Abstract
Purpose
We examined total, light, and moderate-to-vigorous physical activity (MVPA) as predictors of mortality in a nationally representative sample of older adults. Then, we explored the theoretical consequences of replacing sedentary time with the same duration of light activity or MVPA.
Methods
Using accelerometer measured activity, the associations between total, light (100 to 2019 counts per minute), and moderate-to-vigorous (>2019 counts per minute) activity counts and mortality were examined in adults aged 50 to 79 in the National Health and Nutrition Examination Survey, 2003-2006 (n=3,029), with mortality follow-up through December 2011. Cox proportional hazards models were fitted to estimate mortality risks. An isotemporal substitution model was used to examine the theoretical consequences of replacing sedentary time with light activity or MVPA on mortality.
Results
After adjusting for potential confounders, including age, sex, race/ethnicity, education, body mass index, and the presence of comorbid conditions, those in the highest tertile of total activity counts had one fifth the risk of death of those in the lowest tertile (HR: 0.21, 95% CI: 0.12, 0.38), and those in the middle tertile had one third the risk of death (HR: 0.36, 95% CI: 0.30, 0.44). In addition, replacing thirty minutes of sedentary time with light activity was associated with significant reduction in mortality risk (After 5 years of follow-up: HR = 0.80, 95% CI: 0.75, 0.85). Replacing thirty minutes of sedentary time with MVPA was also associated with reduction in mortality risk (HR = 0.49, 95% CI: 0.25, 0.97).
Conclusions
Greater total activity is associated with lower all-cause mortality risk. Replacing sedentary time with light activity or MVPA may reduce mortality risk for older adults.
Keywords: Accelerometer, light activity, moderate to vigorous physical activity, prospective cohort study, sedentary
INTRODUCTION
Physical activity, an important behavioral predictor of health, morbidity, and mortality (12, 19), is often categorized by its intensity. Moderate (3.0-6.0 metabolic equivalents (METs)) to vigorous (>6 METs) physical activity (MVPA) comprises activities such as brisk walking or running, that generally require significant movement and increased energy expenditure; sedentary behavior refers to activities such as sitting that involve minimal movement or energy expenditure and fall in the range of 1.0 to 1.5 METs; and light activity refers to activity in between sedentary and MVPA, such as standing, walking at slow to usual pace, and routine housework (1).
Objective measurement of physical activity via accelerometry provides an advantage over self-reported physical activity because self-reports are known to overestimate duration and intensity of physical activity (29, 35). Accelerometers also provide data on intensity every minute or less, potentially allowing estimation of the duration and intensity of activity with greater precision than self-reports (28). Sedentary and light activity are particularly difficult to measure using self-reports, and are often not included in studies based on self-report (34). Cut-points for MVPA, light activity, and sedentary behavior have been proposed for accelerometry corresponding to equivalent MET intensity values (35).
Greater MVPA is protective against morbidity and mortality (5, 9, 12). One study using accelerometry suggests that fewer than 10% of adults get the recommended 30 minutes per day of MVPA on at least 5 of 7 days (35) and estimates of adherence based on self-report are often between 30 and 60%. This proportion declines with age; for example, Troiano et al. found that only 2.4% of people over age 60 meet the recommendations (35). Regardless of whether adherence estimates from accelerometry or self report are correct, many adults fail to meet recommendations for MVPA, and MVPA may be difficult for some adults to engage in (e.g. disability or multiple co-morbidities). Thus recent studies have begun to explore the role of light intensity activity and sedentary time in relation to health and mortality, especially in older adults. Studies have shown that greater sedentary time is predictive of morbidity and mortality, regardless of the amount of time spent in MVPA (4, 11). There is growing interest in whether light activity, which may be more attainable than MVPA for certain populations, might also be protective against the risk of mortality. Light activity accounts for a majority of total daily activity for the average person (8, 14); it is therefore important to understand its influence on mortality risks. Several studies have found an association between greater light-intensity activity and reduced mortality when using self-reported physical activity data (6, 16, 40) but only a handful of studies have examined relationships with objectively measured physical activity.
The aims of this paper are two-fold. First, we examined accelerometer-measured total, light, and moderate-to-vigorous physical activity as predictors of mortality in a nationally representative sample of older adults. We hypothesized that greater total, light, and moderate-to-vigorous physical activity would each be associated with reduced mortality risk. Second, we used an isotemporal substitution model (17) to explore the theoretical consequences of replacing sedentary time with the same duration of light activity or with MVPA, and, conversely, replacing MVPA with the same duration of light activity. We hypothesized that replacement of sedentary time with light activity or MVPA would reduce mortality risk, while replacing MVPA with light activity would increase mortality risk.
METHODS
Study population
Data are from the 2003-2004 and 2005-2006 waves of the National Health and Nutrition Examination Survey (NHANES), a stratified, multistage probability sample representative of the civilian non-institutionalized U.S. population, described in detail elsewhere (21). These data are linked to death records from the National Death Index through December 31, 2011 (22), which provide vital status. If deceased, length of time (in months) between the NHANES examination and the subject’s death is provided. There were 3,653 subjects aged 50 and older at baseline examination who provided sufficient accelerometry data, defined as at least one day of at least 10 hours of wear time to be consistent with prior evidence (11, 36, 37). The threshold of 10 hours is appropriate because a simulation study of NHANES data found that the proportion of time subjects spent in activities of different intensities was the same whether a valid day was defined as 10 hours or 14 hours of wear time (7). There were 6 subjects with unknown vital status and 1 with unknown survival time, and an additional 33 subjects were missing data on measured body mass index (BMI); these subjects were excluded. A further 10 subjects who died of accidental causes and 574 subjects aged 80 and above were excluded for analytical purposes as outlined below in the Statistical analysis section. The final analytic sample contained 3,029 observations of persons aged 50 to 79 at baseline.
Measures
Physical activity was measured with the ActiGraph AM-7164 accelerometer (ActiGraph, LLC, Fort Walton Beach, Florida), using methods described in detail elsewhere (11, 20, 35). Participants were instructed to wear the device on a belt around the waist for seven consecutive days, except when sleeping or bathing. The accelerometers measure movement and its intensity in activity counts per minute, with higher count values corresponding to more-intense movement. Non-wear time was defined as intervals of at least 60 consecutive minutes of zero counts, with allowance for up to two minutes of counts between 1 and 100 (11, 25). Total physical activity volume was measured a priori in total activity counts per day by sex-specific tertiles (39).
