supplies the workforce through education and training (numbers and competencies required), and management relates to the recruitment, retention, and support of personnel. Estimating the number of personnel required within the respective disciplines that make up OH is not always easy. In the UK, development of OH human resources has been hampered by an inability to credibly predict the size and composition of a future OH workforce as well as to address delivery of training satisfactorily. Training must be adequately resourced with respect to the provision and delivery of academic programs, availability of training places, and affordability for students. Where there is very little OH provision (Stages 1 and 2 of the Basic Occupational Health Services model), the focus is on having at least some basic health and safety inputs. However, for Stages 3 and 4, the potential skill mix becomes complex. There needs to be clarity about the roles that different practitioners play in delivering OH and also how these professionals may interact. Weinger [32] refers to several strategies for estimating the number of personnel needed for specific functions. A market-orientated strategy is based on the demand for services. This may be linked to affordability. An incremental change strategy sets a target for the production and delivery of services over a period of time. The targets may be set by national authorities. A normative strategy applies standards, or norms, that have been derived. For example, there may be a standard set for the number of occupational physicians per employee. The standard is usually empirically based.
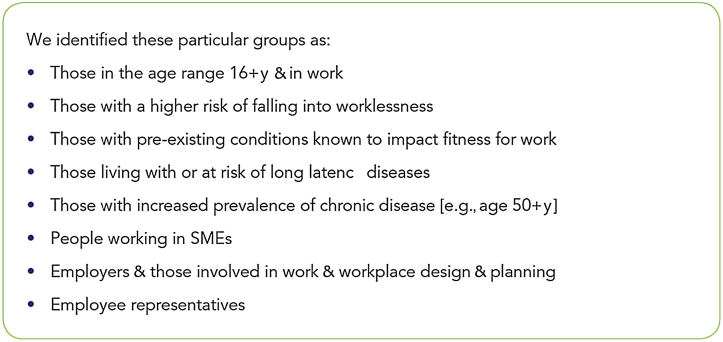
In the UK, an OH workforce planning project adopted a population-centric planning approach to estimating future OH needs and practice [33]. A strategic analysis suggested that the scope of practice for OH over the next 20 years will be a working age population comprising those groups likely to consume, or benefit from, OH advice (see Fig. 4). This is consistent with previous literature [34].
Fig. 4.
Differentiation of the working age population [33].
Note. From: The Council for Work and Health, Planning the future: delivering a vision of good work and health in the UK for the next 5-20 years and the professional resources to deliver it, p. 7 [Internet]. UK: The Council for Work and Health. 2014 [cited 2015 Mar 31]. Available from: https://www.som.org.uk/fileadmin/user_upload/Office/docs/Planning_the_Future-OH_and_its_Workforce-April_2014.pdf. Copyright 2014, Finnish Institute of Occupational Health. Reproduced with permission.
SME, small and medium-sized workplace.
A series of case studies were developed that were intended to act as proxies for a future OH market, that is, areas of practice for which there is likely to be a demand for OH. Each of the 10 case studies provides a pen portrait or profile of the people it is envisaged will need an OH input. Each case study has a vignette describing the problem to be solved, background information giving context to the vignette, and suggested solutions involving a multiprofessional OH provision. The vignettes include a baker working in a small bakery who develops asthma at work, a factory worker with low back pain who is too young to leave work and draw a pension, a call-center operative with obsessive-compulsive disorder, a second-generation Asian secretary with metabolic syndrome, and a chief executive officer of a small- and medium-sized biotech company who wants to address high staff turnover by investing in health and well-being initiatives. The output from the strategic analysis will inform future work on OH delivery models, future OH practice, competencies for an OH workforce, and the numbers and skill mix that will be required. It will also address the challenge of recruiting appropriately qualified and experienced OH professionals at a time when a career in OH is not particularly attractive.
6. Conclusion
OH practice arose from the social changes of the industrial revolution and, in some cases, is now seen as an integral component of a successful business. However, access to specialist OH advice is usually restricted to workers employed by large organizations. The public health challenges of the increasing prevalence of noncommunicable diseases and aging populations will lead to changes in national healthcare systems and an opportunity for OH to become integrated within the new systems. A new OH paradigm embracing health and well-being in the workplace and the community, in order to promote the employability of people, poses questions about the future composition and capacity of the OH workforce. These questions must be answered by means of effective workforce planning and development of human resources.
Conflicts of interest
All authors have no conflicts of interest to declare.
