Key messages
Approximately 1 in 7 Canadian children and adolescents is obese.
Obesity prevalence rates in Canadian children and adolescents have not changed significantly since 2007. These rates are projected to remain stable over the next two decades.
Approximately 1 in 4 Canadian adults is obese.
Obesity prevalence rates in Canadian adults are projected to continue to increase over the next two decades.
The increase in obesity rates is projected to be greater in males than females across the lifespan.
Background
The prevalence of obesity, defined as body mass index (BMI) of 30 kg/m2 or higher for adults and as 2 standard deviations above the World Health Organization growth standard mean for children, has increased in many parts of the world.1 Obese adults are at an increased risk of certain chronic conditions, including hypertension, type 2 diabetes, cardiovascular diseases and some cancers, and of premature death.2,3 Obese children have increased cardiometabolic risk, including dyslipidemia, insulin resistance and elevated blood pressure.4,5,6 Excess childhood body weight that continues into adulthood can affect quality of life, educational attainment and earnings over the lifecourse.7,8
The Public Health Agency of Canada has projected an annual direct health care cost (including physician, hospitalization and medication costs) of those categorized as obese in Canada in constant 2001 Canadian dollars. Calculated as $7.0 billion in 2011, this annual direct health care cost is projected to rise to $8.8 billion by 2021, based on simulated average direct health care costs, which are higher among the obese ($2,283) than the overweight ($1,726), the underweight ($1,298) and those at normal weight ($1,284).9 Canadian estimates from 2006 and 2008 that used different methodologies place the annual economic burden (direct and indirect costs) of obesity between $4.6 billion and $7.1 billion.10,11
The purpose of this evidence brief is to show current Canadian obesity prevalence rates and estimates for the future using objectively measured height and weight to calculate BMI. The use of objectively measured height and weight to derive BMI is strongly recommended, especially for children and adolescents,12 as self- or proxy-reported height and weight tend to underestimate actual weight and consequently BMI and obesity prevalence.13,14
Data sources
Before 2007, only a few national population-level surveys directly measured the height and weight of children and adolescents: the Canada Health Survey (age 0 and older) in 1978/1979; the Canada Fitness Survey (age 7 years and older) in 1981; the Campbell’s Survey on Well-being in Canada (age 7 years or older) in 1988; and the Canadian Community Health Survey (CCHS), Cycle 2.2 Nutrition (age 2 years or older) in 2004. Since 2007, the Canadian Health Measures Survey (CHMS) has systematically collected objectively measured BMI; data collection through the CHMS occurs in two-year cycles.15
We generated projections of past, current and future BMI from 2001 through to 2031 using the POpulation Health Microsimulation model for childhood and adult BMI (POHEM-BMI).16 POHEM-BMI is a continuous-time, Monte Carlo microsimulation model in which the basic unit of analysis is the individual. The dynamic simulation recreates the Canadian population at a given point in time through births, immigration and emigration, and ages it, one person at a time, until death. Life events such as smoking initiation and cessation, changes in physical activity and BMI, and incidence and progression of diseases affect the life trajectory and mortality of individual simulated people. POHEM-BMI integrates data distributions and equations derived from sources that include nationally representative cross-sectional and longitudinal surveys, and vital statistics and cancer registries.9,16 In particular, multivariate regression equations estimated from the longitudinal National Population Health Surveys from 1994 to 2006 simulate the plausible dynamics of BMI, adjusting for self- and proxy-report bias. The POHEM-BMI model is auto-regressive and includes variables that have predictive power beyond that of the history of BMI, such as age, sex, physical activity and smoking status. POHEM-BMI projections assume that current behaviour patterns continue and nothing new is done to prevent obesity.
Obesity trends in Canadian children and adolescents
Obesity prevalence rates that used objectively measured BMI more than doubled in Canadian children and adolescents (aged under 18 years) between 1978/79 and 2004, from 6.3% (in 2 to 17 year olds) to 13.3% (in 6 to 17 year olds).17 Obesity prevalence rates are higher in boys than in girls and higher in adolescents (12–17 years) than in younger children (6–11 years). Data from the 2007–2009, 2009–2011 and 2012–2013 cycles of CHMS suggest that obesity prevalence rates have stabilized between 11.6% and 14.3% (in 6 to 17 year olds). These observations are consistent with POHEM-BMI,16 which projects that obesity among Canadian children aged 6 to 17 years will stabilize after 2013, resulting in 1 in 7 children being obese (Figure 1).
