Abstract
Objective
Evidence regarding the benefits of strong primary care has influenced health policy and practice. This study focuses on changes in the breadth of services provided by general practitioners (GPs) in Europe between 1993 and 2012 and offers possible explanations for these changes.
Design
Data on the breadth of service profiles were used from two cross-sectional surveys in 28 countries: the 1993 European GP Task Profile study (6321 GPs) and the 2012 QUALICOPC study (6044 GPs). GPs’ involvement in four areas of clinical activity (first contact care, treatment of diseases, medical procedures, and prevention) was established using ecometric analyses. The changes were measured by the relative increase in the breadth of service profiles. Associations between changes and national-level conditions were examined though regression analyses. Data on the national conditions were used from various other public databases including the World Databank and the PHAMEU (Primary Health care Activity Monitor) database.
Setting
A total of 28 European countries.
Subjects
GPs.
Main outcome measure
Changes in the breadth of GP service profiles.
Results
A general trend of increased involvement of European GPs in treatment of diseases and decreased involvement in preventive activities was observed. Conditions at the national level were associated with changes in the involvement of GPs in first contact care, treatment of diseases and, to a limited extent, prevention. Especially in countries with stronger growth of health care expenditures between 1993 and 2012 the service profiles have expanded. In countries where family values are more dominant the breadth in service profiles decreased. A stronger professional status of GPs was positively associated with the change in first contact care.
Conclusions
GPs in former communist countries and Turkey have increased their involvement in the provision of services. Developments in Western Europe were less evident. The developments in the service profiles could only to a very limited extent be explained by national conditions. A main driver of reform seems to be the changes in health care expenditure, which may indicate a notion of urgency because there may be a pressure to curb the rising expenditures.
Key points
Broad GP service profiles are an indicator of strong primary care in a country. It is expected that developments in the breadth of GP service profiles are influenced by various national conditions related to the urgency to reform, politics, and means.
Between 1993 and 2012 the involvement of GPs in European countries in treatment of diseases increased and their involvement preventive activities decreased.
The national conditions were found to be associated with changes in GPs’ involvement as first contact of care, treatment of diseases, and, to a limited extent, prevention.
More specifically, in countries with a stronger growth in health care expenditures, service profiles of European GPs have expanded more in the past decades.
Keywords: General practice, health services research, health policy, primary care, the Netherlands
Introduction
Societal developments and changing health needs have influenced health care and general practice in European countries during the past two decades. Some health care systems have undergone fundamental changes. In the early 1990s, health status and life expectancy in the post-communist countries (hereafter: transitional countries) was very poor and the health care systems were unable to respond effectively.[1–3] Most of these countries chose drastic health sector reforms by introducing primary care with a central role for general practitioners (GPs) coupled with a gradual reduction of the extensive hospital sector.[4–6] They mainly took social insurance systems as examples.[1] In other European countries, rising health expenditures and the increasing complexity of health care needs required adaptations to health care systems.
Based on evidence, the solution to these challenges was sought partly in strengthening primary care, in particular general practice.[5] General practice was expected to increase the efficiency and responsiveness of health care systems when serving as the entry to the system, the focal point for coordination, and dealing with most health problems.[7–10] However, the feasibility and practical implementation of the principles to strengthen and maintain strong primary care varied between countries, as health care systems differed.[4,5,11,12] The extent to which strengthening primary care has been adopted as a solution to the challenges is expected to be visible in the service profiles of GPs. These profiles consist of the range of curative and preventive activities plus the first contact care for their patients.[10,13,14] First contact care concerns the services that address problems for which people will first consult their GP instead of doctors in secondary or hospital care. A broad service package provided by GPs determines the strength of primary care, as a comprehensive service package within primary care indicates a stronger process quality (10).
While stronger primary care could be seen as a common solution, countries have responded differently to challenges and developments. Reasons for this must not only be sought in the variation in health care systems, but also in the different social and political contexts. Implementation of measures to strengthen primary care depends on the “will” and the “means” to address problems.[15,16] The greater the urgency of a problem, the greater the political will to put it on the policy agenda.[15,17] For example, the decrease in life expectancy in the transitional countries just after the fall of communism created an urgency to put a complete health care system reform on the agenda. The increasing costs of health care in Western countries also created an urgency to counteract these increases by, for example, strengthening primary care. The will to address a problem is also likely to be influenced by politics through, for instance, the political composition of governments.[15] Strong primary care does not just emerge spontaneously, but requires an interventionist policy.[18] Left-wing governments favour greater state intervention than right-wing and liberal governments.[15]
Furthermore, the means of a country determines its ability to implement a policy successfully. For example, a government that functions more effectively will be better able to implement a health policy.[15,17] In a more centralized health care system, the government may also be able to steer, more effectively, health care providers towards stronger primary care. A stronger professional status, consisting of, for example, the creation of an association and the establishment of specialized education, is expected to influence GP service profiles positively. In these countries, the tools are provided to offer services, e.g. through education.
Given the above, we pose three questions related to the developments between 1993 and 2012 in 28 European countries:
How has the role of GPs as the doctor of first contact developed?
How has the breadth of the curative and preventive GP service profiles developed?
What conditions, related to the urgency to reform, the political situation, and the means of a country, are associated with the changes in the breadth of GP service profiles?
Material and methods
Data, based on cross-sectional questionnaire surveys among GPs from 28 countries, are derived from the 1993 European Task Profile study (n = 6321 participating GPs) [14] and the 2012 QUALICOPC study (n = 6044 GPs).[19,20] The countries include: Austria, Belgium, Bulgaria, Czech Republic, Denmark, Estonia, Finland, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, the Netherlands, Norway, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey, and the UK. In each country the aim was to reach a representative sample of GPs. Details of the sampling procedures are described elsewhere for 1993 [21] and 2012.[19,22] The questions in the 1993 survey on GP service profiles were repeated in 2012 with the purpose of comparing general practice between the two time points. As question and answering categories were copied either literally or only revised slightly without changing the meaning, the data can be compared.
Breadth of GP service profiles
The questionnaires measured GPs’ activities related to: (1) their role in first contact care; (2) the management and follow-up of a range of acute and chronic conditions; that is, treatment of diseases; (3) minor medical technical procedures; and (4) preventive care. For each of the first three areas, a number of topics were presented and GPs were asked to fill in their involvement on a four-point scale ranging from “never” (1 point), to “almost always or always” (4 points).[14,20] For example, GPs were asked to state to what extent they are involved in the treatment and follow-up of patients with a herniated intervertebral disc lesion and whether an anxious man aged 45 would contact him or her as the first health care provider (for a complete overview of the items included see Appendix 1). Regarding preventive activities, GPs were asked a set of questions related to their systematic involvement in blood pressure and cholesterol measurement and health education (Yes/No).
Scale scores for the breadth of service profiles in the four areas were calculated using ecometric analyses (latent multilevel variable analysis). Details of this approach are presented in Appendix 2. The scores were adjusted for various individual GP and GP practice characteristics and the variance at the GP practice level was taken out. The change between 1993 and 2012 was measured through calculating the relative increase in the breadth of the service profiles compared with 1993. The results of the scale construction are presented in Appendix 2.
Independent variables influencing the breadth of GP service profiles.
The independent variables include indicators related to the urgency of reform, politics, and means. Box 1 outlines these indicators and how they are measured.
Box 1. Operationalization of independent variables.
