Abstract
Purpose
To test feasibility and impact of a 10-week after-school exercise program for children with ADHD and/or disruptive behavior disorders (DBD) living in an urban poor community.
Methods
Children were randomized to exercise (n=19) or a comparable but sedentary attention control program (n=16). Cognitive and behavioral outcomes were collected pre-post. Intent-to-treat mixed models tested group × time and group × time × attendance interactions. Effect sizes were calculated within and between groups.
Results
Feasibility was evidenced by 86% retention, 60% attendance, and average 75% maximum heart rate. Group × time results were null on the primary outcome, parent-reported executive function. Among secondary outcomes, between-group effect sizes favored exercise on hyperactive symptoms (d=0.47) and verbal working memory (d=0.26), and controls on visuospatial working memory (d=-0.21) and oppositional defiant symptoms (d=-0.37). In each group, within-group effect sizes were moderate-large on most outcomes (d=0.67 to 1.60). A group × time × attendance interaction emerged on visuospatial working memory (F[1,33]=7.42, p<.05), such that attendance to the control program was related to greater improvements (r=.72, p<.01) while attendance to the exercise program was not (r=.25, p=.34).
Conclusions
While between-group findings on the primary outcome, parent-reported executive function, were null, between-group effect sizes on hyperactivity and visuospatial working memory may reflect adaptations to the specific challenges presented by distinct formats. Both groups demonstrated substantial within-group improvements on clinically relevant outcomes. Findings underscore the importance of programmatic features such as routines, engaging activities, behavior management strategies, and adult attention; and highlight the potential for after-school programs to benefit children with ADHD and DBD living in urban poverty where health needs are high and services resources few.
Keywords: behavior disorders, physical activity, ADHD, executive function, urban poverty
Introduction
Attention deficit hyperactivity disorder (ADHD) and disruptive behavior disorders (DBD) (i.e., oppositional defiant disorder [ODD] and conduct disorder) are the most common mental health disorders in childhood (37). National prevalence estimates range from 3% to 5% for ADHD and 2% to 5% for DBD (31, 52). However, teachers report rates as high as 44% for ADHD and 21% for DBD among African-American students (37). The disorders are highly comorbid; 40% to 65% of children with ADHD also meet criteria for DBD (3). If untreated, children with ADHD and DBD are likely to suffer impairments that persist into adulthood and impact educational, occupational, and relationship outcomes (4). Medication is effective for ADHD and DBD but 20% of children experience side effects (3). Psychosocial interventions are also effective but require extensive time and effort by caregivers, resulting in low utilization rates, especially in urban poor racial/ethnic minority communities (22, 48). Parent reports and neuropsychological tests of executive function distinguish ADHD and non-ADHD children, and children with ADHD and comorbid ODD evidence greater executive dysfunction than children with ADHD alone (3, 41). This clinical characteristic makes physical activity an intriguing adjunct treatment for ADHD and DBD, because research indicates that in typically developing children physical activity disproportionately benefits executive function and the brain areas that support it (50).
A promising but methodologically weak literature specific to ADHD and physical activity has emerged in recent years dominated by acute bout studies (16, 34, 39, 40, 49) and single group (19, 47) and non-randomized trials (7, 33, 55) of regular physical activity. This literature provides preliminary evidence of a transient impact of acute physical activity on cognition, and associations between regular physical activity and cognition in children with ADHD. Notably, even results from non-randomized trials are equivocal: McKune et al. did not detect differences between groups over time (33). Rigorous randomized controlled trials are necessary to establish causal impacts of regular physical activity on ADHD outcomes. To date, one large and two smaller trials have investigated the impact of multi-week physical activity interventions on children with ADHD (8, 20, 21). Unfortunately, none of these studies reported heart rate, provided sufficient levels of activity to meet current guidelines (53), excluded siblings from analyses (sibling pairs are not independent observations), or met CONSORT criteria for reporting of clinical trials (i.e., blind, randomization, power analysis, allocation concealment, specification of primary outcome), thereby limiting interpretation (36). There is also a dearth of randomized trials among urban poor racial ethnic minority youth who are at high risk for behavior problems and subsequent severe adverse outcomes (e.g. incarceration, academic failure) (14).