Accelerometer data were also classified into physical activity intensity levels using previously established cut-points based on METs of activity (11, 35). Sedentary behavior was defined as counts per minute below 100; light activity was defined as counts per minute from 100 to 2019; and MVPA was defined as counts per minute of 2020 or higher. Total activity counts comprised the sum of sedentary, light, and MVPA counts. Light activity and MVPA volume were measured in counts per day, by sex-specific tertiles, in parallel to the measure of total activity volume.
In the isotemporal substitution model, minutes per day in each physical activity intensity level, rather than counts per day, were used. Minutes per day were modeled as continuous variables, with each value divided by 10 so that regression coefficients could represent the partial effects of 10 additional minutes in a given activity intensity.
Selection of covariates was based on known confounders of the activity-mortality relationship, from a prior study in NHANES (11). Covariates included age, sex, race/ethnicity (non-Hispanic black, Hispanic, White and other), education (less than high school, high school, more than high school), smoking status (never, former, current), BMI (kg/m2), mobility limitation (yes, no), defined as any difficulty walking a quarter mile or walking up ten steps, and diagnosis of diabetes (yes, no), coronary heart disease (yes, no), congestive heart failure (yes, no), stroke (yes, no), and cancer (yes, no). The time scale in survival model was years since baseline measurement of physical activity. All covariates were self-reported except BMI, where height and weight were measured by NHANES technicians.
Statistical analysis
Descriptive statistics were calculated for the sample as a whole and by tertiles of total activity volume. Linear trends in covariates were tested using an ordinal variable linear regression across tertiles of total activity.
Log-rank tests assessed the unadjusted differences in survival across tertiles of total activity, light activity, and MVPA counts. Cox proportional-hazards models were used to estimate the hazard ratios (HR) and 95% confidence intervals (CI) for total activity, light activity, and MVPA counts. Minimally adjusted models included (X): age, sex, race/ethnicity, and education level, while fully adjusted models added: BMI, smoking, and the presence of chronic diseases and mobility limitations. In a sensitivity analysis, subjects with at least one chronic disease or mobility limitation at baseline were excluded. Formally, the model used was:
| (Equation 1). |
In Equation 1, h0(t) is the baseline hazard function; totaltime is total wear time (minutes) per day; T2 and T3, are indicators that the person’s total activity counts were in the second or third tertile, respectively, with those in the first tertile serving as the reference group; and X is defined above. In models of light activity, the meaning of all the parameters of Equation 1 remain the same, except that T2 and T3 indicate that the person’s light activity counts were in the second or third tertile. Models of light activity counts also adjusted for minutes of MVPA. In models of MVPA, T2 and T3 indicate that the person’s MVPA counts were in the second or third tertile, with all other aspects of the model the same as the model of total activity counts.
The proportional hazards assumption underlying Equation 1 was assessed graphically using log-log plots and observed (Kaplan-Meier) versus predicted (under proportional hazards) plots. In initial models, the proportional hazards assumption with respect to the indicators for activity tertiles (T2 and T3) was violated, as shown by crossover of the log survival time curves of T2 and T3 in the first year of follow-up, suggesting that early deaths were the source of the violation of the proportional hazards assumption. Because the hazard of death over age 80 has a different functional form than that below age 80 (33), subjects over age 80 at baseline were excluded. Subjects whose cause of death was coded as accidental (ICD-10 groups V01 to X59 and Y85 to Y86) were also excluded because the median time to death among these subjects (2.5 years) was considerably shorter than the median time to death for subjects who died from all other causes (3.75 years). After exclusion of these individuals, the proportional hazards assumption was met.
The theoretical result of replacing a defined duration of one physical activity intensity for the same duration of another physical activity intensity was estimated with an isotemporal substitution Cox proportional-hazards model (17). The statistical model was
| (Equation 2). |
In Equation 2, h0(t), totaltime, and X are defined as above. By construction, totaltime is composed of lighttime (minutes of light activity), MVPAtime (minutes of MVPA), and sedentarytime (minutes of sedentary time). By omitting sedentary time from the model, the coefficient β2 represents the partial effect of substituting 10 minutes of sedentary time with 10 minutes of light activity, holding MVPA, the length of the “wear-day”, and the values of covariates in X constant. Similarly, if light activity and total wear time are held constant, then β3 represents the partial effect of replacing 10 minutes of sedentary time with 10 minutes of MVPA (17). To examine the possibility that associations between physical activity and mortality vary over time an interaction variable was defined as Int=lighttime*(years since baseline). For continuous independent variables, such as minutes of activity, this interaction term maintains the statistical validity of the model even if the proportional hazards assumption associated with the variable lighttime is violated. Multicollinearity was assessed by calculating variance inflation factors (VIF) from linear regressions of each physical activity variable onto all the other covariates.
Data were analyzed using Stata MP Version 14.0 (StataCorp, College Station, Texas). Two-year examination weights were divided in half because two waves of NHANES were pooled, and strata and primary sampling units were used to account for complex survey characteristics, as recommended by NHANES (21). All tests were two-sided with significance set at alpha=0.05.
Conventional model fit statistics such as Akaike’s Information Criterion (AIC) and the Bayesian Information Criterion (BIC) do not pertain to models that use survey design-based estimation (13). Approximate comparisons of model fit were developed as follows (13): First, sampling weights were rescaled to sum to the sample size, rather than the population size. Then all models were re-run with the rescaled weights and with additional covariates representing strata and primary sampling units to obtain maximum-likelihood (rather than design-based) parameter and variance estimates. AIC, BIC, and likelihood were obtained from these maximum-likelihood models and assigned to their corresponding design-based models.
INFORMED CONSENT STATEMENT
This study involved analysis of publicly available secondary data only. NHANES operates under the approval of the National Center for Health Statistics Research Ethics Review Board, Protocols #98-12, #2005-06, and #2011-17.
RESULTS
Descriptive statistics of the analytic sample, weighted to be representative of the U.S. population ages 50-79 in years 2003-2006 and stratified by tertiles of total activity volume (counts) accumulated during an average day, are shown in Table 1. The prevalence of diabetes was 14.6% and the prevalence of mobility limitation was 16.0%. Those with the lowest daily volume of total activity were significantly older and had higher prevalence of chronic disease than those with more total activity counts (P-for trends <0.001). The majority of total activity volume in all activity tertiles was accumulated through light activity. Those in higher tertiles of total activity accumulated more MVPA minutes per day (P-for trends <0.001); however, in all tertiles, less than 3% of wear-time consisted of MVPA. A comparison of the analytic sample to the full age-matched NHANES sample (see Table, Supplemental Digital Content 1, which shows descriptive statistics for all NHANES 2003-2006 subjects aged 50-79 years) shows that those lacking valid physical activity had similar baseline characteristics as those in the analytic sample.
