Abstract
Background
Few epidemiologic population-based data are available to describe the wide range of health conditions that affect children with asthma. We conducted this study to identify common comorbidities of asthma during childhood and compare the prevalences of selected comorbidities among children with and without asthma.
Methods
We analyzed weighted data from the 2012 National Health Interview Survey child sample, a sample of 10,954 U.S. children aged 3–17 years. Information about each child's health, including history of asthma and other health conditions, was provided by an adult proxy respondent. We conducted binomial regression to compare the prevalences of 41 selected health conditions among children with and without current asthma.
Results
An estimated 10.4% of children aged 3–17 years (n = 1202) were identified as having current asthma. Nearly all conditions considered were more common among children with than without asthma. Compared to children without asthma, children with asthma had higher prevalences of hay fever or respiratory allergies (prevalence difference [PD]: 30.5%; 95% CI: 26.6, 34.4), eczema or skin allergies (PD: 14.1%; 95% CI: 10.7, 17.5), sinusitis (PD: 11.3%; 95% CI: 8.4, 14.1), food or digestive allergies (PD: 10.4%; 95% CI: 7.7, 13.1), and difficulty with emotions, concentration, behavior, or getting along (PD: 7.9%; 95% CI: 4.7, 11.1).
Conclusions
These results highlight the burden of comorbidities among children with asthma. Improved understanding of the impact of comorbidities among children with asthma may help develop best practices for the assessment, treatment, and control of coexisting health conditions.
Keywords: Adolescent, Asthma, Comorbidity, Epidemiology, Pediatrics, Surveillance
1. Introduction
Children with asthma can be affected by other chronic health conditions [1] and the medical management of multiple chronic conditions, including asthma, poses a unique challenge [2,3]. Among children with asthma, recognizing and treating comorbid conditions may lead to improved asthma outcomes [4]. To date, however, little information is available to inform clinical practice and the research community about the wide range of comorbidities affecting children with asthma and the potential influences they might have on levels of asthma control [2]. Reviews of common comorbidities of asthma have summarized co-occurrence of asthma with allergic rhinitis, anxiety and depressive disorders, atopic dermatitis, chronic sinusitis, diabetes mellitus, gastroesophageal reflux, hormonal disorders, obesity, obstructive sleep apnea, respiratory viral infections, and severe reactions to food allergens [2,5,6]. However, data with which to describe the prevalences of specific comorbidities of asthma among children are sparse.
In an evaluation of asthma comorbidities among low-income children aged 2–17 years in the United States using medical claims data, the most common comorbidity among children with asthma was allergic rhinitis [7]. Another recent investigation of conditions among children with asthma aged 0–17 years in the United States identified elevated prevalences of all conditions considered (cerebral palsy, muscular dystrophy, sickle cell anemia, autism, diabetes, arthritis, congenital heart disease, other heart conditions, and hypertension) as well as elevated associations of asthma attacks and emergency department visits for asthma with increasing numbers of additional comorbid conditions [1]. Despite recent data reporting a nearly 10% prevalence of current asthma among children [8] and the growing body of evidence that comorbid conditions may affect asthma outcomes among children [1], few epidemiologic population-based data are available to describe the overlap of asthma with a wider range of chronic health conditions affecting children. In this study, we evaluated data collected from a representative sample of U.S. children and examined a broad range of self-reported medical conditions to identify common comorbidities of asthma during childhood and to compare the prevalences of selected comorbidities among children with and without asthma.
2. Methods
2.1. National Health Interview Survey
To identify common comorbidities of asthma during childhood, we examined data from the 2012 National Health Interview Survey (NHIS) child dataset. NHIS is a cross-sectional household interview survey conducted annually in the United States using a multistage cluster sample design [9]. For each surveyed family in which a child is present in the household, one sample child is randomly selected and information about the sample child is collected from the sample adult (i.e., the proxy respondent). Additional information about the survey methods is available elsewhere [9,10]. In 2012, the NHIS child sample included information about 13,275 boys and girls aged 0–17 years. Supplemental health outcome questionnaires (e.g., child communication disorders questionnaire and child balance questionnaire) were added to the 2012 NHIS for children aged 3 years and older only [11], therefore, we limited our analysis to children aged 3 years and older.
2.2. Identification of current asthma and selected comorbidities
We categorized each child's current asthma status using his/her proxy respondent's responses to two questionnaire items: (1) has a doctor or other health professional ever told you that [the child] had asthma? and, if yes, (2) does [the child] still have asthma?
Initially, we selected comorbidities based solely on their inclusion in the 2012 NHIS child survey questionnaire. Due to unstable estimates for conditions experienced by few children with or without asthma, we opted not to evaluate the prevalences of several uncommon health conditions (e.g., cystic fibrosis, Down syndrome, muscular dystrophy) included in the survey and present results for the remaining conditions, identified as “selected health conditions”. For each of the selected health conditions considered, we categorized uninformative responses (e.g., refused, don't know) as negative.
