Abstract
This article describes the development and evaluation of a national service to diagnose and remediate central auditory processing disorder (CAPD). Data were gathered from 38 participating Australian Hearing centers over an 18-month period from 666 individuals age 6, 0 (years, months) to 24, 8 (median 9, 0). A total of 408 clients were diagnosed with either a spatial processing disorder (n = 130), a verbal memory deficit (n = 174), or a binaural integration deficit (n = 104). A hierarchical test protocol was used so not all children were assessed on all tests in the battery. One hundred fifty clients decided to proceed with deficit-specific training (LiSN & Learn or Memory Booster) and/or be fitted with a frequency modulation system. Families were provided with communication strategies targeted to a child's specific listening difficulties and goals. Outcomes were measured using repeat assessment of the relevant diagnostic test, as well as the Client Oriented Scale of Improvement measure and Listening Inventories for Education teacher questionnaire. Group analyses revealed significant improvements postremediation for all training/management options. Individual posttraining performance and results of outcome measures also are discussed.
Keywords: Central auditory processing disorder, spatial processing disorder, deficit-specific auditory training
Learning Outcomes: As a result of this activity, the participant will be able to (1) explain the nature and advantages of a hierarchical CAPD assessment structure, and (2) describe the advantages and consequences of offering deficit-specific remediation options.
This article provides a real-world evaluation of a diagnostic and rehabilitation service for central auditory processing disorder (CAPD). CAPD is an umbrella term for a variety of deficits. The disorder, which originates in the central auditory nervous system, is characterized by less accurate perception of auditory signals. The reduced accuracy becomes particularly debilitating when attempting to communicate in noisy environments, such as the classroom.
Australian Hearing began offering CAPD services in mid-2012. The service commenced in two hearing centers and expanded to 38 permanent hearing centers across regional, suburban, and central business district sites, encompassing a range of socioeconomic areas. Initial marketing of the new service was achieved primarily by sending letters to likely referral services (primarily speech pathologists and schools) in the area local to each participating center. To minimize the potential for parents of children with learning and attention disorders unrelated to CAPD requesting assessment, recruitment specifically targeted children experiencing listening deficits in noisy environments.1 (As no government benefits are available in Australia for children with CAPD, the service was provided on a fee-for-service basis.)
Outcomes of the service are presented and evaluated over an 18-month period from April 2012 to December 2013. During that time, 700 individuals were seen by Australian Hearing centers, of which 666 were found suitable for inclusion in the analysis. Over 400 clients were diagnosed with an auditory processing deficit or a verbal short-term or working memory deficit, and 150 of those clients proceeded with some type of remediation option. Remediation can be generic and applied to a broadly described condition such as CAPD irrespective of the specific deficit that led to the diagnosis of CAPD. Alternatively, remediation can be specific to the subtype of CAPD deficit for which the client has been diagnosed. The services offered by Australian Hearing followed the second path to the highest degree possible with the knowledge available at the time when the clinical protocols were finalized in 2012 prior to the commencement of the trial.
Optimal remediation of CAPD depends on accurate identification of the type of disorder present. However, differentially diagnosing deficits in auditory processing from the myriad of learning and attention disorders that mimic the behavioral manifestations of CAPD is a complex and challenging task for the researcher and clinician alike.2 The assessment tools implemented by the Australian Hearing CAPD service were designed to test for listening difficulties that are specifically linked to poor educational outcomes and for which there are remediation or management options that have been scientifically validated as improving children's outcomes. For example, spatial processing disorder (SPD),3 a specific form of CAPD characterized by a deficit in the ability to utilize binaural cues to achieve spatial release from masking, is assessed using the Listening in Spatialized Noise–Sentences Test (LiSN-S).4 5 6 7 8 9 10 SPD is more likely to occur when children have had extensive or repeated bouts of otitis media during their early childhood. In addition, the earlier the onset and the greater the duration of otitis media, the greater the resulting deficit in spatial advantage, even though the otitis media has entirely resolved when the child is later assessed for SPD.11 12 The condition can be reversed with deficit-specific auditory training with the LiSN & Learn software,13 which is computer-administered in the home environment.3 14 15
The LiSN-S and the LiSN & Learn were both developed by the National Acoustic Laboratories and have been the subject of extensive research over the past 10 years. This article provides an appraisal of the performance of assessment and rehabilitation tools like LiSN-S and LiSN & Learn when used in a clinical environment, removed from the researchers who devised the tools.
In contrast to typical CAPD clinical assessment protocols, Australian Hearing's service is based upon a hierarchical test battery structure.16 The rationale for such a structure is described in detail in the diagnostic assessment procedures section that follows and is summarized in Fig. 1. An additional consideration regarding the test battery construct was the desire to include a diagnostic test only if an evidence-based, commercially available, home-based remediation option existed to treat the disorder that the diagnostic test was designed to detect. Whereas this was not the case for the dichotic digit test, nonetheless it was included in the test battery due to the wide usage of this assessment tool worldwide and due to the high proportion of children referred for CAPD assessment who perform outside normal limits on this test.17 A frequency modulation (FM) system was offered to those clients diagnosed with a binaural interaction deficit as such devices provide an immediate improvement in signal-to-noise ratio (SNR), irrespective of the cause of the problem. Furthermore, there is evidence that amplification with assistive listening devices provides therapeutic benefits for children with CAPD and that sustained exposure to high SNR speech improves the precision of processing within the brainstem.18 19 An important aspect of the evaluation, as described in this article, is that the children's outcomes were assessed using a variety of measures, which has allowed for the evaluation of both the test battery and the rehabilitation options provided.
Figure 1.
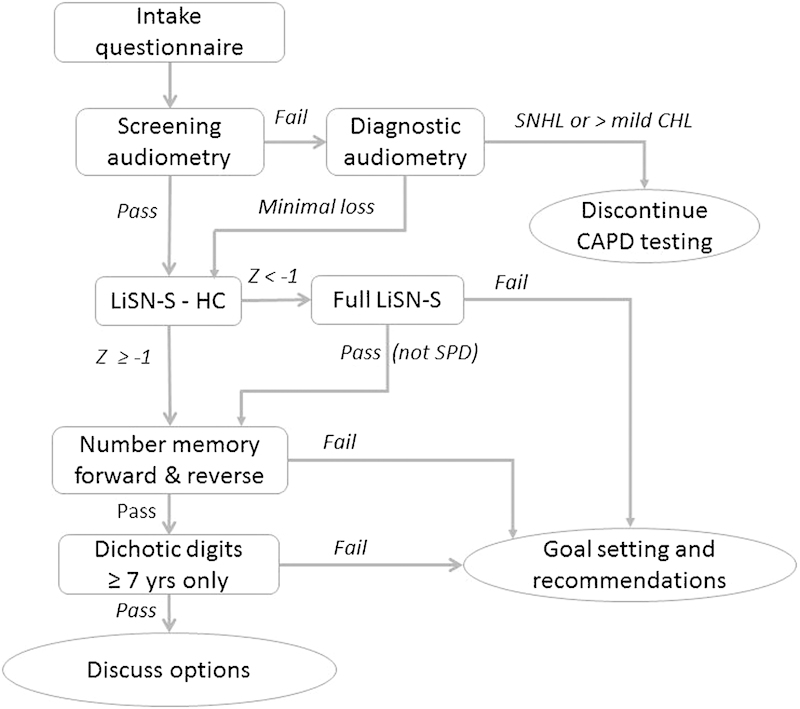
Flowchart of the test appointment procedure used. Abbreviations: CAPD, central auditory processing disorder; CHL, conductive hearing loss; HC, high cue; LiSN-S, Listening in Spatialized Noise–Sentences Test; SNHL, sensorineural hearing loss.
