Abstract
Objective
Diabetes is a so-called ambulatory care sensitive condition. It is assumed that by appropriate and timely primary care, hospital admissions for complications of such conditions can be avoided. This study examines whether differences between countries in diabetes-related hospitalization rates can be attributed to differences in the organization of primary care in these countries.
Design
Data on characteristics of primary care systems were obtained from the QUALICOPC study that includes surveys held among general practitioners and their patients in 34 countries. Data on avoidable hospitalizations were obtained from the OECD Health Care Quality Indicator project. Negative binomial regressions were carried out to investigate the association between characteristics of primary care and diabetes-related hospitalizations.
Setting
A total of 23 countries.
Subjects
General practitioners and patients.
Main outcome measures
Diabetes-related avoidable hospitalizations.
Results
Continuity of care was associated with lower rates of diabetes-related hospitalization. Broader task profiles for general practitioners and more medical equipment in general practice were associated with higher rates of admissions for uncontrolled diabetes. Countries where patients perceive better access to care had higher rates of hospital admissions for long-term diabetes complications. There was no association between disease management programmes and rates of diabetes-related hospitalization. Hospital bed supply was strongly associated with admission rates for uncontrolled diabetes and long-term complications.
Conclusions
Countries with elements of strong primary care do not necessarily have lower rates of diabetes-related hospitalizations. Hospital bed supply appeared to be a very important factor in this relationship. Apparently, it takes more than strong primary care to avoid hospitalizations.
Key points
Countries with elements of strong primary care do not necessarily have lower rates of diabetes-related avoidable hospitalization.
Hospital bed supply is strongly associated with admission rates for uncontrolled diabetes and long-term complications.
Continuity of care was associated with lower rates of diabetes-related hospitalization.
Better access to care, broader task profiles for general practitioners, and more medical equipment in general practice was associated with higher rates of admissions for diabetes.
Keywords: Avoidable hospitalization, diabetes, general practice, health services research, primary care, The Netherlands
Introduction
Ambulatory care sensitive conditions (ACSCs) are conditions for which inpatient admissions can potentially be prevented by appropriate and timely outpatient care.[1,2] Primary care services that manage chronic diseases to prevent complications can reduce or even prevent hospitalization. Diabetes is often seen as one of the most important ACSCs and diabetes-related hospital admissions are frequently used as a quality indicator for primary care.[3,4] Diabetes is an increasing public health issue and causes substantial health services use and costs around the world. In Europe, it is estimated that 8.5% of the adult population has diabetes and annual diabetes-related health care costs are at least US$147 billion worldwide.[5]
Diabetes care is complex and delivered by different care providers in different settings across the healthcare system. Better coordination through all levels of care is hypothesized to result in better health outcomes and fewer hospitalizations. However, evidence for this hypothesis is inconclusive.[6] In most countries, the major part of diabetes care is provided in primary care. Primary care is supposed to provide care close to patients with no access barriers, comprehensive to the needs of patients, coordinate care through all health care levels and is continuous over time.[7,8]
In general, it is believed that primary care for people with early stage diabetes will result in better health and save health care costs. Some features of primary care can influence rates of hospitalization for diabetes.[6,9] For instance, the relationship between better access to primary care and fewer admissions for ACSCs, including diabetes, has been confirmed in several studies.[9,10] Also patients who have a continuous relationship with their care providers have overall better health outcomes in terms of fewer emergency department visits and better control of chronic diseases.[11] Several studies have shown that patients with a continuous relationship with their primary care provider have less chance of being admitted for diabetes complications.[12–15] Likewise, patients in primary care networks that focus on good access to care and employ multidisciplinary teams have fewer hospital admissions.[16]
Most studies investigating the relationship between primary care and diabetes-related hospitalizations focus on a single healthcare system, rather than comparing healthcare systems. A study by Kringos and colleagues compared system features of different European primary care systems and showed a correlation between better accessibility and lower rates of diabetes-related hospitalization.[17] The main research question of the present study is whether strong primary care suffices to prevent potentially avoidable hospital admissions for diabetes. We extend the work of Kringos by using experiences of general practitioners (GPs) and patients with aspects of primary care. First, we will examine whether differences between countries in prevalence of diabetes-related hospitalization are related to differences in the organization of primary care, in terms of continuity, access, comprehensiveness, and coordination, and second which of these aspects are important in reducing diabetes-related hospitalizations. Third, we will explore the influence of hospital bed supply on diabetes-related hospitalizations. The overall rate of avoidable hospital admissions may partly be determined by countries’ capacity to admit patients; countries with a higher number of hospital beds are assumed to be more likely to admit patients.