2.3. Health consequences of asthma and comorbidities
To evaluate health consequences of asthma and comorbidities, we considered the following five outcomes: (1) an asthma attack or episode in the past 12 months; (2) an emergency department or urgent care center visit due to asthma in the past 12 months; (3) taking prescription medication for ≥3 months in the past 12 months; (4) a medical specialist encounter in the past 12 months; and (5) a general practitioner encounter in the past 12 months. Questionnaire items about prescription medication, medical specialist encounters, and general practitioner encounters did not specifically refer to asthma, and are interpreted here as medication use or encounters, respectively, for any condition.
2.4. Statistical analysis
Because the NHIS is conducted using a multistage probability design [12], data collected about the children (hereafter referred to as the “sample”) are representative of a larger population of children in the United States. Weights provided with the data were applied during analysis so that the results generated are representative of a weighted estimate of the U.S. population of children aged 3–17 years (hereafter referred to as the “weighted population estimate”).
First, we conducted descriptive analyses to summarize the demographic characteristics of the sample of children and the weighted population estimate. We then evaluated the prevalences of selected health conditions among children with and without current asthma. Prevalences are presented as percentages, with 95% confidence intervals (CIs), of the weighted population estimates of children with and without current asthma separately.
To evaluate associations between prevalences of selected health conditions among children with and without current asthma, we used binomial regression models specified with an identity link. Standard errors (SEs) were generated by adapting a two-stage approach developed by Natarajan et al. [13] to generate robust variance estimates fitting the binomial error distribution of our data. Briefly described, in stage 1 we obtained regression parameter estimates using weighted linear regression models; specifically, we used SAS proc genmod (SAS Institute Inc., Cary, North Carolina, USA). We then used the predicted means and linear predictors generated by the weighted linear regression models to convert the covariates and outcomes to “pseudo-covariates” and “pseudo-outcomes” [13] for each observation, which were then used in stage 2 to estimate valid standard errors using SAS proc surveyreg. Methodologic details, including code for programming in SAS, have been published by Natarajan et al. (2008) [13]. We adjusted our models for age category (3–4, 5–9, 10–14, 15–17 years), Hispanic ethnicity, parental educational attainment (high school degree/equivalency or less, some college/associate's degree, bachelor's degree or higher), race (white only, black/African-American only, other race only, multiple races), and sex. Parental educational attainment, included as an indicator of socio-economic status, was assigned as the higher of the mother's and father's educational attainment. Adjusted associations are presented as prevalence differences (PDs), which are interpreted as the differences between the prevalences of each selected health condition among children with current asthma and children without current asthma.
For each child, we computed the total number of positive responses out of the 41 health conditions, excluding asthma, in our analysis. We then categorized this total as 0, 1, 2, 3, 4 and 5 or more health conditions and used this categorization to evaluate health consequences of asthma and increasing numbers of comorbidities. Among children with current asthma, we estimated the percentages of children for whom the following two outcomes were reported: (1) an asthma attack or episode in the past 12 months; (2) an emergency department or urgent care center visit due to asthma in the past 12 months. We estimated percentages of both outcomes across categories of the total number of other health conditions (i.e., 0, 1, 2, 3, 4, and 5 or more). We then generated PDs, with 95% CIs, to contrast the prevalences of each outcome among children with one or more of the selected comorbidities to the prevalences of each outcome among children with none of the selected comorbidities. For the remaining three health consequences (taking prescription medication for ≥3 months in the past 12 months, a medical specialist encounter in the past 12 months, and a general practitioner encounter in the past 12 months), we contrasted the prevalences of each outcome among children with asthma to those among children without asthma across categories of selected comorbidities. Comparisons of these three outcomes are also presented as PDs, with 95% CIs.
Following our main analysis, for each health condition with a prevalence of 10% or higher among children with current asthma, we evaluated associations with current asthma across categories of age, race, and sex. We also conducted a sensitivity analysis to evaluate the impact of including in our analysis children younger than five years of age, a population in which asthma may be difficult to diagnose. In this analysis, we evaluated associations between current asthma and each of the selected comorbidities in the sample of children aged 5–17 years.
All analyses were conducted using SAS version 9.3 (SAS Institute Inc., Cary, North Carolina, USA). Results based on fewer than 50 unweighted respondents (i.e., percentages based upon a denominator <50) or for which the relative SE, computed as the SE of the percentage divided by the percentage, is >30% are not reported or interpreted. The analyses presented here were exempted from institutional review board review by the Centers for Disease Control and Prevention.