The following methods and results section is divided into two segments. The first section covers the diagnostic assessment of the 666 children who were assessed as part of the CAPD service over a 20-month period. The second section covers the remediation and management of children diagnosed with a disorder at their assessment appointment. The discussion and conclusion sections will cover both the diagnostic assessment and remediation outcomes.
Diagnostic Assessment
Methods
Participants
Thirty-eight Australian Hearing clinics introduced central auditory processing assessments to their services between April 2012 and December 2013. During this period, 700 individuals were assessed for CAPD. Written consent was obtained from each individual or their parent or guardian in the case of children age less than 18 years; the results of their assessments were provided to the National Acoustic Laboratories (NAL) for analysis. Of the 700 individuals tested, results from 34 were excluded prior to analysis due to deviations from the testing protocols. The following analysis reports results for the remaining 666 individuals. age 6, 0 (years, months) to 24, 8 with a median age of 9, 0.
Test Materials
Preappointment Questionnaire
A short questionnaire, developed specifically for the service, was used to form the basis of the appointment case history. The 26 questions in the questionnaire were designed to be completed by the parent, or adult client, prior to the appointment. The questionnaire is divided into five sections; general history, description of difficulties experienced, birth and development information, medical history, and educational information. The general history section includes eight demographic questions including a question regarding the client's first language. The difficulties section includes six questions designed to elicit details regarding the auditory difficulties that are being experienced, including whether the difficulties are exacerbated by noise. Three questions are included in the birth and development section, with the primary goal of determining whether risk factors for Auditory Neuropathy Spectrum Disorder are present. The medical history section includes five questions relating to potentially relevant medical factors such as history of ear infections, head injuries, or surgeries and previous hearing testing. Given it was anticipated that the majority of clients would be of school age, the final section includes four questions focused on the impact that any auditory difficulties were having on school performance as well as on whether any concerns were being raised by the child's teacher.
Listening in Spatialized Noise–Sentences Test
LiSN-S is a test of spatial processing ability conducted under headphones using stimuli that have been convolved with head-related transfer functions to provide a sense of spatialization.6 9 10 The LiSN-S contains simple sentences presented in a background of two children's stories. Four conditions are incorporated into the test. In each condition the target sentences voiced by a female speaker are spatialized to appear as if coming from 0 degrees azimuth. The conditions differ from each other based on the location of the distracting speech (either 0 degrees azimuth or ± 90 degrees azimuth), and/or the vocal identity of the distracting voices (either the same female speaker or two different female speakers). The baseline test conditions are referred to as “different voices 90 degrees” or high-cue speech reception threshold (SRT); “same voice 90 degrees”; “different voices 0 degrees,” and “same voice 0 degrees” or low-cue speech reception threshold (SRT). Each condition contains a total of 30 sentences. The sentences were initially presented at an SNR of 7 dB and then were adapted based on whether the participant correctly repeated more than or less than 50% of the words correctly in each sentence. After a period of practice, testing in each condition continued until all 30 sentences were presented, or at least 17 scored sentences were presented and the standard error was less than 1 dB. Results are reported by the software in decibels of SNR, and as z scores (i.e., population standard deviations [SDs] above or below the age-appropriate mean). As well as the four baseline measures, three difference scores are calculated—spatial, talker, and total advantage—which reflect the benefit in decibels obtained when spatial, talker, or both spatial and talker cues are available to the listener. The software also reports a spatial processing pattern z score (i.e., in population SDs), which reflects the benefit of spatial separation, averaged across both the same voice, and different voice, conditions.12
Test of Auditory Processing–Third Edition Number Memory Forward Subtest
The number memory forward (NMF) subtest of the Test of Auditory Processing–Third Edition (TAPS-3) is a measure of verbal short-term memory.20 Digit sequences of increasing length were presented live voice by the audiologist. The digits were presented at a rate of one digit per second. The client was tasked with repeating the digits back in the order they were heard. If the digits were repeated in the correct order, without any additional digits inserted, a score of 2 was recorded. If an error was made in the order that the digits were repeated, then the item was scored as 1. If any digits were omitted or inserted during repetition, then a score of 0 was recorded. Testing was discontinued once three consecutive 0-point responses were recorded.
Test of Auditory Processing–Third Edition Number Memory Reversed Subtest
The number memory reversed (NMR) subtest of the TAPS-3 is a measure of verbal working memory. Digit sequences of increasing length were presented live voice by the audiologist, at a rate of one digit per second. The client was tasked with repeating the digits back to the audiologist in the reversed order. Scoring for the NMR was based on the same rules as used for the NMF, as discussed above.
Dichotic Digits Test
The Dichotic Digits Test (DDT) is a test of binaural integration.21 The recordings were presented via the Avante A2D (MedRx, Sonic Innovations, Somerset, NJ) speech audiometry interface through the clinician's laptop at 50 dB (hearing level [HL]). Testing was conducted under headphones. In each trial, two digits, taken from the stimulus set 1, 2, 3, 4, 5, 6, 8, 9, 10, were presented to the right ear at the same time as two different digits were presented to the left ear. Participants were tasked with repeating all four digits heard regardless of the order they were heard in. Five practice items were presented before 20 scored items. A percent score was calculated for the left and right ear and compared with the published normative data.22
Procedures
To avoid the potential confounds of administering a large test battery, such as fatigue or inflation of the statistical error, a hierarchical testing structure was used.16 This test structure is outlined in Fig. 1. This order of testing was chosen based on the following considerations. First, an effective disorder-specific treatment is available for children with SPD,12 13 and children with this condition do not typically have any other auditory deficit detectable with a typical CAPD test battery.8 Consequently, the LiSN-S test was performed first. Second, it is known that poor verbal memory is associated with poor performance on dichotic tests, as multiple items have to be identified, remembered, and repeated back.23 24 25 26 Although the direction of causation is not known, it seems plausible that poor memory will adversely affect dichotic test scores, so verbal memory, for which a deficit-specific remediation was also available, was tested second. The dichotic digit test was administered last, as it was then possible to apply it only to children with verbal memory (based on the NMF and NMR tests) in the normal range.
Prior to any of the CAPD tests being undertaken, each participant's hearing was screened to 20 dB (HL) at octave frequencies between 250 Hz and 4,000 Hz. For participants who failed this initial hearing screen, a full audiogram was completed, including both air conduction and bone conduction, to determine the degree and type of the hearing loss. For participants diagnosed with a sensorineural hearing loss (four-frequency average hearing loss at 500, 1,000, 2,000, and 4,000 Hz > 20-dB HL) or a conductive hearing loss, which exceeded mild in degree (four-frequency average hearing loss > 40-dB HL in one or both ears), no further testing for CAPD was undertaken and the client was referred for further evaluation by Australian Hearing.
Participants who passed their hearing screening or who had only a minimal conductive loss were assessed on the high-cue condition of the LiSN-S. Participants who obtained a score that was worse than −1 SD from the mean score relative to age were assessed with the three remaining conditions of the LiSN-S (same voice 90 degrees, different voices 0 degrees, and same voice 0 degrees). Based on an examination of data collated from 241 individuals from several studies conducted at the NAL using the LiSN-S, if a person obtained a score better than or equal to −1 SD on the LiSN-S high-cue SRT condition, he or she was unlikely to have a score worse than −2 SD on the LiSN-S spatial advantage measure (see Appendix A). If the full LiSN-S results were consistent with SPD, as indicated by a spatial processing pattern score of ≤ − 1.96 SDs from the mean, the CAPD testing was discontinued and the audiologist proceeded with recommendations regarding SPD remediation.