FIGURE 1. Prevalence of obesity among Canadian children and adolescents and adults by calendar year.
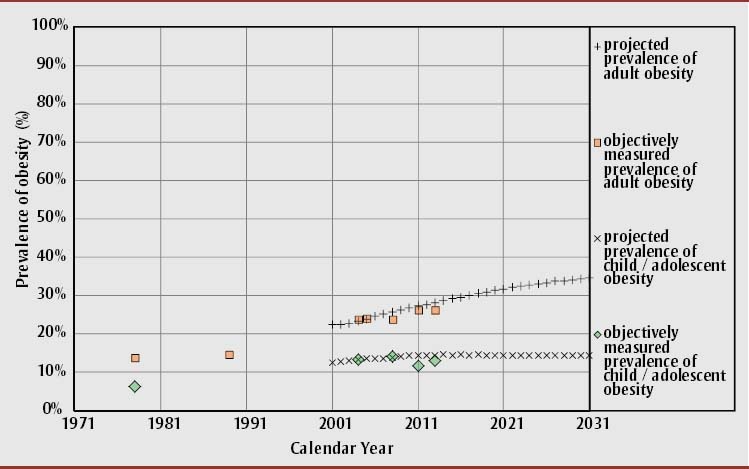
Notes: Projected prevalence using Population Health Model for body mass index (POHEM-BMI) Version 6.0.1.0, March 3, 2015. Objectively measured prevalence from Canadian population health surveys (see Data Sources for details). Children/adolescents encompass ages 6 to 17 years; adults encompass ages 18 to 79 years.
Obesity trends in Canadian adults (18+ years)
Obesity prevalence rates that used objectively measured BMI nearly doubled in Canadian adults between 1978/79 and 2004, from 13.8% to 23.1%.11 Obesity prevalence rates among adults are lowest in early adulthood, increase in middle age and decline slightly in seniors. Data from the 2007–2009, 2009–2011 and 2012–2013 cycles of CHMS suggest adult obesity prevalence was between 23.9% and 26.4%, resulting in 1 in 4 adults being obese. Projections using POHEM-BMI suggest obesity among adults will rise over the next two decades (Figure 1), with the largest increase in adult men (Figure 2).
FIGURE 2. Prevalence of obesity among Canadian children and adolescents and adults by sex and calendar year.
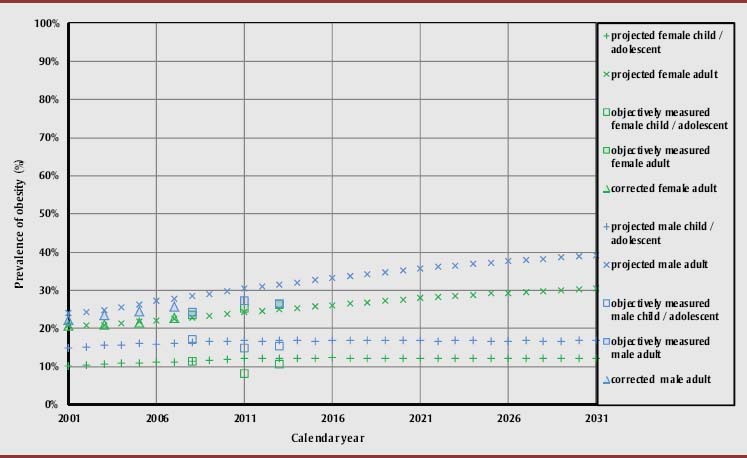
Notes: Projected prevalence using Population Health Model for body mass index (POHEM-BMI) Version 6.0.1.0, March 3, 2015. Objectively measured prevalence from Canadian population health surveys (see Data Sources for details). Children/adolescents encompass ages 6 to 17 years; adults encompass ages 18 to 79 years.
Conclusions
Our analysis of three recent cycles of the CHMS shows that obesity prevalence rates that use objectively measured BMI stabilized in children and adolescents but rose slightly in adults. Our microsimulation projections suggest that despite a stabilization in obesity prevalence among children and adolescents, if nothing new and effective is done to mitigate the trend among adults, objectively measured obesity will rise over the next two decades, affecting more than one in three Canadian adults by 2031. These projections from a validated population health microsimulation model18 provide a realistic benchmark against which to compare new surveillance data to gauge shifts in the trend of obesity among Canadian children and adults.