Kang et al. employed random assignment of 32 children with ADHD and reported greater gains (N=28) on inattention, cooperativeness, working memory, and cognitive flexibility in 6-weeks of “medication and education for behavior control” (N = 15, 50-minutes, bi-weekly, 2 staff) vs. “medication and sports therapy” (N = 13, 90-minutes, bi-weekly, 4 staff) (21). Per protocol analyses excluded 4 children who did not adhere to the assigned conditions. The CONSORT guidance considers a per protocol analysis to be a “non-randomised, observational comparison,” because it compromises randomization by introducing bias (36). In 2015, this same group randomized 35 adolescent males with ADHD to the same conditions. Per protocol analyses, N = 30 with 24% of those initially randomized to sports therapy excluded from analyses for non-adherence, reported greater improvements in brain function and ADHD symptom severity in sports therapy (N = 13, 90-minutes, 3 days/week, 6 staff, 6-weeks) compared to education (N = 17, 50-minutes, biweekly, 2 staff, 6-weeks) (8). In both studies, attendance was not reported and differences between groups in format (active play vs. passive education), staff qualifications, student-to-staff ratios, behavior management strategies, and intervention duration result in multiple confounds that preclude isolation of physical activity's impact on outcomes.
The largest and most rigorous trial of regular physical activity on ADHD to date was Hoza et al. who randomized predominantly white middle class K-2nd grade students at-risk for ADHD (N = 94) and typically developing children (N = 108) to a before-school physical activity program or a structured sedentary attention control program of equal duration (5-days per week, 30-minutes per day, 12-weeks) (20). Both programs used similar behavior management strategies (e.g., praise, effective instruction, token economy), effectively isolating the impact of physical activity. Unfortunately, the study used an unorthodox randomization process (switching group assignment for some children after randomization to re-balance groups rather than stratifying randomization on relevant factors). The authors did not describe who generated the random allocation sequence, allocation concealment, or implementation (36). While intent-to-treat analyses were a strength of the study, last observation carried forward was used to impute missing posttest measures; this commonly used process has been criticized for introducing bias (27, 36, 42). In contrast to the findings from the two smaller trials (8, 21), findings from this trial were essentially null. Among 12 symptom severity, mood, and peer functioning outcomes (none specified as primary) only one, parent-reported inattention severity, was significantly different between intervention groups when ADHD and typically developing children were combined. No differential effects of exercise on ADHD vs. typically developing children were found.
This parallel randomized-controlled trial (“Project Play”) adapted an evidence-based after-school exercise program (26) and tested its feasibility and impact versus a sedentary attention control program for African-American children with ADHD and/or DBD living in an urban poor community. It was hypothesized that feasibility would be demonstrated by 75% retention, 60% attendance, and physical activity intensity at ≥ 75% of estimated maximum heart rate. The treatment group was expected to exhibit greater improvement relative to controls on the primary outcome, parent report on the Behavioral Rating Inventory of Executive Functioning (BRIEF) Global Executive Composite (GEC). Small to medium effect sizes favoring physical activity were expected on secondary outcomes including neuropsychological tests of inhibition and working memory, and parent reports of symptom severity, functional impairment, social skills and problem behaviors.
Methods
Participants
Children with ADHD and/or DBD attending a K-8 elementary school in a predominantly African-American Chicago community were recruited during school events and through an established multiple gating procedure in which teachers refer students struggling with behavior to school staff, who reach out to families to ask if they would be interested in being contacted by the research team (29). Inclusion criteria were: between ages 6 and 12; parental consent and child assent; free of conditions that preclude aerobic activity; and a positive screen of ADHD, ODD, or conduct disorder based upon reports of at least one parent or teacher on the DBD Rating Scale (endorsement of ≥ 6 items on the ADHD inattention scale, ≥ 6 items on the ADHD hyperactivity/impulsivity scale, ≥ 4 items on the ODD scale, or ≥ 3 items on the conduct disorder scale) (38), and Impairment Rating Scale (IRS) (rating ≥ 3 in any of 6 domains: siblings, parents, peers, academics, self-esteem, and family) (12). A positive screen by a teacher on the DBD rating Scale plus a positive screen by the parent on the IRS (or vice versa) would qualify a child for inclusion, consistent with instructions for the measures (12, 38) and prior studies calculating symptom severity using the DBD Rating Scale (24, 44, 45).