For individuals who scored better than or equal to −1 SD on the high-cue condition, or who passed the full LiSN-S, assessment continued with verbal memory testing. Both the NMF and NMR were administered. The raw scores obtained were then converted into scaled scores based on the normative data.20 If a scaled score of 6 or less (corresponding to a z score of −1.33 or less) was found on either the NMF or NMR, CAPD testing was discontinued and the audiologist proceeded with recommendations regarding remediation for memory deficits. In the case of individuals who passed both memory tests and who were age 7 years or older, the DDT was administered and results interpreted. If outside the normal range, and if the parent believed that the child's listening difficulties were most apparent when there was background noise, the use of an FM system to improve the SNR received by the child was discussed. If a child passed all the tests and he or she did not report difficulties listening in noise in the preappointment questionnaire, the family was provided with a list of management strategies and the clinician specified which of these strategies were relevant to their reported difficulties. If difficulties listening in noise were noted on the preappointment questionnaire, an FM system was recommended, as well as the management strategies.
Statistics
Statistical analysis was completed using Statistica version 10 (StatSoft, Inc., Tulsa, OK).
Results
A summary of the data is provided in Fig. 2. In total, 408 individuals were diagnosed with a deficit in one of the three areas assessed. One hundred thirty individuals (19.5% of the sample) were diagnosed with SPD.
Figure 2.
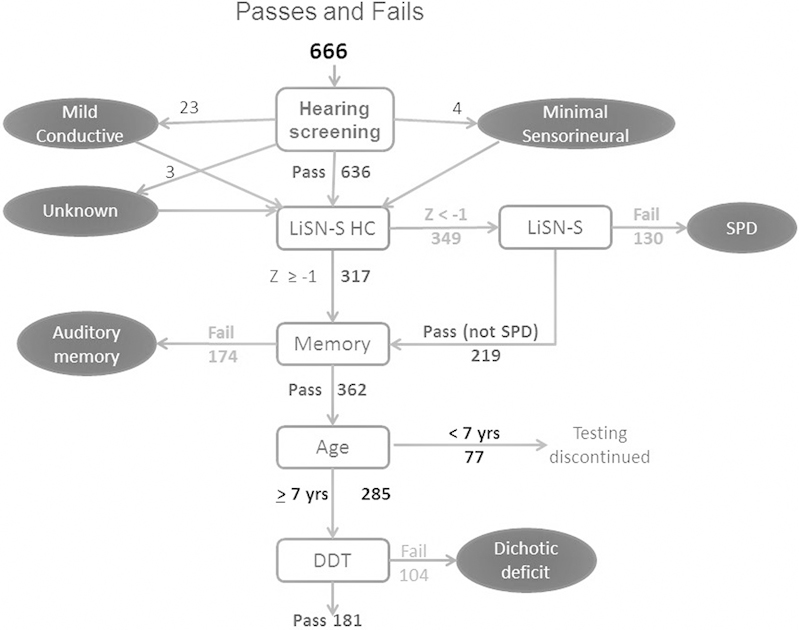
Summary of diagnostic results (n = 666). Abbreviations: DDT, Dichotic Digits Test; LiSN-S HC, high-cue; LiSN-S, Listening in Spatialized Noise–Sentences Test; SPD, spatial processing disorder.
Of the 536 remaining clients who underwent testing with the NMF and NMR subtests of the TAPS-3, 174 (32.5%) were identified as having deficits in either short-term memory or working memory. Table 1 shows the breakdown of how the 174 fails were distributed between NMF and NMR. Two hundred eighty-five individuals went on to be assessed with the DDT. Of these, 104 (36%) failed the DDT in at least one ear (see Table 2 for a distribution of fails by ear).
Table 1. Verbal Memory Results (n = 536).
| Results | NMF | |
|---|---|---|
| Pass | Fail | |
| NMR | ||
| Pass | 362 | 67 |
| Fail | 58 | 49 |
Table 2. Dichotic Digits Test Results (n = 285).
| Results | Right Ear | |
|---|---|---|
| Pass | Fail | |
| Left ear | ||
| Pass | 181 | 27 |
| Fail | 44 | 33 |
Remediation and Management
Methods
Participants
A total of 408 individuals age 6, 0 to 18, 7 were diagnosed with a deficit in one of the three areas assessed. Of these individuals, 130 (age 6, 0 to 13, 0) were identified as having an SPD. A total of 174 individuals (age 6, 0 to 18, 7) were diagnosed with a deficit in one or more areas of memory. The remaining 104 (age 7, 0 to 14, 7) were found to have a binaural integration deficit. Each of the 408 participants was offered the opportunity to undertake a computer-based training program and/or be fitted with a wireless remote hearing aid, referred to as a FM system, depending on the deficit identified. A total of 150 clients decided to proceed with remediation or management.
Procedure
Three remediation or management options—the LiSN & Learn,11 Memory Booster,27 and/or an FM system—were offered to the individuals based on the deficit identified (see Table 3). Prior to any training or remediation option commencing, rehabilitation goals were established using the NAL Client Oriented Scale of Improvement–Children (COSI-C).28 A copy of the Listening Inventory for Education–Teacher Scale (LIFE) also was given to the parent to be passed on to the participant's main teacher along with instructions asking the teacher to complete and return the scale upon conclusion of the training/trial period.29 30 The remediation/management options and outcome measures are described in detail below.
Table 3. Potential Remediation Options for Each Identified Deficit.
| Deficit | Remediation | |||
|---|---|---|---|---|
| Options | Recommended/Offered | Taken Up | Training Completed (as of December 2013) and Follow-up Data Available | |
| SPD | LiSN & Learn | 130 | 69 | 40 |
| FM System* | – | 3 | ||
| Auditory memory deficit | Memory Booster | 174 | 52 | 29 |
| FM System* | – | 4 | ||
| Binaural integration deficit | FM System | 104 | 19 | N/A |
Abbreviations: FM, frequency modulation; SPD, spatial processing disorder.
Note: Deficit-specific auditory training was recommended to all clients who were diagnosed with SPD or a memory deficit, while noting that the software is most appropriate for 6- to 11-year-olds.
FM system fitting for clients diagnosed with SPD or memory deficits occurred as part of a clinical discussion taking into account individual goals and also depended on whether the parent or client wished to take action to resolve the listening difficulty prior to completing the LiSN & Learn or Memory Booster. Further, an FM system was only recommended to clients with memory deficits who reported that background noise exacerbates difficulties.
The client was requested to attend the audiology clinic to evaluate the efficacy of his or her training within 2 weeks of program completion. Clients fitted with an FM were offered a follow-up appointment 6 weeks after the fitting. (Although this was the guideline, actual follow-up appointment times depended upon the availability of the client and the audiologist.) Participants with SPD who had received LiSN & Learn training were retested on the LiSN-S. Those diagnosed with a memory deficit who undertook Memory Booster training were reassessed on the TAPS-3 NMF and NMR. For clients who elected to use an FM system for dichotic deficits, or in conjunction with any of the training software modules, FM usage and management were reviewed at the follow-up appointment. For all clients, the amount of change observed on the COSI-C goals was established, and the results of the LIFE returned by the teacher were discussed.
Remediation Materials and Outcome Measures
LiSN & Learn
The LiSN & Learn auditory training software is a remediation program designed for use with children with SPD.3 11 The training program includes five training games presented on a personal computer over Sennheiser HD215 headphones (Sennheiser, Germany). In each of the training games, distracting speech is presented. The distracting speech takes the form of two children's stories that have been convolved with nonindividualized head-related transfer functions so that they are perceived as coming from ± 90 degrees azimuth. In four of the five training games, grammatically correct but semantically meaningless target sentences are presented from 0 degrees azimuth. After the target sentence, four images appear on the computer screen and the participant is tasked with selecting a picture that matches one of the words in the sentence heard. In the fifth training game, target sentences in the form of directions are presented from 0 degrees azimuth (e.g., “Move left three spaces”). The participant responds by selecting the direction and number of spaces heard from a visual display. All of the training games employ an adaptive procedure to adjust the SNR and determine a speech-reception threshold over 40 sentences.
