Abstract
Here, we report the first successful endoscopic resection of an exophytic gastrointestinal stromal tumor (GIST) using a novel perforation-free suction excavation technique. A 49-year-old woman presented for further management of a gastric subepithelial tumor on the lesser curvature of the lower body, originally detected via routine upper gastrointestinal endoscopy. Abdominal computed tomography and endoscopic ultrasound showed a 4-cm extraluminally protruding mass originating from the muscularis propria layer. The patient firmly refused surgical resection owing to potential cardiac problems, and informed consent was obtained for endoscopic removal. Careful dissection and suction of the tumor was repeated until successful extraction was achieved without serosal injury. We named this procedure the suction excavation technique. The tumor’s dimensions were 3.5 cm × 2.8 cm × 2.5 cm. The tumor was positive for C-KIT and CD34 by immunohistochemical staining. The mitotic count was 6/50 high-power fields. The patient was followed for 5 years without tumor recurrence. This case demonstrated the use of endoscopic resection of an exophytic GIST using the suction excavation technique as a potential therapy without surgical resection.
Keywords: Gastrointestinal stromal tumor, Endoscopic resection, Submucosal tumor, Subepithelial tumor, En bloc resection
Core tip: Most small gastrointestinal stromal tumor (GISTs) are treated surgically, and endoscopic resection is contraindicated as the risk of perforation and incomplete resection is high. However, several authors recently reported successful results with endoscopic resection of a subepithelial tumor originating from the muscularis propria layer, including GISTs. A GIST with exophytic growth was previously considered a contraindication for endoscopic resection. In cases of exophytic GISTs, surgical or endoscopic full-thickness resection with laparoscopic support is generally indicated. However, this case shows that even exophytic GISTs can potentially be endoscopically resected without perforation using the suction excavation method.
INTRODUCTION
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumor of the gastrointestinal tract, especially of the stomach. Most small GISTs are treated surgically, and endoscopic resection was previously contraindicated as the risk of perforation and incomplete resection is high. Recently, however, several authors have reported successful results using endoscopic resection for subepithelial tumors (SETs) originating from the muscularis propria layer, including GISTs[1-3]. However, GISTs with exophytic growth have been considered a contraindication for endoscopic resection. Few studies on endoscopic resection of an extragastric bulging SET have been published, and the procedure reported previously was full-thickness resection of the gastric wall with laparoscopic support. In cases of exophytic GISTs, surgical or endoscopic full-thickness resection with laparoscopic support is usually indicated. However, the case presented here shows that even exophytic GISTs can potentially be endoscopically resected without perforation. We report the first successful endoscopic resection of a GIST with exophytic growth using a suction excavation technique.
CASE REPORT
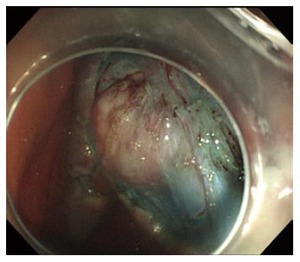
A 49-year-old woman visited our hospital for further evaluation and management of a gastric SET, detected via routine upper gastrointestinal endoscopy at a private health clinic. The esophagogastroduodenoscopy performed outside the hospital showed a 4-cm mass with a smooth tapered margin located in the lower body, on the side of lesser curvature (Figure 1). The mass was hard and immovable upon palpation with biopsy forceps. Endoscopic ultrasound showed a heterogeneous hypoechoic mass with extraluminal growth, originating from the muscularis propria layer (Figure 2). An abdominal CT scan showed a 4-cm extraluminally protruding mass compressing the gastric wall (Figure 3). Our initial treatment plan was surgical resection owing to the tumor’s extraluminal growth pattern. However, the patient resolutely refused surgical resection and we therefore chose to attempt an endoscopic removal of the tumor. The endoscopic submucosal dissection procedure was performed using a cap-fitted gastroscope (GIF-Q260; Olympus, Tokyo, Japan). The endoscopic procedure is clearly illustrated and presented in Figure 4. Marking was done along the tumor’s margin using an argon plasma coagulation probe. After submucosal injection of sodium hyaluronate, a circumferential incision was made along the marking line using a hook knife (KD-620Q; Olympus). After the circumferential incision, the overlying mucosa was removed by snare resection and dissection of the muscular tissue between the tumor and the serosa (Figure 5). Muscular dissection was carefully performed using a hook knife. Shortly after muscular dissection, suction was applied to the tumor using the end of the cap-fitted gastroscope. This careful dissection and suction of the tumor was repeated until, finally, the tumor was successfully extracted without serosal injury (Figure 6). The procedure time was approximately 1 h. Propofol was initially injected intravenously to induce sedation (0.5 mg/kg), and additional propofol was administered repeatedly during the endoscopic procedure (10-20 mg per each injection). Supplemental oxygen was administered nasally throughout sedation.
Figure 1.
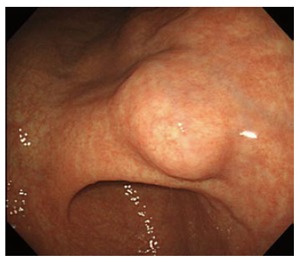
Endoscopic view of the lesion.
Figure 2.
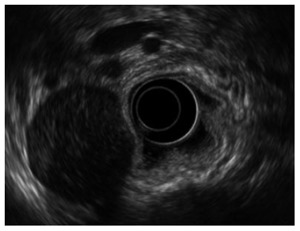
Endoscopic ultrasound. Endoscopic ultrasonography showed a heterogenic hypoechoic mass with extraluminal growth originating from the muscularis propria layer.
Figure 3.

Abdominal computerized tomography scan showing the 3.5 cm × 2.5 cm tumor with exophytic growth.
Figure 4.
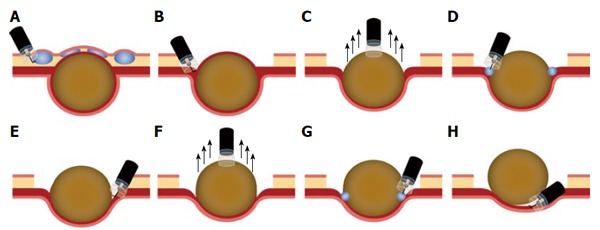
Illustration of the endoscopic suction excavation technique. A: After submucosal injection of sodium hyaluronate, a circumferential incision and removal of the overlying mucosa were performed; B, E: Careful muscular dissection between the tumor and serosa with a hook knife; C, F: Endoscopic suction using the end of a cap-fitted endoscope attached to the tumor; D, G: Submucosal injection of sodium hyaluronate; H: Tumor fully extracted after repeated careful dissection and endoscopic suction.
Figure 5.
Tumor was exposed after removing the overlying mucosa.
Figure 6.
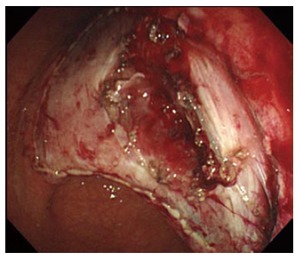
Extraction showing no perforation.
The tumor dimensions were 3.5 cm × 2.8 cm × 2.5 cm (Figure 7). Immunohistochemical staining showed that the tumor was positive for C-KIT and CD34. It was diagnosed as GIST. The mitotic count was 6/50 high-power fields. Although the patient had a high risk of recurrence according to risk stratification analysis, further surgery could not be performed owing to the patient’s unwillingness to undergo surgical resection. No tumor recurrence occurred during the 5-year follow-up period (Figure 8).
Figure 7.
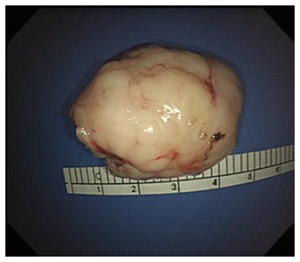
Extracted tumor after repeated muscular dissection and endoscopic suction.
Figure 8.
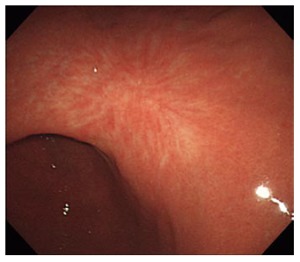
Endoscopic submucosal dissection scar after 5 years.
DISCUSSION
The number of clinical trials investigating endoscopic resection of SETs originating from the muscularis propria layer has recently increased. These trials have reported that some SETs originating from the muscularis propria layer can be safely resected by using gastrointestinal endoscopy without perforation or any other serious complications. However, it is not yet known which of these tumors is an appropriate indication for endoscopic resection. Appropriate indications for endoscopic resection should be based on low complication and recurrence rates. A previous study showed that a positive rolling sign and a small tumor size are appropriate indications for endoscopic removal. In addition, successful endoscopic resection of GISTs depends on their location in the gastric wall[4]. Submucosal tumors that protrude mainly into the serosal side of the gastric wall are not easy to resect completely using an endoscopic method. Nevertheless, further studies are required to verify these findings. In cases of exophytic GISTs, surgical or endoscopic full-thickness resection with laparoscopic support is generally indicated. However, this case shows that even exophytic GISTs can potentially be endoscopically resected without perforation.
Previous endoscopic therapy did not emphasize the suction concept, but we showed that suction excavation is useful for SET removal. Full endoscopic suction can move SETs in an endoluminal direction, so our technique has the advantage of reducing perforation risk compared with previous endoscopic submucosal dissection techniques. However, the suction excavation technique has its own limitations. If the SETs do not move inward by endoscopic suction, this technique cannot be used for endoscopic resection. Therefore, it is difficult to apply our suction excavation technique to all exophytic SET resections. The use of the suction excavation technique to remove exophytic SETs has limited indications, such as a positive rolling sign, small tumor size, and moving sign by endoscopic suction. However, the suction excavation technique can be useful for removing simple SETs as well as exophytic SETs in clinical practice.
Most cases of recurrence after surgical resection of a GIST involve intraperitoneal or hepatic recurrence. Local recurrence itself is very rare. The risk factors of GIST recurrence include not only tumor size and the number of mitoses but also exposure of tumor cells in the abdominal cavity after the capsule of the tumor is ruptured[5]. If gastric perforation can be avoided during endoscopic resection, the risk of tumor cell exposure in the abdominal cavity could be lower than that of surgical resection and the frequency of intra-abdominal recurrence would decrease accordingly. As such, avoidance of gastric perforation during endoscopic resection is critical. In this case, the patient was followed for 5 years without tumor recurrence. A recent study comparing the results of endoscopic versus surgical resection of a GIST in the upper gastrointestinal tract found that endoscopic resection could be an alternative therapeutic modality in selective cases[5]. In our subject’s case, the tumor showed extraluminal bulging or exophytic growth, and thus, the risk of perforation during endoscopic resection was very high. This suction excavation method can be safer than endoscopic submucosal dissection. Although this method does require physician experience, it can be helpful in difficult cases of endoscopic GIST removal.
In the case presented here, a full-thickness resection with laparoscopic support followed by laparoscopic gastroparietal suture, as opposed to an endoscopic-only procedure, is usually indicated. In this case, endoscopic resection of the extraluminal bulging SET using a suction excavation technique without laparoscopic support was successfully performed for the first time. Although not all exophytic GISTs can be resected endoscopically using this excavation technique, we do hope that this method may aid in the removal of tough submucosal tumors using gastrointestinal endoscopy.
COMMENTS
Case characteristics
A 49-year-old woman presented for further management of a gastric subepithelial tumor on the lesser curvature of the lower body, originally detected via routine upper gastrointestinal endoscopy.
Clinical diagnosis
The esophagogastroduodenoscopy performed outside the hospital showed a 4-cm mass with a smooth tapered margin located in the lower body, on the side of lesser curvature. The mass was hard and immovable upon palpation with biopsy forceps.
Differential diagnosis
Subepithelial tumor: Gastrointestinal stromal tumor, leiomyoma, granular cell tumor, ectopic pancreas.
Laboratory diagnosis
All labs were within normal limits.
Imaging diagnosis
Endoscopic ultrasound showed a heterogeneous hypoechoic mass with extraluminal growth, originating from the muscularis propria layer. An abdominal CT scan showed a 4-cm extraluminally protruding mass compressing the gastric wall.
Pathological diagnosis
Immunohistochemical staining showed that the tumor was positive for C-KIT and CD34. It was diagnosed as gastrointestinal stromal tumors (GISTs). The mitotic count was 6/50 high-power fields.
Treatment
Endoscopic resection of an exophytic GIST using the suction excavation technique.
Related reports
Most GISTs are treated surgically, and endoscopic resection was contraindicated as the risk of perforation and incomplete resection is high. However, several authors have recently reported successful results using endoscopic resection of a subepithelial tumor (SET) originating from the muscularis propria layer, including GISTs. A GIST with exophytic growth was previously considered a contraindication for endoscopic resection. In cases of exophytic GISTs, surgical or endoscopic full-thickness resection with laparoscopic support is generally indicated. However, this case shows that even exophytic GISTs can potentially be endoscopically resected without perforation using the suction excavation method.
Term explanation
GISTs are the most common mesenchymal neoplasms of the gastrointestinal tract that arise in smooth muscle pacemaker cells such as interstitial cells of Cajal.
Experiences and lessons
The suction excavation technique described here is a helpful technique to remove exophytic SETs. Previous endoscopic therapy did not emphasize the suction concept, but we showed that suction excavation is useful for SET removal.
Peer-review
The paper is well written.
Footnotes
Supported by Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea, No. HI14C3477; and Korea University grant, No. K1523601.
Institutional review board statement: The study was approved by the institutional review board of Korea University Anam Hospital, No. AN15332-001.
Informed consent statement: This patient provided informed consent before participation.
Conflict-of-interest statement: The authors have no conflicts of interest to declare.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: February 2, 2016
First decision: March 21, 2016
Article in press: May 4, 2016
P- Reviewer: Amornyotin S, Aytac E S- Editor: Qi Y L- Editor: A E- Editor: Ma S
References
- 1.Choi HS, Chun HJ, Keum B, Jeen YT. The indications for endoscopic resection of esophageal submucosal tumor. Gastrointest Endosc. 2012;76:225–226; author reply 226. doi: 10.1016/j.gie.2012.01.043. [DOI] [PubMed] [Google Scholar]
- 2.Chun SY, Kim KO, Park DS, Lee IJ, Park JW, Moon SH, Baek IH, Kim JH, Park CK, Kwon MJ. Endoscopic submucosal dissection as a treatment for gastric subepithelial tumors that originate from the muscularis propria layer: a preliminary analysis of appropriate indications. Surg Endosc. 2013;27:3271–3279. doi: 10.1007/s00464-013-2904-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chun HJ, Hyun JH. Endoscopic removal of submucous tumours. Baillieres Best Pract Res Clin Gastroenterol. 1999;13:145–163. doi: 10.1053/bega.1999.0014. [DOI] [PubMed] [Google Scholar]
- 4.Kim HH. Endoscopic treatment for gastrointestinal stromal tumor: Advantages and hurdles. World J Gastrointest Endosc. 2015;7:192–205. doi: 10.4253/wjge.v7.i3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Joo MK, Park JJ, Kim H, Koh JS, Lee BJ, Chun HJ, Lee SW, Jang YJ, Mok YJ, Bak YT. Endoscopic versus surgical resection of GI stromal tumors in the upper GI tract. Gastrointest Endosc. 2016;83:318–326. doi: 10.1016/j.gie.2015.07.034. [DOI] [PubMed] [Google Scholar]


