Abstract
Measurement-based care (MBC) can be defined as the practice of basing clinical care on client data collected throughout treatment. MBC is considered a core component of numerous evidence-based practices (e.g., Beck & Beck, 2011; Klerman, Weissman, Rounsaville, & Chevron, 1984) and has emerging empirical support as an evidence-based framework that can be added to any treatment (Lambert et al., 2003, Trivedi et al., 2007). The observed benefits of MBC are numerous. MBC provides insight into treatment progress, highlights ongoing treatment targets, reduces symptom deterioration, and improves client outcomes (Lambert et al., 2005). Moreover, as a framework to guide treatment, MBC has transtheoretical and transdiagnostic relevance with broad reach across clinical settings. Although MBC has primarily focused on assessing symptoms (e.g., depression, anxiety), MBC can also be used to assess valuable information about (a) symptoms, (b) functioning and satisfaction with life, (c) putative mechanisms of change (e.g., readiness to change), and (d) the treatment process (e.g., session feedback, working alliance). This paper provides an overview of the benefits and challenges of MBC implementation when conceptualized as a transtheoretical and transdiagnostic framework for evaluating client therapy progress and outcomes across these four domains. The empirical support for MBC use is briefly reviewed, an adult case example is presented to serve as a guide for successful implementation of MBC in clinical practice, and future directions to maximize MBC utility are discussed.
Keywords: measurement-based care, outcome monitoring, progress monitoring, feedback systems
The observation that it takes 17 years for only 14% of research to reach consumers (Balas & Boren, 2000) has prompted the scientific study of successful strategies for integrating evidence-based practices (EBPs) into real-world settings. Unfortunately, research suggests that clinicians may not use full-package, complex EBPs due to the burden associated with training, negative attitudes toward manuals or protocols, and beliefs that these EBPs may not be appropriate for clients in the settings in which they practice (e.g., Simons, Rozek, & Serrano, 2013). Moreover, research indicates that even if initially implemented with success, these complex EBPs are not likely to be sustained over time (Stirman et al., 2012). To address these barriers to full–package EBP implementation, Chorpita, Daleiden, and Weisz (2005) developed an innovative methodology for reviewing the treatment literature that focused on distilling EBPs down to their core or common practice elements (Chorpita et al., 2005). Outcomes of this distillation methodology have been used to develop modular treatment approaches that enable clinicians to systematically apply a variety of practice elements matched to client characteristics (PracticeWise, 2013; Weisz, Ugueto, et al., 2011). A second approach is the use of evidence-based practice frameworks such as the Collaborative Assessment and Management of Suicidality (CAMS; Jobes, 2006). Specifically, the CAMS framework encourages clinicians to continue treatment-as-usual while collaboratively engaging the client in open but semistructured communication to effectively manage and resolve suicidal ideation. Given the difficulties associated with implementing full-package EBPs, implementation of modular treatments or frameworks could serve as an effective and resource-efficient method for enhancing treatment as usual. Preliminary evidence suggests clinicians receive these approaches (Comtois et al., 2011) more favorably than full-package, manual-based approaches (e.g., Borntrager et al., 2009).
Measurement-Based Care
Incorporating systematic measurement of client outcomes into treatment has been referred to in the published literature as progress monitoring, outcome monitoring, measurement-based care, or the use of feedback systems (Bickman, 2008; Lambert, Harmon, Slade, Whipple, & Hawkins, 2005; Saggese, 2005; Trivedi et al., 2006; Valenstein et al., 2009). In many but not all cases, these terms refer to a process in which the clinician obtains client progress and outcome data by administering validated measures across treatment. Throughout this paper, we will adopt the term measurement-based care (MBC) to refer to a procedure that can be broadly defined as the use of systematic data collection to monitor client progress and directly inform care decisions (Morris & Trivedi, 2011; Trivedi et al., 2006). Preliminary research suggests that MBC, when used as a framework to guide practice, results in superior client outcomes when compared to usual care (Lambert et al., 2002). Given MBC’s potential to improve outcomes, it may be one of the minimum interventions necessary for change (MINC; e.g. Kessler & Glasgow, 2011) that could be implemented in lieu of more complex and burdensome full-package EBPs.
The goal of this paper is to highlight relevant literature that summarizes the effectiveness and applicability of MBC as a practice framework for enhancing usual care (Trivedi & Daly, 2007). The term “framework” is used to describe MBC given that it may be implemented in the context of many different treatment modalities or approaches. This paper addresses five specific aims: (a) to discuss the utility of MBC across stakeholder levels; (b) to discuss the broad reach and flexibility of MBC as a transtheoretical and transdiagnostic framework; (c) to expand MBC coverage across four domains (symptoms, life satisfaction, theorized mechanisms of change, and the therapeutic process) and provide resources for psychometrically validated measures; (d) to present a case example showcasing the utility of MBC for guiding treatment with complex adult clients; and (e) to elucidate potential challenges associated with MBC implementation.
MBC Utility Across Stakeholder Levels
Utility of MBC for Clients
Progress and outcome monitoring are key elements of numerous EBPs, including cognitive behavioral therapy (CBT; Beck & Beck, 2011) and interpersonal therapy (Klerman et al., 1984). Research has shown that adding MBC to usual care can result in significant improvement in client outcomes with respect to psychological disturbance, interpersonal problems, social role functioning, and quality of life, especially for clients identified as likely to experience treatment failure (Lambert et al., 2003). Additionally, youth clients with clinicians who received feedback about treatment progress have demonstrated faster improvement in symptoms than clients with clinicians who did not receive feedback (Bickman, Kelley, Breda, de Andrade & Riemer, 2011). MBC also appears to encourage the active involvement of clients in the treatment process. Eisen, Dickey, and Sederer (2000) demonstrated that clients assigned to clinicians who reviewed the self-report Behavior and Symptom Identification Scale in session were more likely to endorse a greater sense of involvement in decisions about treatment than clients receiving treatment as usual (i.e., no review of self-report symptom monitoring). Dowrick and colleagues (2009) found that clients who completed self-reports of depressive symptoms expressed that the measures allowed them to quantify their symptoms and gain a better understanding of their experience with depression.
Utility of MBC for Clinicians
These observed improvements in client outcomes have been tied to MBC’s role in alerting clinicians to lack of progress, which then encourages the clinician to alter the intervention accordingly (Lambert et al., 2003; Morris & Trivedi, 2011). That is, depending on the measure (e.g., established, psychometrically validated depression symptoms) or approach (e.g., idiographic assessment) used, MBC can provide important information about targets for clinician intervention. Moreover, MBC can streamline the assessment process and aid clinicians in making differential diagnoses (e.g., Kroenke, Spitzer, & Williams, 2001). Additional support for MBC suggests that it may be useful for enhancing the accuracy of clinician judgments by providing an objective assessment of client treatment progress (Sapyta, Riemer, & Bickman, 2005).
MBC may also be a valuable tool for facilitating collaborative care among providers within and across organizations. Katon and colleagues (2010) used a standardized depression measure to assess symptom severity in clients with comorbid depression and medical conditions, with results demonstrating that depression outcomes improved when scores were communicated to both the primary care physician and nurses involved in the client’s care. Additionally, the IMPACT trials found that improvement in depression outcomes occurred when the same depression measure was administered weekly and the attending psychiatrist used the data to make treatment recommendations across a team (nurse practitioners, case workers, etc.; Unützer et al., 2002).