Participants who opted to undertake LiSN & Learn training were advised to complete two training games per day, 5 days per week until 100 games were completed. The training was completed in the participant's home, and progress was monitored by his or her clinician three times during the training period. Parents were asked to e-mail the clinician a training report generated by the software after the child completed 10, 50, and 100 training games. Feedback was provided to the parents after each of the training reports were received. In the case that reports were not received from the parents, clinicians attempted to follow up with the family via phone and email.
Memory Booster
Memory Booster is a computer-based training program that teaches different memory strategies for children.31 The program is introduced through a short animated story and then children are presented with the concepts of rehearsal, visual imagery, creating stories, and chunking. After each strategy is introduced, the child is provided with a period of training. During this training period, the child is given either a single item or a series of items to remember before several images appear on the computer screen. Among the images are the item(s) the child was tasked with remembering, and the child selects these using the computer mouse. The program adapts in difficulty, both in terms of the number of items to be remembered and in terms of the delay between the child hearing the item(s) and the images appearing on the screen for selection.
Memory Booster training involved 15 to 20 minutes of training per day, 5 days per week, for 8 weeks. As with the LiSN & Learn, Memory Booster training was completed in the participant's home and progress was monitored via training certificates generated by the software, which were emailed to the clinician on three occasions. Participants who missed training sessions were advised to add additional training sessions to the end of the training period until the required 8 weeks' worth of training had been finished. Clinicians provided feedback to the participant and their family after each report was received.
FM Systems
Three different FM receivers were offered through the service. The iSense Classic FM receiver by Phonak (Phonak, Stafa, Switzerland) is a body-level receiver worn on a lanyard around the neck and connected to two in-the-ear receivers by a thin Y-cable to deliver the FM signal binaurally. For participants who preferred a more discrete option, the iSense Micro ear level receiver was offered (either unilaterally or bilaterally). When one receiver was fitted, the choice of ear was based on client preference. The third receiver option was the Amigo R5, a body-level receiver used with lightweight headphones or binaural earbuds, which is manufactured by Oticon (Oticon, Denmark). Individuals who were fitted with either of the iSense FM receivers were provided with an Inspiro FM transmitter Vietnam. The Amigo R5 receiver was paired with the Amigo T5 transmitter (Oticon, Inc., Somerset, NJ).
Participants who chose to proceed with FM fitting attended the clinic for an additional appointment to be issued with their FM system (unlike for the other remediation options that could be offered during the assessment appointment because the hierarchical test structure allowed the time for this with the other items). At this fitting appointment, the participant and their family were shown how to operate both the transmitter and receiver component of the system, how to put on the receiver and change batteries, and how to perform any cleaning that was required. Subjective checks of maximum output and the volume of the device were performed. The gain of the iSense Micro can be adjusted by the clinician via the Inspiro transmitter. The iSense Classic has a nonlockable volume control that the child can access. The Amigo has a volume control that can be locked or unlocked as considered appropriate by the clinician. The participant used the FM system for 6 weeks before returning to the clinic for a follow-up appointment. Parents and clients were instructed during the appointment in the use of the FM. Written instructions were also provided to the parents. The parent liaised directly with the client's teacher regarding FM use in the classroom. If the teacher had any questions regarding FM usage, he or she was able to seek assistance from the audiologist.
Client Oriented Scale of Improvement–Children
The COSI-C is a clinical tool developed by NAL that can help direct a child's habilitation program as well as document the benefit that the habilitation program has provided. The client's individual goals and needs were documented following a discussion with the family. The SMART guidelines for developing goals ensuring they are specific, measurable, achievable, realistic, and timely.32 Improvements in hearing ability are measured on a four-point scale (no change; small change; significant change; goal achieved).33
Listening Inventory for Education–Teacher Scale
The LIFE–Teacher is a measure of postintervention listening difficulty comprised of 16 items, each describing an educational situation. For example, item 4 asks whether attention has improved when listening to directions presented to whole class. Item 16 reads: “Based on my knowledge and observations I believe that the amplification system is beneficial to the student's overall attention.” The words amplification system were changed to training software for children who received LiSN & Learn or Memory Booster training. A 5-point response scale is used from +2 (agree) to −2 (disagree). All items are added to produce a composite score on an incremental scale from −35 to +35 (i.e., a continuum from “the intervention was highly unfavorable” to “strong positive change/intervention was highly beneficial”).
Results
Lisn & Learn
LiSN & Learn training was commenced by 69 children. At the time of data analysis (December 2013), 41 children had completed training. A range of reasons were supplied for the 28 participants who had not complete the training at the time of analysis, including three for whom training was ongoing, and these are outlined in Fig. 3. Of the 41 children who completed training, follow-up data were available for 40 children. Training took an average 20.2 weeks to complete (range: 10.7 to 43.6).
Figure 3.
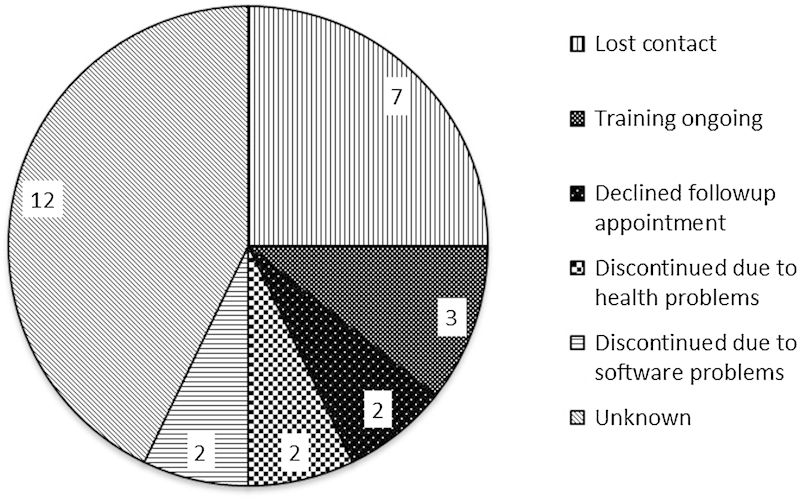
Pie chart displaying reasons provided for incomplete LiSN & Learn training (n = 28).
Due to the clinical nature of the service, full follow-up data were not available for all participants. In some instances, follow-up appointments had to be cut short due to poor client cooperation or time constraints. In others, objective testing with the LiSN-S was completed but the subjective measures of improvement—the LIFE and the COSI-C—were not completed. The data set analyzed (40 cases) contained 33 full LiSN-S and COSI-C results, 6 LiSN-S high-cue results only, and 15 LIFE results.
The available posttraining data were analyzed to investigate the efficacy of the training program. A repeated-measures analysis of variance (ANOVA) revealed a significant difference in LiSN-S results between pre- and posttraining (see Fig. 4). Planned comparisons were conducted to determine which of the changes between pre- and posttraining testing on the LiSN-S were significant. Significant improvements were found for the low-cue SRT (F [1, 33] = 14.9, p = 0.0005), high-cue SRT (F [1, 39] = 71 = 71.7, p < 0.00001), spatial advantage (F [1, 33] = 46.5, p < 0.00001), and total advantage (F [1, 33] = 33.3, p < 0.00001). No significant difference was found between pre- and posttraining on the talker advantage measure (F [1, 33] = 1.9, p = 0.183).
Figure 4.

Mean performance on the LiSN-S pre- (dashed line) versus post- (solid line) LiSN & Learn training (n = 40 high cue; n = 34 other conditions) *conditions with significant differences over time are preceded by an asterisk. Performance is expressed in population standard deviation units from the mean. Error bars represent 95% confidence intervals. Abbreviations: adv, advantage; LiSN-S, Listening in Spatialized Noise–Sentences Test.
