SUMMARY
Salbutamol-induced cardiac complications are well-established. Herein, we describe a case of a 24-year female who was admitted to the emergency department because of a suicide attempt with salbutamol (76 mg). Salbutamol abuse induced the development of supraventricular tachycardia and ventricular fibrillation. Regular sinus rhythm was restored with defibrillation. The hypokalemic patient who stayed in the intensive care unit was discharged after 48 hours of hospitalization.
Key words: Salbutamol, suicide, ventricular fibrillation
Introduction
Short-acting β-agonists are used in the management of intermittent asthma or chronic obstructive pulmonary disease (COPD) exacerbation.[1] Salbutamol shortens both the sinus cycle length and sinus node recovery time. In addition, it increases atrioventricular (AV) nodal conduction and reduces the AV nodal refractory time as well as myocardial refractoriness.[2] Over the past 40 years, it has been well-documented that β adrenergic agonists are associated with several cardiovascular adverse effects including ischemia, myocardial depression, atrial fibrillation (AF), ventricular arrhythmia, fatal myocardial band necrosis, and sudden cardiac death.[3]
In this article, we report a 24- year-old female case of suicide attempt with salbutamol, which caused ventricular fibrillation (VF) in the light of β adrenergic agonist-related side effects.
Case Report
A 24-year-old female case was admitted to the emergency department by her relatives due to a suicide attempt with salbutamol 76 mg (Ventolin 4 mgx19) four hours post attempt. The patient history revealed no known chronic disease. Upon admission, the patient had mild anxiety with a normal overall status and a Glasgow Coma Scale score of 15. Her arterial blood pressure was 110/60 mmHg, while her pulse rate, respiratory rate, and SPO2 was 126 bpm, and 18 min, 96%, respectively. The patient's heart sounds were rhythmic and tachycardic. Pulmonary auscultation revealed no rales or rhonchi and systemic examination indicated no pathology. The patient was monitored and an intravenous (I.V.) route was restored. Nasogastric decompression was performed and activated charcoal (50 g) was administered. Baseline electrocardiography (ECG) showed sinus tachycardia. Blood samples were collected for biochemistry tests and 0.9% NaCl was infused. Supraventricular tachycardia (SVT) developed at 30 minutes (Figure 1). A metoprolol tartarate-5 mg I.V. push was initiated to the patient without a history of bronchospasm. The patient was unresponsive to β blocker therapy and lost consciousness and developed ventricular fibrillation (Figure 2). Biphasic defibrillator at 200 Joules was used to restore regular heart rhythm. Spontaneous circulation was returned. The patient was in sinus rhythm following defibrillation. Biochemistry test results on admission were as follows: glucose 230 mg/dL, blood urea nitrogen 23.5 mg/dL, creatinine 0.74 mg/dL, aspartate aminotransferase 19 U/L, alanine amino transaminase 20 U/L, amylase 62 U/L, lipase 27 U/L, total bilirubin 0.24 mg/dL, sodium 139 mmol/L, potassium 2.7 mmol/L, chlorine 107 mmol/L, calcium 9.25 mg/dL, prothrombin time 11.7 sec, partial thromboplastin time 21.3 sec, international normalized ratio 1.05, white blood cells 12.76x103, hemoglobin: 12 g/dL, hematocrit: 37.2 RU, platelets 304.000, pH 7.38, HCO3std 21.6 mmol/L, K+ 2.3 mmol/L lactate 3 mg/dL, glucose 231 mg/dL, osmolarity 281 mOsm/kg. The hypokalemic patient was administered potassium infusion and hospitalized in the intensive care unit (ICU) for 48 hours. No malignant arrhythmia was observed during hospitalization. The patient followed in intensive care unit and discharged with the psychiatric consultation.
Figure 1.

Electrocardiography showing supraventricular tachycardia.
Figure 2.
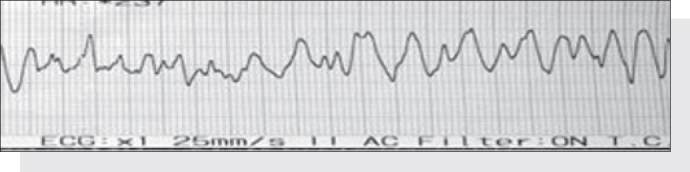
Electrocardiography showing ventricular fibrillation.
Discussion
In recent years, the incidence of suicide has been increasing worldwide. Infact, suicide is more prevalent among girls and young adults than males. Consistent with this, the incidence of suicide is 3.53/100 in men and 2.31/100 in women with rates in young adults (aged 15 to 24 years) of 4.58/100 in male individuals and 5.22/100 in female individuals according to the Turkish Statistical Institute (TurkStat).[4] kose et al.[5] also reported that women have a higher rate of suicide than men and the most commonly used method was drug or toxic agent use. In addition, some authors reported that the most frequently preferred agents for suicide attempt were analgesics followed by antidepressants, antipsychotics, and cardiovascular medications.[6] Similarly, our case was a female adult and admitted to the emergency service with suicide attempt with salbutamol.