3. Results
The 2012 NHIS child sample included information about 13,275 boys and girls aged 0–17 years. After excluding children aged 0–2 years (n = 2321; 16%), we analyzed a final study population of 10,954 children, estimated to represent over 61.6 million children aged 3–17 years in the United States. Of the 10,954 children in our final sample, 9133 (84.1%) were categorized as never having had asthma and 619 (5.5%) were categorized as ever, but not still, having asthma; 1202 (10.4%) were categorized as still having asthma, rendering our final categorization of current asthma as no (n = 9752; 89.6%) versus yes (n = 1202; 10.4%) (Table 1). The estimated prevalence of current asthma increased across categories of age from 7.9% among children aged 3–4 years to 11.3% among children 14–17 years of age. The average ages of children with and without current asthma were similar (10.3 and 10.0 years, respectively). Overall, 67.3% of children were identified as having one or more of the 41 selected other health conditions, with the percentages also increasing across categories of age from 52.5% among children aged 3–4 years to 73.9% among children 14–17 years of age. The average age of children with one or more of the selected health conditions was one year older than that of children without any of the conditions (10.4 and 9.4 years, respectively). Among children with current asthma, 87.8% (95% CI: 85.7, 90.0) had one or more of the selected health conditions, compared to 65.0% (95% CI: 63.6, 66.4) among children without current asthma. The distribution of the total number of selected health conditions per child ranged from 0 to 28 (mean: 4.1; 95% CI: 3.8, 4.4) among children with asthma and 0 to 21 (mean: 2.0; 95% CI: 1.9, 2.0) among children without asthma.
Table 1.
Characteristics of the study sample and percentages of the weighted population estimate with current asthma and with any selected health conditions excluding asthma.
| Sample children |
Weighted population estimate |
With current asthma |
With any selected health conditionb |
||
|---|---|---|---|---|---|
| No. | No.a | Percent (95% CI) | Percent (95% CI) | Percent (95% CI) | |
| Total | 10,954 | 61,696 | 100. | 10.4 (9.6, 11.1) | 67.3 (66.0, 68.6) |
| Age, in years | |||||
| 3–4 | 1473 | 8040 | 13.0 (12.2, 13.9) | 7.9 (6.1, 9.7) | 52.5 (49.2, 55.8) |
| 5–9 | 3441 | 20,512 | 33.2 (32.1, 34.4) | 10.6 (9.2, 11.9) | 66.9 (64.8, 69.0) |
| 10–14 | 3562 | 20,695 | 33.5 (32.4, 34.7) | 10.5 (9.3, 11.7) | 69.6 (67.6, 71.5) |
| 14–17 | 2478 | 12,448 | 20.2 (19.2, 21.1) | 11.3 (9.7, 12.9) | 73.9 (71.7, 76.1) |
| Asthma history | |||||
| Current | 1202 | 6389 | 10.4 (9.6, 11.1) | 100.0 | 87.8 (85.7, 90.0) |
| Former | 619 | 3391 | 5.5 (5.0, 6.0) | 0.0 | 80.4 (76.5, 84.2) |
| Never | 9133 | 51,915 | 84.1 (83.3, 85.0) | 0.0 | 64.0 (62.5, 65.4) |
| Hispanic ethnicity | |||||
| No | 7780 | 47,093 | 76.3 (75.1, 77.5) | 10.5 (9.7, 11.3) | 69.6 (68.1, 71.2) |
| Yes | 3174 | 14,602 | 23.7 (22.5, 24.9) | 10.0 (8.5, 11.5) | 59.9 (57.7, 62.1) |
| No. selected health conditionsb | |||||
| 0 | 3531 | 20,157 | 32.7 (31.4, 34.0) | 3.9 (3.1, 4.6) | 0.0 |
| 1 | 2437 | 13,524 | 21.9 (20.9, 22.9) | 8.0 (6.7, 9.4) | 100.0 |
| 2 | 1595 | 8779 | 14.2 (13.4, 15.0) | 9.5 (7.6, 11.5) | 100.0 |
| 3 | 1021 | 5824 | 9.4 (8.8, 10.1) | 13.7 (11.2, 16.2) | 100.0 |
| 4 | 684 | 3762 | 6.1 (5.5, 6.7) | 18.4 (14.4, 22.4) | 100.0 |
| 5+ | 1686 | 9649 | 15.6 (14.8, 16.5) | 22.8 (20.3, 25.3) | 100.0 |
| Parental education | |||||
| High school degree or less | 4182 | 21,267 | 34.5 (33.0, 35.9) | 11.8 (10.5, 13.0) | 63.7 (61.6, 65.7) |
| Some college | 3397 | 19,159 | 31.1 (29.8, 32.3) | 11.6 (10.3, 13.0) | 70.7 (68.7, 72.8) |
| Bachelor's degree or higher | 3375 | 21,269 | 34.5 (33.0, 36.0) | 7.8 (6.7, 8.9) | 67.9 (65.6, 70.2) |
| Race | |||||
| Black/African-American only | 1796 | 8761 | 14.2 (13.3, 15.1) | 17.7 (15.6, 19.8) | 67.8 (66.3, 69.2) |
| White only | 7689 | 46,032 | 74.6 (73.4, 75.8) | 9.0 (8.1, 9.8) | 66.7 (63.5, 69.8) |
| Otherc only | 861 | 3857 | 6.3 (5.6, 6.9) | 8.5 (5.4, 11.6) | 72.7 (67.8, 77.5) |
| Multiple race | 608 | 3046 | 4.9 (4.4, 5.5) | 12.6 (9.2, 16.0) | 59.6 (55.4, 63.8) |
| Sex | |||||
| Female | 5382 | 30,182 | 48.9 (47.8, 50.1) | 9.7 (8.7, 10.7) | 65.4 (63.6, 67.2) |
| Male | 5572 | 31,513 | 51.1 (49.9, 52.2) | 11.0 (10.0, 11.9) | 69.2 (67.7, 70.7) |
In thousands.