An examination of individual results for the 33 participants for whom full posttraining LiSN-S results were available showed that the pattern measure improved for 30 of these participants and fell within the normal range for 27 of them, as shown in Fig. 5.
Figure 5.
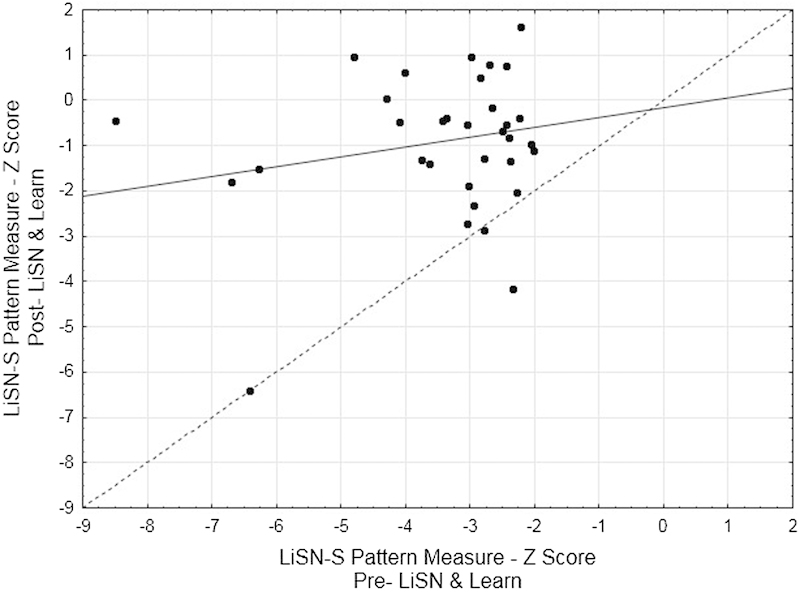
Scatterplot of Listening in Spatialized Noise–Sentences Test (LiSN-S) pattern score pre- versus post-LiSN & Learn training (n = 34). Solid line represents least squares regression line. The dashed line indicates no change in performance after training.
Of the 33 participants for whom the COSI-C was completed, only 3 reported no change for their set goals. The majority of participants reported significant change (see Fig. 6). For the 15 participants for whom the LIFE questionnaire was returned by the teacher, on the incremental scale from −35 to +35, mean improvement score was 19 (range −1 to 35).
Figure 6.
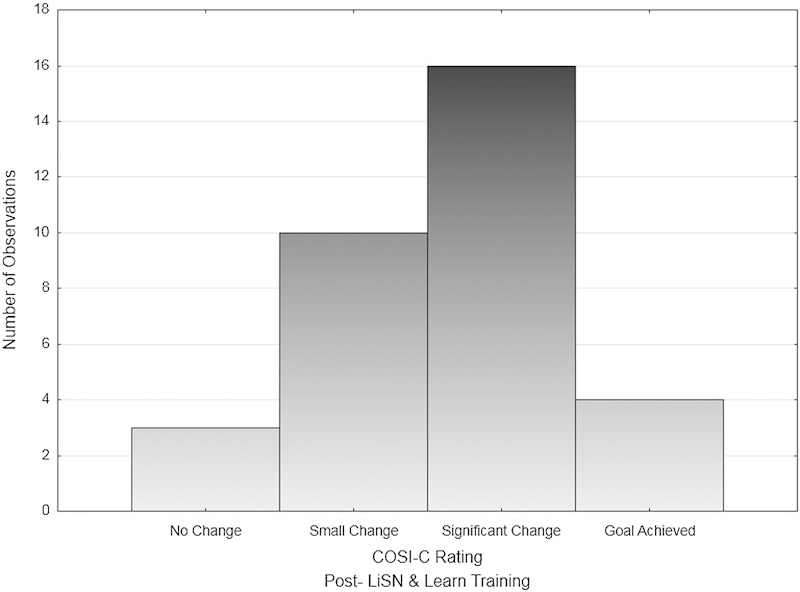
Histogram of Client Oriented Scale of Improvement–Children (COSI-C) ratings for participants who completed the LiSN & Learn (n = 33).
Memory Booster
Memory Booster training was commenced by 52 children and completed by 30. Follow-up data were available for 29 of these children. The reasons provided for why training was not completed are shown in Fig. 7. Of the 29 participants, training took on average 16.3 weeks to complete (range: 7.8 to 36.1). As with the LiSN & Learn results discussed above, full follow-up data were not available for all participants. The analyzed data set contained 29 NMF and NMR results, 25 COSI-C results, and 12 LIFE results.
Figure 7.

Pie chart displaying reasons for incomplete Memory Booster training (n = 21).
Memory Booster is recommended for children who fail either, or both, of the TAPS-3 conditions (that is, NMF and/or NMR). There were cases, therefore, where a child failed NMR but passed NMF and undertook the training (and vice versa). Therefore, in the following analyses, if a child undertook training because he or she failed only one subtest of the TAPS-3 (and was within normal limits on the other subtest), that child would be only included in the analysis for which he or she was outside normal limits. Of the 29 children for whom data were available, 18 failed NMF, 17 failed NMR, and 6 failed both.
To determine whether Memory Booster training was effective in remediating either short-term memory deficits or working memory deficits, two repeated-measures ANOVAs were conducted. Posttraining performance on the NMF scaled score was found to be significantly better than pretraining performance (F [1, 17] = 11.769, p = 0.003). However, the average posttraining NMF score remained outside the normal range (Fig. 8A), raising questions about the efficacy of Memory Booster training in terms of returning short-term memory abilities, of the type measured by NMF and NMR digit span tests, to within the normal range. Posttraining performance on the NMR scaled score also was found to be significantly better than pretraining performance (F[1, 16] = 14.236, p = 0.002). Posttraining, the mean score on NMR was 7.53, which is within the normal range (see Fig. 8B). However, based on the 95% confidence intervals it is difficult to conclude with any confidence that Memory Booster training, even on average, can return auditory working memory performance to normal. As reflected in the individual results shown in Fig. 9A and B, the scores for many children remain outside the normal range posttraining, with scaled scores lower than 7.
Figure 8.
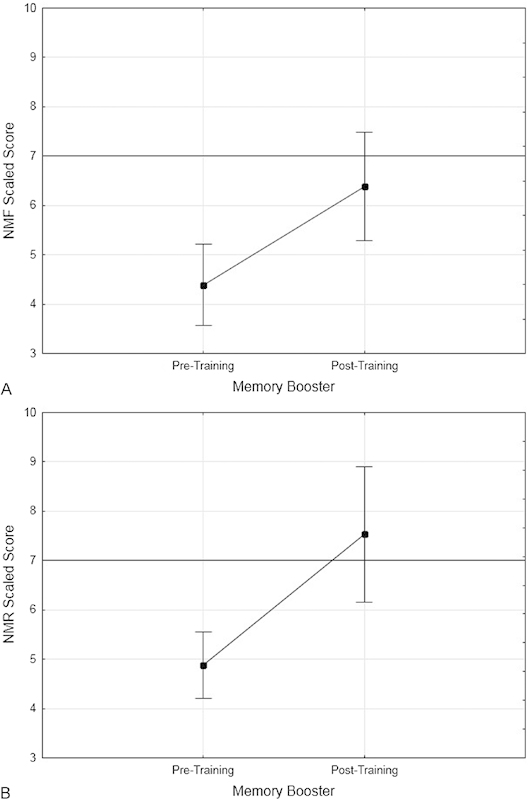
Dot plot of mean results on the (A) number memory forward (NMF) and (B) number memory reversed (NMR) Test of Auditory Processing–Third Edition subtests (n = 18 and 17, respectively) pre- and posttraining with Memory Booster. Error bars represent the 95% confidence intervals.
Figure 9.