Utility of MBC for Mental Health Organizations
If used routinely by all clinicians, MBC can also provide evaluative data for the organization and serve as an indicator of overall performance that can be reported to accreditation organizations (Bickman, 2008; Garland, Kruse, & Aarons, 2003). This performance assessment may then serve to inform funding decisions, provide additional quality-of-care management, and ultimately improve client care through the addition of new programs (Garland et al., 2003; Goebel, 1997). MBC may also encourage clinicians within organizations to follow standardized treatment guidelines, thereby maximizing the likelihood that evidence-based care is provided to all clients seeking mental health services (Trivedi & Daly, 2007).
The Broad Reach and Flexibility of the MBC Framework
Transtheoretical Relevance
There is emerging evidence that clinicians can implement MBC regardless of their theoretical orientation or training background. Clinicians who have participated in studies demonstrating MBC’s (also referred to as the use of feedback systems and outcome monitoring) effectiveness have had a variety of theoretical orientations, including CBT, psychodynamic, experiential, and eclectic. Clinicians in these studies have also had varying levels of experience, ranging from graduate students to experienced psychotherapists (Crits-Christoph et al., 2012; Harmon et al., 2007; Hawkins, Lambert, Vermeersch, Slade, & Tuttle, 2004; Lambert, Hansen, & Finch, 2001; Lambert et al., 2005; Slade, Lambert, Harmon, Smart, & Bailey, 2008). This preliminary evidence suggests that the MBC framework may not require clinicians to change their theoretical orientation, thereby eliminating a potential barrier to implementation.
Transdiagnostic Relevance
MBC’s reach is also extended due to its transdiagnostic relevance. MBC has been effectively conducted with youth (Athay & Bickman, 2012; Kelley & Bickman, 2009) and adults (Lambert et al., 2003). Moreover, appropriate measures exist to assess severity of depression (Gaynes et al., 2008; Kendrick et al., 2009; Kroenke & Spitzer, 2002; Simon, VonKorff, Rutter, & Wagner, 2000; Trivedi & Daly, 2007), bipolar disorder (Eisen, Normand, Belanger, Spiro, & Esch, 2004), anxiety (Spitzer, Kroenke, Williams, & Löwe, 2006), substance abuse (Crits-Christoph et al., 2012; Eisen et al., 2004), and comorbid mental health and medical conditions (Katon et al., 2010). MBC’s transdiagnostic relevance is clearly demonstrated in the work by Hawaii’s Child and Adolescent Mental Health System, which has implemented a monthly progress monitoring system with transdiagnostic treatment targets (Higa-McMillan, Powell, Daleiden, & Mueller, 2011; Nakamura, Daleiden, & Mueller, 2007).
Idiographic vs. Nomothetic Self-Report Assessment Procedures
Idiographic assessment procedures (e.g., a mood rating at the start of each session, live observation procedures) differ from nomothetic assessment procedures (e.g., client self-report measures that are standardized and have normative reference samples) as they provide the clinician with a way to individualize measurement-based care while allowing them to still employ psychometrically valid assessment techniques (Weisz, Chorpita, et al., 2011). Idiographic measures have proven useful for allowing clinicians to obtain data that can be used for case conceptualization and to guide treatment (Haynes, Mumma, & Pinson, 2009; Lyon, Borntrager, Nakamura, & Higa-McMillan, 2013; Weisz, Chorpita, et al., 2011). This approach allows tailoring of assessment targets, questions, and ratings to the needs, values, and skills of the client. Clinicians may opt to use idiographic assessments to complement or replace nomothetic self-report measures in order to maximally individualize care for both children and adults (McLeod, Jensen-Doss, & Ollendick, 2013). Thus, the use of idiographic assessment procedures further enhances the transtheoretical and transdiagnostic relevance of MBC. However, despite the benefits of idiographic assessment procedures (which includes practicality), there are inherent disadvantages including a lack of standardized administration and scoring (Jackson, 1999) that would allow for comparison across clients (including benchmarking with normative populations), clinicians, and organizations.
Substantial value has been placed on the application of nomothetic self-report and other-report measures because the client (or family member, teacher) can independently provide responses to identical questions over the course of treatment to assess nuanced changes using standardized response options that are consistent across measure administrations (Garber, Nau, Erickson, Aikens, & Lawrence, 2004). The use of validated nomothetic self–report measures enables clinicians to benchmark client scores with national averages and may promote the ease with which organizations can evaluate and compare treatment progress and outcomes across clients. However, nomothetic measures also have a number of disadvantages. First, nomothetic measures inherently are not tailored to each client’s problems. Second, nomothetic measures must be vetted to ensure they demonstrate strong psychometrics and sensitivity to change to capitalize on understanding change through repeated assessment across treatment. Taking the advantages and disadvantages of both approaches into account, the ideal MBC battery may consist of a combination of complementary idiographic and nomothetic assessment methods (McLeod et al., 2013).
Implementation of MBC: Expanding the Coverage of MBC Across Multiple Domains
MBC has historically been applied to evaluate client progress with respect to symptom change for both children and adults (e.g., Crits-Christoph et al., 2012; Kelley & Bickman, 2009; Lambert et al., 2003; Trivedi & Daly, 2007). However, assessment of additional domains including therapy process variables (e.g., therapeutic alliance), life satisfaction and functioning, and putative mechanisms of change might maximize the utility of MBC. Assessment across these particular domains would provide the clinician and client with additional information to guide treatment efforts and identify potential intervention targets (i.e., poor therapeutic alliance, low life satisfaction, lack of readiness to change). Below we provide brief overviews of these assessment domains and examples of validated measures for the purpose of enhancing the clarity of the clinical example. As a comprehensive review of measures is beyond the scope of this paper, clinicians interested in implementing MBC are encouraged to explore the resources provided below to find the assessment battery best matched to their clients and settings.
Symptom Severity
There are numerous reliable and valid self-report measures of symptoms both for specific disorders (e.g., depression, anxiety) and for more general symptoms (i.e., cross-diagnostic measures like the BASIS-24; Eisen et al., 2004). The goal of administering symptom measures is to characterize severity over the course of treatment. Some examples of brief, no-cost adult symptom measures, used below in the clinical example, include the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001), the Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006), and the Brief Phobia Scale (Department of Health, 2011). These scales assess common presenting problems (i.e., depression, anxiety disorders, phobias), aid in making differential diagnoses, and are sensitive to change. Examples of additional validated MBC appropriate self-report symptom measures for both children and adults may be found by consulting the PROMIS measures (Cella et al., 2007); those available at PracticeGround (PracticeGround, 2013); The Handbook of Psychiatric Measures (Rush, First, & Blacker, 2008); the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (5th edition) online symptom measures for adults and children (American Psychiatric Association, 2012); Mental Health Outcome Measures for Children and Young People (Deighton & Wolpert, 2010); and those in The Practitioner’s Guides to Empirically Based Measures of Depression and Anxiety (Antony, Orsillo, & Roemer, 2001; Nezu, Ronan, Meadows, & McClure, 2002).