Table 1.
Baseline Means (SDs) or Percentages in Analytic Sample: Full Sample and by Tertile of Total Activity Counts. National Health and Nutrition Examination Survey, United States, 2003-2006.
| Overall | Tertile 1 (Least) |
Tertile 2 | Tertile 3 (Most) |
P for trend |
|
|---|---|---|---|---|---|
| (n=3,029) | (n=1,011) | (n=1,009) | (n=1,009) | ||
| Sociodemographic characteristics | |||||
| Age (years) | 61.3 (8.4) | 65.9 (9.0) | 61.1 (8.2) | 58.1 (6.4) | <.001 |
| Female (%) | 53.4% | 54.5% | 53.0% | 53.0% | 0.486 |
| White (%) | 79.5% | 79.4% | 79.5% | 79.7% | 0.869 |
| Black (%) | 9.4% | 11.8% | 8.5% | 8.5% | 0.011 |
| Hispanic (%) | 6.6% | 4.4% | 6.1% | 8.7% | <.001 |
| < HS education (%) | 9.4% | 14.2% | 8.3% | 6.7% | 0.028 |
| > HS education (%) | 26.7% | 21.7% | 28.7% | 28.8% | 0.027 |
| Health behaviors and prevalent conditions | |||||
| Current smoker (%) | 18.5% | 22.6% | 18.3% | 15.6% | 0.006 |
| BMI (kg/m2) | 29.0 (6.2) | 30.6 (7.5) | 29.3 (6.2) | 27.6 (4.8) | <.001 |
| Diabetes (%) | 14.6% | 26.1% | 13.5% | 6.8% | <.001 |
| CHD (%) | 7.3% | 13.7% | 6.4% | 3.2% | <.001 |
| CHF (%) | 4.8% | 11.2% | 2.7% | 1.8% | <.001 |
| Stroke (%) | 4.5% | 9.5% | 2.9% | 2.1% | <.001 |
| Cancer (%) | 15.5% | 21.4% | 13.7% | 12.7% | <.001 |
| Mobility lim. (%) | 16.0% | 29.6% | 15.5% | 6.1% | <.001 |
| Daily physical activity | |||||
| Sedentary minutes | 533 (138) | 616 (148) | 538 (112) | 467 (118) | <.001 |
| Light minutes | 322 (99) | 220 (69) | 321 (53) | 401 (75) | <.001 |
| MVPA minutes | 16 (18) | 3 (3) | 11 (7) | 30 (20) | <.001 |
| Valid minutes of wear time | 871 (121) | 839 (138) | 869 (111) | 898 (111) | <.001 |
| Counts from Sed. (thousands) | 8.2 (2.2) | 7.8 (2.4) | 8.5 (2.1) | 8.2 (1.9) | 0.011 |
| Counts from Light (thousands) | 167.8 (73.2) | 88.6 (31.9) | 159.8 (26.5) | 235.1 (56.4) | <.001 |
| Counts from MVPA (thousands) | 47.8 (62.3) | 8.3 (10.4) | 29.8 (23.7) | 93.7 (73.7) | <.001 |
| Total counts (thousands) | 223.8 (113.9) | 104.7 (35.1) | 198.2 (27.8) | 337.0 (88.3) | <.001 |
Abbreviations: SD, standard deviation; T, Tertile; HS, High School; BMI, Body Mass Index; CHD, Coronary Heart Disease; CHF, Congestive Heart Failure; Sedentary, <100 counts per minute; MVPA, Moderate-to-vigorous physical activity (>2,019 counts per minute); Minutes, minutes per day.
Mobility lim. = any difficulty walking 1/4 mile or walking up ten steps.
Means, percentages, and SDs are survey-weighted.
Minimum and maximum total daily counts, by sex and tertile:
Males: Tertile 1, (14,665, 160,580); Tertile 2, (160,590, 260,860); Tertile 3, (261,710, 877,750).
Females: Tertile 1, (20,173, 148,250); Tertile 2, (148,380, 225,170); Tertile 3, (225,500, 913,000).
There were 387 deaths in 19,757 person-years at risk, corresponding to a crude, unweighted death rate of 1.96 deaths per 100 person-years. Mean follow-up time was 6.5 years, with a maximum of 8 years, 11 months. The oldest observed age at death was 88 years, 10 months. Causes of death were provided based on the three leading characters in ICD-10 codes. The most common causes of death in the NHANES sample were malignant neoplasms (116 deaths), a residual category (107 deaths), and diseases of the heart (85 deaths).
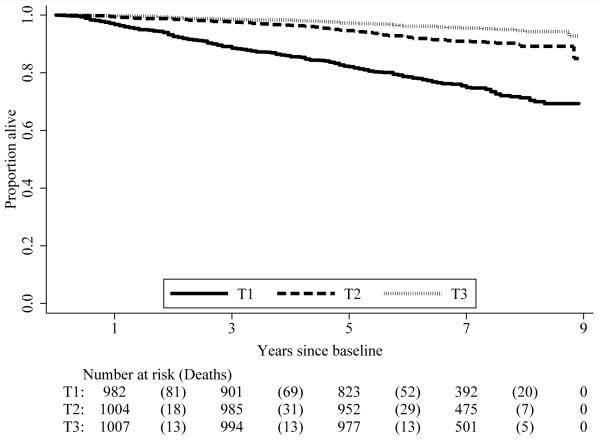
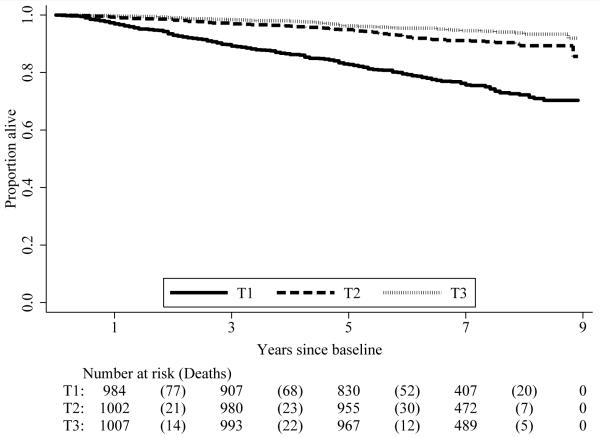
In unadjusted models, those in higher tertiles of total activity volume and light activity volume had a reduced mortality risk compared to those in lower tertiles (log-rank test P<0.001). Figure 1 shows the proportions surviving over time, by total activity tertile and light activity tertile. This figure shows that for both total activity (top panel) and light activity (bottom panel), individuals in Tertile 1 – that is, those with the least total or light activity – were much less likely to survive a given length of time than those in the other two tertiles, while the differences in survival between tertiles 2 and 3 were much smaller. The same pattern appears when comparing individuals by tertile of MVPA (see Figure, Supplemental Digital Content 2, which show Kaplan-Meier survival curves by tertile of MVPA).