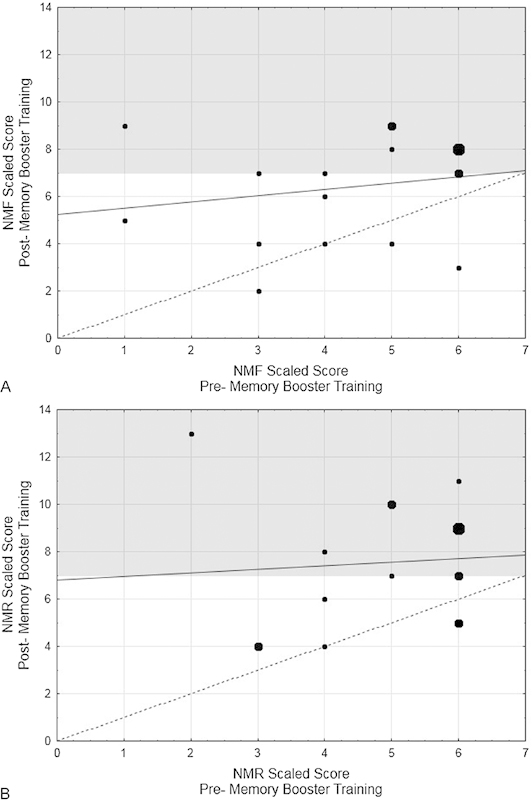
Scatterplot of individual results on the (A) number memory forward (NMF) and (B) number memory reversed (NMR) Test of Auditory Processing–Third Edition subtests (n = 18 and 17 respectively) pre- and posttraining with Memory Booster. Large dots represent data points for three participants, medium dots represent two participants. Solid line represents least squares regression line. The dashed line indicates no change in performance after training. The shaded area represents performance within normal limits.
Of the 25 participants for whom the COSI-C was completed, only three reported no change for their set goals. The majority of participants reported small or significant change (see Fig. 10). For the 12 participants for whom the LIFE questionnaire was returned by the teacher, on the incremental scale from −35 to +35 mean improvement score was 15 (range −2 to 32).
Figure 10.
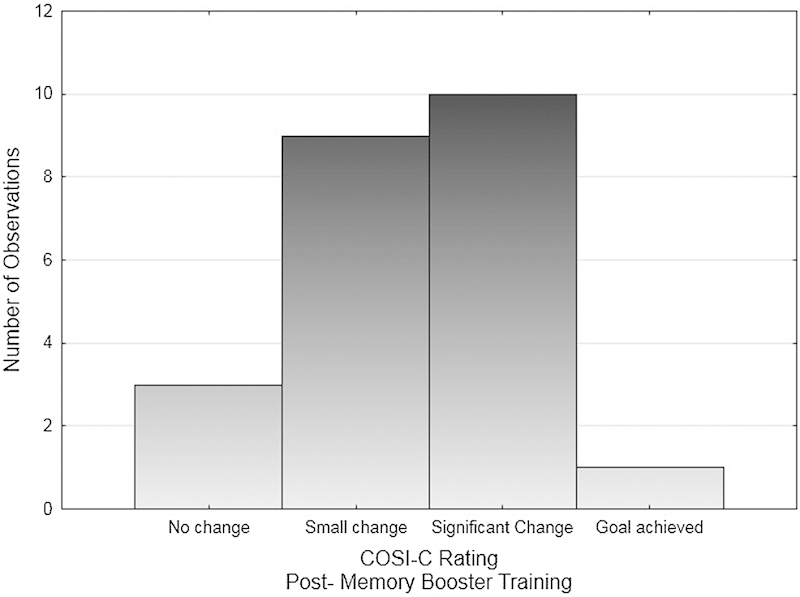
Histogram of Client Oriented Scale of Improvement–Children (COSI-C) ratings for participants who completed Memory Booster training (n = 25).
FM Systems
Twenty-nine participants were fitted with an FM only (19 diagnosed with dichotic deficits, 4 with memory deficits, 3 with SPD, and 3 who passed all tests but reported deficits listening in noise). Sixteen (55%) returned for their follow-up appointments. Fig. 11 displays the range of COSI-C results obtained. All participants reported some positive change against their identified goals following FM fitting. Furthermore, positive improvement was reported for eight participants by each of the teachers who had returned the LIFE questionnaire (mean score = 24.3, range: 6 to 35).
Figure 11.
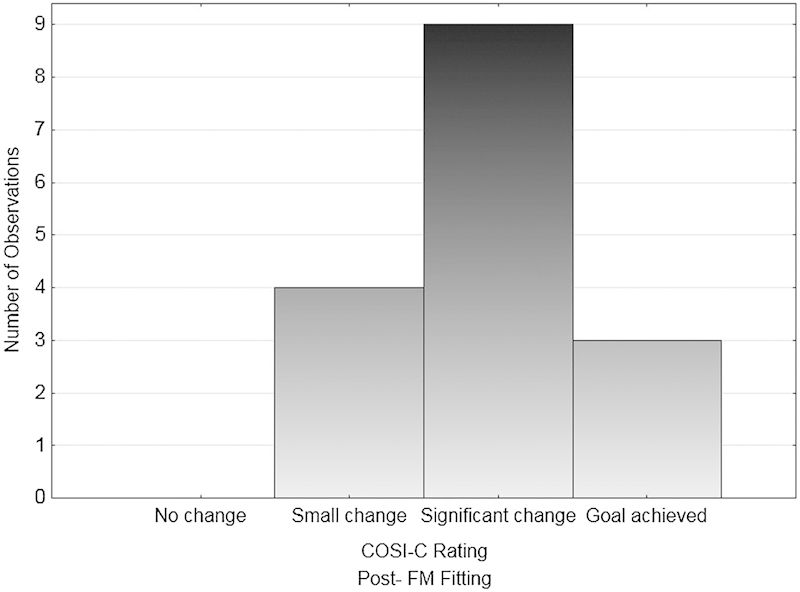
Histogram of Client Oriented Scale of Improvement–Children COSI-C scores for participants fitted with a frequency modulation system (FM) only (n = 16).
Discussion
The analysis of outcomes from the Australian Hearing CAPD service revealed that of the 666 clients assessed over an 18-month period, 408 (61%) were identified with either a subtype of CAPD or a verbal memory deficit. Of those, 130 clients (32%) were diagnosed with an SPD; 104 (25%) were identified as having a binaural integration deficit, and 174 (43%) had a verbal memory deficit. The relatively high rate of clients diagnosed with SPD (20% of the 666 clients assessed) may be attributed to the recruitment materials, which specifically targeted those with listening deficits in noise. Due to the growing evidence that SPD is highly correlated to duration and age of onset of chronic otitis media,14 15 asking ear, nose, and throat specialists to inform parents that protracted otitis media may lead to SPD may increase the detection rates of the disorder when the children are older.
Considering that the test battery was developed, where possible, to include only diagnostic tools for which there was deficit-specific, at-home training available should a deficit be detected, of some concern was the low uptake of training and/or remediation options. Only 69 clients (53%) diagnosed with SPD elected to take up LiSN & Learn training; 52 (30%) diagnosed with verbal memory deficits commenced training with Memory Booster software, and 19 clients (18%) diagnosed with binaural interaction deficits purchased an FM system. It is not clear why so many parents/clients chose not to proceed with a targeted management option. In the case of verbal memory, it is possible that as deficits in this area are not in the realm of auditory processing, and the TAPS-3 NMF and NMR tests were included mainly to rule out memory deficits that may impact on dichotic digit performance, parents preferred to investigate further testing with an educational psychologist and/or explore other training avenues. However, in respect to SPD, the LiSN & Learn is the only training option available for treatment of this form of CAPD. If the training software was purchased through the Australian Hearing center, the client was monitored during training and assessed posttraining, and an additional cost was added to the price of the software to cover the provision of this service. It is possible that parents may not have wanted to pay for this service and decided to purchase the software directly. Parents may also not have had access to a compatible personal computer or they may have simply wished to proceed with the compensatory strategies provided to all clients. Alternatively, the benefits of training may not have been clear to the parent. The rate of uptake of FM systems for those diagnosed with binaural integration deficits was very low. One reason for this may be willingness of the client to use the device in the classroom. Furthermore, funding for personal FM systems is not provided by the Australian education system. Whereas a variety of FM systems were offered that ranged in price, it is unclear whether the cost of the device was a factor in the low uptake of this management option.