Quality of Life, Life Satisfaction, and Functioning
While symptom change often remains the primary goal of treatment, quality of life, life satisfaction, and role functioning have also been prioritized to achieve the goal of mental health and not simply absence of mental illness. Quality of life is a commonly used metric for assessing the cost utility of treatment and thus may be included within an MBC battery designed to promote mental health. Changes in life satisfaction occur over the course of treatment for certain clients (Pavot & Diener, 1993) and can be reliably and validly assessed with as few as five items (Diener, Emmons, Larsen, & Griffin, 1985). Assessing improvement in role functioning is also critical, especially when the goal of treatment is to assist the client in obtaining employment and moving away from disability services (Comtois, Kerbrat, Atkins, Harned, & Elwood, 2010). Reviews of psychometrically validated measures for this domain exist for both children (Huebner, 2004) and adults (e.g., Eiser & Morse, 2001; McDowell, 2006; Thornicroft & Tansella, 2010).
Putative Mechanisms of Change: Readiness to Change
A body of literature has emerged seeking to identify mechanisms of change that promote symptom improvement (Kazdin, 2007). By systematically assessing changes in theorized mechanisms, clinicians may be able to identify treatment targets. One proposed mechanism is the client’s readiness to change, which is a transtheoretical model characterized by four stages through which clients purportedly move over the course of treatment: precontemplation, contemplation, action, and maintenance (Prochaska & DiClemente, 1983). Literature suggests that clients entering treatment in the precontemplation stage are more likely to drop out (e.g., May et al., 2007), whereas CBT effectiveness is mediated by increases in the client’s action orientation (Lewis et al., 2009). Systematic assessment of the client’s readiness to change (using the Stages of Change Scale; McConnaughy, Prochaska, & Velicer, 1983) may allow clinicians to match interventions to a client’s current stage of readiness (Prochaska & DiClemente, 1983). Unfortunately, there is a dearth of literature to guide the exploration of mechanisms of change; therefore, we direct the reader to a review of studies of readiness to change for both children and adolescents (e.g., Norcross, Krebs, & Prochaska, 2011) as well as seminal articles denoting the importance of this understudied area and recommendations for improvement (e.g., Kazdin, 2006; Kazdin & Nock, 2003).
Feedback About the Therapy Process
Therapy process variables, such as the therapeutic alliance, have also been identified as critical to achieving treatment success (Barber, Connolly, Crits-Christoph, Gladis & Siqueland, 2009; Feeley, DeRubeis, & Gelfand, 1999); a positive correlation between the alliance and symptom change across therapy has been consistently observed, regardless of the type of therapy or client presenting problem (Castonguay, Constantino, & Holtforth, 2006). Assessment of the alliance via self-report (e.g., using the Working Alliance Short Form; WAI-S; Tracey & Kokotovic, 1989) may be especially important for both child and adult psychotherapy (Elvins & Green, 2008), although observer and clinician reports may also be useful for gauging the quality of the alliance (see Martin, Garske, & Davis, 2000).
Practice Monitoring with MBC
Maximizing the utility and effectiveness of MBC may ultimately be achieved through simultaneous clinician practice monitoring. For instance, a clinician may wish to monitor the effects of individual practice elements (e.g., activity scheduling within a CBT treatment protocol) on client change across a variety of domains (i.e., symptoms, life satisfaction, etc.). Systematic assessment of progress (or lack thereof) can then be linked to specific interventions to inform future clinical decisions (Chorpita, Bernstein, Daleiden, & Research Network on Youth Mental Health, 2008). PracticeWise (a modular based treatment approach for youth) includes use of a clinician dashboard for this exact purpose. Unfortunately, not all MBC systems include this multilevel assessment, and clinicians may need to rely on progress notes or memory to make these important connections between interventions and client change.
A Case Example Illustrating the Clinical Utility of MBC
In order to promote MBC implementation, what follows is a fictional account that draws upon the current paper’s conceptualization of MBC as an EBP framework. It is important to note that while our example focuses on adult mental health treatment, MBC may also be applied successfully to assess children and adolescents with appropriate measures matched to these populations (see Bickman et al., 2011). The clinical example centers on Joanne, a relatively new master’s-level clinician, who has quickly grown a caseload of 40 clients consisting of primarily adults suffering from anxiety and depression with complicated life contexts (e.g., histories of abuse, living in poverty). After attending a mandated training, Joanne decided to try MBC with a new case: Stephanie, a 52-year-old married Caucasian mother of three who presented with complaints of depression. Prior to the diagnostic interview, Joanne had Stephanie complete the PHQ-9, GAD-7, phobia and functioning questions, Readiness to Change, and Satisfaction with Life Scales. During the evaluation, Stephanie primarily wished to discuss the exacerbation of her depressive symptoms, the recent cancer diagnosis her mother received, and the financial and marital problems she faced at home. She expressed feeling “worried” and said she was “shy” but denied “atypical” fears of social situations and stated she really, “just needed help finding the energy to get chores done at home.” The PHQ-9 score confirmed moderately severe depression (total score = 19), but the GAD-7 suggested that Stephanie suffered from severe worry (total score = 20) and her responses to the phobia questions indicated she might struggle with social phobia (score of “8” on the social phobia question). Stephanie’s satisfaction with life fell well below national averages (total score = 9) and she appeared to be contemplating change but not ready to take action (total score on the contemplation subscale = 4).
Based on Stephanie’s verbal account, Joanne hypothesized that Stephanie’s recent experience with life stress had precipitated depressive symptoms that manifested in avoidance behaviors (e.g., missing work, avoiding chores at home) and diminished levels of reinforcement from her environment. However, when Joanne combined Stephanie’s verbal account with information obtained from the self-reports, she generated an alternative hypothesis that Stephanie might also be struggling with social anxiety. She wondered whether Stephanie’s avoidance behaviors could be better explained by a lack of assertiveness and excessive fears of being negatively evaluated.
Joanne asked additional questions to explore this alternative hypothesis in the first session. Joanne learned that Stephanie had suffered from severe social phobia for the majority of her life, which indeed manifested in a passive interaction style preceded and followed by catastrophic interpretations of events, rumination, and worry. Subsequently, Joanne hypothesized that Stephanie’s social phobia might be driving her depression and she posited that initially targeting the social phobia in treatment might ultimately reduce both her anxiety and depression symptoms and improve her satisfaction with life. However, Stephanie was reluctant to receive the social phobia diagnosis and was hesitant to pursue social phobia treatment.
Joanne respected Stephanie’s wishes and began treatment by drawing from available behavioral activation for depression protocols (e.g., Martell, Addis, & Jacobson, 2001). She decided to administer the PHQ-9 and GAD-7 prior to each session with Stephanie. The first two sessions focused on psychoeducation and data collection via mood and behavior monitoring (e.g., sleep patterns, daily experience with pleasure, avoidance patterns). The next five sessions focused on activity scheduling (to increase mastery, pleasure, physical activities, and feelings of closeness), and Stephanie kept an hourly log describing her activities and used an idiographic measure to log depression severity (on a 0 to 10 scale, with 10 reflecting “severely depressed”). For instance, Stephanie had wanted to go back to school to become an administrative assistant but was anxious about attending classes with “kids” and instead enrolled in an online computer-training course to prepare. She also wished to begin playing tennis again and considered taking lessons at the YMCA. However, in Session eight, Joanne and Stephanie completed TRAP (Trigger, Response, Avoidance Pattern; Dimidjian, Martell, Addis, & Herman-Dunn, 2008) logs for each activity she had failed to initiate and uncovered that these activities triggered Stephanie’s fears about negative evaluation, ultimately leading her to avoid her homework.
