SUMMARY
Brucellosis is an endemic disease in various regions of the world. Testicular abscess is a very rare complication of brucellosis which can be misdiagnosed as a testicular mass and may lead to unnecessary orchiectomy. To our knowledge there are only eight reported cases in the literature of a brucellar testicular abscess. We present a case of testicular abscess due to brucellosis diagnosed with serologic tests and color Doppler sonography, and treated with antibiotics and fine needle aspiration.
Key words: Abscess, brucellosis, color Doppler sonography, testicular, ultrasonography
Introduction
Brucellosis is an endemic, zoonotic disease in some regions of the world and affects several organs and tissues in humans. Direct contact with infected animals or ingestion of contaminated animal products are routes of transmission to humans.1, 2 Brucellar orchi-epididymitis is a complication of systemic brucellosis in humans and can be seen in 5.7% of affected patients.[1] Brucellar testicular abscess can be misdiagnosed as a necrotic testicular mass leading to unnecessary orchiectomy.3, 4, 5, 6, 7, 8 Thus, the diagnosis of an abscess is of critical importance to avoid testicular loss in these patients. We present the case of a 23-year-old man with a brucellar testicular abscess that was diagnosed with color Doppler sonographic findings, and treated with drainage and administration of combined antibiotic therapy.
Case Report
A 23-year-old male patient was admitted to the Emergency Department for right testicular swelling for 2 months. The patient declared that he was prescribed gentamycin 1×100 mg in 7 days by a family physician one month before his admission, but his complaints continued. The patient had no history of direct contact with infected animals but had a history of relatively recent ingestion of unpasteurized cheese. Physical examination revealed a body temperature of 36.5 °C and blood pressure of 110/70 mmHg. There was right testicular swelling and tenderness. There was no color change on the scrotum. His laboratory findings included: leukocytes 8470/ mm3, hemoglobin 13.4 g/dl, thrombocytes 467.000/mm3, ALT (alanine aminotransferase) 24.7 IU/L (normal range, 7-40), AST (aspartate aminotransferase) 27.1 IU/L (normal range, 8-41), ESR (erythrocyte sedimentation rate) 19 mm/h, CRP (C-reactive protein) 0.335 mg/dl (normal value, 5 mg/dl), and the Brucella agglutinin titer was positive at 1/1280. The blood cultures of the patient were negative. Sonographic evaluation was performed with a Nemio ultrasound scanner using a 9-12 MHz linear transducer (Toshiba, Tokyo, Japan). Real time scrotal sonography revealed an anechoic cystic lesion with irregular borders and a thick wall measuring 31x41x74 mm, and containing low level echoes with few septa, which almost replaced the entire right testis (Figure 1a). The peripheral border of the lesion and the septa were hypervascular on color Doppler sonography suggestive of an abscess (Figure 1b). The right epididymis and entire right testis tissue were also hypervascularized on Doppler sonography consistent with orchi-epididymitis. The left testis was normal on scrotal gray-scale and Doppler sonography. The patient was diagnosed with brucellar orchi-epididymitis with right testicular abscess based on the constellation of laboratory and sonographic findings. Antibiotic therapy with doxycycline (100 mg twice daily) and streptomycin (1 gram daily) was initiated for 7 days. However, the diameter of the abscess did not change at the end of 7 days, and we decided to drain the abscess using fine needle aspiration to reduce the size of lesion and increase the efficacy of medication. The patient received a 6-week course of oral doxycycline (100 mg twice daily) and rifampicin (600 mg once daily), and follow-up scrotal sonography after two months showed complete resolution of the lesion leaving a residual small area of heterogeneity in the right testis (Figure 1c).
Figure 1.