Excluding asthma.
Includes American Indian, Alaska Native, Asian, and other race groups not identified.
Percentages of the weighted population estimates of children with each of the selected health conditions are presented in Table 2. While all conditions were more common among children with than without current asthma, the most notable adjusted differences occurred in the prevalences of hay fever or respiratory allergies (PD: 30.5%; 95% CI: 26.6, 34.4), eczema or skin allergies (PD: 14.1%; 95% CI: 10.7, 17.5), sinusitis (PD: 11.3%; 95% CI: 8.4, 14.1), food or digestive allergies (PD: 10.4%; 95% CI: 7.7, 13.1), difficulty with emotions, concentration, behavior, or getting along (PD: 7.9%; 95% CI: 4.7, 11.1), and fatigue or lack of energy ≥3 days (PD: 7.8%; 95% CI: 5.2, 10.3). Indeed, for all conditions shown in Table 3, adjusted differences in the prevalences of the weighted population estimates of children with and without asthma were statistically significant at α = 0.05, with the exception of differences in prevalences with autism.
Table 2.
Percentages of the weighted population estimate of children with selected health conditions by asthma history.
| Current asthma |
PD (95% Cl)a | ||||
|---|---|---|---|---|---|
| Yes |
No |
||||
| Sample children |
Weighted population estimate |
Sample children |
Weighted population estimate |
||
| No. | Percent (95% CI) | No. | Percent (95% CI) | ||
| Allergies | |||||
| Eczema/skin allergyb | 303 | 24.8 (21.4, 28.3) | 989 | 10.1 (9.3, 10.9) | 14.1 (10.7, 17.5) |
| Food/digestive allergyb | 166 | 15.0 (12.2, 17.7) | 416 | 4.4 (3.9, 5.0) | 10.4 (7.7, 13.1) |
| Hay fever/respiratory allergyb | 521 | 45.2 (41.4, 49.1) | 1481 | 15.2 (14.2, 16.2) | 30.5 (26.6, 34.4) |
| Cardiovascular or metabolic | |||||
| Congenital heart disease or other heart condition | 27 | 2.4 (1.2, 3.6) | 102 | 1.1 (0.8, 1.4) | 1.4 (0.3, 2.4) |
| High cholesterolb | 18 | 1.4 (0.6, 2.2) | 78 | 0.7 (0.5, 0.9) | 0.7 (0.005, 1.3) |
| Hypertensionb | 23 | 2.1 (1.0, 3.1) | 60 | 0.7 (0.4, 0.9) | 1.1 (0.3, 2.0) |
| Overweightb | 129 | 9.9 (7.9, 12.0) | 544 | 4.9 (4.4, 5.4) | 4.0 (2.2, 5.9) |
| Gastrointestinal | |||||
| Abdominal painb | 142 | 10.4 (8.5, 12.4) | 586 | 5.9 (5.3, 6.4) | 3.9 (2.0, 5.8) |
| Constipation requiring medicationb | 87 | 6.5 (4.7, 8.3) | 244 | 2.7 (2.3, 3.1) | 3.9 (2.0, 5.7) |
| Diarrhea/colitisb | 28 | 1.8 (0.9, 2.7) | 116 | 1.2 (0.9, 1.5) | 0.9 (0.02, 1.8) |
| Hearing | |||||
| Trouble hearing or deaf without a hearing aid | 66 | 6.8 (4.5, 9.1) | 188 | 2.0 (1.6, 2.3) | 4.6 (2.4, 6.9) |
| Infectious | |||||
| Ear infections, ≥3 in the past 3 months | 106 | 9.2 (6.8, 11.6) | 381 | 3.8 (3.4, 4.3) | 5.0 (2.8, 7.2) |
| Influenza or pneumoniab | 129 | 10.6 (8.4, 12.9) | 457 | 4.6 (4.1, 5.2) | 6.0 (3.9, 8.2) |
| Sinusitisb | 197 | 18.0 (15.0, 20.9) | 573 | 6.1 (5.5, 6.8) | 11.3 (8.4, 14.1) |