By Session nine, Stephanie’s PHQ-9 (total score = 18) and GAD-7 (total score = 20) scores had not improved (see Figure 1), and she had endorsed a score of “1” on the PHQ-9 item nine, indicating she had thoughts she would be better off dead. Moreover, despite Joanne’s efforts to help Stephanie engage in alternative coping, Stephanie provided countless reasons for why the activities would not work. Joanne opted to seek supervision for this complex case. Joanne’s supervisor highlighted the lack of clinically significant change and then asked Joanne to readminister the satisfaction with life scale and discuss the apparent lack of progress and emergence of suicidal or morbid ideation with Stephanie in the next session.
Figure 1.
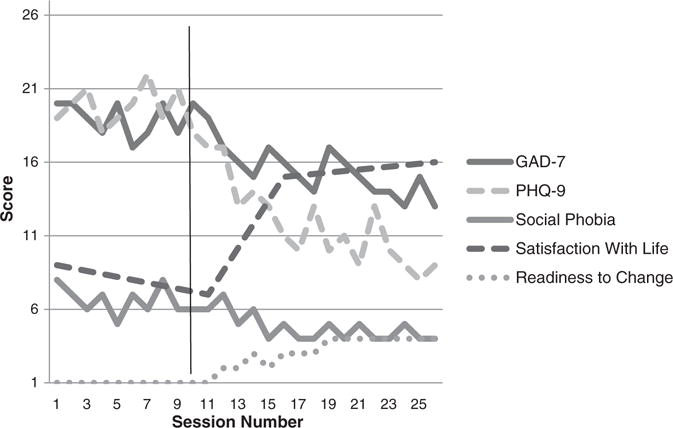
Measurement Based Care Scale Total Score Trajectories for Sample Client: Stephanie. Lower scores on the GAD-7 (Generalized Anxiety Disorder 7-items), PHQ-9 (Patient Health Questionnaire 9-items; Depressive severity measure), and Social Phobia scale indicate clinical improvement. Conversely, higher scores on the Satisfaction with Life Scale and Readiness to Change (specifically Action) Scale indicate improvement. The vertical line at Session 10 depicts a change in the treatment plan to focus on social phobia, whereas the previous sessions focused on depression. Session 11 involved Motivational Interviewing techniques targeting the low Action scores on the Stages of Change Scale.
Joanne compiled the self-report data and shared graphs of Stephanie’s scores at the beginning of Session 10. After confirming that these scores reflected Stephanie’s personal experience, Joanne revisited her initial conceptualization that social phobia was driving Stephanie’s depression. Joanne used guided discovery to discuss the scores (the decline in her life satisfaction, and the emergence of morbid ideation) alongside Stephanie’s attempts at behavioral activation (e.g., tennis lessons, online computer training) and the TRAP data. Joanne engaged Stephanie in social phobia psychoeducation, which resonated with her interpersonal struggles. Stephanie agreed that a change in the treatment plan might be appropriate.
At the beginning of the next session, along with the PHQ-9 and the GAD-7, Joanne administered the Stages of Change Scale and the Working Alliance Inventory because she anticipated that Stephanie might struggle to embrace this new treatment trajectory. Stephanie’s readiness to change score indicated that she had regressed into the precontemplative stage of change (total score on the precontemplation subscale = 4), but that she viewed the alliance to be strong. Based on the readiness to change data, Joanne elected to use Motivational Interviewing to increase Stephanie’s motivation. Stephanie reported that she was mostly fearful that she would be unable to change because she had lived a “lifetime” with social phobia, but that she truly wished to change and she trusted Joanne to serve as a supportive guide.
The next session focused on developing an exposure hierarchy. Developing the hierarchy was illuminative for both Joanne and Stephanie because it revealed a profound pervasiveness of her social anxiety. Stephanie reported difficulty leaving her house for fear she would have an unplanned interaction with one of her many neighbors. Stephanie approached the next five sessions, which focused on developing cognitive restructuring skills, with curiosity and motivation (evidenced by higher scores on the contemplation subscale of the stages of change scale). However, she then missed a session when it became time to engage in exposures. Fortunately, the therapeutic alliance remained strong, and Stephanie returned the next session, apologizing for her “moment of weakness.” Joanne presented an updated graph with data from the self-reports, which demonstrated that Stephanie had recently experienced improvement in her life satisfaction and a clinically significant change in her GAD-7 and PHQ-9 scores (see Figure 1). This data reinvigorated Stephanie’s commitment to treatment. Stephanie’s readiness to change scores revealed her new action orientation (highest scale score of 4), which Joanne highlighted for her as a good prognostic indicator.
Figure 1 depicts Stephanie’s scores across the duration of treatment (total of 25 sessions with the first 10 focused on behavioral activation). Joanne used this data during their termination planning sessions to help Stephanie understand that peaks and valleys are typical and will continue to occur, and that valleys often coincide with life stressors or challenging situations (e.g., avoiding a valued activity). Joanne also indicated that long periods (e.g., three weeks) of elevated symptom scores were indicative that changes needed to be made. Joanne provided Stephanie with several copies of the self-reports they used (e.g., PHQ-9 and GAD-7) to help her monitor her own symptoms and to guide self-therapy once they terminated. She educated Stephanie regarding how to score the measures and when scores would serve as signs that she might want to revisit her skills or even pursue “booster” therapy sessions. In sum, Joanne was able to leverage MBC to aid in the diagnosis and conceptualization, identify treatment targets, capture lack of progress, appropriately seek out supervision, and adapt treatment to fit Stephanie’s needs.
Challenges in Implementing MBC
Time Restrictions
Despite the numerous potential benefits to using MBC, clinicians are often faced with the challenge of maintaining a heavy caseload that is largely constrained by time limitations. Such time restrictions have been shown to deter both clinicians and agency directors from employing EBPs, despite acknowledging their potential clinical utility (Proctor et al., 2007). It is possible that administration of brief measures may actually streamline treatment by creating a quick method for asking questions that clinicians report are already being assessed (Scott & Lewis, 2014). Advances in technology may help circumvent this time burden by enabling clients to complete assessment measures prior to session on handheld devices in the waiting room (Goldstein et al., 2011). However, even with the use of computerized assessments, the review and interpretation of MBC results may add time-consuming steps to the treatment process.
Organizational Resources
Even with the ability to overcome time constraints, limited organizational resources including finances, measure and technology access, and supervisory support may limit the implementation of MBC (Bickman, 2008; Scott & Lewis, 2014). Large-scale monitoring systems that leverage technology for data collection may be difficult to implement within organizations that lack financial backing and management support (Fixsen, 2005). However, MBC can be implemented on a scale that is appropriately matched to each setting if value is placed on incorporating this practice. For example, clinicians who work in settings where technology is limited may use paper-and-pencil versions of validated measures or idiographic measures to assess client progress. Moreover, numerous no-cost validated nomothetic instruments are available and may be used in lieu of more expensive, copyrighted measures. A list of free measures can be found in the review paper included in this journal’s special section (Beidas et al., 2015–in this issue). Overall, organizational resources may significantly limit the type and extent of MBC that can be implemented; however, small efforts to apply MBC (i.e., monitoring symptom change using idiographic assessments) may be beneficial for improving client outcomes (Weisz, Chorpita, et al., 2011).
