Summary
The phenomenon known as vaccine hesitancy (a term that includes the concepts of indecision, uncertainty, delay and reluctance) is complex, closely linked to social contexts, and has different determinants: historical period, geographical area, political situation, complacency, convenience and confidence in vaccines. The World Health Organization (WHO) recommends that vaccine hesitancy and any proxy of it should be constantly monitored. Given the growing importance and pervasiveness of information and communication technologies (ICTs), the new media could be exploited in order to track lay-people's perceptions of vaccination in real time, thereby enabling health-care workers to actively engage citizens and to plan ad hoc communication strategies. Analysis of so-called "sentiments" expressed through the new media (such as Twitter) and the real-time tracking of web-related activities enabled by Google Trends, combined with the administration of specific online "surveys" on well-defined themes to target groups (such as health-care workers), could constitute a "Fast data monitoring system" that yields a snapshot of perceptions of vaccination in a given place and at a specific time. This type of dashboard could be a strategic tool that enables public services to organize targeted communication actions aimed at containing vaccine hesitancy.
Key words: Digital disintermediation, Vaccine hesitancy, Fast data-monitoring system
Vaccine hesitancy
A complex, multi-faceted phenomenon that dates back to the first vaccinations performed by Dr. Zabdiel Boylston (1721) and Edward Jenner (1796-1798), vaccine hesitancy constitutes a threat to the implementation of immunization programs [1-5]. Concerns and/or misconceptions regarding vaccines may prompt people to delay or refuse vaccination. Consequently, suboptimal vaccination coverage rates may jeopardize the attainment of herd immunity and result in pathogen recrudescence and disease outbreaks. It is therefore crucial to understand the determinants of compliance with vaccination. These have been grouped into the 5A taxonomy (Access, Affordability, Awareness, Acceptance, and Activation) [6] or the 3C model (Complacency, Convenience and Confidence) [7].
Vaccine hesitancy is a major, global issue. Being a very dynamic and heterogeneous phenomenon, it changes throughout space and time, varying according to the context and to geographic and demographic variables. Furthermore, as vaccine hesitancy is setting-dependent and vaccine-specific, it is highly unpredictable.
Today, vaccine hesitancy is closely connected with the increasing importance of the Internet and the new information and communication technologies (ICTs) [8].
The new media
The pervasive diffusion of the web is a characteristic feature of modern society. In 1962, Marshall McLuhan distinguished four different epochs of history: the first dominated by the oral tribe culture, the second by the manuscript culture, the third termed as the Gutenberg Galaxy, and the fourth defined as the electronic age [9]. Technological and information changes have contributed to the rise of the fluid postmodern society, which is characterized by uncertainty, nomadism, fragmentation, disintegration and relativization of the truth [10].
Digital media have dissolved reality into an infinite array of bits, an ocean, a fluctuating swarm, a chaotic magma, that can be navigated interactively by accessing the Internet. Indeed, the static heritage and the rigidly codified system of knowledge and hierarchies of the Gutenberg Galaxy have been broken down by the web.
Whilst the Web 1.0 was static, the Web 2.0 (and its further evolution, including the semantic web) has become a highly dynamic and interactive information reality, enabling users to share their content and to become consumers and producers at the same time (prosumers). Thus, the differences and the distance between webmasters and web surfers are becoming increasingly blurred.
This has led to a phenomenon known, in the field of electronic commerce, as "digital disintermediation"; consumers purchase products directly from producers via the Internet, thereby drastically shortening and modifying the product delivery chain and "disintermediating" the standard supply model. This direct-toconsumer model has its analogues in the medical field; in the emerging postmodern healthcare model, patients proactively search the Web for health-related information, thus bypassing clinicians. In this perspective, the legitimacy of science is questioned and expertise is redefined.
On the other hand, within e-health or health 2.0 – a term that indicates new modalities, strategies, and practices of healthcare delivery that exploit, and are supported by, electronic processes and communication – patients are at the center of healthcare processes, as they are more involved in and informed of the many steps of medical decision-making [11].