| Strep or tonsillitisb | 208 | 18.4 (15.0, 21.9) | 1,110 | 12.3 (11.3, 13.2) | 6.3 (2.6, 10.1) |
| Sore throat other than strep or tonsillitisb | 297 | 25.2 (21.7, 28.7) | 1,779 | 18.6 (17.6, 19.6) | 7.2 (3.6, 10.7) |
| Mood-related | |||||
| Depressionb | 77 | 6.6 (4.7, 8.5) | 261 | 2.5 (2.1, 2.8) | 3.4 (1.8, 5.1) |
| Difficulty with emotions, concentration, behavior, or getting alongc | 321 | 26.9 (23.6, 30.2) | 1,608 | 16.9 (15.9, 17.9) | 7.9 (4.7, 11.1)d |
| Frequently anxious, nervous, or worriedb | 167 | 13.5 (10.9, 16.2) | 713 | 7.1 (6.4, 7.7) | 5.3 (2.8, 7.7) |
| Musculoskeletal | |||||
| Lower back painb | 97 | 7.8 (6.0, 9.7) | 361 | 3.3 (2.8, 3.7) | 3.8 (2.3, 5.3) |
| Neck painb | 70 | 6.7 (4.8, 8.6) | 228 | 2.1 (1.8, 2.5) | 4.3 (2.5, 6.1) |
| Severe sprains or strainsb | 82 | 7.5 (5.4, 9.5) | 351 | 3.5 (3.1, 4.0) | 3.4 (1.8, 4.9) |
| Other chronic painb | 21 | 1.5 (0.6, 2.3) | 66 | 0.7 (0.5, 0.9) | 0.7 (0.04, 1.4) |
| Neurological or cognitive | |||||
| Attention deficit hyperactivity disorder | 185 | 14.8 (12.4, 17.2) | 828 | 8.9 (8.2, 9.6) | 4.5 (2.2, 6.7)d |
| Autism | 28 | 1.8 (0.9, 2.6) | 123 | 1.3 (1.0, 1.5) | 0.6 (−0.01, 1.2) |
| Diagnosed dizziness or balance problems | 43 | 3.9 (2.7, 5.2) | 149 | 1.6 (1.2, 1.9) | 2.3 (1.3, 3.4) |
| Frequent fallsb | 45 | 3.6 (2.2, 4.9) | 108 | 1.1 (0.8, 1.3) | 2.8 (1.5, 4.1) |
| Frequent headaches or migrainesb | 145 | 12.2 (9.8, 14.6) | 556 | 5.2 (4.7, 5.8) | 5.6 (3.4, 7.8) |
| Intellectual disability known as mental retardation | 26 | 2.2 (1.2, 3.2) | 105 | 1.1 (0.8, 1.3) | 1.0 (0.2, 1.8) |
| Learning disability | 164 | 12.9 (10.6, 15.3) | 712 | 7.4 (6.8, 8.1) | 4.4 (2.1, 6.6) |
| Other developmental delay | 101 | 8.4 (6.4, 10.4) | 422 | 4.5 (4.0, 5.0) | 3.7 (1.7, 5.7) |
| Vertigob | 36 | 2.7 (1.5, 3.9) | 135 | 1.4 (1.1, 1.7) | 1.4 (0.4, 2.5) |
| Sleep and fatigue | |||||
| Excessive sleepiness during the dayb | 154 | 7.4 (5.6, 9.3) | 521 | 3.3 (2.9, 3.8) | 3.6 (1.8, 5.4) |
| Fatigue or lack of energy ≥3 daysb | 90 | 13.6 (11.0, 16.2) | 342 | 5.4 (4.8, 6.0) | 7.8 (5.2, 10.3) |
| Insomnia or trouble sleepingb | 132 | 12.0 (9.6, 14.4) | 453 | 4.6 (4.0, 5.1) | 6.6 (4.4, 8.9) |
| Vision | |||||
| Trouble seeing | 65 | 5.9 (4.1, 7.6) | 305 | 2.8 (2.4, 3.2) | 2.9 (1.1, 4.7) |
| Voice, swallowing, speech, and language | |||||
| Diagnosed voice, swallowing, speech, or language problem | 108 | 9.3 (7.2, 11.4) | 442 | 5.1 (4.5, 5.6) | 4.3 (2.2, 6.3) |
| Stuttered/stammeredb | 52 | 4.0 (2.6, 5.4) | 172 | 1.7 (1.4, 2.0) | 1.8 (0.7, 3.0) |
| Miscellaneous | |||||
| Anemia | 29 | 2.1 (1.2, 2.9) | 109 | 1.0 (0.8, 1.2) | 1.3 (0.5, 2.1) |
| Dental painb | 120 | 9.9 (7.8, 12.1) | 622 | 6.3 (5.7, 6.9) | 3.0 (1.1, 4.9) |
| Surgery or surgical procedureb | 82 | 6.8 (4.8, 8.7) | 356 | 3.6 (3.1, 4.1) | 3.3 (1.5, 5.0) |
Adjusted for age, Hispanic ethnicity, parental educational attainment, race, and sex.
In the past 12 months.