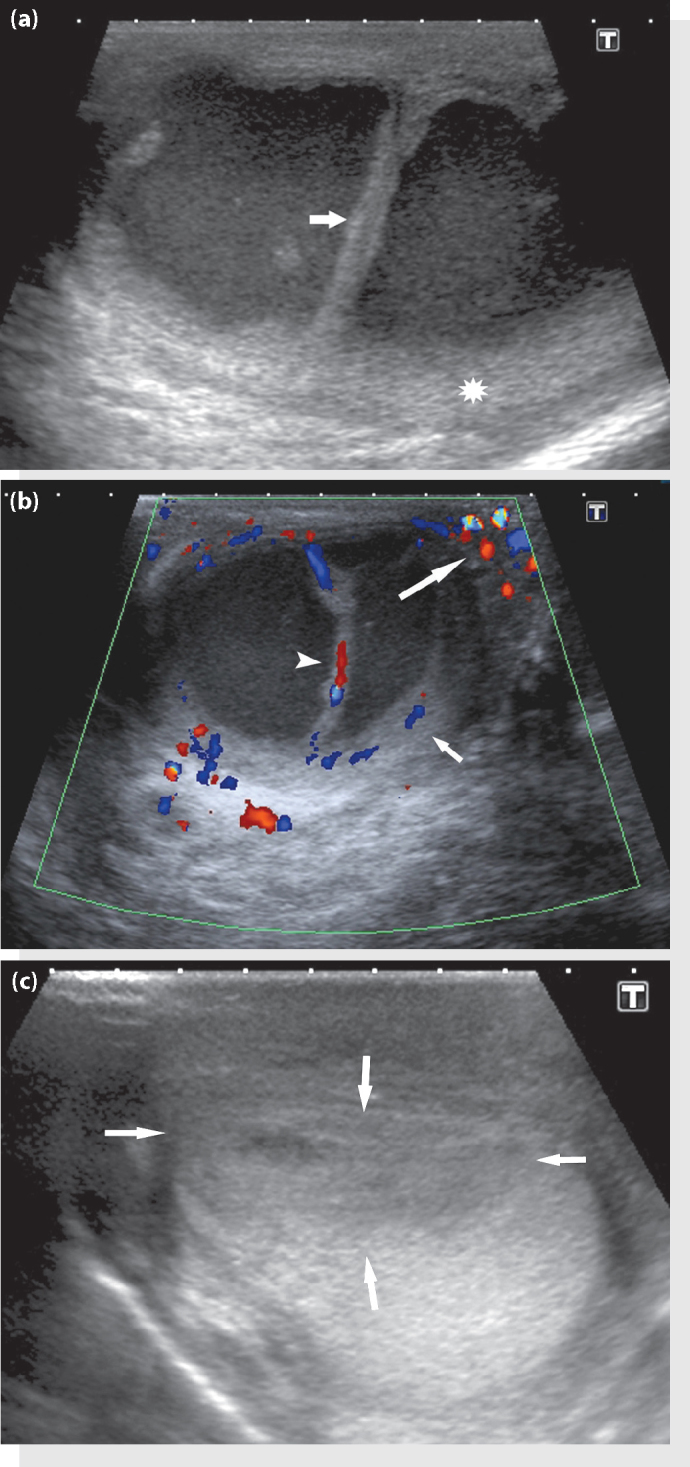
(a) Gray-scale sonography image demonstrates a large anechogenic cystic mass with a thick septum (arrow) and pressed testicular parenchyma (asterisk). (b) Color Doppler sonography image demonstrates the hypervascularity in the thick septum (arrow head), pressed testicular parenchyma (short arrow) and epididymis (long arrow) resembling orchi-epididymitis. (c) Gray-scale sonography image demonstrates heterogeneous hypoechogenic area (arrows) at the right testis on follow up sonography after 2 months.
Discussion
Brucellosis, caused primarily by B. melitensis, remains the most common zoonotic disease all over the world, and it is endemic particularly in Mediterranean countries.1, 2, 7 Brucellosis is a multisystem infectious disease which may cause suppurative complications most frequently at the bones and joints.[2] Most common clinical findings of brucellosis are fever, osteoarticular involvement, and sweating. The genitourinary system is the second most common site of focal brucellosis which can appear as orchi-epididymitis or nephritis. Orchi-epididymitis can be seen in 5.7% of affected patients.[1] Brucellar abscess occurs when the necrosis occurs in the region of granulomatous infection induced by the persistence of the bacteria in macrophages.[9] Testicular abscesses associated with brucellosis in the process of orchiepididymitis are very rare, and only eight cases have been reported in the literature to our knowledge.3, 4, 5, 6, 7, 8, 10, 11 The characteristics of the reported cases are summarized in Table 1.
Table 1.