Vaccines and the web
Within the above-mentioned model, ICTs play a role in parents' decisions on whether or not to vaccinate their children. In Italy, according to the latest available data released by the National Institute of Statistics (ISTAT), 80% of parents use the Internet to search for vaccinerelated information [12]. Moreover, a recent publication by CENSIS has shown that 48.6% and 42% of parents use social networks and the web, respectively, to obtain information on vaccines [13]. This implies that workers in the field of Public Health have to rethink their way of interacting with the media, especially the new media, in order to combat the unjustified alarmism and hoaxes regarding vaccination. Furthermore, they need to combine the accuracy and scientific rigor of information with a modality of communication that can be easily understood by lay-people. Targeted and authoritative information can be accompanied by awareness campaigns and school interventions. Indeed, while 91.1% of parents are aware that vaccines have eradicated diseases and constitute an important means of protecting themselves and the community, they still have doubts, uncertainties and concerns about vaccine safety. This highlights a specific information gap that needs to be properly addressed.
The Web 2.0 acts as a post-modern Pandora's box, which is difficult to control and to discipline. It can therefore spread disinformation, misleading news and falsehoods [14, 15]. Indeed, many critical websites or pages show anti-vaccination content. Despite being of low quality, these are highly ranked and are therefore frequently returned by search engines and consulted by users. Furthermore, they are more readable than websites containing information from reliable sources [16, 17]. Moreover, websites that are openly skeptical or even hostile to vaccinations are highly active on the Internet [18]. Since 2010, however, public institutions have increased the presence of sites in favor of vaccination. Consequently, in 2015, the use of such search terms as "immunization" or "vaccination" was seen to yield a predominance of pro-vaccination websites created by public institutions, scientific societies or individual health professionals [19].
Challenges and opportunities
The issue of vaccination is increasingly influencing political agendas.
Opportunities derive directly from the considerations that vaccine hesitancy is unpredictable and fluid and that anti-vaccination movements exploit the new ICTs. Workers in the field of Public Health can also exercise their role of advocacy on the Internet. An example of this is the website VaccinarSì (http://www.vaccinarsi.org/), which initially emerged from an idea by Mrs. Ulrike Schmidleithner (http://vaccinarsi.blogspot.it) [20]. Another example of bottom-up initiatives is that of an online pro-vaccination campaign started by an Italian mother, Miriam Maurantonio. Concerned about low vaccination coverage and the growing visibility of antivaccination movements, Mrs Maurantonio asked parents to take "selfies" and to post them by using the hashtag #iovaccino (#Ivaccine). This initiative has spread to other social networks, such as Facebook and Instagram, reaching thousands of followers and subscribers.
Further exploitation of ICTs involves applications for smart-phones, the popularity of which is rapidly increasing. In Italy, for example, the app "Pneumo Rischio" has been developed specifically to increase public awareness of invasive pneumococcal disease and its prevention [21].
All these instruments can be exploited in order to empower lay-people and increase their health literacy. Local Health Units (LHUs) can utilize the new media to establish a novel, interactive dialogue with residents in their territories. This model has been termed as "@ Prevention" [22]. However, in order to exploit the new media effectively, it is essential to improve the information skills of clinicians and pediatricians. To this end, the Italian Scientific Society of Pediatricians (FIMP) has launched the "Hermes project", named after the Greek god of communication, the protector and patron of oratory and wit, literature and poetry [23]. This project provides a step-by-step course that teaches pediatricians how to open a Twitter account and to dynamically interact and communicate with children's families, so that they can address their concerns or doubts about vaccination.
Another opportunity is constituted by "infodemiology" (a port-manteau of information and epidemiology) and "infoveillance" (a port-manteau of information and surveillance), which have been introduced by Gunther Eysenbach as new emerging concepts and approaches [24]. Public health and epidemiological research can be based on large-scale monitoring and data-mining.
Infodemiology and infoveillance take into consideration all the virtual activities carried out by lay-people while surfing health-related sites and/or communicating and sharing their health status. These pieces of information are known as "fast" or "big" data, in that this incredible wealth of data is quickly available to researchers.
Analysis of the so-called "sentiments" expressed through the new media (i.e. Tweets) [25] and the real-time tracking and monitoring of web-related activities, enabled by Google Trends, can yield a snapshot of the "social climate"; this picture could also be combined with ad hoc online surveys on well-defined themes and topics, administered to specific target groups (i.e. health workers). The resulting "Fast data monitoring system" could provide a real-time representation of perceptions of vaccination. Moreover, the use of georeferentiation through sophisticated and advanced geographic information systems (GIS) could capture perception in a specific place and at a given time.