Minor or definite/severe difficulty.
Not adjusted for parental educational attainment due to model non-convergence.
Table 3.
Percentages of the weighted population estimate of children with current asthma with a reported asthma attack in the past 12 months or emergency department or urgent care center visit due to asthma in the past 12 months and associations with the number of comorbid conditions.
| No. comorbidities | Percent(SE) | PD (95% CI)a | |
|---|---|---|---|
| Asthma attackb | 0 | 40.3 (4.3) | 0.0 (referent) |
| 1 | 46.1 (4.8) | 4.7 (−7.3, 16.7) | |
| 2 | 50.0 (4.8) | 8.0 (−3.7, 19.6) | |
| 3 | 58.3 (5.4) | 12.1 (−2.0, 26.1) | |
| 4 | 47.9 (5.2) | 5.2 (−8.2, 18.6) | |
| 5+ | 68.2 (2.8) | 29.2 (19.1, 39.2) | |
| Emergency department or urgent care center visit due to asthmab | 0 | 11.5 (2.6) | 0.0 (referent) |
| 1 | 16.9 (3.6) | 5.3 (−1.4, 12.1) | |
| 2 | 17.2 (3.8) | 5.6 (0.2, 11.0) | |
| 3 | 20.5 (4.1) | 6.4 (−1.2, 14.1) | |
| 4 | 17.3 (4.0) | 6.6 (0.4, 12.8) | |
| 5+ | 26.1 (2.5) | 15.8 (9.9, 21.6) |
Adjusted for age, Hispanic ethnicity, parental educational attainment, race, and sex.
In the past 12 months.
Among children with asthma, percentages with a reported asthma attack in the past 12 months increased from 40.3% (95% CI: 31.8, 48.7) among children with no comorbidities to 68.2% (95% CI: 62.5, 74.0) among children with five or more comorbidities (adjusted PD: 29.2%; 95% CI: 19.1, 39.2) (Table 3). Similarly, among children with asthma, percentages with a reported emergency department or urgent care center visit due to asthma in the past 12 months increased from 11.5% (95% CI: 6.4, 16.5) among children with no comorbidities to 26.1% (95% CI: 6.4, 16.5) among children with five or more reported comorbidities (adjusted PD: 15.8%; 95% CI: 9.9, 21.6).
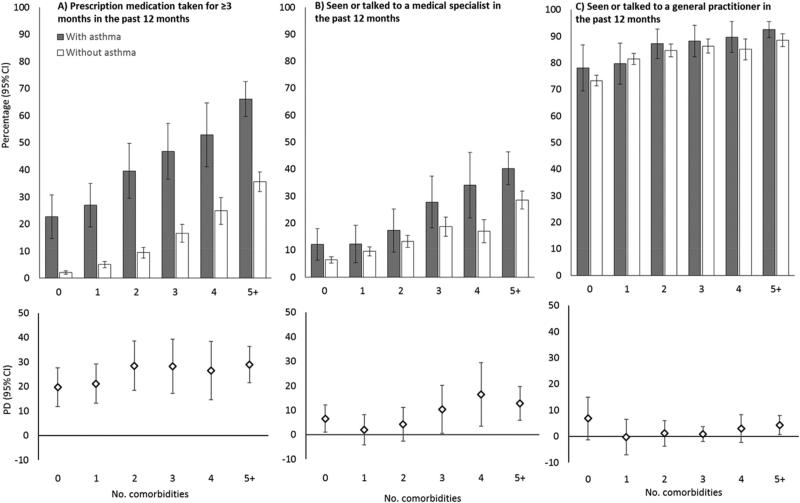
Percentages of weighted population estimates of children with several functional consequences of asthma across categories of the number of comorbidities reported and by current asthma status are shown in Fig. 1. Across categories of comorbidities, percentages of children taking prescription medication for ≥3 months in the past 12 months and percentages of children who had an encounter with a medical specialist in the past 12 months (panels A and B, respectively) were consistently higher among children with current asthma than among those without current asthma. In contrast, no differences were observed in the percentages of children with than without current asthma who had seen or talked to a general practitioner in the past 12 months (panel C). As indicated by the PDs shown in the bottom panels of Fig. 1, there was little variation in the prevalences of each of the three outcomes with increasing numbers of comorbidities.
Fig. 1.
Percentages of the weighted population estimate of children taking prescription medication for ≥3 months in the past 12 months (panel A, top), with a medical specialist encounter in the past 12 months (panel B, top), and with a general practitioner encounter within the past 12 months (panel C, top) among children with and without current asthma and associations between asthma and each outcome across categories of the number of comorbidities (panels A–C, bottom). Associations are adjusted for age, Hispanic ethnicity, parental educational attainment, race, and sex.