References
- 1.Harrison J. Occupational safety and health in the United Kingdom: securing future workplace health and wellbeing. Ind Health. 2012;50:261–266. doi: 10.2486/indhealth.ms1376. [DOI] [PubMed] [Google Scholar]
- 2.Meiklejohn A. E and S Livingstone; Edinburgh (Scotland): 1957. Charles Turner Thackrah: the effect of arts, trades and professions on health and longevity, with an introductory essay on his life, work and times. [Google Scholar]
- 3.International Labour Organisation (ILO). C161 Occupational Health Services Convention (No. 161) [Internet]. Geneva (Switzerland): ILO. 1985 [cited 2015 Jan 10]. Available from: http://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_ILO_CODE: C161.
- 4.World Health Organisation (WHO). WHO definition of health [Internet]. 1948 [cited 2015 Apr 1]. Available from: http://who.int/about/definition/en/print.html.
- 5.World Health Organisation (WHO). Workplace health protection and promotion in the policy and practice of social and health insurance institutions. [Internet]. Report on a WHO Meeting, 1999 Oct 21-22. Bilthoven (Netherlands). 1999 [cited 2015 Apr 1]. Available from: http://www.who.int/occupational_health/regions/en/oeheurworkplaceprotect.pdf.
- 6.World Health Organisation (WHO). 5 Keys to Healthy Workplaces. WHO global model for action [Internet]. 2011 [cited 2015 Feb 25]. Available from: http://www.who.int/occupational_health/5_keys_EN_web.pdf?ua=1.
- 7.MacLeod D, Clarke N. Engaging for success: enhancing performance through employee engagement. A report to Government. Department for Business, Innovation and Skills, UK Government [Internet]. 2009 [cited 2015 Apr 1]. Available from: http://webarchive.nationalarchives.gov.uk/20090609003228/http://www.berr.gov.uk/files/file52215.pdf.
- 8.Kivimaki M., Head J., Ferrie J.E., Shipley M.J., Vahtera J., Marmot M.G. Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. BMJ. 2003;327:364. doi: 10.1136/bmj.327.7411.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Organisation for Economic Cooperation and Development. Sickness, disability and work—keeping on track in the economic downturn [Internet]. Background paper for the high level forum. Stockholm (Sweden): 2009 May 14-15. 2009 [cited 2015 Feb 23]. Available from: http://www.oecd.org/employment/emp/42699911.pdf.
- 10.Black F, Frost D. Health at work—an independent review of sickness absence. Department of Work and Pensions [Internet]. 2011 [cited 2015 Feb 25]. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/181060/health-at-work.pdf.
- 11.Waddell G, Burton KA, Kendall NAS. Vocational rehabilitation—what works for whom and when? [Internet]. London (UK): The Stationary Office. 2008 [cited 2015 Feb 25]. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/181060/health-at-work.pdf.
- 12.Aging in the American Workforce. Wikipedia [Internet]. 2016 [cited 2015 Feb 25]. Available from: http://en.wikipedia.org/wiki/Aging_in_the_American_workforce.
- 13.Meeting the challenge of Europe's ageing workforce—The Public Employment Service response [Internet]. 2011 [cited 2015 Feb 25]. Available from: file:///C:/Users/John%20Harrison/Downloads/HoPES_Meeting_Challenges_Aging_Workforce_EN[1][1]%20(1).pdf.
- 14.Vernon K. 2010. Ageing: impact on companies in Asia. Community Business [Internet] [cited 2015 Apr 4]. Available from: http://www.communitybusiness.org/images/cb/publications/2010/Ageing.pdf. [Google Scholar]
- 15.World Health Organisation (WHO). Active ageing—A policy framework [Internet]. Madrid (Spain): WHO. 2002 [cited 2015 Feb 25]. Available from: http://whqlibdoc.who.int/hq/2002/WHO_NMH_NPH_02.8.pdf?ua=1.
- 16.Healthy workplaces—a global model for action [Internet]. 2011 [cited 2015 Feb 25]. Available from: http://www.who.int/occupational_health/healthy_workplaces/en/.
- 17.World Health Organisation. Workers' health: global plan of action. World Health Organisation, Sixtieth World Health Assembly [Internet]. 2007 May 23 [cited 2015 Mar 02]. Available from: http://www.who.int/occupational_health/WHO_health_assembly_en_web.pdf?ua=1.