Client Complexity
Despite the broad applicability of MBC, clients in community settings often present with complex challenges (Aarons & Palinkas, 2007). Clinicians have expressed that some clients may not be capable of completing the measures or that certain measures may not be a good fit for clients with multiple diagnoses due to their focused nature (i.e., measure focused solely on depression, anxiety, etc.; Scott & Lewis, 2014). However, clinicians can work to establish an MBC protocol (which might include only idiographic assessments) that best fits the client’s case conceptualization, preferences, and treatment status. Another solution would be to adopt a multifaceted assessment tool that covers a range of symptoms and functioning such as the OQ-45 feedback system (Lambert et al., 2005) or the BASIS-24 self-report measure (Eisen et al., 2004).
Establishing MBC Implementation Procedures
Another potential challenge is the need for an understanding of the logistics and procedures necessary for administration and review of validated measures, as well as for using MBC to guide clinical decision-making. Although clinicians may be able to independently implement MBC, training efforts and organizational support to (a) establish the utility of self-report assessment, (b) delineate frequency of administration and review of measures, (c) identify methods for optimizing data collection (i.e., use of technology), and (d) establish procedures for using MBC to make clinical judgments and guide treatment may be important to ensure successful implementation of MBC (Slade, Thornicroft, & Glover, 1999; Trivedi et al., 2007). Organizations seeking to implement MBC procedures may wish to consider providing targeted training to optimize MBC’s utility. Beyond simply training clinicians in the application of MBC, training may also be important to build buy-in for MBC implementation, as negative attitudes about evidence-based practices may limit their application (Aarons et al., 2012; Jensen-Doss & Hawley, 2010). Preliminary data suggest that MBC can be successfully introduced to clinicians using the theory of planned behavior (see Casper, 2007), which attempts to promote attitude and behavior change. However, few established protocols (or trainings) exist for using MBC to guide clinical decision–making in the context of psychotherapy. PracticeWise (2013) uses a clinical dashboard technology that integrates practice element and outcome monitoring and draws upon the literature (through complex algorithms that interact within their database) to guide clinicians in selecting evidence-based practice elements. In the event that clinical decision support systems like PracticeWise are not feasible, training in a case formulation–based approach might be necessary to guide the integration of MBC with clinician treatment planning. Regardless, emerging evidence demonstrates that simply providing the infrastructure for MBC improves client outcomes, thereby suggesting that this framework has great promise for enhancing usual care.
Limitations and Future Directions
This overview attempted to define MBC and extend its reach by highlighting its transtheoretical and transdiagnostic relevance, expanding MBC assessment domains (beyond symptoms to also include practice monitoring), and providing an example of MBC implementation for complex clinical adult cases. However, it is important to note that both self-report and idiographic measures have limitations with respect to accurate assessment of client experiences. Both assessment measures assume that clients have insight into their experiences, and that they are willing to share this information with the clinician. Additionally, clinicians must ensure that the self-report measures they implement are psychometrically strong, and that individualized idiographic measures are applied in a consistent manner across treatment to maximize accuracy. Despite these limitations, these assessments may provide an avenue for communication between the client and clinician.
Additionally, since component analyses, dismantling studies, and sequential multiple assignment research trials (SMART; e.g., Almirall, Compton, Gunlicks-Stoessel, Duan, & Murphy, 2012) have yet to be conducted, we cannot conclude that MBC is an ideal framework for stand-alone implementation. There are important unanswered questions regarding how best to leverage MBC as a clinical decision aid. It is also possible that other evidence-based frameworks or practice elements may be equally or more effective for enhancing usual care. Even so, MBC may be a logical first step as it can provide the infrastructure and data necessary to evaluate the effect of gradually introducing other practice elements or full package EBPs.
Conclusions
MBC can be conceptualized as an EBP framework that involves systematic assessment of therapy progress and outcome to guide and adapt treatment. MBC has been shown to improve clinical outcomes, inform collaborative care efforts, enhance treatment decision-making processes, and increase client engagement in therapy. MBC can also be adapted to fit the context of the organization by matching psychometrically sound measures of appropriate length and content to the needs of clients receiving care. MBC shows great promise as a transdiagnostic and transtheoretical framework that may be useful for enhancing treatment-as-usual. However, additional research is needed to substantiate the effectiveness of MBC as a stand-alone framework and establish MBC implementation strategies. Despite this need for further research, this paper may serve as a starting point for clinicians interested in adding evidence-based frameworks such as MBC to their repertoire of clinical skills.
Acknowledgments
The authors would like to acknowledge and thank Dr. Jacqueline Persons for her consultation and feedback regarding the conceptualization of the paper, particularly with respect to the development of the clinical case example.
Contributor Information
Kelli Scott, Indiana University.
Cara C. Lewis, Indiana University and University of Washington
References
- Aarons GA, Glisson C, Green PD, Hoagwood K, Kelleher KJ, Landsverk J. The organizational social context of mental health services and clinician attitudes toward evidence-based practice: a United States national study. Implementation Science. 2012;7(1):56. doi: 10.1186/1748-5908-7-56. http://dx.doi.org/10.1186/1748-5908-7-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Palinkas LA. Implementation of evidence-based practice in child welfare: Service provider perspectives. Administration and Policy in Mental Health and Mental Health Services Research. 2007;34(4):411–419. doi: 10.1007/s10488-007-0121-3. http://dx.doi.org/10.1007/s10488-007-0121-3. [DOI] [PubMed] [Google Scholar]
- Almirall D, Compton SN, Gunlicks-Stoessel M, Duan N, Murphy SA. Designing a pilot sequential multiple assignment randomized trial for developing an adaptive treatment strategy. Statistics in Medicine. 2012;31(17):1887–1902. doi: 10.1002/sim.4512. http://dx.doi.org/10.1002/sim.4512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Online assessment measures. 2012 Retrieved from. http://www.psychiatry.org/practice/dsm/dsm5/online-assessment-measures#Level1.