Material and methods
Data sources
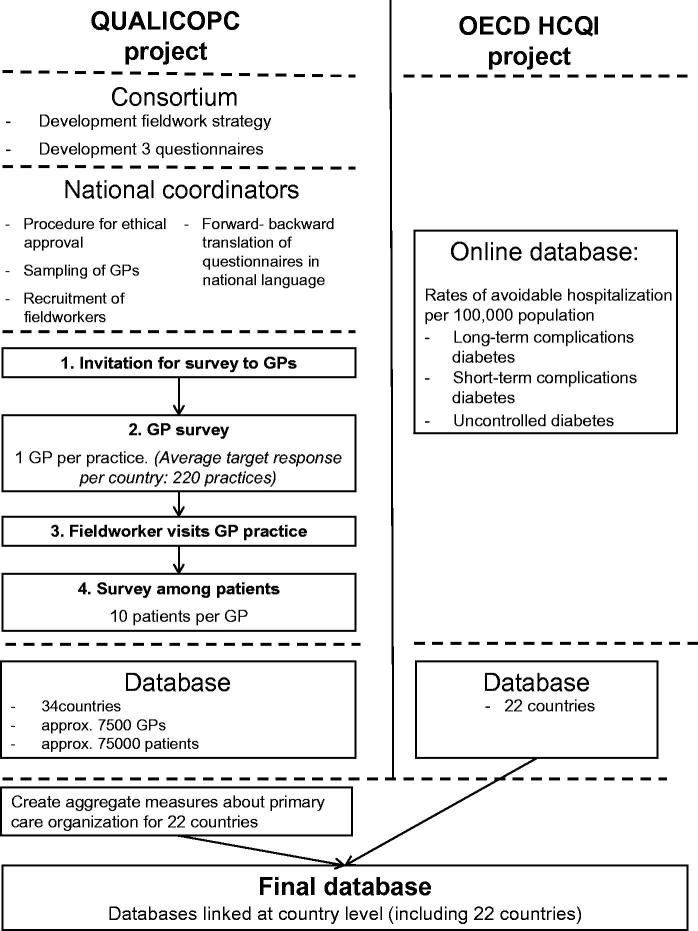
Two data sources were used to explore the association between primary care organization and the rate of diabetes-related hospitalizations (Figure 1). First, data on hospitalization for diabetes at country level were obtained from the OECD Healthcare Quality Indicators project.[3] For 22 countries, age and sex-standardized hospitalization rates were obtained per 100 000 population. Additionally, data on hospitalization for England were obtained from NHS England; the data had been collected in accordance with the definition of the OECD healthcare quality indicator data collection.
Figure 1. Used data sources.
Second, data regarding the organization of primary care were collected in the context of the cross-sectional QUALICOPC study (Quality and Costs of Primary Care in Europe), by means of standardized surveys among GPs and patients in 31 European countries including the EU 27 (except for France), FYR Macedonia, Iceland, Norway, Switzerland, and Turkey and three non-European countries (Australia, Canada, and New Zealand). Data collection took place between October 2011 and December 2013. In each country a national representative sample of GPs filled out a questionnaire (target n = 220; for Cyprus, Iceland, Luxembourg, and Malta n = 80). Random sampling was used to select practitioners in countries where national registers of practitioners were available. In countries with only regional registers, random samples were drawn from regions that represent the national setting. If only lists of facilities in a country existed a random selection of these lists was made. Per practice or health centre, one GP was eligible for participation. Information on participation rates can be found elsewhere.[18,19] In every GP practice, nine people who visited the GP filled out a patient experience questionnaire concernning the consultation that had just occurred. Patients do not necessarily have diabetes, but they constitute a sample of the general population. Ethical approval was acquired in accordance with the legal requirements in each country. Details concerning the study protocol and questionnaire development have been published elsewhere.[20,21]
Dependent variables
We would have liked to measure the dependent variables on patient level. This was, however, not achievable because the prevalence of avoidable hospitalization is low, for example the mean prevalence of asthma in the included countries was 49 per 100 000. An individual level analysis would not be feasible at such an international level with any dataset available. Therefore, we used an aggregated measure on a higher level. Data on diabetes-related hospitalizations at country-level were available for uncontrolled diabetes, long-term complications, and short-term complications. These three outcome measures were used as dependent variables. Short-term complications were defined as not maternal or neonatal, that occur in people aged 15 years or older and are the result of an insulin deficiency. Examples include coma or ketoacidosis. Long-term complications were defined as not maternal or neonatal, that occur in people aged 15 years or older, and include complications like renal, eye, or circulatory problems. Admissions for uncontrolled diabetes included inpatient admissions with the principal diagnosis code for uncontrolled diabetes. Details on which ICD-codes are included in the three outcome measures are presented in appendix Table SI.