For the clients who did decide to take up training for SPD and who had completed that training at the time of analysis, and for which complete follow-up data were available (n = 33), the real-world results mirrored those found in research studies. Repeated-measures ANOVA revealed significant differences between average pre- and posttraining scores on the LiSN-S test for all spatial processing measures. Further, 27 children (82%) were within the normal range across all LiSN-S measures posttraining, and 30 (91%) reported a change in performance posttraining based on the set goals in their COSI-C rating, with 20 (61%) noting a significant change or goal achieved. LIFE teacher ratings saw an average improvement score of 19 (on a scale of −35 to +35). The similarity of LiSN & Learn outcomes in the clinical setting to the results of research studies may be due to the fact that the design of the research studies were more in line with an effectiveness trial rather than an efficacy trail, in that training took place in the child's own home on the home computer and under parent supervision rather than in the laboratory setting.14 15
For the 29 children who completed the Memory Booster and for whom diagnostic test follow-data were available, the average posttraining scores for both NMF and NMR were significantly better than the pretraining scores. However, for NMF the average of the posttraining scores was still outside the normal range. For NMR, the average was within the normal range but not for every individual. Although the memory training results might be considered disappointing, with many scores remaining outside the normal range after training, especially for the NMF test, the degree of improvement in the NMF and NMR scores was still substantial. The mean improvement in the NMF and NMR scores were equivalent to 1.3 and 1.7 population SDs, respectively, on these tests. This marked improvement is reflected in the COSI results for those undergoing this training, with 20 of 25 children for whom these data were available (80%), reporting a change in performance posttraining, and with 11 of these (44%) noting a significant change or goal achieved. To this end, the nature of much of Memory Booster training provided (especially creating imagery and stories) is unrelated to the abilities used to perform the digit span test, either forward or reverse. It is possible that the children had more generalized memory deficits, of which the digit span test results are but one reflection. If so, the training may have provided benefits that were not apparent in the digit span repeat testing, but which were apparent to the children's' parents, and which led them to give the mostly positive ratings evident in Fig. 10. Likewise, for the children fitted with an FM system for any reason (binaural integration disorder, memory deficits, SPD or generalized deficits listening in noise), positive change was reported for both the COSI-C and LIFE teacher ratings.
The LiSN & Learn and Memory Booster took, on average, twice as long to complete than the time recommended. The specific reasons for such delays are unknown, but based on anecdotal information reasons could include illness, family matters, vacations, and computer issues. Finally, considering the postremediation improvement in diagnostic test scores—particularly for children with SPD who undertook LiSN & Learn training—and that the positive COSI outcomes indicate that the remediation undertaken and/or FM fitting was valued, it seems reasonable to adopt a hierarchical testing approach and proceed with correcting a deficit once found, even though testing is not performed to determine if other deficits exist. Certainly this approach helped to minimize the expense to the parents.
Conclusions
This article has provided a real-world evaluation of a CAPD diagnostic and remediation service over an 18-month time period over a large number of hearing centers in differing socioeconomic and regional areas. In general, the client recruitment strategies resulted in a relatively high proportion of deficits detected. The hierarchical nature of the test battery resulted in a time-effective diagnostic procedure that minimized the demand on client attentional resources and, as such, had the potential to more accurately determine the true nature of client deficits. It also minimized the financial cost of the service to the families. The emphasis on only using assessment tools for which at-home, deficit-specific training existed ensured that in most cases clients who were diagnosed with a disorder could be offered remediation that had the potential to resolve their issues. Although uptake of remediation options was lower than expected, results of training were encouraging and certainly in the case of auditory training for SPD reflected research outcomes. Indeed, ratings of postremediation client and teacher outcome measures across all remediation options showed that the remediation had a very positive impact. Whereas the results of the study are positive, it should be borne in mind that there is always room for improvement in respect to both diagnostic and remediation services for CAPD, and clinicians should view development and administration of their services as a dynamic process that should be constantly evaluated in light of the results of the ever increasing research available in this area.
Acknowledgments
The authors would like to acknowledge the financial support of the Commonwealth Department of Health. Parts of the research described in this article were presented at the XXXII World Congress of Audiology, Brisbane, Australia, May 2014.
Footnotes
Declaration of Interest This research was funded by Australian Hearing. The authors would like to disclose that the LiSN-S test described in this article is distributed under license by Phonak Communications AG. The LiSN & Learn auditory training software described in this article is distributed by the National Acoustic Laboratories. Financial returns from the sale of the LiSN-S and the LiSN & Learn benefit the National Acoustic Laboratories and Dr. Cameron.
Appendix A
Calculation of Cutoff Score on Listening in Spatialized Noise–Sentences Test High-Cue Speech Reception Threshold Condition for Screening
To determine an appropriate cutoff score for the LiSN-S high-cue condition on which to base the decision about administering the remainder of the LiSN-S test, the LiSN-S data from 241 children on the NAL research database were analyzed. These children were age 6, 0 to 12, 0, plus one participant with an age of 18, 8. The following relationships are supported by the scatterplots in Fig. A1A, B, and C.
Figure A1.
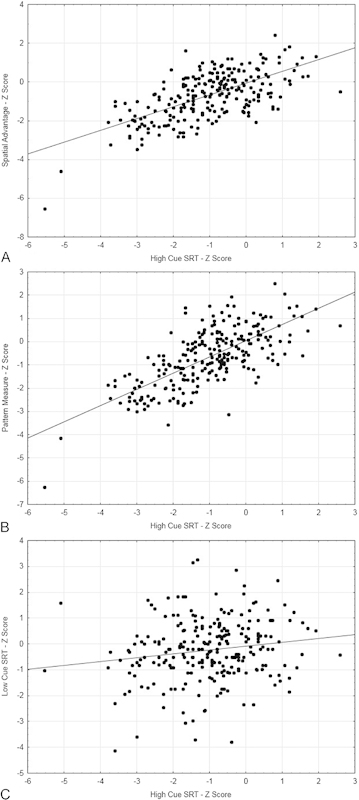
Relationship between scores on the Listening in Spatialized Noise–Sentences Test high-cue test and (A) the spatial advantage, (B) pattern measure, and (C) low-cue measures. Abbreviation: SRT, Speech Reception Threshold.
Spatial advantage z scores poorer than −2 were always associated with high-cue SRT scores poorer than +0.3 and were nearly always associated with high-cue SRT scores poorer than −1.0.
Pattern measure z scores poorer than −2 were always associated with high-cue SRT scores poorer than −0.5 and were nearly always associated with high-cue SRT scores poorer than −1.3.
Low-cue SRT z scores poorer than −2 were always associated with high-cue SRT scores poorer than +0.3 and were nearly always associated with high-cue SRT scores poorer −1.0.
It was therefore determined that children with high-cue scores better than or equal to −1.0 would rarely be outside normal limits on any of the spatial advantage, spatial pattern, or low-cue measures. Consequently, as scores within the normal range on these three measures would be very unlikely to lead to any remediation recommendation, the time taken to administer the remaining three subtests of the LiSN-S could be better spent in other ways, so it was recommended to clinicians that the LiSN-S test be truncated whenever the high-cue score was better than −1.0.