The urgency of reform is measured by four indicators:
|
The means of a country is measured by the indicators:
|
In the analyses we adjusted for the breadth of the service profiles in 1993. This was because it is expected that the countries with a lower starting point in 1993 have more room for change. We also adjusted for the relative growth in GDP per capita between 1993 and 2012 in order to take into account the differences in wealth between countries. Data on GDP per capita in Purchasing Power Parities (constant 2005 international $) were derived from the World Data Bank.[23] Appendix 3 provides an overview of the values of all dependent variables.
Statistical analyses
Descriptive figures are provided on the changes in the independent variables. The variance between and within countries is analysed using multilevel modelling. The associations between the independent and dependent variables were analysed using linear regression analyses. Independent variables have been added one by one due to the low number of observations (28 countries). Regression coefficients were standardized by transforming all values into betas. Betas above 0.3 are considered to be high, between 0.25 and 0.3 moderately high, and below 0.25 low. Significance largely depends on the number of observations and is therefore less useful in international comparative research. Beta values around 0.30 correspond to p = 0.1. One-tailed p-values were used (p < 0.1). In 1993, GPs in many of the Eastern European countries were at the starting point of developing their service profiles, whereas GPs in many Western European countries already had more developed service profiles. To account for this, in each model the breadth of the service profiles in 1993 was included. Besides, all models were repeated including the relative growth in GDP per capita. The multicollinearity between these and the other variables was tested through calculating inflation factors (VIF). This was done to avoid the correlations between the independent variables that were used in the same models being too high. All VIF values were below 3, indicating that the variables did not interfere with each other. Analyses were performed in Stata version 13.0™ (StataCorp LP, College Station, TX, USA) and MLWin version 2.29 (http://www.bristol.ac.uk/cmm/software/mlwin/).
Results
Changes in the breadth of GP service profiles
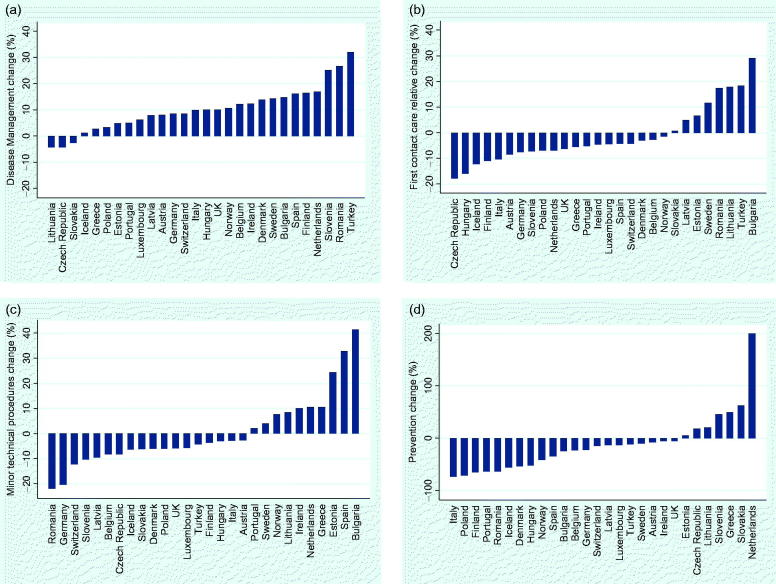
The changes in the breadth of the GP service profiles between 1993 and 2012 are presented in Figure 1(a–d) (detailed figures can be found in Appendix 4).
Figure 1.
a–d. Relative changes in GPs’ service profiles 1993–2014.
Most countries show a decrease in the GP’s role in first contact care. In several transitional countries, Turkey, and Sweden the GP’s role as a doctor of first contact has increased. GPs have become more involved in first contact care for women’s and children’s problems and less for psycho-social issues. In 1993, GPs in most Western European countries had a stronger role as the doctor of first contact care than in most of the transitional countries. In 2012 the distinction between the Western and transitional countries is much less obvious. Service profiles related to treatment of diseases have become broader in almost all countries, except for the Czech Republic, Lithuania, and Slovakia. A significant increase was found in GPs’ involvement in treatment of diseases all over Europe. Minor technical procedures were carried out more frequently in nine countries in 2012 than in 1993. There was a significant fall in both Germany and Romania. The involvement in preventive activities decreased in most countries, though in the Netherlands a strong relative increase was observed.
Conditions associated with changes
Table 1 presents a summary of the results of the relationship between the conditions at the national level and the changes in the breadth of GPs’ service profiles. Beta coefficients and p-values are provided for the national conditions before and after adjustment for the breadth of services in 1993 and the relative increase in GDP. Appendix 5 provides detailed results.
Table 1.
Results regression analyses between independent variables and the relative increase in breadth of service profiles (summary).
| First contact care | Treatment of diseases | Technical Procedures | Prevention | |
|---|---|---|---|---|
| Urgency to reform | ||||
| In-/decrease in life expectancy 1990–1995: | ||||
| Model 1 | ||||
| Life expectancy: Stand. B (p-value) | −0.366 (0.055)* | 0.255 (0.191) | −0.234 (0.231) | −0.066 (0.737) |
| Model 1 + breadth service profiles 1993 | ||||
| Life expectancy: Stand. B (p-value) | −0.218 (0.135) | 0.145 (0.431) | −0.174 (0.393) | −0.082 (0.649) |
| Model 1 + GDP growth | ||||
| Life expectancy: Stand. B (p-value) | −0.139 (0.560) | 0.159 (0.538) | −0.323 (0.217) | −0.024 (0.927) |
| In-/decrease health care expenditure (% GDP): | ||||
| Model 1 | ||||
| Health care expenditure: Stand. B (p-value) | 0.115 (0.562) | 0.432 (0.022)* | −0.014 (0.945) | 0.275 (0.156) |
| Model 1 + breadth service profiles 1993 | ||||
| Health care expenditure: Stand. B (p-value) | 0.315 (0.028)* | 0.339 (0.057)* | 0.060 (0.768) | 0.206 (0.256) |
| Model 1 + GDP growth | ||||
| Health care expenditure: Stand. B (p-value) | 0.364 (0.060)* | 0.397 (0.056)* | 0.021 (0.924) | 0.376 (0.081)* |
| In-/decrease % population > 65 (n = 28): | ||||
| Model 1 | ||||
| Increase in % population > 65: Stand. B (p-value) | 0.072 (0.714) | 0.017 (0.931) | −0.008 (0.969) | 0.078 (0.695) |
| Model 1 + breadth service profiles 1993 | ||||
| Increase in % population > 65: Stand. B (p-value) | −0.131 (0.383) | −0.021 (0.908) | −0.121 (0.573) | 0.229 (0.219) |
| Model 1 + GDP growth | ||||
| Increase in % population > 65: Stand. B (p-value) | −0.091 (0.639) | 0.118 (0.569) | −0.020 (0.925) | 0.057 (0.792) |
| Family orientation (n = 25): | ||||
| Model 1 | ||||
| Family orientation: Stand. B (p-value) | 0.314 (0.126) | −0.201 (0.335) | 0.077 (0.714) | −0.152 (0.469) |
| Model 1 + breadth service profiles 1993 | ||||
| Family orientation: Stand. B (p-value) | −0.347 (0.095)* | −0.451 (0.019)* | −0.270 (0.413) | −0.052 (0.788) |
| Model 1 + GDP growth | ||||
| Family orientation: Stand. B (p-value) | 0.137 (0.535) | −0.079 (0.738) | 0.071 (0.774) | −0.232 (0.340) |
| Politics | ||||
| Left-wing government (n = 27): | ||||
| Model 1 | ||||
| Left-wing government: Stand. B (p-value) | 0.015 (0.941) | 0.224 (0.269) | −0.079(0.661) | 0.023 (0.908) |
| Model 1 + breadth service profiles 1993 | ||||
| Left-wing government: Stand. B (p-value) | 0.138 (0.386) | 0.254 (0.208) | −0.050 (0.755) | 0.178 (0.346) |
| Model 1 + GDP growth | ||||
| Left-wing government: Stand. B (p-value) | 0.075 (0.682) | 0.191 (0.333) | −0.071 (0.733) | 0.034 (0.870) |
| Means | ||||
| Government effectiveness (n = 28): | ||||
| Model 1 | ||||
| Government effectiveness: Stand. B (p-value) | −0.560 (0.002)* | −0.110 (0.577) | −0.099(0.615) | 0.081 (0.683) |
| Model 1 + breadth service profiles 1993 | ||||
| Government effectiveness: Stand. B (p-value) | −0.069 (0.760) | 0.227 (0.293) | 0.176 (0.533) | 0.075 (0.679) |
| Model 1 + GDP growth | ||||
| Government effectiveness: Stand. B (p-value) | −0.470 (0.034)* | −0.434 (0.073)* | −0.089 (0.735) | 0.213 (0.404) |
| Centralization health care system (n = 28): | ||||
| Model 1 | ||||
| Centralization health care system: Stand. B (p-value) | 0.284 (0.143) | −0.091 (0.644) | 0.280 (0.149) | 0.084 (0.669) |
| Model 1 + breadth service profiles 1993 | ||||
| Centralization health care system: Stand. B (p-value) | 0.211 (0.140) | −0.011 (0.953) | 0.249 (0.201) | 0.125 (0.489) |
| Model 1 + GDP | ||||
| Centralization health care system: Stand. B (p-value) | 0.121 (0.543) | 0.017 (0.936) | 0.302 (0.165) | 0.062 (0.781) |
| Professional status of GPs: | ||||
| Model 1 | ||||
| Professional status: Stand. B (p-value) | 0.211 (0.281) | 0.188 (0.337) | −0.009 (0.963) | 0.062 (0.752) |