Independent variables
The independent variables are measured based on the responses of the GP and patient to the questionnaire of the QUALICOPC study. For the operationalization of organizational characteristics of primary care, nine scales were created for the following concepts: continuity, comprehensiveness, coordination, and access. Scale scores range from 0 to 10; the higher the score the better a concept is incorporated within a country. Details on the scales can be found in appendix Table SII.
Continuity: Two scales were created for primary care continuity: longitudinal continuity and informational continuity. Longitudinal continuity indicates the long-term relationship between primary care providers and patients, and informational continuity refers to the availability of patients’ medical information, such as medical records.
Coordination: Coordination of care refers to the ability of the system to coordinate care across different levels of healthcare. Two scales were included: GPs’ involvement in chronic care management for diabetes and skill mix within GP practices. Skill mix included the following disciplines working within GP practices besides GPs: receptionist/medical secretary, practice nurse, community or home care nurse, nurse practitioner, laboratory assistant, physiotherapist, and pharmacist.
Comprehensiveness: Comprehensiveness of care indicates the availability of services in GP practices to serve the needs of patients, including the availability of medical equipment for diagnosis and management of diabetes, health-promotion activities that are systematically performed, and the broadness of GPs’ task profile.
Access: Access to primary care services was measured by two features: patient perceived access and out-of-hours care arrangements.
Statistical analyses
Because of the high aggregation level of the dependent variables, the independent variables were also summarized at country level. To be able to do so, scale scores were created using the ecometrics approach in which multi-level analyses were used to construct a contextual variable at a higher level unit based on several related individual variables.[22] An additional level for the related scale items was added in a multi-level model. We used a four-level model (items, patients, GPs and countries). To calculate the average scale value, a weighted item average was used for each item and the item variance was taken into account. The scales are created using MLwiN and range from 0 to 10. The reliability of all constructed ecometric scales was estimated based on the variance at the different levels, i.e. items nested within respondents and respondents nested within countries.[22] The correlation between the different scales is presented in appendix Table SIII.
After creating the scales, the associations between dependent and independent variables were estimated with negative binomial analyses using Stata 13™ (StataCorp LP, College Station, TX, USA). Negative binomial analyses were preferred to normal Poisson regression because of over-dispersion of the dependent variables. All independent variables were analysed separately because of the small number of observations. First, the association between dependent and independent variables was controlled for diabetes prevalence. Diabetes prevalence was derived from the International Diabetes Federation (IDF) Atlas.[5] Second, the models were estimated including a variable for hospital bed supply. This variable was derived from the OECD health data and defined as the total number of available hospital beds per 1000 population.[3] Incident rate ratios (IRR) were calculated. Because of low statistical power, p-values of both 0.05 and 0.10 are presented. Residual analyses were done to identify potential outliers and influential cases.
The following countries were included in the analyses: Australia, Austria, Belgium, Canada, Czech Republic, Denmark, England, Finland, Germany, Hungary, Iceland, Ireland, Italy, Latvia, New Zealand, Norway, Poland, Portugal, Spain, Sweden and Switzerland. The Netherlands and Slovenia were excluded from the analyses of uncontrolled diabetes hospital admission because of lacking data.
Results
Scales on the primary care characteristics were created with scale scores for 23 countries based on questionnaires from 45 082 patients and 5098 GPs. Sample sizes per country can be found in Table 1. The reliability of the scales created varied from 0.856 to 0.997. Table 2 gives the mean and range of the variables. Table 3 gives the results of the regression analyses both controlled and not controlled for hospital bed supply. In all analyses of admission rates for uncontrolled diabetes and long-term complications, hospital bed supply had a strong positive association with hospitalization rates.
