Abstract
Background
In renal biopsy reporting, quantitative measurements, such as glomerular number and percentage of globally sclerotic glomeruli, is central to diagnostic accuracy and prognosis. The aim of this study is to determine the number of glomeruli and percent globally sclerotic in renal biopsies by means of registration of serial tissue sections and manual enumeration, compared to the numbers in pathology reports from routine light microscopic assessment.
Design
We reviewed 277 biopsies from the Nephrotic Syndrome Study Network (NEPTUNE) digital pathology repository, enumerating 9,379 glomeruli by means of whole slide imaging. Glomerular number and the percentage of globally sclerotic glomeruli are values routinely recorded in the official renal biopsy pathology report from the 25 participating centers. Two general trends in reporting were noted: total number per biopsy or average number per level/section. Both of these approaches were assessed for their accuracy in comparison to the analogous numbers of annotated glomeruli on WSI.
Results
The number of glomeruli annotated was consistently higher than those reported (p<0.001); this difference was proportional to the number of glomeruli. In contrast, percent globally sclerotic were similar when calculated on total glomeruli, but greater in FSGS when calculated on average number of glomeruli (p<0.01). The difference in percent globally sclerotic between annotated and those recorded in pathology reports was significant when global sclerosis is greater than 40%.
Conclusions
Although glass slides were not available for direct comparison to whole slide image annotation, this study indicates that routine manual light microscopy assessment of number of glomeruli is inaccurate, and the magnitude of this error is proportional to the total number of glomeruli.
Introduction
The morphologic assessment of renal biopsies is a well-established practice and provides important diagnostic and prognostic information. Standardized assessment and reporting for these specimens is essential [1]. Although most renal biopsy diagnoses are dependent on qualitative features, semi-quantitative metrics are routinely applied for prognostic measures and treatment decisions. Semi-quantitative approaches were first introduced in lupus nephritis and emphasized the detailed evaluation of all lesions in glomerular and tubulointerstitial compartments [2–4]. Subsequently, similar approaches to systematic semi-quantitative biopsy interpretation have been applied to other renal diseases [5–9]. Thus, accuracy in reporting quantitative and semiquantitative values is emphasized by consensus papers for routine renal pathology reporting [1, 10]. Renal pathologists report glomerular numbers in renal biopsies utilizing various approaches, including a) attempting assessment of the total number of glomeruli by looking at all sections available, b) averaging the number of glomeruli per section either counting all glomeruli in each levels as individual glomeruli, or by using the level with the most and the least, c) providing a range using the sections with the least and the most glomeruli. It is, however, appreciated that there are technical limitations independent of the individual pathologists experience and accuracy.
The Nephrotic Syndrome Study Network (NEPTUNE) implemented a digital pathology repository (DPR) that includes whole slide images (WSI) of all kidney biopsy levels available for each case and a copy of the de-identified pathology report [11]. The NEPTUNE digital pathology protocol (NDPP), by application of glomerular annotation in discontinuous but sequential sections, sought to standardize reporting metrics by refining accuracy. The annotation and enumeration of glomeruli in all available WSI sections enables not only the estimation of the overall number of glomeruli, but also of affected glomeruli by any parameter of choice [12].
Here, we applied WSI and annotation software to evaluate the most basic quantitative metrics: total number of glomeruli and number/percentage of globally sclerotic glomeruli. Additionally, by comparing the digital quantitative analysis to the manual light microscopy (LM) analysis as routinely reported, we test its potential value in improving clinical practice.
Methods
NEPTUNE DPR and case selection
Renal biopsies are an enrollment criteria of the NEPTUNE study (ClinicalTrials.gov Identifier: NCT01240564). All patients were consented at enrollment, and the study was approved by Institutional Review Boards of all participating institutions (http://www.rarediseasesnetwork.org/cms/neptune).