Figure 1.
Kaplan-Meier curve by tertile of total activity counts (top panel) and tertile of light activity counts (bottom panel), National Health and Nutrition Examination Survey, 2003-2006. Subjects aged 50-79 at baseline; mortality follow-up through 2011 (n=3,029). T1=Tertile 1 (fewest activity counts), T2=Tertile 2, T3=Tertile 3 (most activity). Embedded tables show number of subjects at risk at specific points: 1, 3, 5, 7, and 9 years of follow-up, and number of deaths occurring in the intervals between these points. Values in embedded tables are unweighted.
Table 2 (top panel) shows the association between total activity counts (in tertiles) and mortality in minimally and fully adjusted models. Those in tertiles 2 and 3 had significantly lower mortality rates than those in the tertile with the least total activity. The covariate-adjusted differences in mortality between those in the tertile with the least activity and those in the next-least-active tertile were quite large: those in Tertile 2 had about a third of the hazard of death of those in Tertile 1. The same pattern of results held in the minimally adjusted models (Model A) as well as in the models that excluded those with mobility limitations or chronic diseases at baseline (Model C). As reflected in the Kaplan-Meier curves shown in Figure 1, the largest survival gain is associated with the difference between the least-active tertile and the second tertile; survival differences between Tertile 2 and Tertile 3 were smaller in magnitude and not statistically significant.
Table 2.
Association between Total Activity Counts, Light Activity Counts, MVPA Counts, and Mortality
| N Deaths | PY Lived | Model A | Model B | Model C | ||||
|---|---|---|---|---|---|---|---|---|
| (Unadjusted) | Unadjusted) | HR | [95% CI] | HR | [95% CI] | HR | [95% CI] | |
| Tertile of Total Activity | ||||||||
| 1 (Ref.) | 251 | 6,118 | 1 | [Ref.] | 1 | [Ref.] | 1 | [Ref.] |
| 2 | 90 | 6,749 | 0.29 | [0.23,0.37] | 0.36 | [0.30,0.44] | 0.39 | [0.22,0.70] |
| 3 | 46 | 6,891 | 0.16 | [0.09,0.30] | 0.21 | [0.12,0.38] | 0.30 | [0.14,0.62] |
| P-value for difference (Tertile 3 - Tertile 2) | 0.063 | 0.092 | 0.430 | |||||
| Tertile of Light Activity | ||||||||
| 1 (Ref.) | 244 | 6,186 | 1 | [Ref.] | 1 | [Ref.] | 1 | [Ref.] |
| 2 | 88 | 6,721 | 0.29 | [0.22,0.39] | 0.37 | [0.27,0.49] | 0.37 | [0.20,0.69] |
| 3 | 55 | 6,850 | 0.22 | [0.14,0.36] | 0.28 | [0.17,0.46] | 0.47 | [0.25,0.86] |
| P-value for difference (Tertile 3 - Tertile 2) | 0.323 | 0.374 | 0.508 | |||||
| Tertile of MVPA | ||||||||
| 1 (Ref.) | 243 | 6,155 | 1 | [Ref.] | 1 | [Ref.] | 1 | [Ref.] |
| 2 | 94 | 6,725 | 0.36 | [0.26,0.51] | 0.44 | [0.32,0.61] | 0.49 | [0.30,0.80] |
| 3 | 50 | 6,878 | 0.20 | [0.11,0.35] | 0.27 | [0.15,0.47] | 0.22 | [0.10,0.48] |
| P-value for difference (Tertile 3 - Tertile 2) | 0.041 | 0.082 | 0.065 | |||||
Light activity: counts per minute 100-2,019. MVPA: >2,019 counts per minute.
Subjects aged 50 to 79 (last birthday) at baseline; mortality follow-up through 2011 (n=3,029).
Models A adjust for baseline age, sex, race/ethnicity, education, minutes of device wear-time; Models B add covariates for body mass index (kg/m2), smoking, and the presence of diabetes, coronary heart disease, congestive heart failure, stroke, cancer, and mobility limitation. Model (C) excludes those with prevalent chronic illnesses (diabetes, coronary heart disease, congestive heart failure, stroke, and cancer) or mobility limitations at baseline (n=1,424). Models incorporate sampling weights and complex survey characteristics of NHANES.
N deaths and Person-Years columns are unadjusted and unweighted.
P-Values for differences are computed using a t-test of the linear combination βT3 – βT2 with the null hypothesis that this quantity is zero.
The second panel of Table 2 shows the relation between light activity volume and mortality, holding constant the full set of covariates, including minutes of MVPA. Again, those in Tertiles 2 and 3 had lower mortality hazards than those in the lowest-activity tertile. Those in Tertile 3 did not consistently survive longer than those in Tertile 2.
The bottom panel of Table 2 shows the relation between MVPA and mortality. Again, those in higher-activity tertiles had large survival advantages over those with the least MVPA. A comparison of the top and middle panels to the bottom panel shows that the magnitude of the survival advantage among those in the second and third tertiles of MVPA is similar to those in the second and third tertiles of light activity. An examination of variance inflation factors for the physical activity variables indicates that multicollinearity did not seriously affect the results shown in Table 2 (see Table, Supplemental Digital Content 3, which shows VIF for physical activity variables).
Maximum-likelihood analogs to the survey design-based models shown in Table 2 were used to assess model fit (see Table, Supplemental Digital Content 4, which shows model fit statistics). The differences between Models A and B were small; however, for total activity, light activity, and MVPA, Model B consistently had a somewhat higher log-likelihood and somewhat lower AIC and BIC than Model A, indicating a better fitting model. Model C had higher log-likelihood values and much lower AIC and BIC, indicating that excluding individuals who had mobility limitations or chronic conditions at baseline improved the fit of the model.