This type of dashboard could be a strategic tool for public services, which could then organize targeted communication actions aimed at containing vaccine hesitancy (Fig. 1).
Fig. 1.
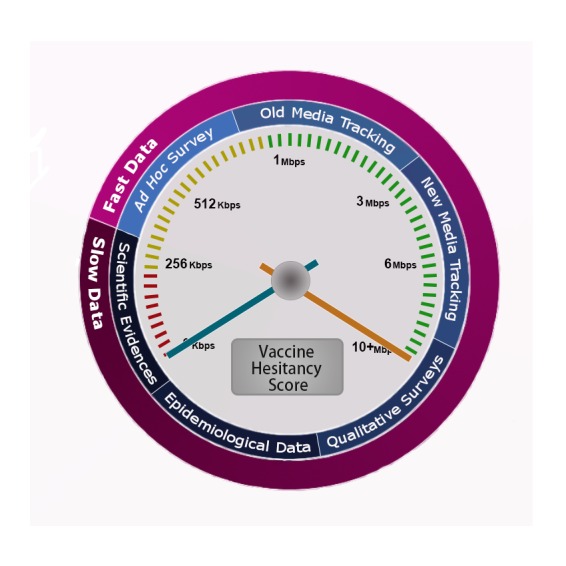
Vaccine hesitancy is a fluid and constantly changing phenomenon that needs to be monitored over time. As recommended by the Strategic Advisory Group of Experts (SAGE) on vaccine hesitancy, an integrated approach based on a combination of both slow and fast data collection (scientific evidence and, in particular, systematic reviews, epidemiological data, qualitative surveys, ad hoc surveys, old and new media tracking) can ensure proper tracking of the phenomenon.
Conclusions
The World Health Organization (WHO) recommends that vaccine hesitancy and any proxy of it should be constantly monitored [26]. Given the growing importance and pervasiveness of ICTs, the new media could be exploited in order to track lay-people's perceptions of vaccination in real time, thereby enabling health-care workers to actively engage citizens and to plan ad hoc communication strategies [27-29].
Acknowledgments
No funding declared for this overview.
References
- 1.Shrivastava SR, Shrivastava PS, Ramasamy J. The growing global problem of vaccine hesitancy: time to take action. Int J Prev Med. 2016;7:18–18. doi: 10.4103/2008-7802.173924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumar D, Chandra R, Mathur M, Samdariya S, Kapoor N. Vaccine hesitancy: understanding better to address better. Isr J Health Policy Res. 2016;5:2–2. doi: 10.1186/s13584-016-0062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salmon DA, Dudley MZ, Glanz JM, Omer SB. Vaccine hesitancy: causes, consequences, and a call to action. Vaccine. 2015;33(Suppl 4):D66–D71. doi: 10.1016/j.vaccine.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 4.Jacobson RM, St Sauver JL, Finney Rutten LJ. Vaccine hesitancy. Mayo Clin Proc. 2015;90:1562–1568. doi: 10.1016/j.mayocp.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz JL. New media, old messages: themes in the history of vaccine hesitancy and refusal . Virtual Mentor. 2012;14:50–55. doi: 10.1001/virtualmentor.2012.14.1.mhst1-1201. [DOI] [PubMed] [Google Scholar]
- 6.Thomson A, Robinson K, Vallée-Tourangeau G. The 5As: a practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016;34:1018–1024. doi: 10.1016/j.vaccine.2015.11.065. [DOI] [PubMed] [Google Scholar]
- 7.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. SAGE Working Group on Vaccine Hesitancy. [DOI] [PubMed] [Google Scholar]
- 8.Tafuri S, Gallone MS, Cappelli MG, Martinelli D, Prato R, Germinario C. Addressing the anti-vaccination movement and the role of HCWs . Vaccine. 2014;32:4860–4865. doi: 10.1016/j.vaccine.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 9.McLuhan M. The Gutenberg Galaxy: the making of typographic man. Toronto, CA: University of Toronto Press; 1962. [Google Scholar]
- 10.Bauman Z. Liquid times: living in an age of uncertainty. Cambridge: Polity; 2006. [Google Scholar]
- 11.Bragazzi NL. From P0 to P6 medicine, a model of highly participatory, narrative, interactive, and "augmented" medicine: some considerations on Salvatore Iaconesi's clinical story. Patient Prefer Adherence. 2013;7:353–359. doi: 10.2147/PPA.S38578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. ISTAT. Citizens and new technologies. Available at http://www.istat.it/en/archive/citizens+and+new+technologies. [Accessed on 10/02/2016]
- 13. CENSIS. 49th report on the social situation of the country. 2015.