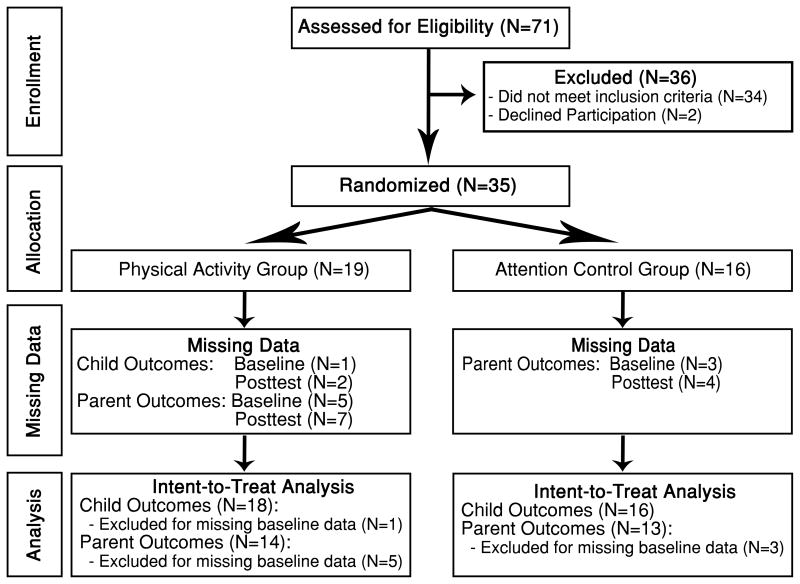
Among 71 participants screened, 35 participants met eligibility criteria and were randomized (Figure 1). Following enrollment, 31 parents/guardians (80% of whom were biological mothers) completed the disruptive disorders section of the National Institute of Mental Health Diagnostic Interview Schedule for Children Version IV (DISC-IV-P), a structured diagnostic interview (43). This interview, which was conducted by 2 graduate student research assistants trained by the PI and study child psychologists (SLF & DR) (13), was not used as an inclusion criterion but to characterize the sample. For each disorder, the DISC-IV-P places children into one of three categories: negative (i.e., minimal symptoms across diagnoses), intermediate (i.e., diagnostic criteria not met, but symptoms and impairments present), or positive (i.e., full DSM-IV criteria met). Participant characteristics are presented in Table 1. Most children met positive or intermediate criteria for ADHD (N=26, 84%), ODD (N=14, 45%), or conduct disorder (N=6, 19%), 32% (N=10) met positive criteria for 2 or more disorders, and 13% (N=4) did not meet positive or intermediate criteria for any disorder. Over half of children (58%) were classified as overweight or obese and only 14% had ever taken medication for their mental health (only 1 was on medication [methylphenidate] during the intervention and his guardian was asked not to provide him his medication on testing days). Importantly, no children changed their medication status during the study.
Figure 1. Participant flow diagram.
Table 1. Baseline demographics, symptom severity, functional impairment, and mental health service use of participants by group.
| Attention Control (N = 16) | Treatment (N = 19) | |
|---|---|---|
|
| ||
| % or M (SD) | % or M (SD) | |
| Child & Parent/Guardian Demographics | ||
| Child Age (years) | 8.7 (2.0) | 9.4 (2.2) |
| Child Male Gender | 69% | 68% |
| Child African-American / Latino | 100% / 6% | 100% / 0% |
| Parent/Guardian Female Gender | 94% | 84% |
| Parent/Guardian Married | 21% | 7% |
| Parent/Guardian Annual Household Income | ||
| $0-$10,000 / $10,001-$20,000 / $20,001-$40,000 | 54% / 23% / 23% | 50% / 25% /25% |
| Parent/Guardian Employed | 43% | 50% |
| Parent/Guardian Highest Education | ||
| < High School / High School Grad / Some College | 25% / 50% / 25% | 54% / 31% / 15% |
|
| ||
| Combined Parent & Teacher Reports on Disruptive Behavior Disorder Rating Scale - Symptom Severity (0-3) | ||
| Inattention | 1.6 (0.8) | 1.5 (0.7) |
| Hyperactivity/Impulsivity | 1.4 (0.7) | 1.4 (0.9) |
| Oppositional Defiant Disorder | 1.4 (0.8) | 1.3 (0.7) |
| Conduct Disorder | 0.3 (0.3) | 0.3 (0.3) |
|
| ||
| Combined Parent & Teacher Reports on Impairment Rating Scale (0-6) | ||
| Domains Endorsed as Impaired | 3.9 (1.7) | 3.7 (1.7) |
|
| ||
| Lifetime Mental Health Service Use | ||
| Seen a Mental Health Provider* | 31% | 7% |
| Medication for Mental Health | 21% | 7% |
| Non-disruptive Comorbidities | 14% | 5% |
|
| ||
| Diagnostic Interview Schedule for Children, Version IV – Parent Interview a | ||
| ADHD Positive / Intermediate Diagnosis | 60% / 33% | 50% / 25% |
| ODD Positive / Intermediate Diagnosis* | 33% / 33% | 25% / 0% |
| CD Positive / Intermediate Diagnosis | 0% / 20% | 6% / 13% |
| Comorbid (multiple positive diagnoses) | 27% | 38% |
|
| ||
| Body Mass Index (BMI) | ||
| Score | 20.2 (5.1) | 23.8 (8.3) |
| Age/Gender Percentile | 72.3 (25.8) | 81.8 (25.3) |
| Normal weight / Overweight / Obese | 47% / 27% / 27% | 36% / 9% / 55% |
Note: No significant differences between groups (t-tests & chi-square) except:
= p < .05.
Procedure
The University of Illinois at Chicago Institutional Review Board and Chicago Public Schools Research Review Board approved study activities. Written informed consent was obtained from participating parents and teachers, and written assent was obtained from participating children. Intervention and data collection activities were completed at the school. Recruitment was conducted during Fall of 2012 and the intervention during Winter of 2013. Baseline data was collected M = 6.2, SD = 16.1 days prior to the intervention start date for child neuropsychological tasks, and M = 39.5, SD = 23.1 days prior for parent report measures. Posttest data was collected M = 4.1, SD = 5.0 days prior to intervention completion for child neuropsychological tasks and M = 18.3, SD = 8.5 days after intervention completion for parent-report measures. After baseline data collection, children were assigned by the study statistician (LFF) using the Microsoft Excel 2010 RAND function with equal allocation ratio (35), to a physically active (n = 19) or sedentary attention control (n = 16) after-school program. To meet family needs, siblings were invited to participate but were not included in the analysis. Research staff blind to condition collected data individually from parents and children during school and after-school hours. Only the parent/guardian that completed measures at baseline was allowed to complete measures at posttest. Teachers completed eligibility screening questionnaires on their own time. Teacher report was excluded for program outcomes due to a low response rate during eligibility screening (data received for only 15 children).
Interventions
Children in each group met for ten weeks in separate classrooms after school from 3:15-6:00 pm on school days (five days per week). Lead instructors were five graduate students from Kinesiology, Nursing, Public Health, and Pharmacy with prior experience working with children (e.g., Girl Scout Troop leader, special education teacher, obesity prevention program coordinator, sports coach, dance instructor). Assistant instructors were 8 undergraduate students from Kinesiology, Premedicine, and Psychology with prior experience working with children (e.g., younger siblings and cousins, church service, youth sports, tutoring, mentoring, and working as nannies and babysitters). Instructors received 16 hours of training on study activities and behavior management strategies with the PI (E.E.B) and clinical child psychologist (D.R.) (14). Trainings focused on conceptual issues related to behavior management and were adapted from trainings led by Dr. Frazier's research team throughout Chicago Park District (CPD) sites (14). Sample themes included, utilizing simple and clear rules and instructions, using “do” as opposed to “don't” commands, “catch 'em being good,” be proactive not reactive, give attention to desirable behaviors, ignore undesirable behavior, prepare engaging age-appropriate activities (by definition children cannot be engaged in the activity and simultaneously misbehaving). Training also focused on specific instruction in study behavior management techniques, such as the good behavior game, token economy, stars of the day, and good news notes. In each case, the concepts were reviewed and practiced through role play, with time allocated afterwards for feedback and discussion. Ongoing daily supervision and weekly staff meetings with the PI provided opportunities to review the previous week, plan for the upcoming week, troubleshoot problems, and seek consultation from study clinical child psychologists (D.R. and S.L.F.).