References
- 1.World Health Organization . World Health Organization; 2014. Global status report on non-communicable diseases 2014 [Internet]. pp. 78–83. Available from: http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1. [Google Scholar]
- 2.Guh DP, Zhang W, Bansback N, Zubin A, Laird BC, Anis Aslam H. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katzmarzyk PT, Ardern CI. Overweight and obesity mortality trends in Canada 1985–2000. Can J Public Health. 2004;95:16–20. doi: 10.1007/BF03403627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Malley G, Santoro N, Northrup V, et al. High normal fasting glucose level in obese adolescents: a marker for insulin resistance and beta cell dysregulation. Diabetologia. 2010;53:1199–209. doi: 10.1007/s00125-010-1693-0. [DOI] [PubMed] [Google Scholar]
- 5.Sinha R, Fisch G, Teague B, et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med. 2002;346:802–10. doi: 10.1056/NEJMoa012578. Erratum in: N Engl J Med. 2002;346:1756. [DOI] [PubMed] [Google Scholar]
- 6.Ostchega Y, Carroll M, Prineas RJ, McDowell MA, Louis T, Tilert T. Trends of elevated blood pressure among children and adolescents: data from the National Health and Nutrition Examination Survey 1988-2006. Am J Hypertens. 2009;22:59–67. doi: 10.1038/ajh.2008.312. [DOI] [PubMed] [Google Scholar]
- 7.Herman KM, Craig CL, Gauvin L, Katzmarzyk PT. Tracking of obesity and physical activity from childhood to adulthood: the Physical Activity Longitudinal Study. Int J Pediatr Obes. 2009;4((4)):281–8. doi: 10.3109/17477160802596171. [DOI] [PubMed] [Google Scholar]
- 8.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17:941–64. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 9.Nadeau C, Asakawa K, Flanagan W, Wall RW, Bancej C, Morrison H. Projection of body mass ondex (BMI), chronic conditions and healthcare costs in Canada: an application of microsimulation. Can J Diab. 2013;37((2)):S243–4. [Google Scholar]
- 10.Anis AH, Zhang W, Bansback N, Guh DP, Amarsi Z, Birmingham CL. Obesity and overweight in Canada: an updated cost-of-illness study. Obes Rev. 2010;11:31–40. doi: 10.1111/j.1467-789X.2009.00579.x. [DOI] [PubMed] [Google Scholar]
- 11.Public Health Agency of Canada and Canadian Institute for Health Information . Obesity in Canada: a joint report from the Public Health Agency of Canada and the Canadian Institute for Health Information [Internet] Ottawa (ON): Public Health Agency of Canada; 2011 [cited 2014 Feb 25]. pp 29-30. Joint publication of Canadian Institute for Health Information. Available from: http://www.phac-aspc.gc.ca/hp-ps/hl-mvs/oic-oac/assets/pdf/oic-oac-eng.pdf. [Google Scholar]
- 12.Shields M, Gorber SC, Janssen I, Tremblay MS. Obesity estimates for children based on parent-reported versus direct measures. Health Rep. 2011;22((3)):47–58. [PubMed] [Google Scholar]
- 13.Elgar FJ, Stewart JM. Validity of self-report screening for overweight and obesity. Evidence from the Canadian Community Health Survey. Can J Public Health. 2008;99((5)):423–7. doi: 10.1007/BF03405254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hattori A, Sturm R. The obesity epidemic and changes in self-report biases in BMI. Obesity (Silver Spring) 2013;21((4)):856–60. doi: 10.1002/oby.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tremblay MS, Wolfson M, Connor Gorber S. Canadian Health Measures Survey: rationale, background and overview. Health Rep. 2007;18(Suppl.):7–20. [PubMed] [Google Scholar]
- 16.Nadeau C, Flanagan W. POHEM-BMI: a dynamic microsimulation model of impact of body mass index and health outcomes and costs for Canada. Ottawa (ON): Health Analysis Division, Statistics Canada; 2011. [Google Scholar]
- 17.Shields M, Tremblay MS. Canadian childhood obesity estimates based on WHO, IOTF and CDC cut-points. Int J Pediatr Obes. 2010;5:265–73. doi: 10.3109/17477160903268282. [DOI] [PubMed] [Google Scholar]
- 18.Kopec JA, Fines P, Manuel DG, et al. Validation of population-based disease simulation models: a review of concepts and methods. BMC Public Health. 2010;10:710. doi: 10.1186/1471-2458-10-710. [DOI] [PMC free article] [PubMed] [Google Scholar]