- 14.Kata A. A postmodern Pandora's box: anti-vaccination misinformation on the Internet. Vaccine. 2010;28:1709–1716. doi: 10.1016/j.vaccine.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 15.Gasparini R, Panatto D, Lai PL, Amicizia D. The "urban myth" of the association between neurological disorders and vaccinations. J Prev Med Hyg. 2015;56:E1–E8. [PMC free article] [PubMed] [Google Scholar]
- 16.Sak G, Diviani N, Allam A, Schulz PJ. Comparing the quality of pro- and anti-vaccination online information: a content analysis of vaccination-related webpages. BMC Public Health. 2016;16:38–38. doi: 10.1186/s12889-016-2722-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ochoa AG. Content attributes of vaccine promotion websites as compared to claims made by anti-vaccine groups. Houston, DX: The University of Texas School of Public Health; 2015. pp. 36–36. 1598348. [Google Scholar]
- 18.Davies P, Chapman S, Leask J. Antivaccination activists on the world wide web. Arch Dis Child. 2002;87:22–26. doi: 10.1136/adc.87.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keelan J, Pavri-Garcia V, Tomlinson G, Wilson K. YouTube as a source of information on immunization: a content analysis . JAMA. 2007;298:2482–2484. doi: 10.1001/jama.298.21.2482. [DOI] [PubMed] [Google Scholar]
- 20.Ferro A, Odone A, Siddu A, Colucci M, Anello P, Longone M, Marcon E, Castiglia P, Bonanni P, Signorelli C. Monitoring the web to support vaccine coverage: results of two years of the portal VaccinarSì. Epidemiol Prev. 2015;39(4 Suppl 1):88–93. [PubMed] [Google Scholar]
- 21.Panatto D, Domnich A, Gasparini R, Bonanni P, Icardi G, Amicizia D, Arata L, Bragazzi NL, Signori A, Landa P, et al. Development and preliminary data on the use of a mobile app specifically designed to increase community awareness of invasive pneumococcal disease and its prevention . Vaccin Immunother. 2016 Jan;21:1–5. doi: 10.1080/21645515.2015.1114196. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosselli R, Onesti A, Martini M, Cartiglia C, Sticchi L, Alberti M. @Prevention: a website project for prevention in the healthcare setting . J Prev Med Hyg. 2011;52:59–63. [PubMed] [Google Scholar]
- 23. Federazione Italiana dei Medici Pediatri (FIMP). Progetto FIMP HERMES. Available at http://www.fimp.veneto.it/sites/default/files/Progetto%20FIMP%20HERMES%5B1%5D.pdf. [Accessed on 10/02/2016]
- 24.Eysenbach G. Infodemiology and infoveillance: framework for an emerging set of public health informatics methods to analyze search, communication and publication behavior on the internet. J Med Internet Res. 2009;11:e11–e11. doi: 10.2196/jmir.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bahk CY, Cumming M, Paushter L, Madoff LC, Thomson A, Brownstein JS. Publicly available online tool facilitates real-time monitoring of vaccine conversations and sentiments . Health Aff (Millwood) 2016;35:341–347. doi: 10.1377/hlthaff.2015.1092. [DOI] [PubMed] [Google Scholar]
- 26. World Health Organization (WHO). Addressing vaccine hesitancy. Available at http://www.who.int/immunization/programmes_systems/vaccine_hesitancy.
- 27.Capurro D, Cole K, Echavarría MI, Joe J, Neogi T, Turner AM, et al. The use of social networking sites for public health practice and research: a systematic review. J Med Internet Res. 2014;16:e79–e79. doi: 10.2196/jmir.2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication . J Med Internet Res. 2013;15:e85–e85. doi: 10.2196/jmir.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vance K, Howe W, Dellavalle RP, et al. Social internet sites as a source of public health information. Dermatol Clin. 2009;27:133–136. doi: 10.1016/j.det.2008.11.010. [DOI] [PubMed] [Google Scholar]