Case-control studies showed that β-2 adrenergic agonists increased the risk of myocardial infarction (MI), congestive heart failure (CHF), cardiac arrest, and sudden cardiac death at varying degrees (odds ratio [OR] 1.3 to 3.4).7, 8 Single dose β-2 adrenergic agonist produced an increased heart rate by 9.12 bpm (confidence interval [CI] 95%, 5.32 to 12.92) compared to placebo. The cardiovascular side effects including major ones such as increased risk of sinus tachycardia (risk ratio [RR] 3.06; 95% CI; 1.7 to 5.5), ventricular tachycardia, AF, syncope, CHF, and sudden cardiac death were also increased with a β-2 adrenergic agonist than placebo (RR 2.54%; 95% CI; 0.18 to 0.54). The risk of major cardiovascular side effects was estimated as 1.61 (95%, CI 0.76 to 3.42), however; it did not reach statistical significance. In another study, β-2 adrenergic agonist was associated with ventricular and atrial ectopic heart beats and prolonged Q Tc interval.[8] Furthermore, sinus tachycardia and tachyarrhythmias were defined in several case reports.[9] In our case, we observed sinus tachycardia on admission and SVT followed by VF development. Fortunately, the patient responded to defibrillation.
In another study, single dose β-2 adrenergic agonist produced 0.36 mmol/L decrease in blood potassium level (95% CI, 0.18 to 0.54).[7] Hyperglycemia and hypotension were also among the side effects of the treatment. Additionally, hypokalemia was associated with increased risk of ventricular tachycardia and VF in susceptible patients.[10] Similarly, our case developed hypokalemia and hyperglycemia. After SVT, ventricular fibrillation developed during treatment. This can most likely be attributed to the hypokalemia of the patient. We believe that the increased adrenergic activity and hypokalemia combined facilitated the ventricular fibrillation.
Conclusion
In conclusion, β-2 adrenergic agonists at therapeutic doses may cause cardiac and metabolic side effects. Such effects may be considerably evident in patients with drug abuse. The patients with salbutamol abuse should be under medical supervision for the management of electrolyte disturbances and malignant arrhythmias.
Acknowledgments
The authors would like to thank Dr Hakan Sari for his contribution.
Conflict of Interest
The authors declare that there is no potential conflicts of interest.
Footnotes
Published online: March 07, 2015
References
- 1.National Asthma Education and Prevention Program: Expert panel report III: Guidelines for the diagnosis and management of asthma. Bethesda, MD: National Heart, Lung, and Blood Institute, 2007. (NIH publication no. 08–4051) www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm (Accessed on March 21, 2011).
- 2.Kallergis EM, Manios EG, Kanoupakis EM, Schiza SE, Mavrakis HE, Klapsinos NK. Acute electrophysiologic effects of inhaled salbutamol in humans. Chest. 2005;127:2057–2063. doi: 10.1378/chest.127.6.2057. CrossRef. [DOI] [PubMed] [Google Scholar]
- 3.Lulich KM, Goldie RG, Ryan G, Paterson JW. Adverse reactions to beta 2-agonist bronchodilators. Med Toxicol. 1986;1:286–299. doi: 10.1007/BF03259844. [DOI] [PubMed] [Google Scholar]
- 4.Coskun M, Zoroglu S, Ghaziuddin N. Suicide rates among Turkish and American youth: a cross-cultural comparison. Arch Suicide Res. 2012;16:59–72. doi: 10.1080/13811118.2012.640612. CrossRef. [DOI] [PubMed] [Google Scholar]
- 5.Köse A, Eraybar S, Köse B, Köksal Ö, Akköse Aydın Ş, Armağan E. Patients Over the Age of 15 Years Admitted for Attempted Suicide to the Emergency Department and the Psychosocial Support Unit. JAEM. 2012;11:193–196. CrossRef. [Google Scholar]
- 6.Andersen UA, Andersen M, Rosholm JU, Gram LF. Psychopharmacological treatment and psychiatric morbidity in 390 cases of suicide with special focus on affective disorders. Acta Psychiatr Scand. 2001;104:458–465. doi: 10.1034/j.1600-0447.2001.00191.x. CrossRef. [DOI] [PubMed] [Google Scholar]
- 7.Salpeter SR, Ormiston TM, Salpeter EE. Cardiovascular effects of beta-agonists in patients with asthma and COPD: a metaanalysis. Chest. 2004;125:2309–2321. doi: 10.1378/chest.125.6.2309. CrossRef. [DOI] [PubMed] [Google Scholar]
- 8.Cazzola M, Imperatore F, Salzillo A, Di Perna F, Calderaro F, Imperatore A. Cardiac effects of formoterol and salmeterol in patients suffering from COPD with preexisting cardiac arrhythmias and hypoxemia. Chest. 1998;114:411–415. doi: 10.1378/chest.114.2.411. CrossRef. [DOI] [PubMed] [Google Scholar]
- 9.Boucher A, Payen C, Garayt C, Ibanez H, Dieny A, Doche C. Salbutamol misuse or abuse with fatal outcome: a casereport. Hum Exp Toxicol. 2011;30:1869–1871. doi: 10.1177/0960327110388957. CrossRef. [DOI] [PubMed] [Google Scholar]
- 10.Nordrehaug JE, Johannessen KA, von der Lippe G. Serum potassium concentration as a risk factor of ventricular arrhythmias early in acute myocardial infarction. Circulation. 1985;71:645–649. doi: 10.1161/01.cir.71.4.645. CrossRef. [DOI] [PubMed] [Google Scholar]