- Antony MM, Orsillo SM, Roemer L, editors. Practitioner’s guide to empirically based measures of anxiety. New York: Kluwer Academic/Plenum; 2001. [Google Scholar]
- Athay MM, Bickman L. Development and psychometric evaluation of the youth and caregiver Service Satisfaction Scale. Administration and Policy in Mental Health and Mental Health Services Research. 2012;39(1–2):71–77. doi: 10.1007/s10488-012-0407-y. http://dx.doi.org/10.1007/s10488-012-0407-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearbook of Medical Informatics. 2000:65–70. [PubMed] [Google Scholar]
- Barber JP, Connolly MB, Crits-Christoph P, Gladis L, Siqueland L. Alliance predicts patients’ outcome beyond in-treatment change in symptoms. Personality Disorders: Theory, Research, and Treatment. 2009;(1):80–89. doi: 10.1037//0022-006x.68.6.1027. http://dx.doi.org/10.1037/1949-2715.S.1.80. [DOI] [PubMed]
- Beck JS, Beck AT. Cognitive behavior therapy: Basics and beyond. New York: Guilford Press; 2011. [Google Scholar]
- Beidas RS, Stewart RE, Walsh L, Lucas S, Downey MM, Jackson K, Mandell DS. Free, brief, and validated: Standardized instruments for low-resource mental health settings. Cognitive and Behavioral Practice. 2015;22(1):5–19. doi: 10.1016/j.cbpra.2014.02.002. in this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickman L. A measurement feedback system (MFS) is necessary to improve mental health outcomes. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(10):1114. doi: 10.1097/CHI.0b013e3181825af8. http://dx.doi.org/10.1097/CHI.0b013e3181825af8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickman L, Kelley SD, Breda C, de Andrade AR, Riemer M. Effects of routine feedback to clinicians on mental health outcomes of youths: Results of a randomized trial. Psychiatric Services. 2011;62(12):1423–1429. doi: 10.1176/appi.ps.002052011. http://dx.doi.org/10.1176/appi.ps.002052011. [DOI] [PubMed] [Google Scholar]
- Borntrager C, Chorpita B, Higa-McMillan C, Weisz J. Provider attitudes toward evidence-based practices: Are the concerns with the evidence or with the manuals? Psychiatric Services. 2009;60(5):677–681. doi: 10.1176/ps.2009.60.5.677. http://dx.doi.org/10.1176/appi.ps.60.5.677. [DOI] [PubMed] [Google Scholar]
- Casper E. The theory of planned behavior applied to continuing education for mental health professionals. Psychiatric Services. 2007;58(10):1324–1329. doi: 10.1176/ps.2007.58.10.1324. http://dx.doi.org/10.1176/appi.ps.58.10.1324. [DOI] [PubMed] [Google Scholar]
- Castonguay LG, Constantino MJ, Holtforth MG. The working alliance: Where are we and where should we go? Psychotherapy. 2006;43(3):271. doi: 10.1037/0033-3204.43.3.271. http://dx.doi.org/10.1037/0033-3204.43.3.271. [DOI] [PubMed] [Google Scholar]
- Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, Rose M. The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Medical Care. 2007;45(5):S3. doi: 10.1097/01.mlr.0000258615.42478.55. http://dx.doi.org/10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Bernstein AD, Daleiden EL, the Research Network on Youth Mental Health Driving with roadmaps and dashboards: Using information resources to structure the decision models in service organizations. Administration and Policy in Mental Health and Mental Health Services Research. 2008;35:114–123. doi: 10.1007/s10488-007-0151-x. http://dx.doi.org/10.1007/s10488-007-0151-x. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Weisz JR. Identifying and selecting the common elements of evidence based interventions: A distillation and matching model. Mental Health Services Research. 2005;7(1):5–20. doi: 10.1007/s11020-005-1962-6. http://dx.doi.org/10.1007/s11020-005-1962-6. [DOI] [PubMed] [Google Scholar]
- Comtois KA, Jobes DA, S O’Connor S, Atkins DC, Janis K, E Chessen C, Yuodelis-Flores C. Collaborative assessment and management of suicidality (CAMS): feasibility trial for next-day appointment services. Depression and Anxiety. 2011;28(11):963–972. doi: 10.1002/da.20895. http://dx.doi.org/10.1002/da.20895. [DOI] [PubMed] [Google Scholar]
- Comtois KA, Kerbrat AH, Atkins D, Harned M, Elwood L. Recovery from disability for individuals with borderline personality disorder: A feasibility trial of DBT-ACES. Psychiatric Services. 2010;61(11):1106–1111. doi: 10.1176/ps.2010.61.11.1106. http://dx.doi.org/10.1176/appi.ps.61.11.1106. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Ring-Kurtz S, Hamilton JL, Lambert MJ, Gallop R, McClure B, Rotrosen J. A preliminary study of the effects of individual patient-level feedback in outpatient substance abuse treatment programs. Journal of Substance Abuse Treatment. 2012;42(3):301–309. doi: 10.1016/j.jsat.2011.09.003. http://dx.doi.org/10.1016/j.jsat.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deighton J, Wolpert M. Mental health outcome measures for children and young people. London: Anna Freud Centre/UCL; 2010. [Google Scholar]
- Department of Health. IAPT Data Handbook version 2. 2011 Available at www.iapt.nhs.uk.
- Diener ED, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. Journal of Personality Assessment. 1985;49(1):71–75. doi: 10.1207/s15327752jpa4901_13. http://dx.doi.org/10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Martell CR, Addis ME, Herman-Dunn R. Behavioral activation for depression. In: Barlow D, editor. Clinical handbook of psychological disorders A step-by-step treatment manual. New York: Guilford Press; 2008. pp. 328–364. [Google Scholar]
- Dowrick C, Leydon GM, McBride A, Howe A, Burgess H, Clarke P, Kendrick T. Patients’ and doctors’ views on depression severity questionnaires incentivised in UK quality and outcomes framework: qualitative study. BMJ. 2009;338 doi: 10.1136/bmj.b663. http://dx.doi.org/10.1136/bmj.b663. [DOI] [PubMed] [Google Scholar]
- Eisen SV, Dickey B, Sederer LI. A self-report symptom and problem rating scale to increase inpatients’ involvement in treatment. Psychiatric Services. 2000;51(3):349–353. doi: 10.1176/appi.ps.51.3.349. [DOI] [PubMed] [Google Scholar]
- Eisen SV, Normand SL, Belanger AJ, Spiro A, Esch D. The revised Behavior and Symptom Identification Scale (BASIS-R): Reliability and validity. Medical Care. 2004:1230–1241. doi: 10.1097/00005650-200412000-00010. [DOI] [PubMed] [Google Scholar]
- Eiser C, Morse R. A review of measures of quality of life for children with chronic illness. Archives of Disease in Childhood. 2001;84(3):205–211. doi: 10.1136/adc.84.3.205. http://dx.doi.org/10.1136/adc.84.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elvins R, Green J. The conceptualization and measurement of therapeutic alliance: An empirical review. Clinical Psychology Review. 2008;28(7):1167–1187. doi: 10.1016/j.cpr.2008.04.002. http://dx.doi.org/10.1016/j.cpr.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Feeley M, DeRubeis RJ, Gelfand LA. The temporal relation of adherence and alliance to symptom change in cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67(4):578. doi: 10.1037//0022-006x.67.4.578. http://dx.doi.org/10.1037/0022-006X.67.4.578. [DOI] [PubMed] [Google Scholar]
- Fixsen DL. Implementation research: A synthesis of the literature. National Implementation Research Network; 2005. [Google Scholar]
- Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: A summary of the literature. Medical Care. 2004;42(7):649–652. doi: 10.1097/01.mlr.0000129496.05898.02. [DOI] [PubMed] [Google Scholar]
- Garland AF, Kruse M, Aarons GA. Clinicians and outcome measurement: What’s the use? The Journal of Behavioral Health Services & Research. 2003;30(4):393–405. doi: 10.1007/BF02287427. http://dx.doi.org/10.1007/BF02287427. [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Trivedi MH, McGrath PJ, Thase ME, Klinkman M, Nierenberg AA, Fava M. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: Results from STAR* D. Journal of General Internal Medicine. 2008;23(5):551–560. doi: 10.1007/s11606-008-0522-3. http://dx.doi.org/10.1007/s11606-008-0522-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goebel LJ. A peer review feedback method of promoting compliance with preventive care guidelines in a resident ambulatory care clinic. The Joint Commission Journal on Quality Improvement. 1997;23(4):196. doi: 10.1016/s1070-3241(16)30309-1. [DOI] [PubMed] [Google Scholar]