References
- 1.Australian Hearing CAPD service offered by Australian Available at: http://www.hearing.com.au/capd-service-offered-australian-hearing/2013. Accessed September 10, 2015
- 2.Musiek F, Chermak G. Vol. I. San Diego, CA: Plural Publishing; 2014. Preface; pp. xi–xiii. [Google Scholar]
- 3.Cameron S, Dillon H. Vol. II. San Diego, CA: Plural Publishing; 2014. Remediation of spatial processing issues in central auditory processing disorder; pp. 201–224. [Google Scholar]
- 4.Brown D K, Cameron S, Martin J S, Watson C, Dillon H. The North American Listening in Spatialized Noise-Sentences test (NA LiSN-S): normative data and test-retest reliability studies for adolescents and young adults. J Am Acad Audiol. 2010;21(10):629–641. doi: 10.3766/jaaa.21.10.3. [DOI] [PubMed] [Google Scholar]
- 5.Cameron S, Brown D, Keith R, Martin J, Watson C, Dillon H. Development of the North American Listening in Spatialized Noise-Sentences test (NA LiSN-S): sentence equivalence, normative data, and test-retest reliability studies. J Am Acad Audiol. 2009;20(2):128–146. doi: 10.3766/jaaa.20.2.6. [DOI] [PubMed] [Google Scholar]
- 6.Cameron S, Dillon H. Development of the Listening in Spatialized Noise-Sentences Test (LISN-S) Ear Hear. 2007;28(2):196–211. doi: 10.1097/AUD.0b013e318031267f. [DOI] [PubMed] [Google Scholar]
- 7.Cameron S, Dillon H. The listening in spatialized noise-sentences test (LISN-S): test-retest reliability study. Int J Audiol. 2007;46(3):145–153. doi: 10.1080/14992020601164170. [DOI] [PubMed] [Google Scholar]
- 8.Cameron S, Dillon H. The listening in spatialized noise-sentences test (LISN-S): comparison to the prototype LISN and results from children with either a suspected (central) auditory processing disorder or a confirmed language disorder. J Am Acad Audiol. 2008;19(5):377–391. doi: 10.3766/jaaa.19.5.2. [DOI] [PubMed] [Google Scholar]
- 9.Cameron S, Dillon H. Murten, Switzerland: Phonak Communications AG; 2009. Listening in Spatialized Noise–Sentences test (LISN-S) (Version 2.003) [Computer software] [Google Scholar]
- 10.Cameron S, Glyde H, Dillon H. Listening in Spatialized Noise-Sentences Test (LiSN-S): normative and retest reliability data for adolescents and adults up to 60 years of age. J Am Acad Audiol. 2011;22(10):697–709. doi: 10.3766/jaaa.22.10.7. [DOI] [PubMed] [Google Scholar]
- 11.Cameron S, Dillon H, Glyde H, Kanthan S, Kania A. Prevalence and remediation of spatial processing disorder (SPD) in indigenous children in regional Australia. Int J Audiol. 2014;53(5):326–335. doi: 10.3109/14992027.2013.871388. [DOI] [PubMed] [Google Scholar]
- 12.Tomlin D, Rance G. Long-term hearing deficits after childhood middle ear disease. Ear Hear. 2014;35(6):e233–e242. doi: 10.1097/AUD.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 13.Cameron S, Dillon H. Sydney, Australia: National Acoustic Laboratories; 2012. LISN & Learn Auditory Training Software (Version 3.0.0) [Computer software] [Google Scholar]
- 14.Cameron S, Dillon H. Development and evaluation of the LiSN & learn auditory training software for deficit-specific remediation of binaural processing deficits in children: preliminary findings. J Am Acad Audiol. 2011;22(10):678–696. doi: 10.3766/jaaa.22.10.6. [DOI] [PubMed] [Google Scholar]
- 15.Cameron S, Glyde H, Dillon H. Efficacy of the LiSN & Learn auditory training software: randomized blinded controlled study. Audiol Res. 2012;2:e15. doi: 10.4081/audiores.2012.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dillon H, Cameron S, Glyde H, Wilson W, Tomlin D. An opinion on the assessment of people who may have an auditory processing disorder. J Am Acad Audiol. 2012;23(2):97–105. doi: 10.3766/jaaa.23.2.4. [DOI] [PubMed] [Google Scholar]
- 17.Tomlin D, Dillon H, Sharma M, Rance G. The impact of auditory processing and cognitive abilities in children. Ear Hear. 2015;35(6):233–242. doi: 10.1097/AUD.0000000000000172. [DOI] [PubMed] [Google Scholar]
- 18.Keith W J, Purdy S C. Assistive and therapeutic effects of amplification for auditory processing disorder. Semin Hear. 2014;35(1):27–38. [Google Scholar]
- 19.Hornickel J, Zecker S G, Bradlow A R, Kraus N. Assistive listening devices drive neuroplasticity in children with dyslexia. Proc Natl Acad Sci U S A. 2012;109(41):16731–16736. doi: 10.1073/pnas.1206628109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martin N, Brownell R. Novato, CA: Academic Therapy Publications; 2005. Test of Auditory Processing Skills. 3rd ed. [Google Scholar]
- 21.Wilson R H, Strouse A. Mountain Home, TN: VA Medical Centres; 1998. Tonal & speech materials for auditory perceptual assessment (Disc 2.0) [CD] [Google Scholar]
- 22.Singer J, Hurley R M, Preece J P. Effectiveness of central auditory processing tests with children. Am J Audiol. 1998;7(2):73–84. doi: 10.1044/1059-0889(1998/015). [DOI] [PubMed] [Google Scholar]
- 23.Ahmmed A U, Ahmmed A A, Bath J R, Ferguson M A, Plack C J, Moore D R. Assessment of children with suspected auditory processing disorder: a factor analysis study. Ear Hear. 2014;35(3):295–305. doi: 10.1097/01.aud.0000441034.02052.0a. [DOI] [PubMed] [Google Scholar]
- 24.Bryden M P. Order of report in dichotic listening. Can J Psychol. 1962;16(14):291–299. doi: 10.1037/h0083256. [DOI] [PubMed] [Google Scholar]
- 25.Lawfield A, McFarland D J, Cacace A T. Dichotic and dichoptic digit perception in normal adults. J Am Acad Audiol. 2011;22(6):332–341. doi: 10.3766/jaaa.22.6.3. [DOI] [PubMed] [Google Scholar]
- 26.Maerlender A C, Wallis D J, Isquith P K. Psychometric and behavioral measures of central auditory function: the relationship between dichotic listening and digit span tasks. Child Neuropsychol. 2004;10(4):318–327. doi: 10.1080/09297040490909314. [DOI] [PubMed] [Google Scholar]
- 27.Leedale R, Singleton C, Thomas K. East Yorkshire, UK: Lucid Innovations Ltd; 2008. Memory Booster [Computer software] [Google Scholar]
- 28.NAL COSI-C: Client Oriented Scale of Improvement for Children Available at: http://www.nal.gov.au/outcome-measures_tab_cosi.shtml. Accessed September 29, 2015
- 29.Anderson K L, Smaldino J J. Tampa, FL: Educational Audiology Association; 1998. Listening Inventory for Education: An Efficacy Tool—Teacher Appraisal of Listening Difficulty. [Google Scholar]
- 30.Anderson K L, Smaldino J J. Listening inventories for education: a classroom measurement tool. Hear J. 1999;52(10):74–76. [Google Scholar]
- 31.St Clair-Thompson H, Stevens R, Hunt A, Bolder E. Improving children's working memory and classroom performance. Educ Psychol. 2010;30(2):203–219. [Google Scholar]
- 32.Doran G T. There's a S.M.A.R.T. way to write management's goals and objectives. Manage Rev. 1981;70(11):35–36. [Google Scholar]
- 33.Dillon H. Turramurra, Australia: Boomerang Press; 2012. Hearing Aids. [Google Scholar]