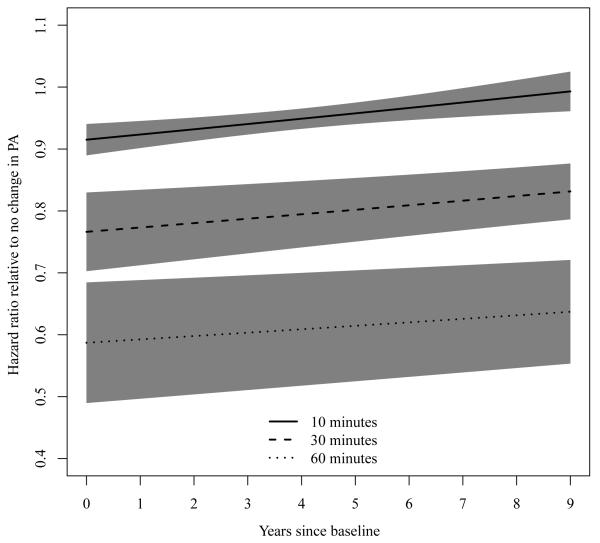
Table 3 shows the hazard ratios in the isotemporal substitution models of physical activity intensity time. The interaction between time and minutes of light activity was significant at alpha=0.05, meaning the theoretical effects of replacing sedentary minutes with light-activity minutes changed over the course of the follow-up period. Holding constant the full set of covariates (Model B), daily replacement of 10 minutes of sedentary time with a 10 minute increase in light activity time was associated with an 8% reduction in mortality risk after one year of follow-up (HR = 0.92, 95% CI: 0.90, 0.95; top panel, Model B, linear combination of coefficients on light activity and interaction term). For comparison, replacing 10 minutes of sedentary time with 10 minutes of MVPA was associated with a 21% reduction in mortality risk (HR = 0.79, 95% CI: 0.63, 0.99, top panel, Model B); however, the difference between light activity and MVPA as replacements for sedentary time was not statistically significant (P=0.197).
Table 3.
Association between Minutes of Light Activity and Mortality: Isotemporal Substitution Models.
| Model A | Model B | Model C | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Replacing 10 Sedentary Minutes | ||||||
| Light Minutes | 0.90 | [0.88,0.93] | 0.92 | [0.89,0.94] | 0.91 | [0.86,0.96] |
| Interaction: (Light Minutes)*(years) | 1.01 | [1.01,1.02] | 1.01 | [1.00,1.01] | 1.01 | [1.00,1.03] |
| MVPA Minutes | 0.73 | [0.57,0.94] | 0.79 | [0.63,0.99] | 0.70 | [0.57,0.85] |
| P for difference (Light - MVPA) | 0.098 | 0.197 | 0.012 | |||
| Replacing 10 MVPA minutes | ||||||
| Light Minutes | 1.23 | [0.96,1.58] | 1.15 | [0.92,1.44] | 1.30 | [1.06,1.59] |
| Interaction: (Light Minutes)*(Years) | 1.01 | [1.01,1.02] | 1.01 | [1.00,1.01] | 1.01 | [1.00,1.03] |
| Sedentary Minutes | 1.36 | [1.06,1.75] | 1.26 | [1.01,1.58] | 1.43 | [1.17,1.74] |
| P for difference (Light - Sedentary) | <0.001 | <0.001 | <0.001 | |||
Abbreviations: HR, hazard ratio; CI, confidence interval; Light, Light activity (counts per minute 100-2,019), MVPA, moderate to vigorous physical activity (counts per minute > 2,019).
Subjects aged 50 to 79 (last birthday) at baseline; mortality follow-up through 2011 (n=3,029).
Models (A) adjust for baseline age, sex, race/ethnicity, education, and minutes of device wear-time. Models (B) additionally adjust for body mass index (kg/m2), smoking, and the presence of diabetes, coronary heart disease, congestive heart failure, stroke, cancer, and mobility limitation. Model (C) excludes those with prevalent chronic illnesses (diabetes, coronary heart disease, congestive heart failure, stroke, and cancer) or mobility limitations at baseline (n=1,424). Models incorporate sampling weights and complex survey characteristics of NHANES.
P-Values for differences are computed using a t-test of the linear combination βLight – βMVPA or βLight – βSed with the null hypothesis that this quantity is zero.
The lower panel of Table 3 shows that replacing 10 daily minutes of MVPA with 10 minutes of light activity was associated with a 17% increase in mortality risk after one year of follow-up (HR = 1.17, 95% CI: 0.93, 1.45; lower panel, Model B, linear combination of coefficients on light activity and interaction term). However, in contrast to physical activity variables in other models, physical activity variables in models of replacement of MVPA had a high degree of multicollinearity (see Table, Supplemental Digital Content 3, which shows variance inflation factors for all models), because MVPA comprised such a small portion of the average day (Table 1). The high degree of multicollinearity is reflected in the wide confidence intervals in the lower panel of Table 3.
A comparison of Model A to Model B within each panel in Table 3 shows that the association between light activity and mortality changed minimally with the inclusion of health-related covariates such as BMI and the presence of comorbid conditions. The results were also similar when those with mobility limitations or chronic diseases at baseline were excluded (Model C). A hazard ratio of greater than 1 for the interaction between follow-up time and minutes of light activity indicates that the positive effects of replacing sedentary minutes with light-activity minutes declined over time. Log likelihood, AIC, and BIC (see Table, Supplemental Digital Content 4, which shows model fit statistics) all show the same patterns they did with the activity-tertile models: a slight improvement in fit from Model A to Model B, and the best fit with Model C.
Figure 2 shows the relative reduction in mortality risk associated with replacing sedentary time with light activity time. Hazard ratios and their confidence intervals are plotted over the follow-up period from baseline to 9 years, for replacements of 10, 30, and 60 minutes of sedentary time with light activity time. The hazard ratio of 1 represents the population baseline hazard (i.e., no change in activity). From that point there was a graded decline in mortality risk due to replacing sedentary time with progressively more minutes of light activity. For example, replacing 30 minutes of daily sedentary time with 30 minutes of light activity time (dashed lines) was associated with a 20% reduction in mortality risk after 5 years of follow-up (HR = 0.80, 95% CI: 0.75, 0.85), while replacing 60 minutes of daily sedentary time with 60 minutes of light activity (dotted lines) was associated with a 39% reduction in mortality risk after 5 years of follow-up (HR = 0.61, 95% CI: 0.53, 0.70). The positive slope of each curve implies that over time, the positive effect of replacing sedentary minutes with light activity minutes on mortality risk diminishes. However, the mortality benefits persist throughout the duration of follow-up, and after 9 years of follow-up, the hazard ratio remained below 1.