Table 1.
Sample sizes per country within QUALICOPC study.
| Country | No. of general practitioners questionnaires | No. of patient experience questionnaires |
|---|---|---|
| Australia | 113 | 1190 |
| Austria | 180 | 1596 |
| Belgium | 411 | 3677 |
| Canada | 553 | 5009 |
| Czech Republic | 220 | 1980 |
| Denmark | 212 | 1878 |
| England | 160 | 1296 |
| Finland | 139 | 1196 |
| Germany | 237 | 2117 |
| Hungary | 221 | 1934 |
| Iceland | 90 | 761 |
| Ireland | 191 | 1694 |
| Italy | 219 | 1959 |
| Latvia | 218 | 1951 |
| Netherlands | 228 | 2012 |
| New Zealand | 131 | 1150 |
| Norway | 203 | 1529 |
| Poland | 220 | 1975 |
| Portugal | 212 | 1920 |
| Slovenia | 219 | 1963 |
| Spain | 433 | 3731 |
| Sweden | 88 | 773 |
| Switzerland | 200 | 1791 |
| Total | 5098 | 45 082 |
Table 2.
Description of dependent and independent variables.
| Dependent variable: | Mean rate per 100 000 | Lowest (country) | Highest (country) |
|---|---|---|---|
| Hospitalization | |||
| Long-term diabetes complications | 87.6 | 19.4 (England) | 249.9 (Hungary) |
| Short-term diabetes complications | 18.3 | 7.8 (Italy) | 37.5 (Ireland) |
| Uncontrolled diabetes | 43.2 | 7.2 (Australia) | 180.7 (Austria) |
| Independent variable: | Mean (SD) | Lowest (country) | Highest (country) |
| Continuity | |||
| Long-term continuity | 9.37 (0.49) | 7.83 (Sweden) | 9.78 (New Zealand) |
| Availability of medical information | 8.99 (0.61) | 7.76 (Hungary) | 9.82 (Canada) |
| Coordination | |||
| Skill mix | 3.13 (2.14) | 0.27(Belgium) | 7.88 (Finland) |
| Diabetes chronic care management | 6.16 (1.72) | 2.89 (Switzerland) | 8.88 (England) |
| Comprehensiveness | |||
| Medical equipment | 6.61 (2.10) | 1.93 (Italy) | 9.73 (Switzerland) |
| Task profile | 7.46 (0.68) | 6.09 (Czech Republic) | 8.46 (Sweden) |
| Health promotion | 1.59 (1.02) | 0.41(Denmark) | 3.95 (England) |
| Access | |||
| Organizational access | 8.72 (0.43) | 7.60 (Spain) | 9.30 (Netherlands) |
| Out-of-hours care | 6.55 (2.50) | 1.42 (Italy) | 9.85 (Netherlands) |
| Control variable: | Mean | Lowest (country) | Highest (country) |
| Diabetes prevalence (%) | 6.2 | 3.3 (Iceland) | 9.8 (Portugal) |
| Hospital bed supply, rate per 1000 | 4.6 | 2.7 (Sweden) | 8.3 (Germany) |
Table 3.
Results of negative binomial regression analyses of avoidable diabetes admissions and characteristics of primary care organization1.