| Model 1 + breadth service profiles 1993 | ||||
| Professional status: Stand. B (p-value) | 0.259 (0.066)* | 0.251 (0.156) | −0.018 (0.927) | 0.031 (0.867) |
| Model 1 + GDP | ||||
| Professional status: Stand. B (p-value) | 0.142 (0.437) | 0.237 (0.226) | −0.003 (0.987) | 0.050 (0.805) |
*Significant at p < 0.10.
In countries with a stronger decrease in life expectancy during the early 1990s, there has been a stronger relative increase in GPs’ involvement in first contact care. However, this association disappeared after adjusting for the breadth of services in 1993 and after adjusting for the increase in GDP. Furthermore, it is found that, in countries with a higher increase in health care expenditures between 1993 and 2012, GPs’ involvement in first contact care and in treatment of diseases increased. An increase in health care expenditure is also found to be associated with a relative increase in prevention, after adjustment for growth in GDP. After adjusting for the breadth of services in 1993, a stronger decrease was found in first contact care and treatment of diseases in countries with a stronger family orientation. Both of these indicators are seen as a condition that may have provided the countries with a stronger urgency to reform towards stronger primary care.
Finally, a moderately high positive association was found between the professional status of GPs and the relative increase in involvement in first contact care, but only after adjusting for the breadth of services in 1993. The professional status of GPs is in this study measured through indicators on the collective organisation of GPs in associations and the strength of family medicine within the medical education system, which may be used as tools to broaden service profiles of GPs in a country. Therefore this indicator is seen as part of the means of a country.
No associations were found between the various conditions and the changes in the application of technical procedures. The hypotheses could not be confirmed for the increase in the elderly population, the political composition of the government, the level of government effectiveness, the centralization of the health care system, and the relative changes observed in GP service profiles.
Discussion
The service profiles of GPs in Europe have developed in various directions during the past two decades. GPs in transitional countries and Turkey have increased their involvement in one or more areas. Considerable changes were observed, indicating that it is possible to reform health services extensively in a country. Although developments in Western Europe were less evident, a general trend of increased involvement of GPs in treatment of diseases and decreased involvement in the other areas, specifically in preventive activities, could be observed. From this study it is not known whether there is less availability of these preventive services in the countries, or if these activities have been taken up by other health care providers.
The conditions related to the “will” and “means” of governments to strengthen primary care were related to changes in the involvement of GPs in first contact care, in treatment of diseases and in prevention. The hypotheses were confirmed for features that are related to the urgency to reform. A strong positive association was found between the increase in health care expenditures and the relative increase in GPs’ service profiles. Policy-makers are most probably under greater pressure when there are financial indications of a problem. In countries with a stronger family orientation the involvement of GPs decreased. The political composition of the countries’ governments was not associated with the change in service profiles. Both findings on left-wing party dominance and family orientation are confirmed by a previous study.[28] Finally, it was confirmed that a stronger professional status of GPs is positively associated with changes in first contact care.
A strong point of this study is that large samples of GPs in many European countries have been surveyed, systematically, regarding the services they deliver. The fact that, in 2012, this has been done in a similar way to what was undertaken in 1993 has provided us with comparative information on the involvement of European GPs during an important period relating to primary health care policy. Associations with various circumstances at a national level could be tested for both 1993 and 2012. Due to the sampling strategy, scale scores at the country level could be constructed in a multilevel model in which GPs are grouped within countries.
A possible weakness is that the samples of two countries are not entirely comparable. The sample of Germany in 1993 concerned only West Germany, but in 2012 covered the whole of a united Germany. In 1993 data were collected for the whole of the UK, while the 2012 sample concerns only part of England. A limitation of the use of the variable on political composition as an indicator for politics in a country is that it does not take into account the stability of governments. Nevertheless, we have also included a composite measure on government effectiveness, which comprises information on the credibility of the government’s commitment to policies.[26] Furthermore, there are many other conditions that we did not measure in this study, but which may also play a role in the changes to GP service profiles. For example, changes in the method of remuneration of GPs may have influenced this. Ideally, we should also have evaluated the interdependence of conditions of will and means,[25] but also the interdependence of the four components of the service profiles. For the latter it could be hypothesized that the increase in one area, e.g. treatment of diseases, may have led to the decrease in another area, e.g. preventive activities. However, the low number of observations (n = 28 countries) makes it possible only to include a maximum of two variables in the analyses at the same time.
This study evaluated changes in the service profiles of GPs in European countries. Even though the countries have been treated as separate units of analysis, it must be noted that European countries are not independent of each other. This is also known as Galton’s problem. Countries border each other, which means that they can influence each other. The countries included are, for the most part, members of the European Union, which may also have influenced developments in health services. Another remaining issue is that this study does not allow us to make causal inferences. As the study concerns a cross-sectional survey, the direction of the associations is not certain.
The results of this study provide insight into changes in service profiles and provide guidance for the development of training programmes for GPs, tailored to the needs of European countries. For example, most European countries show a decrease in the involvement of GPs in preventive activities, which include, for example, the measurement of blood pressure and cholesterol, but also health education. These are important tasks for GPs and so national governments should consider what is behind this and whether this role should be strengthened again. It is not always likely that these tasks are currently carried out by other professionals outside the GP practice.
Furthermore, this study provides more general lessons, which may also be applicable to service reforms in other health care contexts, countries or even in other sectors. It has been found that the changes in GP service profiles are only associated to a limited extent with conditions at the national level. A main driver for reform seems, however, to be health care expenditure. Factors associated with the change of the breadth of GP service profiles are probably also present at the level of the individual GP practice. If a country’s government intends to strengthen the role of GPs, the role of conditions at the practice level needs to be taken into account.