- Goldstein LA, Connolly Gibbons MB, Thompson SM, Scott K, Heintz L, Green P. Outcome assessment via handheld computer in community mental health: consumer satisfaction and reliability. Journal of Behavioral Health Services & Research. 2011;38(3):414–423. doi: 10.1007/s11414-010-9229-4. http://dx.doi.org/10.1007/s11414-010-9229-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmon SC, Lambert MJ, Smart DM, Hawkins E, Nielsen SL, Slade K, Lutz W. Enhancing outcome for potential treatment failures: Therapist–client feedback and clinical support tools. Psychotherapy Research. 2007;17(4):379–392. http://dx.doi.org/10.1080/10503300600702331. [Google Scholar]
- Hawkins EJ, Lambert MJ, Vermeersch DA, Slade KL, Tuttle KC. The therapeutic effects of providing patient progress information to therapists and patients. Psychotherapy Research. 2004;14(3):308–327. http://dx.doi.org/10.1093/ptr/kph027. [Google Scholar]
- Haynes SN, Mumma GH, Pinson C. Idiographic assessment: Conceptual and psychometric foundations of individualized behavioral assessment. Clinical Psychology Review. 2009;29(2):179–191. doi: 10.1016/j.cpr.2008.12.003. http://dx.doi.org/10.1016/j.cpr.2008.12.003. [DOI] [PubMed] [Google Scholar]
- Higa-McMillan CK, Powell CKK, Daleiden EL, Mueller CW. Pursuing an evidence-based culture through contextualized feedback: Aligning youth outcomes and practices. Professional Psychology: Research and Practice. 2011;42(2):137–144. http://dx.doi.org/10.1037/a0022139. [Google Scholar]
- Huebner ES. Research on assessment of life satisfaction of children and adolescents. Social Indicators Research. 2004;66(1–2):3–33. http://dx.doi.org/10.1023/B:SOCI.0000007497.57754.e3. [Google Scholar]
- Jackson JL. Psychometric considerations in self-monitoring assessment. Psychological assessment. 1999;11(4):439. http://dx.doi.org/10.1037/1040-3590.11.4.439. [Google Scholar]
- Jensen-Doss A, Hawley KM. Understanding barriers to evidence-based assessment: Clinician attitudes toward standardized assessment tools. Journal of Clinical Child & Adolescent Psychology. 2010;39(6):885–896. doi: 10.1080/15374416.2010.517169. http://dx.doi.org/10.1080/15374416.2010.517169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobes DA. Managing suicidal risk: A collaborative approach. New York: Guilford Press; 2006. [Google Scholar]
- Katon WJ, Lin EHB, Von Korff M, Ciechanowski P, Ludman EJ, Young B, McCulloch D. Collaborative care for patients with depression and chronic illnesses. New England Journal of Medicine. 2010;363(27):2611–2620. doi: 10.1056/NEJMoa1003955. http://dx.doi.org/10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE. Mechanisms of change in psychotherapy: advances, breakthroughs, and cutting-edge research (do not yet exist) In: Bootzin RR, McKnight PE, editors. Strengthening research methodology: Psychological measurement and evaluation. Washington, DC: American Psychological Association; 2006. http://dx.doi.org/10.1037/11384-005. [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. http://dx.doi.org/10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. http://dx.doi.org/10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kelley SD, Bickman L. Beyond outcomes monitoring: Measurement feedback systems (MFS) in child and adolescent clinical practice. Current Opinion in Psychiatry. 2009;22(4):363. doi: 10.1097/YCO.0b013e32832c9162. http://dx.doi.org/10.1097/YCO.0b013e32832c9162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendrick T, Dowrick C, McBride A, Howe A, Clarke P, Maisey S, Smith PW. Management of depression in UK general practice in relation to scores on depression severity questionnaires: analysis of medical record data. British Medical Journal. 2009;338 doi: 10.1136/bmj.b750. http://dx.doi.org/10.1136/bmj.b750. [DOI] [PubMed] [Google Scholar]
- Kessler R, Glasgow RE. A proposal to speed translation of healthcare research into practice: dramatic change is needed. American Journal of Preventive Medicine. 2011;40(6):637–644. doi: 10.1016/j.amepre.2011.02.023. http://dx.doi.org/10.1016/j.amepre.2011.02.023. [DOI] [PubMed] [Google Scholar]
- Klerman GL, Weissman MM, Rounsaville BJ, Chevron ES. Interpersonal psychotherapy of depression. New York: Basic Books; 1984. [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32(9):1–7. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert MJ, Hansen NB, Finch AE. Patient-focused research: Using patient outcome data to enhance treatment effects. Journal of Consulting and Clinical Psychology. 2001;69(2):159. http://dx.doi.org/10.1037/0022-006X.69.2.159. [PubMed] [Google Scholar]
- Lambert MJ, Harmon C, Slade K, Whipple JL, Hawkins EJ. Providing feedback to psychotherapists on their patients’ progress: Clinical results and practice suggestions. Journal of Clinical Psychology. 2005;61(2):165–174. doi: 10.1002/jclp.20113. http://dx.doi.org/10.1002/jclp.20113. [DOI] [PubMed] [Google Scholar]
- Lambert MJ, Whipple JL, Hawkins EJ, Vermeersch DA, Nielsen SL, Smart DW. Is It time for clinicians to routinely track patient outcome? A meta-analysis. Clinical Psychology: Science and Practice. 2003;10(3):288–301. http://dx.doi.org/10.1093/clipsy.bpg025. [Google Scholar]
- Lambert MJ, Whipple JL, Vermeersch DA, Smart DW, Hawkins EJ, Nielsen SL, Goates M. Enhancing psychotherapy outcomes via providing feedback on client progress: A replication. Clinical Psychology & Psychotherapy. 2002;9(2):91–103. http://dx.doi.org/10.1002/cpp.324. [Google Scholar]
- Lewis CC, Simons AD, Silva SG, Rohde P, Small DM, Murakami JL, March JS. The role of readiness to change in response to treatment of adolescent depression. Journal of Consulting and Clinical Psychology. 2009;77(3):422. doi: 10.1037/a0014154. http://dx.doi.org/10.1037/a0014154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon AR, Borntrager C, Nakamura B, Higa-McMillan C. From distal to proximal: Routine educational data monitoring in school-based mental health. Advances in School Mental Health Promotion. 2013;6(4):263–279. doi: 10.1080/1754730X.2013.832008. http://dx.doi.org/10.1080/1754730X.2013.832008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martell CR, Addis ME, Jacobson NS. Depression in context: Strategies for guided action. New York: WW Norton; 2001. [Google Scholar]
- Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. Journal of Consulting and Clinical Psychology. 2000;68(3):438. http://dx.doi.org/10.1037/0022-006X.68.3.438. [PubMed] [Google Scholar]
- May DE, Kratochvil CJ, Puumala SE, Silva SG, Rezac AJ, Hallin MJ, March JS. A manual-based intervention to address clinical crises and retain patients in the Treatment of Adolescents With Depression Study (TADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(5):573–581. doi: 10.1097/chi.0b013e3180323342. http://dx.doi.org/10.1097/chi.0b013e3180323342. [DOI] [PubMed] [Google Scholar]
- McConnaughy EA, Prochaska JO, Velicer WF. Stages of change in psychotherapy: Measurement and sample profiles. Psychotherapy: Theory, Research and Practice. 1983;20(3):368–375. http://dx.doi.org/10.1037/h0090198. [Google Scholar]
- McDowell I. Measuring health: a guide to rating scales and questionnaires. New York: Oxford University Press; 2006. [Google Scholar]
- McLeod BD, Jensen-Doss A, Ollendick TH. Overview of diagnostic and behavioral assessment. In: McLeod BD, Jensen-Doss A, Ollendick TH, editors. Diagnostic and behavioral assessment in children and adolescents: A clinical guide. New York: Guilford Press; 2013. [Google Scholar]
- Morris DW, Trivedi MH. Measurement-based care for unipolar depression. Current Psychiatry Reports. 2011;13(6):446–458. doi: 10.1007/s11920-011-0237-8. http://dx.doi.org/10.1007/s11920-011-0237-8. [DOI] [PubMed] [Google Scholar]
- Nakamura BJ, Daleiden EL, Mueller CW. Validity of treatment target progress ratings as indicators of youth improvement. Journal of Child and Family Studies. 2007;16(5):729–741. http://dx.doi.org/10.1007/s10826-006-9119-9. [Google Scholar]
- Nezu AM, Ronan GF, Meadows EA, McClure KS. Practitioner’s guide to empirically based measures of depression. New York: Kluwer Academic/Plenum; 2002. [Google Scholar]
- Norcross JC, Krebs PM, Prochaska JO. Stages of change. Journal of Clinical Psychology. 2011;67(2):143–154. doi: 10.1002/jclp.20758. http://dx.doi.org/10.1002/jclp.20758. [DOI] [PubMed] [Google Scholar]
- Pavot W, Diener E. Review of the satisfaction with life scale. Psychological Assessment. 1993;5(2):164–172. http://dx.doi.org/10.1037/1040-3590.5.2.164. [Google Scholar]
- PracticeGround. Assessment measures. 2013 Retrieved from https://practiceground.org/pages/view/assessment-measures.