| Uncontrolled diabetes (n = 21) |
Long-term complications (n = 23) |
Short-term complications (n = 23) |
|||||
|---|---|---|---|---|---|---|---|
| IRR | 95% CI | IRR | 95% CI | IRR | 95% CI | ||
| Continuity | |||||||
| Long-term continuity | Model 1 | 0.54 | 0.25–1.19 | 0.86 | 0.43–1.70 | 0.86 | 0.59–1.26 |
| Model 2 | 0.643 | 0.39–1.04 | 1.00 | 0.66–1.53 | 0.84 | 0.58–1.22 | |
| Availability of medical information | Model 1 | 0.442 | 0.28–0.70 | 0.482 | 0.32–0.70 | 1.313 | 0.97–1.75 |
| Model 2 | 0.73 | 0.40–1.34 | 0.74 | 0.48–1.15 | 1.31 | 0.90–1.89 | |
| Coordination | |||||||
| Skill mix | Model 1 | 0.92 | 0.81–1.06 | 0.852 | 0.76–0.96 | 1.04 | 0.96–1.13 |
| Model 2 | 1.05 | 0.92–1.19 | 0.96 | 0.86–1.08 | 1.03 | 0.94–1.12 | |
| Diabetes chronic care management | Model 1 | 1.08 | 0.86–1.35 | 0.97 | 0.80–1.18 | 1.09 | 0.98–1.21 |
| Model 2 | 1.08 | 0.92–1.27 | 1.02 | 0.88–1.17 | 1.08 | 0.97–1.20 | |
| Comprehensiveness | |||||||
| Medical equipment | Model 1 | 1.10 | 0.91–1.32 | 0.87 | 0.74–1.03 | 1.00 | 0.91–1.10 |
| Model 2 | 1.142 | 1.02–1.28 | 0.97 | 0.86–1.09 | 0.99 | 0.90–1.09 | |
| Task profile | Model 1 | 0.72 | 0.45–1.14 | 0.572 | 0.71–0.78 | 1.11 | 0.87–1.43 |
| Model 2 | 2.152 | 1.36–3.41 | 0.91 | 0.61–1.36 | 1.02 | 0.71–1.47 | |
| Health promotion | Model 1 | 1.13 | 0.77–1.66 | 1.04 | 0.73–1.49 | 1.03 | 0.87–1.24 |
| Model 2 | 0.89 | 0.68–1.16 | 0.89 | 0.70–1.12 | 1.05 | 0.88–1.25 | |
| Access | |||||||
| Organizational access | Model 1 | 1.50 | 0.69–3.25 | 2.312 | 1.22–4.37 | 1.06 | 0.70–1.62 |
| Model 2 | 0.84 | 0.46–1.53 | 1.662 | 1.07–2.60 | 1.13 | 0.74–1.73 | |
| Out-of-hours care | Model 1 | 1.05 | 0.91–1.22 | 0.913 | 0.82–1.01 | 1.00 | 0.92–1.07 |
| Model 2 | 1.093 | 0.99–1.21 | 0.96 | 0.89–1.04 | 0.99 | 0.92–1.06 | |
Notes: All primary care characteristics were analysed separately. Bold values indicate either p < 0.10 or p < 0.05.
Model 1 shows the results controlled for diabetes prevalence only; model 2 shows the results controlled for diabetes prevalence and hospital bed supply. IRR =incident rate ratio.
p < 0.05
p < 0.10.
Continuity
The variation in continuity of care between countries was small for both measures. The mean score for long-term continuity was 9.4 on a scale from 0 to 10, with Sweden showing the lowest score (7.8), and New Zealand showing the highest score (9.8). There was no significant association between long-term continuity of primary care and rates of avoidable hospitalization for diabetes-related complications. When controlled for diabetes prevalence and hospital bed supply, countries with higher scores on the long-term continuity scale had lower incidence rates of uncontrolled diabetes admissions (IRR 0.64, 95% CI 0.39–1.04, p < 0.1).
The mean score for the availability of medical information was 9.0, with a range from 7.8 in Hungary to 9.8 in Canada. When controlled for diabetes prevalence, the availability of medical information was strongly associated with lower admission rates for uncontrolled diabetes and long-term complications.
Coordination
There was more variation between countries on the primary care feature “coordination of care” compared with continuity. England, Germany, and Denmark scored the highest on the scale for diabetes chronic care management, with scores higher than 8 on a scale from 0 to 10. Switzerland, Iceland, and Norway were less involved in diabetes chronic care management, having scores below 4. Involvement in chronic care for diabetes was not associated with diabetes-related admission rates.
A large degree of variation was found between countries for skill mix within primary care. Belgium had the lowest number of disciplines working in GP practices, scoring 0.3, while Finland scored 7.9. When controlling for diabetes prevalence, a broader skill mix was associated with lower admission rates for long-term complications (IRR 0.85, 95% CI 0.76–0.96). However, after controlling for hospital bed supply, the association had the same direction but was no longer statistically significant.
Comprehensiveness
Scores on availability of medical equipment in GP practices used for management of diabetes was lowest in Italy (1.9) and highest in Switzerland (9.7). More medical equipment was significantly associated with higher rates of avoidable hospitalization for uncontrolled diabetes (IRR 1.17, 95% CI 1.02–1.33).
Health-promotion activities performed by GPs were not common in most countries. All countries scored below four on the scale from 0 to 10, with Denmark scoring lowest with a score of 0.41. Health promotion was not associated with diabetes admissions.
In Sweden, GPs had the broadest task profile; the score was 8.5. The broader the GP’s task profile, the higher the incidence rate of uncontrolled diabetes hospital admissions when controlled for diabetes prevalence and hospital bed supply (IRR 2.15, 95% CI 1.36–3.41). When controlled for diabetes prevalence, the results for admissions for long-term complications showed a decrease in incidence rate for a broader task profile (IRR 0.57; 95% CI 0.71–0.78). After additional controlling for hospital bed supply, this association was no longer statistically significant.
Access
Patient-perceived access was high in all countries. The mean score was 8.7. A higher perceived access was associated with a higher incidence rate of admissions for long-term complications (IRR 1.66, 95% CI 1.07–2.60). The availability of out-of-hours GP care varied widely between countries. Italy scored lowest (2.0) and the Netherlands scored highest with 8.8. Out-of-hours primary care arrangements were not associated with rates of diabetes-related admissions.
Discussion
The results of this study show that when taking country differentials in hospital bed supply into account, countries where GP practices have more medical equipment, and GPs have a broader task profile, rates of hospital admission for uncontrolled diabetes tend to be higher. In addition, patients perceiving better accessibility are more likely to be admitted for long-term complications.
We hypothesized that healthcare systems with easy access to primary care have lower hospitalization rates because problems are detected at an earlier stage and disease deterioration can be prevented. However, the results reject this hypothesis and show an association in the opposite direction: in countries where patients experience good access, patients have a significantly higher chance of being admitted for long-term complications.
Kringos investigated the association between primary care accessibility and rates of admission for short-term complications and showed that this association was correlated with reduced rates of hospitalization.[17] In the present study we found no such association, which might be explained by differences in data collection and analyses.
Continuity of primary care in this study is not associated with reduced diabetes admissions rates when hospital bed supply is taken into account. One possible explanation is that all countries scored high on continuity, with little variation between countries. In several national studies, patients with a continuous relationship with their primary care providers have a lower chance of being admitted for diabetes complications.[6] Likewise, countries that coordinate care within disease management programmes are not necessarily correlated with reduced diabetes admissions rates. Disease management programmes are often assumed to improve patient health outcomes and reduce health care costs. However, the effectiveness of such programmes is ambiguous and debated.[6,23]
In this study we found several results which reject our hypothesis that strong primary care prevents avoidable hospital admissions. We found some expected associations but they disappeared when hospital bed supply is taken into account. The higher the number of hospital beds in a country, the higher the number of avoidable hospital admissions. In our study, a country’s number of hospital beds seems to have more impact than aspects of good primary care, or rather the effect of primary care on reducing admissions is overshadowed by hospital bed supply.
The interaction between number of hospital beds, primary care, and admissions may be more complicated than it seems. The correlation between hospital beds and admissions is consistent with previous studies and is often explained by Roemer’s Law: “a built bed is a filled bed”.[24–26] When hospital bed occupancy is low, hospitals may be tempted to fill beds by easing indication criteria for admissions. GPs may be more likely to refer patients when thresholds are lower. Such an effect was shown for the Netherlands.[27] On the other hand, there may also be a reverse causation. In our study, we found that countries with more skill mix as well as broader task profiles in primary care also had a lower hospital bed supply. Such countries are probably more primary care oriented, deal with more health problems in primary care, and therefore need fewer hospital beds. Longitudinal studies, containing data before and after system reforms, are required to further unravel these relations.
Certain potential limitations to this study must be recognized. The analyses were performed at country level, with small numbers of observations. Avoidable hospitalization rates were not measured at patient level within the framework of the QUALICOPC study. At that level hospitalization rates are too low to measure, which would have led to insufficient statistical power. In addition, to avoid over-determination, only a few variables could be added simultaneously in the regression analyses. Therefore, we were unable to include all primary care measures in the multivariate model. Another downside of the use of country-level data was that, although the data were standardized on age to the OECD population, other relevant patient characteristics such as comorbidities could not be included.
Another limitation is that a sample of the general population who visited the GP were asked to participate in the QUALICOPC study. Therefore the participants did not necessarily have diabetes. Perspectives of the general population may differ from those who have diabetes, which is not taken into account in this study. Finally, the OECD states that differences in coding and differences in disease classification systems between practices and countries may affect the comparability of data.[3] For instance, we have seen that there is a very large range between countries in rates of avoidable hospitalizations. This might partly be explained by coding differences. The OECD is currently working on a combined measure for diabetes-related avoidable hospitalization in order to avoid this problem. Another problem of working with OECD data is that a distinction between type 1 and type 2 diabetes was not possible. The treatment for the two types differs, which may have affected the results. On the other hand, some primary care characteristics, such as continuity and accessibility, are important for both types.
The results show that the effect of primary care on reducing potentially avoidable hospitalizations, as was found in several studies focusing on one country or one healthcare system, is not necessarily confirmed between countries or between healthcare systems. The association between primary care and hospitalization might be influenced by other organizational factors. Countries differ with regard to the organization of primary care and other outpatient services. In some countries other ambulatory care settings feature more prominently in the healthcare system and may contribute to reducing diabetes-related admissions, like outpatient clinics, prevention clinics, and diagnostic and therapy services. The role of outpatient care in decreasing the rate of hospitalization for ACSCs, such as diabetes, has not yet been explored. In addition, different payment models for primary and secondary care exist within and between countries. They may conceivably have an effect on avoidable admissions. These models are not taken into account in the current study. The role of outpatient services and payment models is beyond the scope of the current study; however, it is good to bear in mind these considerations when interpreting our findings.
Hospitalizations for diabetes are supposed to be avoidable by timely and appropriate primary care. The present study showed that countries with elements of strong primary care do not necessarily have lower rates of diabetes-related avoidable hospitalization. That is to say, strong primary care alone might not suffice to reduce hospitalizations for conditions such as diabetes.
Supplementary Material
Acknowledgements
The authors would like to thank their partners in the QUALICOPC project for their role throughout the study and their coordination of the data collection: W. Boerma, P. Groenewegen, W. Schäfer, F. Schellevis, P. Spreeuwenberg, D. Kringos (NIVEL, coordinator, the Netherlands); J. De Maeseneer, E. De Ryck, L. Hanssens, A. Van Pottelberge, S. Willems (Belgium); S. Greß, S. Heinemann (Germany); G. Capitani, S. De Rosis, A.M. Murante, S. Nuti, C. Seghieri, M. Vainieri (Italy); D. Rotar Pavlič, I. Švab (Slovenia). They would also like to thank the coordinators of the data collection in each country and all persons who have supported the national coordinators in the data collection in their countries. Finally, the authors thank W. Limburg for English editing.
Ethical approval
Ethical approval was acquired in accordance with the legal requirements in each country. Both GP and patient surveys were carried out anonymously.
Disclosure statement
The authors declare that they have no competing interest. The authors are responsible for the content and writing of the paper.
Funding information
This article is based on the QUALICOPC (Quality and Costs of Primary Care in Europe) project, co-funded by the European Commission under the Seventh Framework Programme (FP7/2007-2013) under grant agreement 242141.