Overall, 15 conditions with prevalences >10% in the weighted population estimate of children with current asthma were identified. Analyses conducted across strata of age category, race, and sex did not reveal notable difference in the measures of association across these demographic categories (not shown). Results of our sensitivity analysis, in which we limited our analysis to children aged 5–17, were largely similar to our main results (not shown). In these analyses, the prevalences of current asthma and reporting any of the selected health conditions were 10.7% (SE: 0.4) and 69.6% (SE: 0.7), respectively, compared to 10.4% (SE: 0.4) and 67.3% (SE: 0.7), in our main analysis. Adjusted differences in the prevalences of hay fever or respiratory allergies (PD: 30.1%; 95% CI: 26.2, 34.0), eczema or skin allergies (PD: 13.6%; 95% CI: 10.1, 17.1), sinusitis (PD: 12.3%; 95% CI: 9.2, 15.4), food or digestive allergies (PD: 10.9%; 95% CI: 8.0, 13.9), difficulty with emotions, concentration, behavior, or getting along (PD: 9.8%; 95% CI: 6.2, 13.3), and fatigue or lack of energy ≥3 days (PD: 8.3%; 95% CI: 5.5, 11.0) were similar in magnitude and precision to those generated in our main analysis.
4. Discussion
We conducted this study to describe the prevalence of selected chronic health conditions among children in the United States and found higher prevalences of conditions among children with asthma than among children without asthma. Among all children, percentages of children taking prescription medication for any reason and with a reported visit to a medical specialist for any reason were consistently higher among children with than without asthma. Among children with asthma, we found increasing prevalences of asthma attacks and emergency department visits with increasing numbers of comorbid conditions.
Our findings support and extend our understanding about the burden of multiple chronic health conditions, including allergic conditions [7] and anxiety and depressive disorders [14], on children with asthma. Most notably, our analysis took advantage of the wide range of comorbidities included in the 2012 NHIS survey to present prevalences of comorbidities experienced in the past 12 months. Our work complements that of Patel et al., who examined NHIS data from 2007 to 2012 to evaluate the prevalences of nine chronic conditions in children with and without asthma [1]. The conditions reported by Patel et al. were all were relatively rare and were all more common among children with asthma than children without asthma [1]. Though limited to a single year of the NHIS, our analysis included a comprehensive list of comorbidities in order to investigate the extent to which children with asthma may be affected by other, more common, conditions.
Children with multiple comorbid conditions of asthma may be taking medications for these conditions, increasing the potential for interactions between medications or confusion about the roles of medications. Children with multiple chronic illnesses may also be more likely to receive care from multiple providers, potentially making their asthma management fragmented and less effective. The finding of increased prevalences of health conditions less likely to have common, proximal etiologic origins suggests that relationships between asthma and these common comorbidities should be considered carefully. One possible explanation for the overlap includes that children with asthma may be more susceptible to, or more likely to be diagnosed with other chronic conditions, such as recurrent respiratory viral infections. Another possibility is that asthma or its treatment may directly cause or contribute to other chronic conditions. For example, prolonged systemic glucocorticoid use may affect blood pressure, glucose metabolism, sleep, and other health outcomes, while the use of beta agonists may induce increased heart rate and tremor [15–17]. Children with chronic conditions may be more susceptible to asthma due to shared mechanistic pathways, such as chronic inflammation [18,19]. If children with at least one medical condition are more likely to seek medical care, they may have more opportunities to have other chronic medical conditions diagnosed. And some children may be simultaneously susceptible to asthma and other health conditions for reasons not yet fully understood. Excluding a bias in the reporting of multiple chronic conditions, improvements in our understanding of the temporal and causal relationships between asthma and other chronic health conditions may inform strategies for the management of asthma.
The NHIS is a questionnaire-based survey and does not include validation of responses or measures of the severity or control of asthma or any of the other selected health conditions included in our analysis. This limitation is counterbalanced by the large number of children in the survey and the wide geographic distribution of the sample. Our results are robust to the exclusion of children younger than five years of age, suggesting that challenges in diagnosing asthma among children under the age of five do not noticeably influence our estimates. While many of the conditions identified in this analysis as co-occurring with asthma in children likely share atopic etiologies (e.g., eczema, hay fever) with asthma, we cannot definitively identify these conditions as atopic without confirmation by allergy testing. Our findings of positive associations of the number of comorbidities with asthma attacks and emergency department or urgent care visits suggest that multiple comorbid conditions may be a risk factor for loss of asthma control. Our investigation was unable to determine whether these relationships might be attributable to intrinsic characteristics of children or modifiable factors such as limited time in a clinical visit to assess asthma control.
5. Conclusions
Our findings extend previous evidence that additional chronic health conditions are more common among children with than without asthma by presenting estimates of the burden of a wide range of health conditions, prevalences of asthma attacks and asthma-related emergency department visits, and metrics of health care utilization. Overall, these results highlight the importance of considering medical comorbidities when treating children with asthma and they may be useful for improved understanding of the simultaneous management of asthma and other health conditions among children aged 3–17 years. Improving our understanding of the burden of comorbidities among children with asthma may help develop best practices for the assessment, treatment, and control of childhood asthma.