Figure 2.
Hazards of death, relative to baseline activity levels, associated with replacing minutes of sedentary time with minutes of light activity.
National Health and Nutrition Examination Survey, 2003-2006. Subjects aged 50 to 79 (last birthday) at baseline; mortality follow-up through 2011 (n=3,029). Figure 2 is based on a Cox proportional hazards model of time to death as a function of minutes of light activity, adjusted for total minutes of device wear-time, minutes of moderate-to-vigorous physical activity, and for baseline age, sex, race/ethnicity, education, smoking, body mass index, mobility limitations, and prevalent chronic disease (congestive heart failure, coronary heart disease, diabetes, stroke, cancer). Solid lines: Replacement of 10 minutes daily of sedentary time with light activity; Dashed lines: Replacement of 30 minutes daily; Dotted lines: 60 minutes. Black lines: Point estimates; Gray areas: 95% confidence interval.
In a sensitivity analysis, all survival models were stratified by sex. Sex-stratified results were similar to results for men and women combined. Greater volumes of total and light activity and MVPA were associated with longer survival. The theoretical replacement of 30 minutes of sedentary time with 30 minutes of light activity time was associated with reduced mortality after 5 years of follow-up (HR=0.74, 95% CI: 0.66, 0.84 for females; HR=0.84, 95% CI: 0.77, 0.92 for males), and these beneficial associations declined somewhat over time.
DISCUSSION
This study shows that a greater volume (counts) of total activity is associated with lower mortality, and greater light activity is also associated with lower mortality independent of MVPA. It also reinforces prior research showing that greater MVPA is independently associated with lower mortality. The study shows that replacing minutes of sedentary time with minutes of light activity or MVPA is associated with lower mortality.
Three previous studies used NHANES accelerometry data to assess the relation between sedentary time and mortality (2, 11, 27), and all found that greater sedentary time was associated with higher mortality risk, independently of MVPA. However, because of a short follow-up period (through 2006 only), the results of these studies could be due to reverse causality, whereby individuals who were already sick and dying at the time of the NHANES observation were more likely than others to have long durations of sedentary time. Our study contributes to the literature by showing via a theoretical model that the protective effects of replacing sedentary time with higher-intensity activity endured almost nine years after physical activity was measured. The long follow-up period in our study, along with obtaining similar results when subjects with mobility limitations or chronic diseases at baseline were excluded, reduces the probability that reverse causality explains our results and demonstrates the long-term predictive power of physical activity for mortality. The other contribution of this study is showing that greater total activity volume, regardless of time spent in any particular intensity, is a strong predictor of mortality over a long follow-up period.
Our results show that as a substitute for sedentary time, light activity would be associated with a smaller mortality decline than MVPA. However, this result was not statistically significant in all models (see top panel of Table 3); furthermore, it is likely that more people are able to replace sedentary time with light activity than are able to replace sedentary time with MVPA. Thus the population attributable effect of exchanging sedentary time for light activity time could be substantial not only for mortality but also for the morbidity and disability that underlies increased risk of death. This latter effect may be particularly important for the older population, who spend much of the day sedentary with limited MVPA. It may be realistic to encourage adults to replace some sedentary time with light activity, rather than focusing solely on increasing MVPA (26). Randomized clinical trials involving exercise regimens show that long-term adherence is often difficult (30), and older adults face additional barriers to maintaining exercise regimens (3). Therefore, for older adults, light activity is most often the alternative to sedentary behavior (23).
One recent substitution analysis on a longitudinal cohort of Australian adults aged 45 and older reported benefits of replacing sedentary time with walking and MVPA, though time spent in different activities was self-reported (31). Our results are also consistent with a large (n>200,000) prospective cohort study in the United States finding that self-reported sedentary time is positively associated with mortality, independent of MVPA (15). A systematic review of studies based on self-reported physical activity found that the largest survival benefit was associated with moving from no activity/sedentary to low levels of activity (40); our results buttress this claim by showing that the survival differences between those in Tertile 1 and those in higher-activity tertiles were larger than the survival differences between Tertiles 2 and 3. Consistent with our findings, the results of past studies suggest that physical activity did not have to be vigorous to be beneficial for older adults (40).
Several limitations must be noted. Most importantly, as an observational study, it is subject to unmeasured confounding. It is possible that, for unmeasured reasons, the same individuals who tend to engage in low levels of light activity are at high risk of mortality. However, the fact that HR estimates did not change meaningfully upon adjustment for health-related covariates in the regression model, including the presence of a number of chronic diseases (Tables 2 and 3), reduces the probability that unmeasured confounding explains the result.
Two limitations are associated with categorizing time into postural or intensity categories. Sedentary behavior is usually defined by a sitting posture, but the accelerometry data do not capture posture; thus, standing could be misclassified as sedentary behavior (10, 15). If standing is protective against mortality relative to sitting, as one large longitudinally study has recently shown (31), then this limitation of accelerometry suggests that our results understate the true benefit of shifting from sedentary to light activity. Second, our categorization of activity based on specific cut-points is consistent with most accelerometer-based studies of physical activity (25) and facilitates comparison with past studies. However, estimates of time spent in different intensity categories are highly sensitive to selected cut-points, and recent research suggests that appropriate cut-points for moderate and vigorous activity may depend on age and cardiorespiratory fitness (18, 24, 32, 38). By limiting the sample to older adults, our study limits the sensitivity of results to specific cut-points (28). Furthermore, the similarity of our study’s results using total activity, which does not depend on cut-points in accelerometer counts, to the results using light activity (Figure 1 and Table 2) suggests that the study results are not sensitive to the choice of cut-points to classify activity intensity.
Strengths of the study include the nationally representative sample, objectively measured activity data, the prospective cohort design, and the ability to follow the cohort for almost nine years for mortality and measure time to death in months. Additionally, we explicitly model the changes in mortality associated with engaging in more light activity at the “expense” of either time spent in sedentary behavior or MVPA, and we show that the role of light activity depends on what type of activity it displaces.
In conclusion, our results support the importance of light-intensity physical activities among adults aged 50 to 79 and reinforce prior findings linking greater MVPA with lower mortality. Future public health recommendations may need to emphasize the health benefits of light activity in comparison to sedentary behavior, without downplaying the protective value of MVPA.