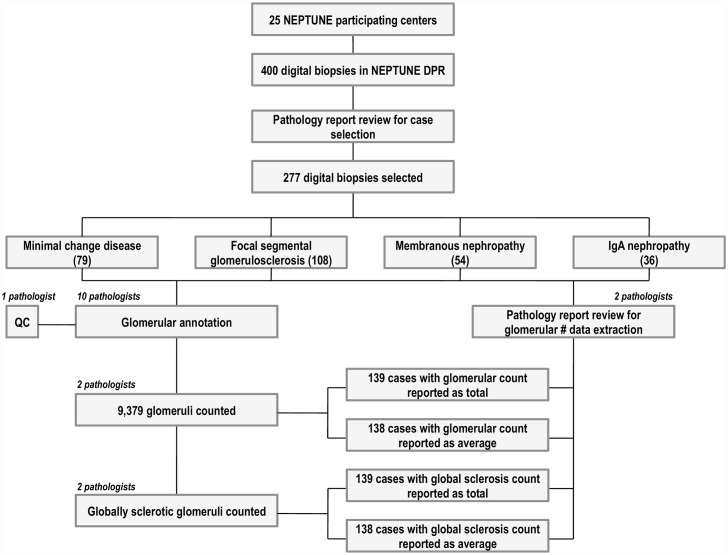
According to the NEPTUNE protocol, all renal biopsies are digitized and together with the de-identified PDF of the pathology report, stored in the NEPTUNE DPR [11, 13]. From a total of 392 digital renal biopsies, 317 cases with a diagnosis of minimal change disease (MCD), focal and segmental glomerulosclerosis (FSGS), membranous glomerulopathy (MN), and IgA nephropathy (IgAN) were eligible for inclusion in this study. Other glomerular diseases were excluded. The pdf of the pathology report was reviewed by two pathologists to determine whether the number of glomeruli and the number of globally sclerotic glomeruli (GS) present in the biopsy was documented. Cases where the pathology report was missing the glomerular number assessment (40/317), either as a total number of glomeruli per biopsy as determined by an assessment across all histology sections, or as an average number of glomeruli per histology level, were excluded. A total of 277/317 cases were selected, distributed across the following diagnosis: 79 MCD, 108 FSGS, 54 MN, and 36 IgAN (Fig 1), all of which contain contained documentation of the the assessment of GS. No glass slides were available for re-review as part of this study.
Fig 1. Summary of workflow for case selection and annotation using the NEPTUNE Digital Pathology repository.
Glomerular counting
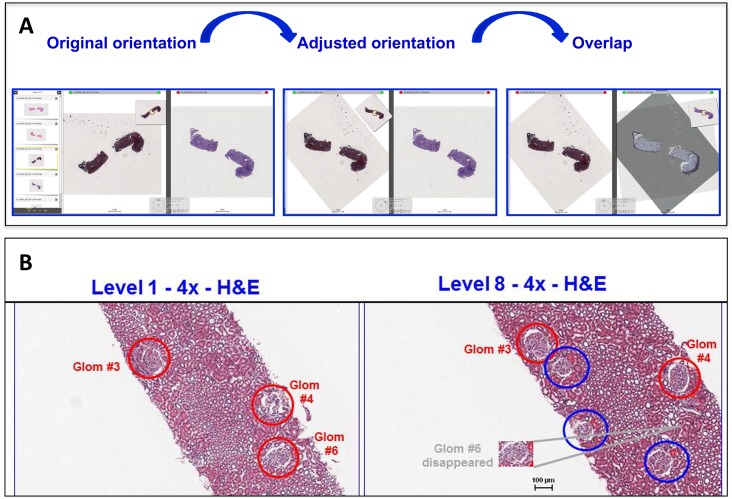
To test the value of annotation for glomerular enumeration and counting, ten pathologists annotated glomeruli in all WSI levels available by remotely accessing the 277 cases stored in the NEPTUNE DPR (Fig 1). As previously described, annotation of glomeruli was achieved by visualizing and aligning up to 4 WSI simultaneously (DIH, Leica, Dublin IR) and enumerating each glomerulus with a unique number that was maintained in all levels examined [11]. (Fig 2) Following initial annotation, each case underwent quality control review for accuracy of annotation by a different pathologist. Two of the ten pathologists independently retrieved the total number of annotated glomeruli in all 277 cases by remotely accessing each biopsy WSI section/level in the NEPTUNE DPR and recording the highest number used for glomerular annotation.
Fig 2. Digital review and annotation of whole slide images in the NEPTUNE digital pathology repository.
A) Example of multiple levels visualized at the same time. The software allows overlapping and orientation of the sections to facilitate multilevel reconstruction and representation of the biopsy levels. B) Digital annotation of whole slide images. Two levels are shown in alignment. Glomeruli in the left panel are annotated in red. In a subsequent level (right panel), two of the red-annotated glomeruli are still present (3 and 4), while one has disappeared (6). Three additional glomeruli, including one adjacent to glomerulus 3 and 6 have appeared in the deeper level (annotated in blue).