Instructors were rotated between groups to balance exposure to staff. Student-to-staff ratios were maintained at 4 to 6 students per instructor. Both groups followed the same routine: 15-min. snack/transition, 45-min. homework, 15-min. transition to school gymnasium (treatment) or room for sedentary play (controls). Children then participated in 60-min. of structured play followed by 30-min. of unstructured play. The experimental manipulation occurred during structured play. In the physical activity group, structured play consisted of staff-led cooperative and competitive physically active games and modified sports aimed at maximizing participation and aerobic activity, with alternatives (e.g., jump rope) offered along the periphery (26) (activities manual available upon request). During the physical activity group's structured play time, children wore heart rate monitors (Polar FT1 heart rate monitor; Polar-T31 coded chest strap) and earned tickets as part of a token economy for achieving higher average heart rates (i.e., 130-139 beats per minute = 1 ticket, 140-149 beats per minute = 2 tickets, etc.). Structured play in the control group consisted of a staff-led art project and sedentary alternatives along the periphery (e.g., Legos, cards, puzzles, board games). Children earned tickets for participation in the arts and crafts activities (e.g., used supplies correctly, cleaned up area). Tickets were redeemable for prizes every other week in both groups. Prizes were an assortment of inexpensive (≤ $1.00) small items (e.g., pencils, stickers, rubber toys, yo-yo's, bubble makers, puzzles, whoopee cushions, slime, goop, etc.). Larger prizes (≤ $10.00) (e.g., basketballs and footballs) were available for larger ticket amounts.
Three strategies helped to minimize disruptive behaviors in both conditions: 1) four rules posted on walls and reviewed at the beginning of each rotation (i.e., respect people, places, and things; be where you are supposed to be; follow directions; participate with a positive attitude); 2) Good Behavior Game, a group contingency-based behavior management system in which children could win pizza parties; and 3) Good News Notes and Stars of the Day Awards sent home to parents praising good behavior (14). We supplemented these with a staff member designated each day as a hallway monitor, a supervised timeout room, and a five-strike offense contract system for serious violations (e.g., physical aggression) that included parent meetings and suspensions and culminated in expulsion. The parent handbook and intervention manual are available upon request.
Measures
Health
Within the treatment group, baseline aerobic fitness and estimated maximum heart rate were measured using the 15 meter Progressive Aerobic Cardiovascular Endurance Run (PACER) (30). The 20 meter shuttle run has demonstrated validity and reliability from ages 8-19 (5) and has been utilized in children as young as 6-years-old (6). The 15 meter shuttle run used in the current study has demonstrated classification agreement with the 20-meter test of 92% among 5th grade boys and 87% among 5th grade girls (32). The 15-meter shuttle run was used in the current study because the school gymnasium was too small for the 20-meter test. Weight was measured with a balance beam scale (Health o meter®) calibrated with standard weights and reported to the quarter pound. Height was measured with a stadiometer to the 1/16 inch. Participants were standing in light clothing and without shoes. Body Mass Index (BMI) was calculated and percentile and weight status evaluated according to CDC growth charts for the United States.
Demographics
Parents reported child age, gender, race, and medications and parent marital status, education, income, and employment status.
Feasibility and Participation Indicators
On a daily basis, staff recorded attendance and tickets earned, stars of the day, good news notes, suspensions, and offense contracts in both groups. Beginning in the third week, staff also recorded average heart rate and highest heart rate achieved each day during the 60-min daily structured physical activity session in the group assigned to PA. Average percentage of maximum heart rate was calculated by dividing the highest average heart rate achieved during the PACER test from the average observed daily heart rate during the program. At posttest, parents reported children's participation in other after-school programs during the study, changes in medication status, psychiatric hospitalization, and police arrests. Parent blind was measured at posttest with a single item, asking their child's assignment: a) physical activity, b) arts & crafts, or c) don't know.
Executive Function
Parents completed the primary outcome, the BRIEF (17), reporting real-world manifestations of executive function at baseline and posttest. Lower T-scores on the BRIEF are adaptive. The validity of the BRIEF has been previously established in children with ADHD (17). Secondary executive function outcomes included the STOPIT task, a test of inhibition that distinguishes ADHD and non-ADHD children via performance differences (ADHD children average reaction times of 367 milliseconds, while typically developing children average 275 milliseconds) that are ameliorated with methylphenidate (28, 54), and the Automated Working Memory Assessment System – Short Version (AWMA-S) (1), which provides automated Standard Scores (M = 100, SD = 15) of verbal and visuospatial working memory (1). Lower scores on the STOPIT task, and higher scores on the AWMA are considered advantageous.