Acknowledgements
The authors thank their partners in the QUALICOPC project for their role throughout the study and their coordination of the data collection; J. De Maeseneer, E. De Ryck, L. Hanssens, A. Van Pottelberge, S. Willems (Belgium); S. Greß, S. Heinemann (Germany); G. Capitani, S. De Rosis, A.M. Murante, S. Nuti, C. Seghieri, M. Vainieri (Italy); D. Rotar Pavlič, I. Švab (Slovenia); D. Kringos (the Netherlands); M. Van den Berg, T. Van Loenen (the Netherlands). The authors would also like to thank the coordinators of the QUALICOPC data collection in each country: K. Hoffmann, M. Maier (Austria); P. Salchev (Bulgaria); B. Seifert, N. Šrámková (Czech Republic); J. Reinholdt Jensen, P. Vedsted (Denmark); M. Lember, K. Põlluste (Estonia); E. Kosunen (Finland); C. Lionis (Greece), I. Rurik (Hungary); J. Heimisdóttir, O. Thorgeirsson (Iceland); C. Collins (Ireland); G. Ticmane (Latvia); S. Macinskas (Lithuania); M Aubart, J. Leners, R. Stein (Luxembourg); T. Bjerve Eide, H. Melbye(Norway); M. Oleszczyk, A. Windak (Poland); L. Pisco (Portugal); D. Farcasanu (Romania); T. Dedeu (Spain); E. Jurgova (Slovakia); C. Björkelund, T. Faresjö (Sweden); T. Bisschoff, N. Senn (Switzerland); M. Akman (Turkey); C. Sirdifield, N. Siriwardena (England). The authors would additionally like to thank all persons who have supported the national coordinators in the data collection in their countries. Finally, the authors would like to thank the coordinators of the data collection of the 1993 GP Task Profile in each country.
Disclosure statement
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Funding information
The QUALICOPC (Quality and Costs of Primary Care in Europe) study has been co-funded by the European Commission under the Seventh Framework Programme (FP7/2007-2013; grant agreement 242141). The 1993 GP Task Profile Study was funded from the EC BIOMED 1 programme (contract no. BMH1-CT92-1636).
Appendix 1.
Appendix 1.
Measurement of first contact role and breadth of service profiles.
| First contact care: | ||||
| In case of the following health problems, to what extent will patients in your practice population (people who normally apply to you for primary medical care) contact you as the first health care provider? (This is only about the first contact, not about further diagnosis or treatment). | (Almost) | Usually | Occasionally | Seldom/always never |
| 1. Child with severe cough | □ | □ | □ | □ |
| 2. Child aged 8 with hearing problem | □ | □ | □ | □ |
| 3. Woman aged 18 asking for oral contraception | □ | □ | □ | □ |
| 4. Man aged 24 with stomach pain | □ | □ | □ | □ |
| 5. Man aged 45 with chest pain | □ | □ | □ | □ |
| 6. Woman aged 50 with a lump in her breast | □ | □ | □ | □ |
| 7. Woman aged 60 with deteriorating vision | □ | □ | □ | □ |
| 8. Woman aged 60 with polyuria | □ | □ | □ | □ |
| 9. Woman aged 60 with acute symptoms of paralysis/paresis | □ | □ | □ | □ |
| 10. Man aged 70 with joint pain | □ | □ | □ | □ |
| 11. Woman aged 75 with moderate memory problems | □ | □ | □ | □ |
| 12. Man aged 35 with sprained ankle | □ | □ | □ | □ |
| 13. Man aged 28 with a first convulsion | □ | □ | □ | □ |
| 14. Anxious man aged 45 | □ | □ | □ | □ |
| 15. Physically abused child aged 13 | □ | □ | □ | □ |
| 16. Couple with relationship problems | □ | □ | □ | □ |
| 17. Woman aged 50 with psycho-social problems | □ | □ | □ | □ |
| 18. Man aged 32 with sexual problems | □ | □ | □ | □ |
| 19. Man aged 52 with alcohol addiction problems | ||||
| Treatment of diseases: | ||||
| To what extent are you involved in the treatment and follow-up of patients in your practice population with the following diagnoses (“practice population” means: people who normally apply to you for primary medical care)? | (Almost) | Usually | Occasionally | Seldom/always never |
| 1. Chronic bronchitis/COPD | □ | □ | □ | □ |
| 2. Hordeolum (Stye) | □ | □ | □ | □ |
| 3. Peptic ulcer | □ | □ | □ | □ |
| 4. Herniated disc lesion | □ | □ | □ | □ |
| 5. Congestive heart failure | □ | □ | □ | □ |
| 6. Pneumonia | □ | □ | □ | □ |
| 7. Peritonsillar abscess | □ | □ | □ | □ |
| 8. Parkinson’s disease | □ | □ | □ | □ |
| 9. Uncomplicated diabetes (type II) | □ | □ | □ | □ |
| 10. Rheumatoid arthritis | □ | □ | □ | □ |
| 11. Depression | □ | □ | □ | □ |
| 12. Myocardial infarction | □ | □ | □ | □ |
| Technical procedures: To what extent are the following activities carried out in your practice population by you, or your staff, and not by a medical specialist? (Practice population means: people normally applying to you for primary medical care). For example, if fundoscopy is almost always done by you, tick that box. | Always/almost | Usually | Occasionally | Seldom/always never |
| 1. Wedge resection of ingrown toenail | □ | □ | □ | □ |
| 2. Removal of sebaceous cyst from the hairy scalp | □ | □ | □ | □ |
| 3. Wound suturing | □ | □ | □ | □ |
| 4. Excision of warts | □ | □ | □ | □ |
| 5. Insertion of IUD | □ | □ | □ | □ |
| 6. Fundoscopy | □ | □ | □ | □ |
| 7 Joint injection | □ | □ | □ | □ |
| 8. Strapping an ankle | □ | □ | □ | □ |
| 9. Cryotherapy (warts) | □ | □ | □ | □ |
| 10.Setting up an intravenous infusion | □ | □ | □ | □ |
| Prevention: | ||||
| When do you, or your staff, measure blood pressure? (More than one answer possible) | □ In connection with relevant clinical conditions | |||
| When do you, or your staff, measure blood cholesterol level? (More than one answer possible) | □ On request | |||
| To what extent are you involved in health education as regards the following topics: (More than one answer possible) | □ Routinely in office contacts with adults (regardless of the reason for visit) | |||
| (1) Smoking | □ In adults invited for this purpose | |||
| (2) Diet | □ In connection with relevant clinical conditions | |||
| (3) Problematic use of alcohol | □ On request | |||
| □ Routinely in office contacts with adults (regardless of the reason for visit) | ||||
| □ In adults invited for this purpose | ||||
| □ No such measures | ||||
| Not involved In connection with In group sessions or normal patient contacts special programmes | ||||
| □ □ □ | ||||
| □ □ □ | ||||
Appendix 2. Explanation and results of the scale construction
Box 1: Explanation of scale construction.
Scale scores on the GP service profiles were computed using the ecometrics approach. This accounts for differences in the number of respondents on which the estimation is based, individual differences in response to certain items, and for dependency among the items that measure the latent variable [29]. In the multilevel model an additional level is added for the related variables, or items, of which the scale is composed. A three- level model was used (items nested within GPs, and GPs nested within countries). A weighted-item average was used for each item to calculate an average scale value. This was done by using the item weights for the fixed effects. Finally, the item variance, an indication of the measurement error, was taken into account [29,30]. Reliability scores for each scale for 1993 and 2012 were calculated and varied between 0.73 and 1.00 at the country level and between 0.61 and 0.97 at the GP practice level.