Abbreviations
- CI
confidence interval
- NHIS
National Health Interview Survey
- PD
prevalence difference
- SE
standard error
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Patel MR, Leo HL, Baptist AP, Cao Y, Brown RW. Asthma outcomes in children and adolescents with multiple morbidities: findings from the national health interview survey. J. Allergy Clin. Immunol. 2015;135(6):1444–1449. doi: 10.1016/j.jaci.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 2.de Groot EP, Duiverman EJ, Brand PL. Comorbidities of asthma during childhood: possibly important, yet poorly studied. Eur. Respir. J. 2010;36(3):671–678. doi: 10.1183/09031936.00185709. [DOI] [PubMed] [Google Scholar]
- 3.Parekh AK, Goodman RA, Gordon C, Koh HK, H. H. S. Interagency Work-group on Multiple Chronic Conditions Managing multiple chronic conditions: a strategic framework for improving health outcomes and quality of life. Public Health Rep. 2011;126(4):460–471. doi: 10.1177/003335491112600403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gershon AS, Wang C, Guan J, To T. Burden of comorbidity in individuals with asthma. Thorax. 2010;65(7):612–618. doi: 10.1136/thx.2009.131078. [DOI] [PubMed] [Google Scholar]
- 5.Cazzola M, Segreti A, Calzetta L, Rogliani P. Comorbidities of asthma: current knowledge and future research needs. Curr. Opin. Pulm. Med. 2013;19(1):36–41. doi: 10.1097/MCP.0b013e32835b113a. [DOI] [PubMed] [Google Scholar]
- 6.Boulet LP. Influence of comorbid conditions on asthma. Eur. Respir. J. 2009;33(4):897–906. doi: 10.1183/09031936.00121308. [DOI] [PubMed] [Google Scholar]
- 7.Clark NM, Lachance L, Benedict MB, Little R, Leo H, Awad DF, et al. The extent and patterns of multiple chronic conditions in low-income children. Clin. Pediatr. (Phila) 2015;54(4):353–358. doi: 10.1177/0009922815574073. [DOI] [PubMed] [Google Scholar]
- 8.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, and mortality in the United States. NCHS Data Brief. 2012;(94):1–8. 2001-2010. [PubMed] [Google Scholar]
- 9.Bloom B, Jones LI, Freeman G. Summary health statistics for U.S. Children: national health interview survey, National Center for Health Statistics. Vital Health Stat. 2012;10(258) 2013. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention [04.06.15];National Center for Health Statistics, About the National Health Interview Survey. 2012 http://www.cdc.gov/nchs/nhis/about_nhis.htm. Updated June 13, 2012.
- 11.Centers for Disease Control and Prevention (CDC) [08.08.15];National Health Interview Survey (NHIS) Public Use Data Release: NHIS Survey Description. 2012 ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2012/srvydesc.pdf. Published 2013.
- 12.Parsons V, Moriarity C, Jonas K, Moore T, Davis K, Tomkins L. Design and estimation for the national health interview survey, 2006-2015. National Center for Health Statistics. Vital Health Stat. 2014;2(165) [PubMed] [Google Scholar]
- 13.Natarajan S, Lipsitz SR, Fitzmaurice G, Moore CG, Gonin R. Variance estimation in complex survey sampling for generalized linear models. J. Roy. Stat. Soc. C-App. 2008;57(1):75–87. [Google Scholar]
- 14.Katon W, Lozano P, Russo J, McCauley E, Richardson L, Bush T. The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared with controls. J. Adolesc. Health. 2007;41(5):455–463. doi: 10.1016/j.jadohealth.2007.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cazzola M, Page CP, Rogliani P, Matera MG. beta2-agonist therapy in lung disease. Am. J. Respir. Crit. Care Med. 2013;187(7):690–696. doi: 10.1164/rccm.201209-1739PP. [DOI] [PubMed] [Google Scholar]
- 16.Schacke H, Docke WD, Asadullah K. Mechanisms involved in the side effects of glucocorticoids. Pharmacol. Ther. 2002;96(1):23–43. doi: 10.1016/s0163-7258(02)00297-8. [DOI] [PubMed] [Google Scholar]
- 17.Adkinson NF, Middleton E. Middleton's Allergy : Principles and Practice. eighth ed. Elsevier/Saunders; Philadelphia, PA: 2014. [Google Scholar]
- 18.Scrivo R, Vasile M, Bartosiewicz I, Valesini G. Inflammation as “common soil” of the multifactorial diseases. Autoimmun. Rev. 2011;10(7):369–374. doi: 10.1016/j.autrev.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Prescott SL. Early-life environmental determinants of allergic diseases and the wider pandemic of inflammatory noncommunicable diseases. J. Allergy Clin. Immunol. 2013;131(1):23–30. doi: 10.1016/j.jaci.2012.11.019. [DOI] [PubMed] [Google Scholar]