- 18.World Health Organisation (WHO). Global health risks: mortality and burden of disease attributable to major risks. [Internet]. Geneva (Switzerland): WHO. 2009 [cited 2015 Mar 02]. Available from: http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_Front.pdf?ua=1.
- 19.Harnois G., Gabriel P. World Health Organisation and International Labour Organisation; Geneva (Switzerland): 2000. Mental health and work: impact, issues and good practices. In: [Internet]. In: Nations for Mental Health [Internet] [cited 2015 Mar 02]. Available from: http://www.who.int/mental_health/media/en/712.pdf. [Google Scholar]
- 20.International Labour Organisation. The prevention of occupational diseases: world day for safety and health at work. [Internet]. 2013 Apr 28 [cited 2015 Mar 02]. Available from: http://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---safework/documents/presentation/wcms_207663.pdf.
- 21.Neira M. 2011. Healthy workplaces: a model for action [Internet] [cited 2015 Apr 04]. Available from: http://www.who.int/occupational_health/publications/launch_hwp_22april.pdf. [Google Scholar]
- 22.Declaration of Alma-Ata International Conference on Primary Health Care [Internet]. 1978 Sep 6-12; Alma-Ata, USSR; 1978 [cited 2015 Apr 04]. Available from: http://www.who.int/publications/almaata_declaration_en.pdf.
- 23.Rantanen J. Basic occupational health services [Internet]. 2007 [cited 2015 Apr 04]. Available from: http://www.ttl.fi/en/publications/Electronic_publications/Documents/BOHS3Edition28Sept2007_3_.pdf.
- 24.Global strategy on occupational health for all: the way to health at work: recommendation of the second meeting of the WHO Collaborating Centres in Occupational Health, Beijing, China, 1994 Oct 11-14 [Internet]. Geneva (Switzerland): World Health Organisation. [cited 2015 Mar 27]. Available from: http://www.who.int/occupational_health/publications/globstrategy/en/index6.html.
- 25.Diamond J., Somers A., Garreau M., Martin D. New health professionals network: the future face of medicine. Nurs Leadership. 2005;18:44–46. doi: 10.12927/cjnl.2005.17833. [DOI] [PubMed] [Google Scholar]
- 26.Rantanen J. 2009. BOHS 5; Risk assessment. Finnish Institute of Occupational Health [Internet] [cited 2015 Apr 10]. Available from: http://www.ttl.fi/en/publications/Electronic_publications/Documents/BOHS_5_FIII%20indd.pdf. [Google Scholar]
- 27.Westerholm P. Occupational health services in eleven countries. In: presentation to Institution of Occupational Safety and Health (IOSH) conference, Cardiff, 2007. Thereafter published as Supporting health at work: an international perspectives on occupational health services [Internet]. IOSH. 2007 [cited 2015 Apr 10]. Available from: www.cardiff.ac.uk/cwerc/events/seminar1/Peter%20Westerholm.ppt.
- 28.Hoefsmit N., Houkes I., Nijhuis F. Intervention characteristics that facilitate return to work after sickness absence: a systematic literature review. J Occup Med. 2012;22:462–477. doi: 10.1007/s10926-012-9359-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Auty A. BackCare and work. BackCare J. 2009:18–22. [Google Scholar]
- 30.Graeve C., McGovern P., Nachreiner N.M., Ayers L. Establishing the value of occupational health nurses' contribution to worker health and safety: a pilot test of a user-friendly estimation tool. Workplace Health Saf. 2014;62:36–41. doi: 10.1177/216507991406200106. [DOI] [PubMed] [Google Scholar]
- 31.Business in the Community. Workwell model [Internet]. 2011 [cited 2015 Apr 4]. Available from: http://www.bitc.org.uk/programmes/wellbeing/workwell-model.
- 32.Weinger M. World Health Organization; Geneva (Switzerland): 1997. Guidelines for human resources planning in environmental and occupational health. [Google Scholar]
- 33.The Council for Work and Health. Planning the future: delivering a vision of good work and health in the UK for the next 5–20 years and the professional resources to deliver it [Internet]. 2014 [cited 2015 Mar 31]. Available from: https://www.som.org.uk/fileadmin/user_upload/Office/docs/Planning_the_Future-OH_and_its_Workforce-April_2014.pdf.
- 34.Macdonald E.B., Sanati K.A. Occupational health services now and in the future: the need for a paradigm shift. J Occup Environ Med. 2010;52:1273–1277. doi: 10.1097/JOM.0b013e3181f7cbf0. [DOI] [PubMed] [Google Scholar]