Reliability of scales at GP practice and country level before adjustment for background characteristics.
| Scale | GP practice level | Country level |
|---|---|---|
| 1. 1993 First contact of care | 0.87 | 0.99 |
| 2. 1993 Treatment of diseases | 0.78 | 0.98 |
| 3. 1993 Technical procedures | 0.77 | 0.99 |
| 4. 1993 Prevention | 0.97 | 0.73 |
| 5. 2012 First contact of care | 0.86 | 0.98 |
| 6. 2012 Treatment of diseases | 0.86 | 0.98 |
| 7. 2012 Technical procedures | 0.75 | 1.00 |
| 8. 2012 Prevention | 0.61 | 0.97 |
Table 2.
Results of multilevel regression analyses after adjustment for background characteristics.
| Model: First contact care ni = 32*; nj = 12 534 | Model: Treatment of diseases ni = 32*; nj = 12 493 | Model: technical procedures ni = 32*; nj = 12 374 | Model: Prevention ni = 32*; nj = 12 559 | |
|---|---|---|---|---|
| Cons | 2.985 (0.069) | 2.973 (0.042) | 2.105 (0.107) | 0.245 (0.018) |
| Year (2012) | −0.089 (0.056) | 0.278 (0.043) | −0.017 (0.050) | −0.054 (0.019) |
| Age | −0.001 (0.000) | 0.002 (0.000) | −0.001 (0.000) | 0.000 (0.000) |
| Sex (Female) | −0.011 (0.009) | −0.036 (0.008) | −0.152 (0.009) | −0.003 (0.003) |
| Practice location:** | −0.163 (0.012) | −0.096 (0.011) | −0.260 (0.013) | −0.003 (0.005) |
| – Big (inner) city | −0.137 (0.011) | −0.069 (0.010) | −0.203 (0.011) | −0.002 (0.004) |
| – Suburbs/small town | −0.069 (0.012) | −0.038 (0.011) | −0.070 (0.013) | 0.011 (0.005) |
| – Mixed urban/rural | −0.003 (0.009) | −0.011 (0.009) | 0.054 (0.010) | −0.003 (0.004) |
| Duo/group practice*** | ||||
| Variance within countries: | ||||
| 1993 | 0.177 (0.003) | 0.139 (0.002) | 0.196 (0.003) | 0.044 (0.001) |
| 2012 | 0.176 (0.003) | 0.172 (0.003) | 0.173 (0.003) | 0.019 (0.000) |
| Variance between countries: | ||||
| 1993 | 0.215 (0.044) | 0.092 (0.020) | 0.684 (0.125) | 0.013 (0.003) |
| 2012 | 0.159 (0.033) | 0.115 (0.024) | 0.679 (0.124) | 0.014 (0.003) |
| ICC: | ||||
| 1993 | 54.8% | 39.7% | 77.7% | 23.3% |
| 2012 | 47.6% | 40.0% | 79.7% | 41.2% |
| Correlation coefficient of countries between years | 0.633 | 0.606 | 0.907 | 0.444 |
*Scales were constructed on the basis of the larger datasets including four extra European countries. However, in the main analyses four countries were taken out as these were only included in one of the two years.
**Reference category = rural practice location.
***Reference category = solo practice. Bold = significant at p < 0.05; ni = country; nj = general practitioners. Reference category for practice location is “Rural”; ICC = intraclass correlation.
Appendix 3. Overview of independent variables
| Country | In-/decrease in life expectancy ‘90 –‘95 | In-/decrease HC expenditure (% GDP) 199 –2012 | In-/decrease % population > 65 1993–2012 | Family orientation* | Left-wing government** | Government effectiveness*** | Centralization HC system**** | Professional status of GPs***** | Increase in GDP per capita 1993–2012 |
|---|---|---|---|---|---|---|---|---|---|
| Austria | 0.31 | 1.88 | 3.07 | 46.06 | 5.75 | 1.86 | 0 | 2.00 | 38.25 |
| Belgium | 0.21 | 3.18 | 1.96 | 37.95 | 8.25 | 1.81 | 0 | 2.75 | 28.54 |
| Bulgaria | –0.16 | 2.18 | 4.55 | 79.59 | 4.25 | –0.31 | 1 | 2.75 | 88.05 |
| Czech Republic | 0.47 | 0.97 | 3.15 | 65.04 | 6.25 | 0.62 | 0 | 2.50 | 65.01 |
| Denmark | 0.11 | 3.07 | 2.00 | 21.97 | 6.25 | 1.91 | 0 | 2.75 | 24.28 |
| Estonia | –0.55 | –0.38 | 5.08 | 59.52 | 5.00 | 0.57 | 1 | 3.00 | 135.85 |
| Finland | 0.42 | 1.30 | 4.42 | 31.12 | 7.00 | 1.42 | 0 | 3.00 | 55.21 |
| Germany | 0.33 | 1.17 | 5.85 | 53.78 | 9.00 | 1.84 | 0 | 2.50 | 29.42 |
| Greece | 0.17 | 0.68 | 4.81 | 86.26 | 11.75 | 0.82 | 0 | 2.50 | 21.80 |
| Hungary | 0.14 | 0.50 | 3.00 | 70.18 | 10.00 | 0.84 | 0 | 3.00 | 52.64 |
| Iceland | –0.01 | 0.86 | 1.53 | . | 3.50 | 1.80 | 1 | 2.00 | 40.68 |
| Ireland | 0.22 | 1.52 | 0.27 | 41.74 | 3.25 | 1.71 | 1 | 3.00 | 10.65 |
| Italy | 0.31 | 2.11 | 4.81 | 50.89 | 4.50 | 0.82 | 0 | 2.50 | 9.51 |
| Latvia | –0.84 | 0.22 | 5.64 | 70.55 | 5.25 | 0.19 | 1 | 2.50 | 169.32 |
| Lithuania | –0.61 | 1.28 | 3.93 | 74.17 | 8.50 | 0.32 | 1 | 3.00 | 140.43 |
| Luxembourg | 0.40 | 1.29 | 0.36 | 45.28 | 6.50 | 2.05 | 0 | 2.00 | 41.27 |
| Netherlands | 0.14 | 4.11 | 3.40 | 22.81 | 6.25 | 2.01 | 0 | 3.00 | 35.02 |
| Norway | 0.31 | 0.44 | –0.68 | . | 10.25 | 2.02 | 0 | 3.00 | 36.14 |
| Poland | 0.28 | 1.24 | 3.33 | 84.38 | 7.00 | 0.78 | 0 | 3.00 | 128.22 |
| Portugal | 0.36 | 1.93 | 4.04 | 57.96 | 7.75 | 1.15 | 0 | 3.00 | 25.37 |
| Romania | –0.08 | 1.89 | 3.52 | 78.62 | 9.50 | –0.51 | 0 | 3.00 | 77.39 |
| Slovakia | 0.37 | 1.74 | 2.02 | 74.91 | 5.75 | 0.57 | 0 | 2.50 | 119.33 |
| Slovenia | 0.21 | 1.30 | 5.43 | 45.21 | 9.50 | 0.89 | 1 | 3.00 | 66.34 |
| Spain | 0.30 | 2.17 | 2.81 | 57.80 | 10.00 | 1.62 | 0 | 2.00 | 32.18 |
| Sweden | 0.31 | 1.65 | 1.28 | 14.82 | 12.00 | 1.96 | 0 | 3.00 | 52.25 |
| Switzerland | 0.30 | 1.96 | 2.82 | . | 4.50 | 1.91 | 0 | 3.00 | 19.40 |
| Turkey | 0.83 | 2.93 | 2.42 | 81.92 | . | –0.01 | 0 | 2.50 | 56.25 |
| UK | 0.25 | 2.68 | 1.34 | 44.58 | 13.00 | 1.88 | 1 | 2.50 | 41.64 |
*% Pop. prefers offspring to take care of one or both parents in case of ill health (2007).