Mental Health
Parent reports on the DBD Rating Scale (symptom severity, 0-3) and IRS (domains impaired, 0-6, see inclusion criteria) were used as additional secondary outcomes of mental health. Parents also completed the Social Skills Improvement System (SSiS), which assesses social skills and problem behaviors of their child on a standardized scale (M = 100, SD = 15) (18). Higher scores are adaptive for social skills and maladaptive for problem behaviors.
Analyses
Power analysis was based upon a large effect size (d = 0.82) observed on the BRIEF GEC in the first wave of a trial randomizing typically developing overweight children to physical activity or sedentary attention control (26). At a one-tailed alpha of .05, an estimated power of 0.80 required a sample size of 20 per group to detect a group × time interaction (9). As a pilot study, this trial was not powered to identify significant differences on secondary outcomes but to establish feasibility and effect sizes to inform future research. Linear mixed effects models were run separately for each outcome as dependent variable and performed with three base factors: group (0 = control, 1 = treatment), time (1 = baseline, 2 = posttest), and interaction of group and time (group × time). Participant nested within group was considered a random effect. Children were included in mixed models only on variables for which they or their parents provided data at baseline, whether or not they were adherent to the assigned intervention or provided data at posttest (Figure 1). One child in the physical activity group did not complete neuropsychological testing at baseline, three parents in the control group and five parents in the physical activity group did not complete parent report measures at baseline; these cases were excluded from analyses only on the outcomes for which they had not provided baseline values. Mixed models handle attrition in an intent-to-treat manner, by including all available data regardless of missing data, and each child's data contributes to the model through a random effect of participant (15, 27). Thus, imputation of missing values was not necessary and was not conducted. Non-normal outcomes were log10 transformed. Within-group and between-group effect sizes (Cohen's d) were calculated using pooled standard deviations (9). Exploratory mixed models investigated the interaction of group, time, and attendance (group × time × attendance) and were followed up by correlations between attendance and change scores in each group to assess dose-response.
Results
Table 1 presents baseline demographics, symptom severity, functional impairment, and mental health service use of participants by group. Table 2 presents measurements obtained during the intervention. Feasibility goals were met with 86% retention and 60% (3 days/week) attendance, including children that were expelled or withdrew from the program (N = 5). Heart rate data was recorded on 71% of days that children were present from weeks 3-10. Heart rate monitors indicated a daily average of M = 141 beats per minute, SD = 17 beats per minute and average daily high of M = 193 beats per minute, SD = 10 beats per minute (75% and 103% of estimated maximum heart rate, respectively), reflecting predominantly vigorous physical activity. Children in the exercise program did not maintain a constant heart rate during exercise in the manner adults participating in aerobic exercise would but instead vacillated between brief periods of vigorous activity and rest in a manner akin to adult interval training. There were no significant differences between groups on attendance, disciplinary action, participant characteristics, or incentives received. A quarter of parents correctly identified their child's group assignment, a rate worse than chance (p = .01).
Table 2. Measurements Obtained During the Intervention, Mean (SD) or %.
| Attention Control (N = 16) | Physical Activity (N = 19) | |
|---|---|---|
| Participation Indicators | ||
|
| ||
| Attendance (% days attended) | 67% (17%) | 54% (31%) |
| Withdrew from study, No. | 0 | 2 |
| Expelled, No. | 2 | 1 |
| Retention | 88% | 84% |
| Progressive Aerobic Cardiovascular Endurance Run | ||
| Laps | - | 12.7 (4.9) |
| Healthy Fitness Zone | ||
| Needs Improvement – Health Risk | - | 50% |
| Needs Improvement | - | 50% |
| Maximum Heart Rate Achieved | - | 188.1 (10.2) |
| Heart Rate Monitors | ||
| Average Heart Rate, beats per min. | - | 140.6 (17.2) |
| Average % Maximum Heart Rate | - | 75 (5) |
| Average Highest Heart Rate Achieved, beats per min. | - | 193.1 (10.0) |
| Average Highest % Maximum Heart Rate Achieved | - | 103 (5) |
| Behavior Management Strategies | ||
| Good News Notes awarded per student | 0.8 (0.6) | 0.7 (1.0) |
| Stars of the Day awarded per student | 1.6 (1.4) | 0.9 (1.1) |
| Tickets earned in token economy per student | 258.3 (96.0) | 209.6 (140.0) |
| Pizza parties earned through Good Behavior Game, No. | 2 | 2 |
| Offense contracts per student | 2.5 (1.8) | 1.9 (2.1) |
| Days suspended per student | 2.7 (3.4) | 2.9 (4.0) |
|
| ||
| Potential Confounders | ||
|
| ||
| Enrolled in other program simultaneously | 21% | 15% |
| Psychiatric hospitalization, No. | 1 | 1 |
| Police arrests, No. | 1 | 3 |
Note: there were no significance differences between groups (t-tests & chi-square).