To investigate concordance between number of glomeruli counted on annotated WSI and number of glomeruli reported in the anonymized pathology reports, reported glomerular count was also recorded by two pathologists either as the absolute total number of glomeruli (139 cases) or the average of the number of glomeruli per histology level (138 cases). The number of annotated glomeruli was then compared to the number of reported glomeruli as follow:
a) for the 139 cases where the total number of glomeruli were recorded in the pathology report, the total number of reported glomeruli per biopsy was compared to the total number of annotated glomeruli counted on the corresponding WSI; b) for the 138 cases where the average number of glomeruli per histology level was reported, this average was compared to the average number of annotated glomeruli per WSI level per biopsy, calculated by dividing the total number of annotated glomeruli per number of WSI levels in each case.
To investigate the impact of annotation on assessment of globally sclerotic glomeruli, two pathologists counted the annotated GS by remotely accessing the NEPTUNE DPR and each biopsy WSI section/level, and recorded the total number or average number of reported GS by reviewing the report pdf. The number and percentage of annotated GS were compared with those recorded in the pathology report. Discrepancy for GS between the two pathologists were resolved by webinar consensus review. The percentages of annotated globally sclerotic glomeruli from WSI and from the pathology reports were calculated using annotated (total or average) and reported number of glomeruli, respectively.
Statistical methods
Descriptive statistics including mean, range, median and interquartile range (IQR). Wilcoxon signed rank tests were used to test the difference in total number and number of globally sclerotic glomeruli from annotated WSI versus given in pathology reports. The Wilcoxon test was used due to non-normality of the paired differences of annotated versus reported glomeruli. The analysis was performed separately for cases with pathology reports giving total versus average numbers of glomeruli, and presented both overall and with stratification by diagnosis (FSGS, MCD, MN, and IgANP).
To estimate the differences between annotated and reported counts and percentages with global sclerosis by categories of number of glomeruli or percent globally sclerotic glomeruli, linear regression models were used. The outcomes were the differences between annotated and reported values, and glomeruli categories were the covariates. All analyses were conducted in SAS software V9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Assessment of annotated glomeruli on WSI
A total of 9,379 annotated glomeruli were counted, of which 1,322 were classified as globally sclerotic. Across all four diagnostic categories, the average number of glomeruli per biopsy was 33 with a range of 3 to 164. Percent globally sclerotic averaged 16.7%, with a range of 0 to 100.
Comparison of total number of annotated versus reported glomeruli
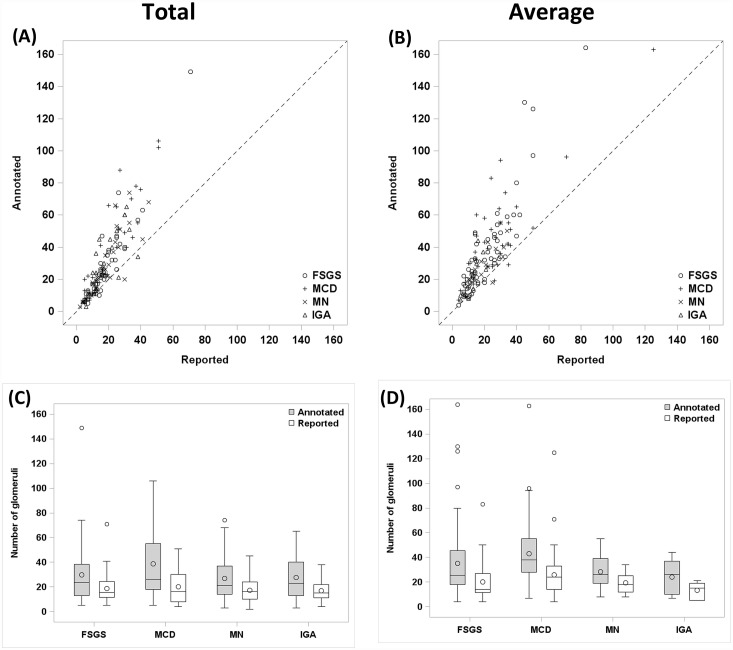
For the 139 cases where the total number of discrete glomeruli was given on the pathology report, the total number of annotated glomeruli per case was higher on average than the total number of glomeruli reported (Annotated: mean glomeruli per case = 30.7; range 3–149; median = 23; IQR 13–43. Reported: mean glomeruli per case = 18.3; range 2–71; median = 16; IQR 10–25; p<0.01) (Table 1). The difference between annotated and reported numbers of glomeruli increased as the number of glomeruli increased, with a ratio approaching 2:1 (Fig 3A). This relationship is also shown in Table 2, where the increase of annotated over reported glomeruli is proportional to the number of reported glomeruli.