References
- [1].Billings J, Zeitel L, Lukomnik J, et al. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood). 1993;12:162–173. [DOI] [PubMed] [Google Scholar]
- [2].Weissman JS, Gatsonis C, Epstein AM.. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA. 1992;268:2388–2394. [PubMed] [Google Scholar]
- [3].OECD. Health at a Glance 2013: OECD Indicators. Geneva: OECD Publishing; 2013. [Google Scholar]
- [4].Agency for Healthcare Research and Quality (AHRQ). AHRQ quality indicators – guide to prevention quality indicators: hospital admission for ambulatory care sensitive conditions Rockville [cited 2014. July 14]. Available from: http://www.qualityindicators.ahrq.gov. [Google Scholar]
- [5].International Diabetes Federation . IDF Diabetes Atlas, 6th edn. Brussels: International Diabetes Federation; 2013. Available from: http://www.idf.org/diabetesatlas. [Google Scholar]
- [6].Van Loenen T, van den Berg MJ, Westert GP, Faber MJ.. Organizational aspects of primary care related to avoidable hospitalization: a systematic review. Fam Pract. 2014; 31:502–516. [DOI] [PubMed] [Google Scholar]
- [7].Kringos DS, Boerma WG, Hutchinson A, et al. The breadth of primary care: A systematic literature review of its core dimensions. BMC Health Services Res. 2010;10:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Starfield B. Is primary care essential? Lancet. 1994;344:1129–1133. [DOI] [PubMed] [Google Scholar]
- [9].Gibson OR, Segal L, McDermott RA.. A systematic review of evidence on the association between hospitalisation for chronic disease related ambulatory care sensitive conditions and primary health care resourcing. BMC Health Services Res. 2013;13:336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Rosano A, Abo Loha C, Falvo R, et al. The relationship between avoidable hospitalization and accessibility to primary care: a systematic review. Eur J Public Health. 2012; 2013 Jun;3:56-60. [DOI] [PubMed] [Google Scholar]
- [11].Saultz JW, Lochner J.. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005;3:159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chen CC, Chen SH.. Better continuity of care reduces costs for diabetic patients. American J Managed Care. 2011;17:420–427. [PubMed] [Google Scholar]
- [13].Christakis DA, Feudtner C, Pihoker C, Connell FA.. Continuity and quality of care for children with diabetes who are covered by Medicaid. Ambulatory Pediatrics. 2001;1:99–103. [DOI] [PubMed] [Google Scholar]
- [14].Hong JS, Kang HC.. Continuity of ambulatory care and health outcomes in adult patients with type 2 diabetes in Korea. Health Policy. 2013;109:158–165. [DOI] [PubMed] [Google Scholar]
- [15].Lin W, Huang IC, Wang SL, et al. Continuity of diabetes care is associated with avoidable hospitalizations: evidence from Taiwan’s National Health Insurance scheme. Int J Qual Health Care. 2010;22:3–8. [DOI] [PubMed] [Google Scholar]
- [16].Manns BJ, Tonelli M, Zhang J, et al. Enrolment in primary care networks: impact on outcomes and processes of care for patients with diabetes. CMAJ. 2012;184:E144–E152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kringos DS, Boerma W, van der Zee J, Groenewegen P.. Europe’s strong primary care systems are linked to better population health but also to higher health spending. Health Aff (Millwood). 2013;32:686–694. [DOI] [PubMed] [Google Scholar]
- [18].Schafer WL, Boerma WG, Murante AM, et al. Assessing the potential for improvement of primary care in 34 countries: a cross-sectional survey. Bull WHO. 2015;93:161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Groenewegen PP GS, Schafer WL.. General practitioners’ participation in a large, multi-country combined general practitioner–patient survey: recruitment procedures and participation rate. [Submitted 2015]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Schafer WL, Boerma WG, Kringos DS, et al. Measures of quality, costs and equity in primary health care instruments developed to analyse and compare primary care in 35 countries. Quality in Primary Care. 2013;21:67–79. [PubMed] [Google Scholar]
- [21].Schafer WL, Boerma WG, Kringos DS, et al. QUALICOPC, a multi-country study evaluating quality, costs and equity in primary care. BMC Fam Pract. 2011;12:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Raudenbush SW, Sampson RJ.. Ecometrics: toward a science of assessing ecological settings, with application to the systematic social observation of neighborhoods. Sociological Methodology. 1999;29:1–41. [Google Scholar]
- [23].De Bruin SR, Heijink R, Lemmens LC, et al. Impact of disease management programs on healthcare expenditures for patients with diabetes, depression, heart failure or chronic obstructive pulmonary disease: a systematic review of the literature. Health Policy. 2011;101:105–121. [DOI] [PubMed] [Google Scholar]
- [24].Brown LJ, Barnett JR.. Influence of bed supply and health care organization on regional and local patterns of diabetes related hospitalization. Soc Sci Med. 1992;35:1157–1170. [DOI] [PubMed] [Google Scholar]
- [25].Delamater PL, Messina JP, Grady SC, et al. Do more hospital beds lead to higher hospitalization rates? A spatial examination of Roemer’s Law. PLoS One. 2013;8:e54900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Roemer MI. Bed supply and hospital utilization: a natural experiment. Hospitals. 1961;35:36–42. [PubMed] [Google Scholar]
- [27].Van de Vijsel AR, Engelfriet PM, Westert GP.. Rendering hospital budgets volume based and open ended to reduce waiting lists: does it work? Health Policy. 2011;100:60–70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.