Supplementary Material
Supplemental Digital Content 2. Figure showing Kaplan-Meier survival curve by tertile of MVPA. pdf
Supplemental Digital Content 1. Table showing descriptive statistics of full NHANES 2003-2006 sample aged 50-79, including those excluded from analytic sample due to lack of valid physical activity data. pdf
Supplemental Digital Content 4. Table showing model fit statistics corresponding to models presented in main text. pdf
Supplemental Digital Content 3. Table showing variance inflation factors for models presented in main text. pdf
Acknowledgments
This work was supported by the Intramural Research Program at the National Institute on Aging, National Institutes of Health, and by Grant Number R01AG040212 from the National Institute on Aging.
We are grateful to Eric Shiroma of the National Institute on Aging, National Institutes of Health; the Statistical Methods and Applications for Research in Technology working group at Johns Hopkins University, Bloomberg School of Public Health; Paul Allison and Samuel Preston of the University of Pennsylvania; Andrew Stokes of Boston University; and two anonymous reviewers for their helpful comments.
The results of the present study do not constitute endorsement by ACSM.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81. doi: 10.1249/MSS.0b013e31821ece12. PubMed PMID: 21681120. [DOI] [PubMed] [Google Scholar]
- 2.Beddhu S, Wei G, Marcus RL, Chonchol M, Greene T. Light-Intensity Physical Activities and Mortality in the United States General Population and CKD Subpopulation. Clin J Am Soc Nephrol. 2015;10(7):1145–53. doi: 10.2215/CJN.08410814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belza B, Walwick J, Shiu-Thornton S, Schwartz S, Taylor M, LoGerfo J. Older Adult Perspectives on Physical Activity and Exercise: Voices from Multiple Cultures. Preventing Chronic Disease. 2004;1(4):12. [PMC free article] [PubMed] [Google Scholar]
- 4.Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–32. doi: 10.7326/M14-1651. PubMed PMID: 25599350. [DOI] [PubMed] [Google Scholar]
- 5.Chomistek AK, Cook NR, Flint AJ, Rimm EB. Vigorous-intensity leisure-time physical activity and risk of major chronic disease in men. Med Sci Sports Exerc. 2012;44(10):1898–905. doi: 10.1249/MSS.0b013e31825a68f3. PubMed PMID: 22543741; PubMed Central PMCID: PMC3445709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamer M, de Oliveira C, Demakakos P. Non-exercise physical activity and survival: English longitudinal study of ageing. Am J Prev Med. 2014;47(4):452–60. doi: 10.1016/j.amepre.2014.05.044. PubMed PMID: 25049216. [DOI] [PubMed] [Google Scholar]
- 7.Herrmann SD, Barreira TV, Kang M, Ainsworth BE. Impact of accelerometer wear time on physical activity data: a NHANES semisimulation data approach. Br J Sports Med. 2014;48(3):278–82. doi: 10.1136/bjsports-2012-091410. PubMed PMID: 22936409. [DOI] [PubMed] [Google Scholar]
- 8.Howard B, Winkler EA, Sethi P, et al. Associations of Low- and High-Intensity Light Activity with Cardiometabolic Biomarkers. Med Sci Sports Exerc. 2015 doi: 10.1249/MSS.0000000000000631. PubMed PMID: 25668400. [DOI] [PubMed] [Google Scholar]
- 9.Hupin D, Roche F, Gremeaux V, et al. Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged >/=60 years: a systematic review and meta-analysis. Br J Sports Med. 2015 doi: 10.1136/bjsports-2014-094306. PubMed PMID: 26238869. [DOI] [PubMed] [Google Scholar]
- 10.Kerr J, Marshall SJ, Godbole S, et al. Using the SenseCam to improve classifications of sedentary behavior in free-living settings. Am J Prev Med. 2013;44(3):290–6. doi: 10.1016/j.amepre.2012.11.004. PubMed PMID: 23415127. [DOI] [PubMed] [Google Scholar]
- 11.Koster A, Caserotti P, Patel KV, et al. Association of Sedentary Time with Mortality Independent of Moderate to Vigorous Physical Activity. PLoS One. 2012;7(6):7. doi: 10.1371/journal.pone.0037696.t001. Epub June 13, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lollgen H, Bockenhoff A, Knapp G. Physical activity and all-cause mortality: an updated meta-analysis with different intensity categories. Int J Sports Med. 2009;30(3):213–24. doi: 10.1055/s-0028-1128150. Epub 2009/02/10. PubMed PMID: 19199202. [DOI] [PubMed] [Google Scholar]
- 13.Lumley T, Scott A. AIC and BIC for modeling with complex survey data. Journal of Survey Statistics and Methodology. 2015;3(1):1–18. doi: 10.1093/jssam/smu021. [DOI] [Google Scholar]
- 14.Martin KR, Koster A, Murphy RA, et al. Changes in Daily Activity Patterns with Age in U.S. Men and Women: National Health and Nutrition Examination Survey 2003-04 and 2005-06. J Am Geriatr Soc. 2014;62(7):1263–71. doi: 10.1111/jgs.12893. Epub 2014/06/26. PubMed PMID: 24962323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95(2):437–45. doi: 10.3945/ajcn.111.019620. Epub 2012/01/06. PubMed PMID: 22218159; PubMed Central PMCID: PMC3260070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matthews CE, Moore SC, Sampson J, et al. Mortality Benefits for Replacing Sitting Time with Different Physical Activities. Med Sci Sports Exerc. 2015;47(9):1833–40. doi: 10.1249/MSS.0000000000000621. PubMed PMID: 25628179; PubMed Central PMCID: PMC4515413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol. 2009;170(4):519–27. doi: 10.1093/aje/kwp163. Epub 2009/07/09. PubMed PMID: 19584129; PubMed Central PMCID: PMC2733862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller NE, Strath SJ, Swartz AM, Cashin SE. Estimating Absolute and Relative Physical Activity Intensity Across Age via Accelerometry in Adults. J Phys Act Health. 2010;18(2):13. doi: 10.1123/japa.18.2.158. PubMed Central PMCID: PMCPMC3292194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moore SC, Patel AV, Matthews CE, et al. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med. 2012;9(11):e1001335. doi: 10.1371/journal.pmed.1001335. Epub 2012/11/10. PubMed PMID: 23139642; PubMed Central PMCID: PMC3491006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Health and Nutrition Examination Survey Data Documentation: Physical Activity Monitor. Hyattsville, MD2007. 2014 Jul 10; Available from: http://wwwn.cdc.gov/nchs/nhanes/2003-2004/PAXRAW_C.htm.