Table 1. Number of annotated versus reported glomeruli stratified by diagnosis.
| Total | Average | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Reported | Annotated | Significance* | Reported | Annotated | Significance* | ||||
| Overall N = 139 | Range | 2–71 | 3–149 | <0.01 | Overall N = 138 | Range | 4–125 | 4–164 | <0.01 |
| Mean | 18.3 | 30.7 | Mean | 21.4 | 36.0 | ||||
| FSGS N = 40 | Range | 5–71 | 5–149 | <0.01 | FSGS N = 68 | Range | 4–83 | 4–164 | <0.01 |
| Mean | 18.7 | 29.9 | Mean | 20.1 | 35.2 | ||||
| MCD N = 33 | Range | 4–51 | 5–106 | <0.01 | MCD N = 46 | Range | 4–125 | 7–163 | <0.01 |
| Mean | 20.2 | 38.8 | Mean | 25.8 | 42.9 | ||||
| MN N = 37 | Range | 2–45 | 3–74 | <0.01 | MN N = 17 | Range | 8–34 | 8–55 | <0.01 |
| Mean | 17.1 | 26.8 | Mean | 19.3 | 28.2 | ||||
| IGA N = 29 | Range | 4–38 | 3–65 | <0.01 | IGA N = 7 | Range | 5–21 | 7–44 | <0.01 |
| Mean | 16.9 | 27.6 | Mean | 13.4 | 24.0 | ||||
Total: n = 139 cases and Average: n = 138 cases.
*Wilcoxon signed rank test
Fig 3. Digital annotation of whole slide images improves accuracy of glomerular enumeration.
(A,B) Scatter plot of annotated glomerular number versus reported glomerular number by diagnosis in cases reporting (A) total number of glomeruli or (B) average number of glomeruli per level. Dotted diagonal line shows where annotated = reported, and highlights the increase in number of glomeruli found by annotation. (A: n = 139; B: n = 138). (C,D) Box plot of annotated glomerular number and reported total glomerular number stratified by diagnosis in cases reporting (C) total number of glomeruli (n = 139) or (D) average number of glomeruli (n = 139).
Table 2. Difference in glomerular count of number of annotated versus reported glomeruli stratified by number of glomeruli.
| Total | Average | ||||||
|---|---|---|---|---|---|---|---|
| # glom | # cases | Mean Δ (annot—report) | Significance | # glom | # cases | Mean Δ (annot—report) | Significance |
| 1–10 | 37 | 3.8[0.1,7.5] | 0.05 | 1–10 | 27 | 5.7[0.6,10.9] | 0.03 |
| 11–20 | 55 | 9.0[5.9, 12.0] | <0.01 | 11–20 | 51 | 13.5[9.8,17.3] | <0.01 |
| 21–30 | 29 | 20.1[15.9, 24.3] | <0.01 | 21–30 | 35 | 15.3[10.7,19.9] | <0.01 |
| 31–40 | 12 | 23.3[16.8,29.9] | <0.01 | 31–40 | 17 | 15.8[9.3,22.3] | <0.01 |
| >40 | 6 | 38.8[29.6,48.1] | <0.01 | >40 | 8 | 46.5[37.0,56.0] | <0.01 |
Total: n = 139 cases and Average: n = 138 cases.
Comparison of average number of annotated versus reported glomeruli
Similarly, for the 138 cases where the average number of glomeruli per level was given on the pathology report, the average numbers of annotated glomeruli per level were higher than the average numbers given on pathology reports (Annotated: mean = 36; range 4–164; median = 30; IQR 19–46. Reported: mean = 21.4; range 4–125; median = 16; IQR 12–28; p<0.01)(Table 1). Again, the approximate 2:1 ratio is seen in the scatterplot between annotated and reported average glomeruli (Fig 3B). The increase in the difference with increasing categories of reported glomeruli (Table 2) mirrors the effect seen with total glomeruli above.