Charesteristics of patients with testicular brucellar abscess
| Study | Age (years) | Imaging findings (US and CDUS) | Biopsy | Serologic Test | Culture | Treatment |
|---|---|---|---|---|---|---|
| Fernandez et al. | ND | Increased testicular size | Abscess | Positive | Negative | Orchiectomy, double drugx |
| Castillo Soria et al. | ND | Complete destruction of testis | Abscess | Positive | Negative | Orchiectomy, double drugx |
| Bayram et al. | ND | Hypoechoic tumor-like lesion | NGO | STA Positive | B.melitensis | Orchiectomy, D+R |
| Gonzalez Sanchez et al. | ND | Hypoechoic tumor-like lesion | NGO | Positive | ND | Orchiectomy, double drugx |
| Kocak et al. | 32 | Hypoechoic tumor-like mass | CGI | STA Positive | Negative | Orchiectomy, C+D |
| Akinci et al. | ND | Hypervascularity | NGO | STA Positive | B.melitensis | Orchiectomy, D+R |
| Koc et al. | 42 | Hypervascular, thick-walled lesion | CGI | STA Positive | B.melitensis | Drainage, D+R |
| Yemisen et al. | 43 | Hypoechoic, heterogeneous, cystic lesion | No biopsy | STA Positive | Negative | D+R |
| Case in this study | 42 | Anechoic cystic lesion with hypervascularization in thetestis and epididimis | Abscess | STA Positive | Negative | Drainage, D+R+S |
C+D: Ciprofloxacin+doxycycline; CDUS: Color Doppler sonography; CGI: Choronic granulamatous inflammation; D+R: Doxycycline+rifampicin; D+R+S: Doxycycline+rifampicin+streptomycine; ND: Not defined; NGO; Necrotizing granulomatous orchitis; S+D: Streptomycine + doxycycline; STA: Standard tube agglutination; US: Ultrasonography. x: Possibly doxycycline and rifampicin.
In the acute phase of brucellosis, blood cultures are positive in only 10-30% of patients and clinical findings are generally nonspecific. Incidence of blood culture positivity decreases during the course of the infection. The main diagnostic criteria for brucellosis are high agglutination titers (>1/160) for anti-Brucella antibodies using the standard tube agglutination (STA) test, and the presence of the clinical signs and symptoms of brucellosis.[1] In chronic brucellosis the STA test can reveal negative or very low agglutination titers (<1/160). In some cases of brucellosis, anemia (35-55%) or leukopenia (21%) can be observed.[12] In our case, the leukocytes and hemoglobin values were within normal range and there were no abnormal results in other blood tests either. The diagnosis of brucellar testicular abscess was established by the positive serologic test results, history of ingestion of unpasteurized dairy product, and the visualization of dense cystic lesion with thick walls on gray-scale sonography, revealing hypervascularization in the region of epididymis and around the abscess on Doppler sonography.
The main differential diagnosis of testicular brucellar abscess is a necrotic tumor. Failure to diagnose the abscess appropriately can lead to unnecessary orchiectomy in patients with delayed diagnosis due to large suspicious lesions which cause partial or total destruction of the testis.[10] Six patients underwent orchiectomy with combined antibiotic treatment among the reported eight cases in the literature.3, 4, 5, 6, 7, 8 A conservative treatment with antibiotics or combined antibiotic therapy and drainage is usually adequate in the treatment of brucellar testicular abscess. Two patients10, 11 underwent conservative treatment with antibiotics and drainage as in our patient. In the report of Yemisen et al,[11] orchiectomy was offered to the patient at one month follow up because of no change in gray-scale sonographic findings, but the patient did not accept the surgery. In the report of Koc et al,[10] the testicular abscess was diagnosed based on color Doppler sonography and the drainage and the administration of combined antibiotic therapy were applied. In our case, the initial clinical diagnosis was also testicular abscess upon clinical, laboratory and color Doppler sonographic findings. We believe that color Doppler sonography plays an important role in the diagnosis of an abscess as it shows hypervascularization at the region of orchi-epididymitis. Therefore, brucellar testicular abscess can be accurately diagnosed by color Doppler sonography on the basis of hypervascularization in the region of epididymis and testis (i.e. orchi-epididymitis) in a patient with consistent clinical and laboratory findings. Color Doppler sonography was performed in two reported cases8, 10 and hypervascularization in the testicular and epididymal region was the main finding in both examinations.