**Weighted years left party dominance between 1995 and 2012.
***Mean of the scores between 1996 and 2011.
****1 = centralized, 0 = decentralized.
*****Measured on a scale between 1 and 3 (2009/10). = Missing value.
Appendix 4. Breadth of GP service profiles and relative changes between 1993 and 2012
| First contact care GP |
Treatment of diseases |
Technical procedures |
Prevention |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1993* | 2012 | Relative change | 1993 | 2012 | Relative change | 1993 | 2012 | Relative change | 1993 | 2012 | Relative change (%) | |
| Austria | 3.05 | 2.79 | −8.6% | 3.08 | 3.33 | 8.0% | 2.14 | 2.08 | −2.7% | 0.33 | 0.3 | −7.8% |
| Belgium | 3.1 | 3.01 | −2.9% | 2.97 | 3.33 | 12.2% | 2.57 | 2.35 | −8.4% | 0.22 | 0.17 | −23.5% |
| Bulgaria | 2.31 | 2.98 | 29.0% | 2.76 | 3.17 | 14.7% | 1.31 | 1.86 | 41.5% | 0.28 | 0.21 | −25.4% |
| Czech Rep. | 2.99 | 2.45 | −18.0% | 2.83 | 2.71 | −4.3% | 1.62 | 1.49 | −8.3% | 0.19 | 0.23 | 18.2% |
| Denmark | 3.5 | 3.39 | −3.2% | 3.11 | 3.54 | 13.8% | 2.73 | 2.57 | −6.1% | 0.15 | 0.07 | −53.6% |
| Estonia | 2.58 | 2.75 | 6.6% | 3.09 | 3.24 | 4.9% | 1.35 | 1.68 | 24.5% | 0.26 | 0.28 | 5.2% |
| Finland | 3.06 | 2.73 | −11.0% | 2.82 | 3.28 | 16.5% | 3.47 | 3.34 | −3.7% | 0.22 | 0.08 | −65.5% |
| Germany | 3.05 | 2.82 | −7.6% | 3.19 | 3.46 | 8.4% | 2.29 | 1.82 | −20.5% | 0.46 | 0.36 | −22.8% |
| Greece | 2.79 | 2.64 | −5.5% | 2.92 | 3 | 2.7% | 2.13 | 2.36 | 10.7% | 0.23 | 0.35 | 49.6% |
| Hungary | 3.22 | 2.7 | −16.1% | 3.04 | 3.34 | 10.1% | 1.45 | 1.41 | −2.9% | 0.31 | 0.15 | −52.2% |
| Iceland | 3.11 | 2.73 | −12.3% | 2.96 | 3 | 1.2% | 3.11 | 2.91 | −6.5% | 0.22 | 0.1 | −56.7% |
| Ireland | 3.41 | 3.25 | −4.7% | 3.2 | 3.59 | 12.3% | 2.40 | 2.65 | 10.0% | 0.21 | 0.2 | −6.3% |
| Italy | 3.22 | 2.88 | −10.5% | 3.06 | 3.36 | 9.8% | 1.48 | 1.44 | −2.8% | 0.25 | 0.07 | −73.6% |
| Latvia | 2.54 | 2.66 | 4.8% | 3 | 3.24 | 7.9% | 1.71 | 1.54 | −9.5% | 0.18 | 0.16 | −14.1% |
| Lithuania | 2.68 | 3.16 | 17.8% | 3.11 | 2.97 | −4.4% | 1.33 | 1.45 | 8.5% | 0.25 | 0.31 | 20.0% |
| Luxembourg | 2.8 | 2.68 | −4.4% | 2.92 | 3.1 | 6.2% | 2.19 | 2.07 | −5.7% | 0.18 | 0.15 | −13.3% |
| Netherlands | 3.60 | 3.35 | −7.0% | 2.86 | 3.34 | 16.9% | 2.94 | 3.25 | 10.6% | 0.05 | 0.14 | 199.7% |
| Norway | 3.27 | 3.22 | −1.5% | 3.18 | 3.52 | 10.6% | 2.89 | 3.11 | 7.7% | 0.19 | 0.11 | −41.6% |
| Poland | 2.85 | 2.65 | −7.0% | 3.11 | 3.21 | 3.3% | 1.46 | 1.37 | −6.1% | 0.26 | 0.07 | −71.6% |
| Portugal | 3.22 | 3.05 | −5.4% | 3.14 | 3.3 | 5.1% | 1.75 | 1.79 | 2.0% | 0.45 | 0.16 | −64.3% |
| Romania | 2.45 | 2.88 | 17.3% | 2.62 | 3.32 | 26.7% | 1.92 | 1.49 | −22.1% | 0.34 | 0.12 | −63.9% |
| Slovakia | 2.59 | 2.61 | 0.7% | 2.68 | 2.61 | −2.7% | 1.48 | 1.39 | −6.2% | 0.15 | 0.25 | 62.0% |
| Slovenia | 3.24 | 3.01 | −7.3% | 2.92 | 3.65 | 25.2% | 1.98 | 1.77 | −10.4% | 0.25 | 0.36 | 45.4% |
| Spain | 3.32 | 3.18 | −4.3% | 3.03 | 3.52 | 16.2% | 1.72 | 2.28 | 32.9% | 0.35 | 0.23 | −35.5% |
| Sweden | 3.04 | 3.4 | 11.6% | 3.11 | 3.56 | 14.3% | 2.89 | 3.00 | 4.0% | 0.14 | 0.13 | −10.5% |
| Switzerland | 3.02 | 2.9 | −4.2% | 3.16 | 3.43 | 8.4% | 2.9 | 2.54 | −12.2% | 0.27 | 0.23 | −15.8% |
| Turkey | 2.07 | 2.45 | 18.4% | 2.11 | 2.78 | 32.0% | 1.88 | 1.79 | −4.3% | 0.1 | 0.09 | −12.1% |
| UK/England | 3.5 | 3.27 | −6.4% | 3.25 | 3.57 | 10.1% | 2.79 | 2.62 | −5.9% | 0.43 | 0.4 | −6.1% |
*Breadth of services is measured at a scale from 1 to 4. Germany: the 1993 sample included only West Germany while the 2012 sample includes a sample from the whole of Germany. UK/England: the 2012 sample included practices from the UK and the 1993 sample only from England
Appendix 5. Outcomes regression analyses, detailed
| First contact care | Treatment of diseases | Technical Procedures | Prevention | |
|---|---|---|---|---|
| Urgency of reform | ||||
| In-/decrease in life expectancy 1990–1995: | ||||
| Model 1 | ||||
| Life expectancy: Stand. B (p-value) | −0.366 (0.055)* | 0.255 (0.191) | −0.234 (0.231) | −0.066 (0.737) |
| R2 | 0.134 | 0.065 | 0.055 | 0.004 |
| Model 1 + breadth service profiles 1993 | ||||
| Life expectancy: Stand. B (p-value) | −0.218 (0.135) | 0.145 (0.431) | −0.174 (0.393) | −0.082 (0.649) |
| Breadth service profiles 1993: Stand. B (p-value) | −0.645 (0.000)* | −0.424 (0.028)* | −0.201 (0.323) | −0.451 (0.018)* |
| R2 | 0.528 | 0.233 | 0.092 | 0.208 |
| Model 1 + GDP | ||||
| Life expectancy: Stand. B (p-value) | −0.139 (0.560) | 0.159 (0.538) | −0.323 (0.217) | −0.024 (0.927) |
| Increase in GDP: Stand. B (p-value) | 0.347 (0.154) | −0.146 (0.569) | −0.138 (0.595) | 0.064 (0.890) |
| R2 | 0.203 | 0.077 | 0.066 | 0.007 |
| In-/Decrease health care expenditure (% GDP): | ||||
| Model 1 | ||||
| Health care expenditure: Stand. B (p-value) | 0.115 (0.562) | 0.432 (0.022)* | −0.014 (0.945) | 0.275 (0.156) |
| R2 | 0.013 | 0.187 | 0.000 | 0.076 |
| Model 1 + breadth service profiles 1993 | ||||
| Health care expenditure: Stand. B (p-value) | 0.315 (0.028)* | 0.339 (0.057)* | 0.060 (0.768) | 0.206 (0.256) |
| Breadth service profiles 1993: Stand. B (p-value) | −0.776 (0.000)* | −0.378 (0.035)* | −0.269 (0.192) | −0.413 (0.028)* |
| R2 | 0.575 | 0.321 | 0.067 | 0.242 |