Stratification by center and disease category
Differences in total and average annotated and reported number of glomeruli were maintained across the 25 centers (data not shown) and all disease categories. (Fig 3C and 3D; Table 1)
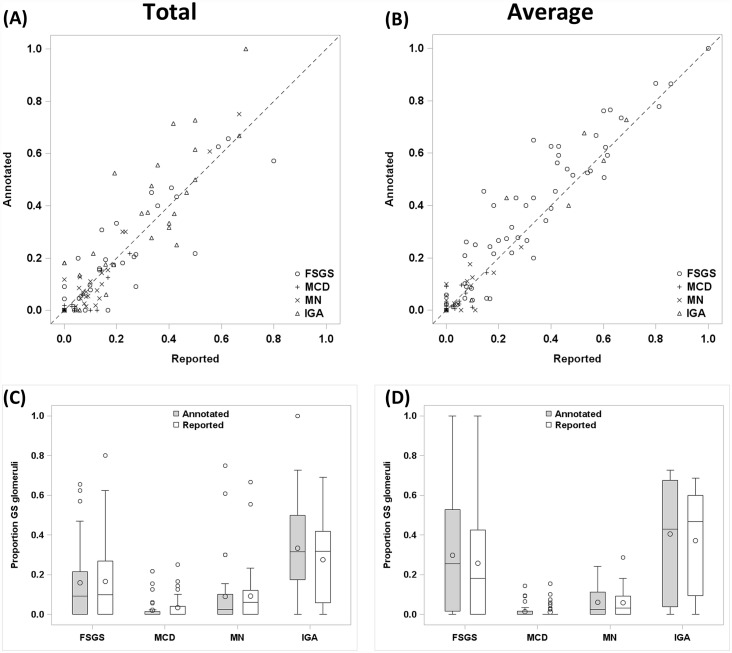
Comparison of annotated versus reported globally sclerotic glomeruli
In the 139 cases where the percentage of globally sclerotic glomeruli was obtained from the reported total number of glomeruli, there was no significant difference in the mean globally sclerotic glomeruli percentage determined on annotated WSI (14.4%) and the pathology reports (13.7%) (Table 3, Fig 4A). In contrast, in cases reporting an average glomerular number (138 cases), annotation yielded a greater mean globally sclerotic glomeruli percentage compared with the corresponding pathology reports (17.9% vs 15.8%, p<0.01) (Table 3, Fig 4B). When cases were stratified by disease (Fig 4C and 4D; Table 3), this discrepancy was statistically significant only in FSGS (29.8% vs 25.8%, p = <0.01). While the overall discrepancy was small in the percentage of globally sclerotic glomeruli between annotated WSI and pathology reports, in cases with > 40% globally sclerotic glomeruli there was a significant underestimation in the biopsy reports by both total and average methodologies (p < 0.01) (Fig 4A and 4B; Table 4); this effect was evident in FSGS and IGA, particularly for the biopsy reports using average glomeruli (Fig 4C and 4D).
Table 3. Number of annotated versus reported percent globally sclerotic (%GS) stratified by diagnosis.
| Total | Average | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Reported %GS | Annotated %GS | Significance* | Reported %GS | Annotated %GS | Significance* | ||||
| Overall N = 139 | Range | 0–80 | 0–100 | 0.71 | Overall N = 138 | Range | 0–100 | 0–100 | <0.01 |
| Mean | 13.7 | 14.4 | Mean | 15.8 | 17.9 | ||||
| FSGS N = 40 | Range | 0–80 | 0–65.6 | 0.99 | FSGS N = 68 | Range | 0–100 | 0–100 | <0.01 |
| Mean | 16.6 | 16.0 | Mean | 25.8 | 29.8 | ||||
| MCD N = 33 | Range | 0–25 | 0–21.7 | <0.01 | MCD N = 46 | Range | 0–15.3 | 0–14.3 | 0.81 |
| Mean | 3.3 | 2.1 | Mean | 1.2 | 1.3 | ||||
| MN N = 37 | Range | 0–66.7 | 0–75 | 0.65 | MN N = 17 | Range | 0–28.6 | 0–24.1 | 0.91 |
| Mean | 9.1 | 8.8 | Mean | 5.8 | 6.1 | ||||
| IGA N = 29 | Range | 0–69.2 | 0–100 | 0.02 | IGA N = 7 | Range | 0–68.8 | 0–72.7 | 0.69 |
| Mean | 27.4 | 33.3 | Mean | 37.2 | 40.6 | ||||
Total: n = 139 cases and Average: n = 138 cases.
*Wilcoxon signed rank test
Fig 4. Digital annotation of whole slide images modestly improves accuracy of global glomerular sclerosis enumeration.