- PracticeWise. 2013 Retrieved from http://www.practicewise.com.
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. Journal of Consulting and Clinical Psychology. 1983;51(3):390. doi: 10.1037//0022-006x.51.3.390. http://dx.doi.org/10.1037/0022-006X.51.3.390. [DOI] [PubMed] [Google Scholar]
- Proctor EK, Knudsen KJ, Fedoravicius N, Hovmand P, Rosen A, Perron B. Implementation of evidence-based practice in community behavioral health: Agency director perspectives. Administration and Policy in Mental Health and Mental Health Services Research. 2007;34(5):479–488. doi: 10.1007/s10488-007-0129-8. http://dx.doi.org/10.1007/s10488-007-0129-8. [DOI] [PubMed] [Google Scholar]
- Rush AJ, First MB, Blacker D, editors. Handbook of psychiatric measures. Arlington, VA: American Psychiatric Publishing; 2008. [Google Scholar]
- Saggese ML. Maximizing treatment effectiveness in clinical practice: An outcome-informed collaborative approach. Families in Society: The Journal of Contemporary Social Services. 2005;86(4):558–564. http://dx.doi.org/10.1606/1044-3894.3461. [Google Scholar]
- Sapyta J, Riemer M, Bickman L. Feedback to clinicians: Theory, research, and practice. Journal of Clinical Psychology. 2005;61(2):145–153. doi: 10.1002/jclp.20107. http://dx.doi.org/10.1002/jclp.20107. [DOI] [PubMed] [Google Scholar]
- Scott K, Lewis CC, editors. A qualitative analysis of contextual factors influencing implementation of measurement based care. 2014. Manuscript in preparation. [Google Scholar]
- Simon GE, VonKorff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. British Medical Journal. 2000;320(7234):550–554. doi: 10.1136/bmj.320.7234.550. http://dx.doi.org/10.1136/bmj.320.7234.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons AD, Rozek DC, Serrano JL. Wanted: Reliable and valid measures for the science of cognitive behavioral therapy dissemination and implementation. Clinical Psychology: Science and Practice. 2013;20(2):181–194. http://dx.doi.org/10.1111/cpsp.12033. [Google Scholar]
- Slade K, Lambert MJ, Harmon SC, Smart DW, Bailey R. Improving psychotherapy outcome: The use of immediate electronic feedback and revised clinical support tools. Clinical psychology & psychotherapy. 2008;15(5):287–303. doi: 10.1002/cpp.594. http://dx.doi.org/10.1002/cpp.594. [DOI] [PubMed] [Google Scholar]
- Slade M, Thornicroft G, Glover G. The feasibility of routine outcome measures in mental health. Social Psychiatry and Psychiatric Epidemiology. 1999;34(5):243–249. doi: 10.1007/s001270050139. http://dx.doi.org/10.1007/s001270050139. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. http://dx.doi.org/10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stirman SW, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implementation Science. 2012;7(17):1–19. doi: 10.1186/1748-5908-7-17. http://dx.doi.org/10.1186/1748-5908-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft GJ, Tansella M, editors. Mental health outcomes measures. London: RCPsych; 2010. [Google Scholar]
- Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1(3):207. http://dx.doi.org/10.1037/1040-3590.1.3.207. [Google Scholar]
- Trivedi MH, Daly EJ. Measurement-based care for refractory depression: A clinical decision support model for clinical research and practice. Drug and Alcohol Dependence. 2007;88:S61–S71. doi: 10.1016/j.drugalcdep.2007.01.007. http://dx.doi.org/10.1016/j.drugalcdep.2007.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi MH, Rush AJ, Gaynes BN, Stewart JW, Wisniewski SR, Warden D, Howland R. Maximizing the adequacy of medication treatment in controlled trials and clinical practice: STAR*D measurement-based care. Neuropsychopharmacology. 2007;32(12):2479–2489. doi: 10.1038/sj.npp.1301390. http://dx.doi.org/10.1038/sj.npp.1301390. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, Fava M. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR* D: Implications for clinical practice. American Journal of Psychiatry. 2006;163(1):28–40. doi: 10.1176/appi.ajp.163.1.28. http://dx.doi.org/10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, Langston C. Collaborative care management of late-life depression in the primary care setting. Journal of the American Medical Association. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. http://dx.doi.org/10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Valenstein M, Adler DA, Berlant J, Dixon LB, Dulit RA, Goldman B, Sonis WA. Implementing standardized assessments in clinical care: Now’s the time. Psychiatric Services. 2009;60(10):1372–1375. doi: 10.1176/ps.2009.60.10.1372. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Chorpita BF, Frye A, Ng MY, Lau N, Bearman SK, Hoagwood KE. Youth Top Problems: Using idiographic, consumer-guided assessment to identify treatment needs and to track change during psychotherapy. Journal of Consulting and Clinical Psychology. 2011;79(3):369. doi: 10.1037/a0023307. http://dx.doi.org/10.1037/a0023307. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Ugueto AM, Herren J, Afienko SR, Rutt C. Kernels vs. ears, and other questions for a science of treatment dissemination. Clinical Psychology: Science and Practice. 2011;18(1):41–46. doi: 10.1111/j.1468-2850.2010.01233.x. http://dx.doi.org/10.1111/j.1468-2850.2010.01233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