In conclusion, testicular abscess is a very rare complication of brucellosis which can be under or misdiagnosed. The initial diagnosis of brucellar testicular abscess can be considered in patients with a history of unpasteurized dairy product consumption, clinical findings and serologic test results, and suggestive color Doppler sonographic findings for orchi-epididymitis. Color Doppler sonography is instrumental in the clinical diagnosis when the gray-scale sonographic findings resemble a necrotic testicular tumor.
Conflict of Interest
The authors declare that there is no potential conflicts of interest.
Footnotes
Published online: June 02, 2014
References
- 1.Pappas G, Akritidis N, Bosilkovski M, Tsianos E. Brucellosis. N Engl J Med. 2005;352:2325–2336. doi: 10.1056/NEJMra050570. CrossRef. [DOI] [PubMed] [Google Scholar]
- 2.Gür A, Geyik MF, Dikici B, Nas K, Cevik R, Sarac J. Complications of brucellosis in different age groups: a study of 283 cases in southeastern Anatolia of Turkey. Yonsei Med J. 2003;44:33–44. doi: 10.3349/ymj.2003.44.1.33. CrossRef. [DOI] [PubMed] [Google Scholar]
- 3.Kocak I, Dündar M, Culhaci N, Unsal A. Relapse of brucellosis simulating testis tumor. Int J Urol. 2004;11:683–685. doi: 10.1111/j.1442-2042.2004.00862.x. CrossRef. [DOI] [PubMed] [Google Scholar]
- 4.Fernández Fernández A, Jiménez Cidre M, Cruces F, Guil M, Bethencurt R, Dehaini A. Brucellar orchitis with abscess. [Article in Spanish] Actas Urol Esp. 1990;14:387–389. [Abstract] [PubMed] [Google Scholar]
- 5.Castillo Soria JL, Bravo de Rueda Accinelli C. Genital brucellosis. A rare cause of testicular abscess. [Article in Spanish] Arch Esp Urol. 1994;47:533–536. [Abstract] [PubMed] [Google Scholar]
- 6.Bayram MM, Kervancioğlu R. Scrotal gray-scale and color Doppler sonographic findings in genitourinary brucellosis. J Clin Ultrasound. 1997;25:443–447. doi: 10.1002/(sici)1097-0096(199710)25:8<443::aid-jcu6>3.0.co;2-j. CrossRef. [DOI] [PubMed] [Google Scholar]
- 7.González Sánchez FJ, Encinas Gaspar MB, Napal Lecumberri S, Rajab R. Brucellar orchiepididymitis with abscess. [Article in Spanish] Arch Esp Urol. 1997;50:289–292. [Abstract] [PubMed] [Google Scholar]
- 8.Akinci E, Bodur H, Cevik MA, Erbay A, Eren SS, Ziraman I. A complication of brucellosis: epididymoorchitis. Int J Infect Dis. 2006;10:171–177. doi: 10.1016/j.ijid.2005.02.006. CrossRef. [DOI] [PubMed] [Google Scholar]
- 9.Cosme A, Barrio J, Ojeda E, Ortega J, Tejada A. Sonographic findings in brucellar hepatic abscess. J Clin Ultrasound. 2001;29:109–111. doi: 10.1002/1097-0096(200102)29:2<109::AID-JCU1008>3.0.CO;2-P. CrossRef. [DOI] [PubMed] [Google Scholar]
- 10.Koc Z, Turunc T, Boga C. Gonadal brucellar abscess: imaging and clinical findings in 3 cases and review of the literature. J Clin Ultrasound. 2007;35:395–400. doi: 10.1002/jcu.20330. CrossRef. [DOI] [PubMed] [Google Scholar]
- 11.Yemisen M, Karakas E, Ozdemir I, Karakas O. Brucellar testicular abscess: a rare cause of testicular mass. J Infect Chemother. 2012;18:760–763. doi: 10.1007/s10156-011-0354-7. CrossRef. [DOI] [PubMed] [Google Scholar]
- 12.Akdeniz H, Irmak H, Seçkinli T, Buzgan T, Demiröz AP. Hematological manifestations in brucellosis cases in Turkey. Acta Med Okayama. 1998;52:63–65. doi: 10.18926/AMO/31333. [DOI] [PubMed] [Google Scholar]