(A,B) Box plot of annotated percent (%) globally sclerotic glomeruli and reported %globally sclerotic glomeruli in cases reporting (A) total number of glomeruli (n = 139) or (B) average number of glomeruli (n = 138). (C,D) Box plot of difference between number of annotated and reported % globally sclerotic glomeruli stratified by % globally sclerotic glomeruli in cases reporting (C) total number of glomeruli (n = 139) or (D) average number of glomeruli (n = 138).
Table 4. Difference in %GS glomeruli between annotated versus reported stratified by number of glomeruli.
| Total | Average | ||||||
|---|---|---|---|---|---|---|---|
| %GS | # cases | Mean Δ (annot—report) | Significance | %GS | # cases | Mean Δ (annot—report) | Significance |
| 0–19% | 103 | -0.80[-22.5,0.1] | 0.30 | 0–19% | 92 | -0.20 [-1.4, 1.1] | 0.77 |
| 20–39% | 17 | -0.24[-38.4, 3.4] | 0.90 | 20–39% | 15 | 3.0 [-0.2, 6.2] | 0.07 |
| 40–59% | 10 | 6.5[1.8,11.2] | <0.01 | 40–59% | 17 | 7.5 [4.5, 10.6] | <0.01 |
| 60–100% | 9 | 12.8[7.7,17.9] | <0.01 | 60–100% | 14 | 10.3 [7.0, 13.7] | <0.01 |
Total: n = 139 cases and Average: n = 138 cases.
Discussion
Glomerular counting is a fundamental metric for renal biopsy providing the denominator for glomerular involvement in primary and secondary kidney diseases. In this study we evaluated the NEPTUNE protocol for glomerular annotation to provide a standardized and reliable estimate of number of glomeruli. Although Whole Slide Imaging is not approved for primary diagnosis in routine pathologic practice in the US [14] it is an enabling technology for the development and validation of evaluation of information gained from light microscopy. WSI with and without annotation has been demonstrated to enhance reproducibility of pathology assessment compared to glass slide review [15–17].
The application of digital annotation facilitates accuracy for renal pathology metric that cannot be achieved by conventional LM. The accuracy of determining the number of glomeruli in a given biopsy by LM is limited by visual-spatial memory of the pathologist across multiple histologic levels. This issue is resolved by the digital software allowing visualization and alignment of multiple levels at the same time, facilitating identification of the same or different glomeruli thru the biopsy. Thus, we found significant differences between the number of glomeruli reported for routine patient care and obtained by LM evaluation, and the number of glomeruli identified by digital annotation. We also demonstrated that discrepancy in glomerular number increases proportionally to the number of glomeruli present within a biopsy, demonstrating the limitation of manual light microscopy to accurately determine the number of glomeruli present. In contrast, the annotated and reported percentages of GS were generally more similar. However, discrepancies were found within disease subgroups and particularly for cases with percent GS over 40%, with annotated values showing higher percent sclerosis in all cases. These data suggest that up to a certain threshold, the discrepancy between annotated and conventional approaches are probably minimally critical for prognostic factors, but may become relevant for biopsies rich in glomeruli and with significant sclerosis. Glomerular density and percentage of GS have been discussed as a risk factor in disease progression [18], IgA [19], risk of progression in membranous glomerulonephritis [20] and obesity-related glomerulopathy [21]. Thus, accurate assessment with improved numerators and denominators is essential in improving prognostication.
Accurate glomerular counting is fundamental to determining biopsy adequacy and improved prognostication. It is anticipated that with digital enumeration of glomeruli, the binomial distribution of abnormal glomeruli (i.e., with segmental lesions), and thus the number of glomeruli needed for accurate sampling, will be greater than previously suggested [22].
Although the ultimate proof of the increased accuracy of digital annotation versus conventional light microscopy would be provided by direct comparison of glomerular number estimate on glass slide and annotated WSI, glass slides were not available and we had to rely on values extracted from the pathology report.
Our study demonstrates the limits of the conventional approach to microscopic examination of tissue in tasks that require enumeration and integration across multiple tissue sections. We have carried out this study in the context of glomerular disease that is a part of the NEPTUNE protocol. The data demonstrates that low frequency events can be accounted for with relative accuracy, as demonstrated by both the overall glomerular enumeration as well as percent global sclerosis data. However, as the number of events increases, the inaccuracy of the estimation increases. With the glomerular number, this reached a level of 2:1 when WSI and manual microscopy are compared. For percent glomerular sclerosis, inaccurate determinations reached statistical significance at 40%GS. These findings suggest that quantization of the histopathology of glomerular disease by an intensive approach, utilizing WSI and piecemeal evaluation of individual glomerular profiles will result in new insights to disease classification, prognostic markers, and potential markers of response to therapy.