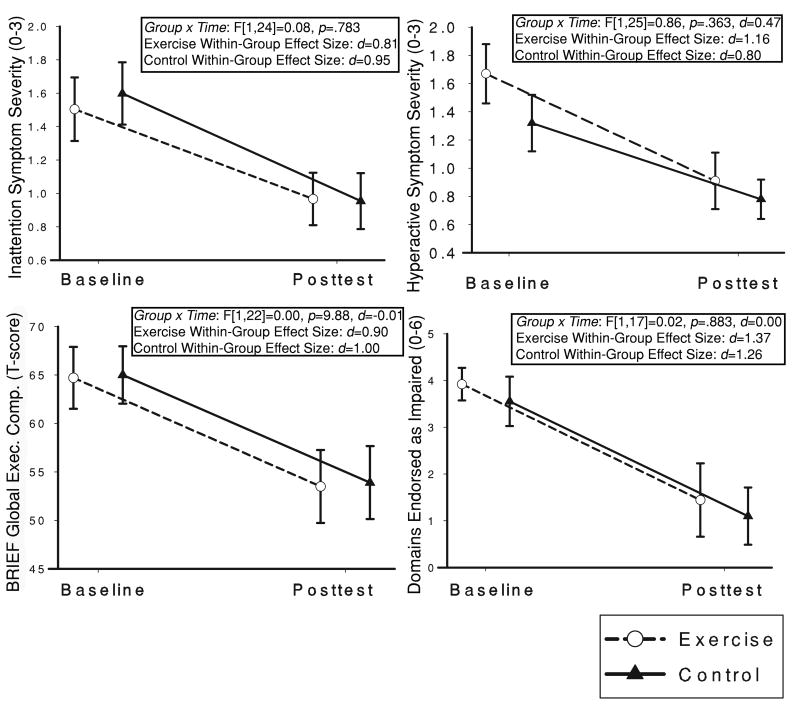
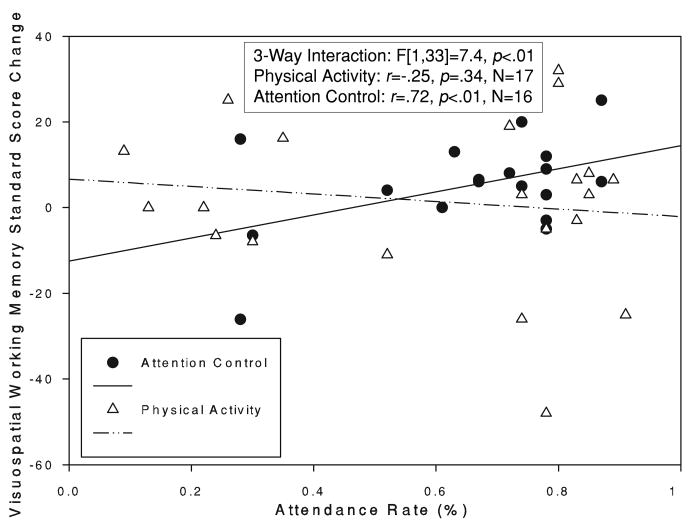
Figure 2 and Table 3 present means, standard deviations, effect sizes, and mean differences for group × time analyses. The group × time interaction was small and not significant for the primary outcome, BRIEF GEC (F[1, 22] = 0.00, p = .988, d = -0.01). