ABSTRACT
Many chronic myelogenous leukemia (CML) patients in chronic phase who respond well to imatinib therapy show fluctuations in their leukemic loads in the long-term. We developed a mathematical model of CML that incorporates the intervention of an autologous immune response. Our results suggest that the patient's immune system plays a crucial role in imatinib therapy in maintaining disease control over time. The observed BCR-ABL/ABL oscillations in such patients provide a signature of the autologous immune response.
KEYWORDS: Chronic myelogenous leukemia, imatinib, mathematical modeling, TKI
Since their introduction in the early 2000s, tyrosine kinase inhibitors (TKIs) such as imatinib mesylate (IM) have transformed chronic phase CML (CP-CML) into a long-term survivable and manageable condition.1 Unfortunately, TKIs are not curative in the majority of cases, and as a result, patients need to continue therapy indefinitely, a requirement that is both expensive and impairs their quality of life. Further study of the underlying mechanisms of action of TKIs will elucidate whether this limitation is the result of a suboptimal therapy schedule (that is, if changes in the timing and dosage might actually result in a curative therapy), or whether TKIs alone are simply insufficient and combination therapy is necessary. Mathematical modeling is a valuable and complementary tool to clinical data that can be used both to investigate existing therapeutic strategies and to propose novel combinations.
Several mathematical modeling groups have studied various aspects of CML and TKI therapy.2–5 Both Michor et al.3 and Roeder et al.4 observed that at the beginning of IM therapy, leukemic loads exhibit an initial sharp exponential decline, followed by a second, slower exponential decline. While Michor et al. argued that this biphasic exponential decline is the result of decreased proliferative capacities of leukemic progenitors and differentiated cells, Roeder et al. hypothesized that IM affects cycling leukemic stem cells while having no direct effect on quiescent cells. Although both modeling frameworks3,4 capture some characteristic initial responses to therapy, they do not include mechanisms that allow oscillations in the BCR-ABL/ABL ratio to develop. While some patients' leukemic loads monotonically decline, resulting in a triphasic exponential decline,5 our patient data indicates that the leukemic loads of many responding patients exhibit fluctuations. These fluctuations do not necessarily indicate relapse but appear to be an integral part of the response to TKI therapy.
The autologous immune response is known to play a significant role in many cancers, including CML. Prior to TKIs, many CML patients were treated with either allogeneic bone marrow transplants6 or interferon-α (IFN-α),7 both of whose success seem to partially depend on inducing an immune response. Although TKIs are the current standard of care nowadays, combinations of TKIs with IFN-α are currently being investigated by us and others,7 in part, because of the latter's immunostimulatory effects. Additionally, in two independent trials,8,9 patients who had responded well to TKIs were taken off therapy in order to determine whether treatment-free remission (TFR) could be achieved. While ∼60% of participants relapsed within the first 6 mo, the remaining 40% remained in TFR for several years. Interestingly, many of these patients continued to harbor small residual leukemic populations but nonetheless remained in remission. In the absence of drug, some other mechanism, for instance the immune system, might be preventing the leukemic cells from expanding.
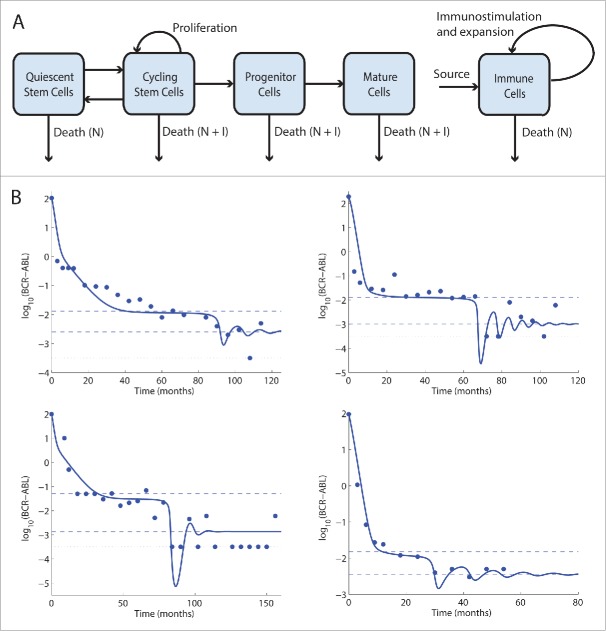
We therefore constructed a mathematical model (depicted in Fig. 1A) that integrates CML and the intervention of an autologous immune response.10 We encode an immune response in which small leukemic loads are an insufficient stimulus, while large leukemic loads suppress the immune system, thereby limiting its response to CML. However, at intermediate levels of leukemia, which we call an immune window, a balance between immunostimulation and immunosuppression is achieved, and the autologous immune system is able to mount an efficient response against CML. This mechanism allowed us to fit our model to patients showing non-monotonic variations in leukemic load. Representative fits of our model to patient data are provided in Fig. 1B.
Figure 1.
(A) A diagram representing our model of CML and the autologous immune system. Leukemic cells are divided into cycling and quiescent stem cells, progenitors, and mature cells, while there is a single immune cell compartment. Unlabeled arrows indicate transitions of leukemic cells between the compartments. Outgoing arrows indicate cell death, which can occur naturally (N) or as a result of an immune response (I). (B) Four representative fits of our model to patient data. Dots represent patient data, while the thick solid lines are our fits. Dashed lines mark the ends of the immune window. The horizontal dotted lines at y = −3.5 approximate the minimal leukemic concentration that is detectable by quantitative RT-PCR. Dots along this line represent zero measurements.
Based on our patient data and modeling results, we hypothesize that patients receiving TKI therapy go through three phases of leukemia reduction.10 The initial two phases are similar to the biphasic decline described previously.3,4 During this time, because leukemic loads are still large, the immune system plays a minimal role, and the decline in the leukemic population is driven primarily by the drug. However, as a result of the biphasic decline, the leukemic load may be driven into the immune window, which allows the immune population to develop an efficient first response, an event that marks the beginning of the third stage of therapy. The leukemic population is driven below the immune window, causing the immune population to contract, allowing the leukemia to partially recover. Eventually the leukemia reenters the immune window, which initiates another weaker immune response. This process repeats, producing oscillations in the leukemic and immune populations as the two populations approach equilibrium.
Our patient data and modeling results suggest that the patient's autologous immune system plays a significant role in the dynamics of TKI therapy. Moreover, the fluctuations that occur following the biphasic exponential decline may be explained by the immune system and therefore serve as a signature of a patient's individual immune profile. Our mathematical model is a potential tool for quantifying such interpatient differences, in order to design patient-specific therapies aimed at achieving TFR. An active collaboration between clinicians, mathematicians, and experimentalists aims at using adaptive and quantitative tools for improving patient care.
Disclosure of potential confllicts of interest
No potentential conflicts of interest were disclosed.
References
- 1.An X, Tiwari AK, Sun Y, Ding PR, Ashby CR Jr, Chen ZS. BCR-ABL tyrosine kinase inhibitors in the treatment of Philadelphia chromosome positive chronic myeloid leukemia: A review. Leukemia Res 2010; 34:1255–68; PMID:20537386; http://dx.doi.org/15988530 10.1016/j.leukres.2010.04.016 [DOI] [PubMed] [Google Scholar]
- 2.Kim P, Lee P, Levy D. Dynamics and potential impact of the immune response to chronic myelogenous leukemia. PloS Comp Biol 2008; 4(6):e1000095; PMID:18566683; http://dx.doi.org/15988530 10.1371/journal.pcbi.1000095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Michor F, Hughes F, Iwasa Y, Branford S, Shah N, Sawyers C, Nowak MA. Dynamics of chronic myeloid leukaemia. Nature 2005; 435(30):1267–70; PMID:15988530; http://dx.doi.org/ 10.1038/nature03669 [DOI] [PubMed] [Google Scholar]
- 4.Roeder I, Horn M, Glauche I, Hochhaus A, Mueller M, Loeffler M. Dynamic modeling of imatinib-treated chronic myeloid leukemia: Functional insights and clinical implications. Nature Med 2006; 12(10):1181–4; PMID:17013383; http://dx.doi.org/ 10.1038/nm1487 [DOI] [PubMed] [Google Scholar]
- 5.Tang M, Gonen M, Quintas-Cardama A, Cortes J, Kantarjian H, Field C, Hughes TP, Branford S, Michor F. Dynamics of chronic myeloid leukemia response to long-term targeted therapy reveal treatment effects on leukemic stem cells. Blood 2011; 118(6):1622–31; PMID:21653938; http://dx.doi.org/ 10.1182/blood-2011-02-339267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kolb HJ, Schattenberg A, Goldman JM, Hertenstein B, Jacobsen N, Arcese W, Ljungman P, Ferrant A, Verdonck L, Niederwieser D et al.. Graft versus leukemia effect of donor lymphocyte transfusions in marrow grafted patients European Group for Blood and Marrow Transplantation Working Party Chronic Leukemia. Blood 1995; 86(5):2041–50; PMID:7655033 [PubMed] [Google Scholar]
- 7.Talpaz M, Hehlmann R, Quintás-Cardama A, Mercer J, Cortes J. Re-emergence of interferon-α in the treatment of chronic myeloid leukemia. Leukemia 2013; 27:803–12; PMID:23238589; http://dx.doi.org/ 10.1038/leu.2012.313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahon FX, Rea D, Guilhot J, Guilhot F, Huguet F, Nicolini F, Legros L, Charbonnier A, Guerci A, Varet S et al.. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol 2010; 11(11):1029–35; PMID:20965785; http://dx.doi.org/ 10.1016/S1470-2045(10)70233-3 [DOI] [PubMed] [Google Scholar]
- 9.Ross DM, Branford S, Seymour JF, Schwarer AP, Arthur C, Yeung DT, Dang P, Goyne JM, Slader C, Filshie RJ et al.. Safety and efficacy of imatinib cessation for CML patients with stable undetectable minimal residual disease: results from the TWISTER study. Blood 2013; 122:515–22; PMID:23704092; http://dx.doi.org/ 10.1182/blood-2013-02-483750 [DOI] [PubMed] [Google Scholar]
- 10.Clapp G, Lepoutre T, El Cheikh R, Bernard S, Ruby J, Labussiere-Wallet H. Implication of the autologous immune system in BCR-ABL transcript variations in chronic myelogenous leukemia patients treated with imatinib. Cancer Res 2015; 75(19):4053–62; PMID:26359456; http://dx.doi.org/ 10.1158/0008-5472.CAN-15-0611 [DOI] [PubMed] [Google Scholar]