These findings suggest the accuracy of detection is object specific, and that findings for one object may not generalize to other objects. Although this study was performed within the limited context of primary glomerular disorders, the findings have broad implications for many observer-based task where integration across image planes is required. The evaluation of renal biopsies for other disorders, including diabetes, SLE and transplant are obvious fields of inquiry, as are renal biopsies of medical conditions of the liver, where portal triads and other features are routinely enumerated. The overall implications are that there are some conventional approaches that may be enhanced by the adoption of computer-aided diagnostic tools. Manual review and enumeration of renal biopsies with current tools is time consuming and complex, however the development of tools to aid the reviewer in a value-added strategy are underway.
Acknowledgments
We would like to thank Dr. Charles Jennette and the CureGN pathology committee, for constructive discussions and feedback.
Data Availability
The NEPTUNE protocol has an established data sharing policy to protect patient confidentiality. Information to request access is available via the corresponding author, or via https://clinicaltrials.gov/ct2/show/NCT01209000?term=neptune&rank=3.
Funding Statement
The Nephrotic Syndrome Study Network Consortium (U54-DK-083912) is a part of the National Center for Advancing Translational Sciences, Rare Disease Clinical Research Network, supported through a collaboration between the Office of Rare Diseases Research, NCATS, and the National Institute of Diabetes, Digestive, and Kidney Diseases. Additional funding and/or programmatic support for this project has also been provided by the University of Michigan, NephCure Kidney International, and the Halpin Foundation. Dr. Jeffrey Hodgin is supported by K08-DK088944 and the NephCure-ASN Foundation. Additional support in part was provided by the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research.
References
- 1.Walker PD, Cavallo T, Bonsib SM, Ad Hoc Committee on Renal Biopsy Guidelines of the Renal Pathology S. Practice guidelines for the renal biopsy. Modern pathology: an official journal of the United States and Canadian Academy of Pathology, Inc. 2004;17(12):1555–63. 10.1038/modpathol.3800239 . [DOI] [PubMed] [Google Scholar]
- 2.Muehrcke RC, Kark RM, Pirani CL, Pollak VE. Lupus nephritis: a clinical and pathologic study based on renal biopsies. Medicine. 1957;36(1):1–145. . [PubMed] [Google Scholar]
- 3.Pirani CL, Pollak VE, Schwartz FD. The Reproducibility of Semiquantitative Analyses of Renal Histology. Nephron. 1964;1:230–7. . [DOI] [PubMed] [Google Scholar]
- 4.Weening JJ, D'Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, et al. The classification of glomerulonephritis in systemic lupus erythematosus revisited. Journal of the American Society of Nephrology: JASN. 2004;15(2):241–50. . [DOI] [PubMed] [Google Scholar]
- 5.Gambara V, Mecca G, Remuzzi G, Bertani T. Heterogeneous nature of renal lesions in type II diabetes. Journal of the American Society of Nephrology: JASN. 1993;3(8):1458–66. . [DOI] [PubMed] [Google Scholar]
- 6.Tervaert TW, Mooyaart AL, Amann K, Cohen AH, Cook HT, Drachenberg CB, et al. Pathologic classification of diabetic nephropathy. Journal of the American Society of Nephrology: JASN. 2010;21(4):556–63. 10.1681/ASN.2010010010 . [DOI] [PubMed] [Google Scholar]
- 7.Working Group of the International Ig ANN, the Renal Pathology S, Roberts IS, Cook HT, Troyanov S, Alpers CE, et al. The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney international. 2009;76(5):546–56. 10.1038/ki.2009.168 . [DOI] [PubMed] [Google Scholar]
- 8.Austin HA 3rd, Balow JE. Henoch-Schonlein nephritis: prognostic features and the challenge of therapy. American journal of kidney diseases: the official journal of the National Kidney Foundation. 1983;2(5):512–20. . [DOI] [PubMed] [Google Scholar]
- 9.Solez K, Axelsen RA, Benediktsson H, Burdick JF, Cohen AH, Colvin RB, et al. International standardization of criteria for the histologic diagnosis of renal allograft rejection: the Banff working classification of kidney transplant pathology. Kidney international. 1993;44(2):411–22. . [DOI] [PubMed] [Google Scholar]
- 10.Sethi S, Haas M, Markowitz GS, D'Agati VD, Rennke HG, Jennette JC, et al. Mayo Clinic/Renal Pathology Society Consensus Report on Pathologic Classification, Diagnosis, and Reporting of GN. Journal of the American Society of Nephrology: JASN. 2015. 10.1681/ASN.2015060612 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barisoni L, Nast CC, Jennette JC, Hodgin JB, Herzenberg AM, Lemley KV, et al. Digital pathology evaluation in the multicenter Nephrotic Syndrome Study Network (NEPTUNE). Clinical journal of the American Society of Nephrology: CJASN. 2013;8(8):1449–59. 10.2215/CJN.08370812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nast CC, Lemley KV, Hodgin JB, Bagnasco S, Avila-Casado C, Hewitt SM, et al. Morphology in the Digital Age: Integrating High-Resolution Description of Structural Alterations With Phenotypes and Genotypes. Seminars in nephrology. 2015;35(3):266–78. 10.1016/j.semnephrol.2015.04.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gadegbeku CA, Gipson DS, Holzman LB, Ojo AO, Song PX, Barisoni L, et al. Design of the Nephrotic Syndrome Study Network (NEPTUNE) to evaluate primary glomerular nephropathy by a multidisciplinary approach. Kidney international. 2013;83(4):749–56. 10.1038/ki.2012.428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fine JL. 21(st) century workflow: A proposal. Journal of pathology informatics. 2014;5:44 10.4103/2153-3539.145733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ozluk Y, Blanco PL, Mengel M, Solez K, Halloran PF, Sis B. Superiority of virtual microscopy versus light microscopy in transplantation pathology. Clinical transplantation. 2012;26(2):336–44. 10.1111/j.1399-0012.2011.01506.x . [DOI] [PubMed] [Google Scholar]
- 16.Jen KY, Olson JL, Brodsky S, Zhou XJ, Nadasdy T, Laszik ZG. Reliability of whole slide images as a diagnostic modality for renal allograft biopsies. Human pathology. 2013;44(5):888–94. 10.1016/j.humpath.2012.08.015 . [DOI] [PubMed] [Google Scholar]
- 17.Barisoni L, Jennette JC, Colvin R, Sitaraman S, Bragat A, Castelli J, et al. Novel quantitative method to evaluate globotriaosylceramide inclusions in renal peritubular capillaries by virtual microscopy in patients with fabry disease. Archives of pathology & laboratory medicine. 2012;136(7):816–24. 10.5858/arpa.2011-0350-OA . [DOI] [PubMed] [Google Scholar]
- 18.Imasawa T, Nakazato T, Ikehira H, Fujikawa H, Nakajima R, Ito T, et al. Predicting the outcome of chronic kidney disease by the estimated nephron number: the rationale and design of PRONEP, a prospective, multicenter, observational cohort study. BMC nephrology. 2012;13:11 10.1186/1471-2369-13-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsuboi N, Kawamura T, Koike K, Okonogi H, Hirano K, Hamaguchi A, et al. Glomerular density in renal biopsy specimens predicts the long-term prognosis of IgA nephropathy. Clinical journal of the American Society of Nephrology: CJASN. 2010;5(1):39–44. 10.2215/CJN.04680709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsuboi N, Kawamura T, Miyazaki Y, Utsunomiya Y, Hosoya T. Low glomerular density is a risk factor for progression in idiopathic membranous nephropathy. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association—European Renal Association. 2011;26(11):3555–60. 10.1093/ndt/gfr399 . [DOI] [PubMed] [Google Scholar]
- 21.Tsuboi N, Utsunomiya Y, Kanzaki G, Koike K, Ikegami M, Kawamura T, et al. Low glomerular density with glomerulomegaly in obesity-related glomerulopathy. Clinical journal of the American Society of Nephrology: CJASN. 2012;7(5):735–41. 10.2215/CJN.07270711 . [DOI] [PubMed] [Google Scholar]
- 22.Corwin HL, Schwartz MM, Lewis EJ. The importance of sample size in the interpretation of the renal biopsy. American journal of nephrology. 1988;8(2):85–9. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The NEPTUNE protocol has an established data sharing policy to protect patient confidentiality. Information to request access is available via the corresponding author, or via https://clinicaltrials.gov/ct2/show/NCT01209000?term=neptune&rank=3.