- 21.National Health and Nutrition Examination Survey . National Health and Nutrition Examination Survey: Analytic Guidelines, 1999-2010. Centers for Disease Control and Prevention; Hyattsville, MD: Jul 14, 2014. 2013. Available from: http://www.cdc.gov/nchs/data/series/sr_02/sr02_161.pdf. [Google Scholar]
- 22.National Health and Nutrition Examination Survey NHANES (1999-2010) Public-use Linked Mortality Files (2011) Hyattsville, MD2015. 2015 Mar 5; Available from: http://www.cdc.gov/nchs/data_access/data_linkage_activities.htm.
- 23.Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc. 2010;85(12):1138–41. doi: 10.4065/mcp.2010.0444. Epub 2010/12/03. PubMed PMID: 21123641; PubMed Central PMCID: PMC2996155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ozemek C, Cochran HL, Strath SJ, Byun W, Kaminsky LA. Estimating relative intensity using individualized accelerometer cutpoints: the importance of fitness level. BMC Med Res Methodol. 2013;13:53. doi: 10.1186/1471-2288-13-53. PubMed PMID: 23547769; PubMed Central PMCID: PMC3617038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pedisic Z, Bauman AE. Accelerometer-based measures in physical activity surveillance: current practices and issues. Br J Sports Med. 2014 doi: 10.1001/jama.299.3.308. Epub November 4, 2014. [DOI] [PubMed] [Google Scholar]
- 26.Prince SA, Saunders TJ, Gresty K, Reid RD. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta-analysis of controlled trials. Obes Rev. 2014;15(11):905–19. doi: 10.1111/obr.12215. PubMed PMID: 25112481; PubMed Central PMCID: PMC4233995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmid D, Ricci C, Leitzmann MF. Associations of objectively assessed physical activity and sedentary time with all-cause mortality in US adults: the NHANES study. PLoS One. 2015;10(3):e0119591. doi: 10.1371/journal.pone.0119591. PubMed PMID: 25768112; PubMed Central PMCID: PMC4358950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schrack JA, Zipunnikov V, Goldsmith J, et al. Assessing the “physical cliff”: detailed quantification of age-related differences in daily patterns of physical activity. J Gerontol A Biol Sci Med Sci. 2014;69(8):973–9. doi: 10.1093/gerona/glt199. PubMed PMID: 24336819; PubMed Central PMCID: PMC4095926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schuna JM, Jr., Johnson WD, Tudor-Locke C. Adult self-reported and objectively monitored physical activity and sedentary behavior: NHANES 2005-2006. Int J Behav Nutr Phys Act. 2013;10:126. doi: 10.1186/1479-5868-10-126. Epub 2013/11/13. PubMed PMID: 24215625; PubMed Central PMCID: PMC3828579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Skender ML, Goodrick GK, Del Junco DJ, et al. Comparison of 2-Year Weight Loss Trends in Behavioral Treatments of Obesity. Journal of the American Dietetic Association. 1996;96(4):342–6. doi: 10.1016/s0002-8223(96)00096-x. [DOI] [PubMed] [Google Scholar]
- 31.Stamatakis E, Rogers K, Ding D, et al. All-cause mortality effects of replacing sedentary time with physical activity and sleeping using an isotemporal substitution model: a prospective study of 201,129 mid-aged and older adults. Int J Behav Nutr Phys Act. 2015;12:121. doi: 10.1186/s12966-015-0280-7. PubMed PMID: 26419654; PubMed Central PMCID: PMC4589071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Strath SJ, Pfeiffer KA, Whitt-Glover MC. Accelerometer use with children, older adults, and adults with functional limitations. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S77–85. doi: 10.1249/MSS.0b013e3182399eb1. PubMed PMID: 22157778; PubMed Central PMCID: PMC3292184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thatcher AR, Kannisto V, Vaupel JW. The Force of Mortality at Ages 80 to 120. Odense University Press; Denmark: 1998. [Google Scholar]
- 34.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996-2011. Am J Prev Med. 2011;41(2):207–15. doi: 10.1016/j.amepre.2011.05.004. Epub 2011/07/20. PubMed PMID: 21767729. [DOI] [PubMed] [Google Scholar]
- 35.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3. Epub 2007/12/20. PubMed PMID: 18091006. [DOI] [PubMed] [Google Scholar]
- 36.Tudor-Locke C, Camhi SM, Troiano RP. A Catalog of Rules, Variables, and Definitions Applied to Accelerometer Data in the National Health and Nutrition Examination Survey, 2003–2006. Preventing Chronic Disease. 2012;9:1–16. doi: 10.5888/pcd9.110332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tudor-Locke C, Johnson WD, Katzmarzyk PT. Accelerometer-determined steps per day in US adults. Med Sci Sports Exerc. 2009;41(7):1384–91. doi: 10.1249/MSS.0b013e318199885c. PubMed PMID: 19516163. [DOI] [PubMed] [Google Scholar]
- 38.Watson KB, Carlson SA, Carroll DD, Fulton JE. Comparison of accelerometer cut points to estimate physical activity in US adults. J Sports Sci. 2014;32(7):660–9. doi: 10.1080/02640414.2013.847278. PubMed PMID: 24188163; PubMed Central PMCID: PMC4589136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wolff DL, Fitzhugh EC, Bassett DR, Churilla JR. Waist-Worn Actigraphy: Population-Referenced Percentiles for Total Activity Counts in U.S. Adults. J Phys Act Health. 2014 doi: 10.1123/jpah.2013-0464. Epub June 4, 2014. [DOI] [PubMed] [Google Scholar]
- 40.Woodcock J, Franco OH, Orsini N, Roberts I. Non-vigorous physical activity and all-cause mortality: systematic review and meta-analysis of cohort studies. Int J Epidemiol. 2011;40(1):121–38. doi: 10.1093/ije/dyq104. PubMed PMID: 20630992. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 2. Figure showing Kaplan-Meier survival curve by tertile of MVPA. pdf
Supplemental Digital Content 1. Table showing descriptive statistics of full NHANES 2003-2006 sample aged 50-79, including those excluded from analytic sample due to lack of valid physical activity data. pdf
Supplemental Digital Content 4. Table showing model fit statistics corresponding to models presented in main text. pdf
Supplemental Digital Content 3. Table showing variance inflation factors for models presented in main text. pdf