| Model 1 + GDP | ||||
| Health care expenditure: Stand. B (p-value) | 0.364 (0.060)* | 0.397 (0.056)* | 0.021 (0.924) | 0.376 (0.081) |
| Increase in GDP: Stand. B (p-value) | 0.591 (0.004)* | −0.083 (0.679) | 0.083 (0.710) | 0.239 (0.259) |
| R2 | 0.301 | 0.192 | 0.006 | 0.123 |
| % population > 65 (n = 28): | ||||
| Model 1 | ||||
| Increase in % population > 65: Stand. B (p-value) | 0.072 (0.714) | 0.017 (0.931) | −0.008 (0.969) | 0.078 (0.695) |
| R2 | 0.005 | 0.000 | 0.000 | 0.006 |
| Model 1 + breadth service profiles 1993 | ||||
| Increase in % population > 65: Stand. B (p-value) | −0.131 (0.383) | −0.021 (0.908) | −0.121 (0.573) | 0.229 (0.219) |
| Breadth service profiles 1993: Stand. B (p-value) | −0.731 (0.000)* | −0.463 (0.015)* | −0.304 (0.164) | −0.515 (0.009)* |
| R2 | 0.499 | 0.213 | 0.076 | 0.249 |
| Model 1 + GDP | ||||
| Increase in % population > 65: Stand. B (p-value) | −0.091 (0.639) | 0.118 (0.569) | −0.020 (0.925) | 0.057 (0.792) |
| Increase in GDP: Stand. B (p-value) | 0.470 (0.021)* | −0.291 (0.168) | 0.081 (0.706) | 0.061 (0.778) |
| R2 | 0.135 | 0.075 | 0.006 | 0.009 |
| Family orientation (n = 25): | ||||
| Model 1 | ||||
| Family orientation: Stand. B (p-value) | 0.314 (0.126) | −0.201 (0.335) | 0.077 (0.714) | −0.152 (0.469) |
| R2 | 0.099 | 0.040 | 0.006 | 0.023 |
| Model 1 + breadth service profiles 1993 | −0.347 (0.095)* | −0.451 (0.019)* | −0.270 (0.413) | −0.052 (0.788) |
| Family orientation: Stand. B (p-value) | ||||
| Breadth service profiles 1993: Stand. B (p-value) | −0.946 (0.000)* | −0.653 (0.001)* | −0.447 (0.181) | −0.470 (0.022)* |
| R2 | 0.556 | 0.404 | 0.085 | 0.234 |
| Model 1 + GDP | ||||
| Family orientation: Stand. B (p-value) | 0.137 (0.535) | −0.079 (0.738) | 0.071 (0.774) | −0.232 (0.340) |
| Increase in GDP: Stand. B (p-value) | 0.365 (0.109) | −0.252 (0.291) | 0.013 (0.958) | 0.166 (0.493) |
| R2 | 0.200 | 0.089 | 0.006 | 0.044 |
| Politics | ||||
| Left-wing government (n = 27): | ||||
| Model 1 | ||||
| Left-wing government: Stand. B (p-value) | 0.015 (0.941) | 0.224 (0.269) | −0.079 (0.661) | 0.023 (0.908) |
| R2 | 0.000 | 0.050 | 0.006 | 0.001 |
| Model 1 + breadth service profiles 1993 | ||||
| Left-wing government: Stand. B (p-value) | 0.138 (0.386) | 0.254 (0.208) | −0.050 (0.803) | 0.178 (0.346) |
| Breadth service profiles 1993 | −0.667 (0.000)* | −0.208 (0.300) | −0.254 (0.212) | −0.521 (0.010)* |
| R2 | 0.431 | 0.092 | 0.070 | 0.249 |
| Model 1 + GDP | ||||
| Left-wing government: Stand. B (p-value) | 0.075 (0.682) | 0.191 (0.333) | −0.071 (0.733) | 0.034 (0.870) |
| Increase in GDP: Stand. B (p-value) | 0.481 (0.014)* | −0.258 (0.195) | 0.065 (0.755) | 0.084 (0.684) |
| R2 | 0.228 | 0.116 | 0.010 | 0.008 |
| Means | ||||
| Government effectiveness (n = 28): | ||||
| Model 1 | ||||
| Government effectiveness: Stand. B (p-value) | −0.560 (0.002)* | −0.110 (0.577) | −0.099 (0.615) | 0.081 (0.683) |
| R2 | 0.314 | 0.012 | 0.010 | 0.007 |
| Model 1 + breadth service profiles 1993 | ||||
| Government effectiveness: Stand. B (p-value) | −0.069 (0.760) | 0.227 (0.293) | 0.176 (0.533) | 0.075 (0.679) |
| Breadth service profiles 1993 | −0.642 (0.008)* | −0.591 (0.010)* | −0.380 (0.184) | −0.447 (0.019)* |
| R2 | 0.485 | 0.248 | 0.079 | 0.206 |
| Model 1 + GDP | ||||
| Government effectiveness: Stand. B (p-value) | −0.470 (0.034)* | −0.434 (0.073)* | −0.089 (0.735) | 0.213 (0.404) |
| Increase in GDP: Stand. B (p-value) | 0.145 (0.494) | −0.521 (0.034)* | −0.020 (0.938) | 0.213 (0.404) |
| R2 | 0.327 | 0.178 | 0.010 | 0.034 |
| Centralization health care system (n = 28): | ||||
| Model 1 | ||||
| Centralization health care system: Stand. B (p-value) | 0.284 (0.143) | −0.091 (0.644) | 0.280 (0.149) | 0.084 (0.669) |
| R2 | 0.081 | 0.008 | 0.078 | 0.007 |
| Model 1 + breadth service profiles 1993 | ||||
| Centralization health care system: Stand. B (p-value) | 0.211 (0.140) | −0.011 (0.953) | 0.249 (0.201) | 0.125 (0.489) |
| Breadth service profiles 1993 | −0.672 (0.000)* | −0.460 (0.017)* | −0.217 (0.261) | −0.459 (0.016)* |
| R2 | 0.527 | 0.213 | 0.125 | 0.216 |
| Model 1 + GDP | ||||
| Centralization health care system: Stand. B (p-value) | 0.121 (0.543) | 0.017 (0.936) | 0.302 (0.165) | 0.062 (0.781) |
| Increase in GDP: Stand. B (p-value) | 0.387 (0.060)* | −0.258 (0.239) | −0.053 (0.803) | 0.054 (0.807) |
| R2 | 0.204 | 0.063 | 0.081 | 0.010 |
| Professional status of GPs: | ||||
| Model 1 | ||||
| Professional status: Stand. B (p-value) | 0.211 (0.281) | 0.188 (0.337) | −0.009 (0.963) | 0.062 (0.752) |
| R2 | 0.045 | 0.035 | 0.000 | 0.004 |
| Model 1 + breadth service profiles 1993 | ||||
| Professional status: Stand. B (p-value) | 0.259 (0.066)* | 0.251 (0.156) | −0.018 (0.927) | 0.031 (0.865) |
| Breadth service profiles 1993 | −0.712 (0.000)* | −0.493 (0.008)* | −0.253 (0.202) | −0.446 (0.020)* |
| R2 | 0.550 | 0.117 | 0.064 | 0.202 |
| Model 1 + GDP | ||||
| Professional status: Stand. B (p-value) | 0.142 (0.437) | 0.237 (0.226) | −0.003 (0.987) | 0.050 (0.805) |
| Increase in GDP: Stand. B (p-value) | 0.414 (0.030)* | −0.290 (0.141) | 0.074 (0.716) | 0.072 (0.725) |
| R2 | 0.212 | 0.117 | 0.006 | 0.009 |
*Significant at p < 0.1.
References
- [1].Marrée J, Groenewegen PP.. Back to Bismarck: Eastern European health care systems in transition. Aldershot: Avebury; 1997. [Google Scholar]
- [2].Saltman RB, Figueras J.. European health care reform: Analysis of current strategies. Copenhagen: WHO Regional Office for Europe; 1997. [Google Scholar]
- [3].McKee M, Healy J, Falkingham J.. Health care in central Asia. Buckingham: Open University Press; 2002. [Google Scholar]
- [4].Boerma WGW, Dubois CA.. Mapping primary care across Europe In: Saltman RB, Rico A, Boerma WGW, editors. Primary care in the driver’s seat? Organizational reform in European primary care. European Observatory on Health Systems and Policies Series. Maidenhead: Open University Press; 2006. p 22–47. [Google Scholar]
- [5].Groenewegen PP, Dourgnon P, Greß S, et al.. Strengthening weak primary care systems: Steps towards stronger primary care in selected western and eastern European countries. Health Policy. 2013:170–179. [DOI] [PubMed] [Google Scholar]
- [6].Seifert B, Svab I, Madis T, et al. Perspectives of family medicine in Central and Eastern Europe. Fam Pract 2008;25:113–118. [DOI] [PubMed] [Google Scholar]
- [7].Starfield B, Shi L, Macinko J.. Contribution of primary care to health systems and health. Milbank Q 2005;83:457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Delnoij D, Van MG, Paulus A, Groenewegen P.. Does general practitioner gatekeeping curb health care expenditure? J Health Serv Res Policy 2000;5:22–26. [DOI] [PubMed] [Google Scholar]
- [9].Shi L, Starfield B, Politzer R, Regan J.. Primary care, self-rated health, and reductions in social disparities in health. Health Serv Res 2002;37:529–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kringos DS, Boerma WG, Hutchinson A, et al.. The breadth of primary care: A systematic literature review of its core dimensions. BMC Health Serv Res 2010;10:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Boerma WGW, Rico A.. Changing conditions for structural reform in primary care In: Saltman RB, Rico A, Boerma WGW, editors. Primary care in the driver’s seat? Organizational reform in European primary care. Maidenhead: Open University Press; 2006. p 50–67. [Google Scholar]
- [12].Rico A, Saltman RB, Boerma WGW.. Organizational restructuring in European health systems: The role of primary care. Social Policy and Administration 2003;37:592–608. [Google Scholar]
- [13].Grielen SJ, Boerma WGW, Groenewegen PP.. Unity or diversity? Task profiles of general practitioners in Central and Eastern Europe. Eur J Public Health 2000:249–254. [Google Scholar]
- [14].Boerma WG, Van der Zee J, Fleming DM.. Service profiles of general practitioners in Europe. European GP Task Profile Study. Br J Gen Pract 1997;47:481–486. [PMC free article] [PubMed] [Google Scholar]
- [15].McKee M, Mackenbach JP.. The will and the means to implement health policies In: Mackenbach JPM, M, editor. Successes and failures of health policy in Europe: Four decades of divergent trends and converging challenges. Maidenhead: Open University Press; 2013. p 66–77. [Google Scholar]
- [16].Mackenbach JP, McKee M.. A comparative analysis of health policy performance in 43 European countries. Eur J Public Health 2013;23:195–201. [DOI] [PubMed] [Google Scholar]
- [17].Kingdon J. Agendas, alternatives and public policies. Boston, MA: Little Brown; 1984. [Google Scholar]
- [18].Groenewegen PP, Dixon J, Boerma WGW.. The regulatory environment of general practice: An international perspective In: Saltman RB, Busse R, Mossialos E, editors. Regulating entrepreneurial behaviour in European health care systems. Buckingham and Philadelphia: Open University Press; 2002. [Google Scholar]
- [19].Schäfer WLA, Boerma WG, Kringos DS, et al. QUALICOPC, a multi-country study evaluating quality, costs and equity in primary care. BMC Fam Pract 2011;12:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Schäfer WLA, Boerma WGW, Kringos DS, et al. Measures of quality, costs and equity in primary health care: Instruments developed to analyse and compare primary health care in 35 countries. Qual Prim Care 2013;21:67–79. [PubMed] [Google Scholar]
- [21].Boerma WGW. Profiles of general practice in Europe: An international study of variation in the tasks of general practitioners. PhD thesis, Utrecht; 2003. [Google Scholar]
- [22].Groenewegen PP; Greß S; Schäfer WLA.. Participation of general practitioners in a large multi-country combined general practitioner: Patient survey. Paper to be submitted; 2014. [Google Scholar]
- [23].World Databank [Internet]. 2014. [cited 10 March 2014]. Website: http://databank.worldbank.org/data/home.aspx- Accessed on 6 May 2014
- [24].TNS Opinion & Social & TNS Special eurobarometer 283 health and long-term care in the European Union. Brussels: European Commission; 2007. [Google Scholar]
- [25].Armingeon KC, R, Knöpfel L, Weisstanner D, et al. . Comparative Political Data Set III 1990–2011. In: Institute of Political Science UoB, editor. Berne; 2013. [Google Scholar]
- [26].Teorell JC, N, Dahlberg S, Holmberg S, et al. . The Quality of Government Basic Dataset made from “The Quality of Government Dataset, version 15 May 13”. University of Gothenburg, Quality of Government Institute, editor. 2013. [Google Scholar]
- [27].Kringos DS, Boerma WG, Bourgueil Y, et al. The European primary care monitor: Structure, process and outcome indicators. BMC Fam Pract 2010;11:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kringos DS, Boerma WGW, Van der Zee J, Groenewegen PP.. Political, cultural and economic foundations of primary care in Europe. Soc Sci Med 2013;99. [DOI] [PubMed] [Google Scholar]
- [29].Raudenbush SW; Sampson RJ.. Ecometrics: Toward a science of assessing ecological settings, with application to the systematic social observation of neighborhoods. Sociological Methodology 1999;29:1–41. [Google Scholar]
- [30].Van Schoten SB, RJ, Spreeuwenberg P, de Bruijne C, et al. The ecometric properties of a measurement instrument for prospective risk analysis in hospital departments. BMC Health Serv Res 2014;14(103). [DOI] [PMC free article] [PubMed] [Google Scholar]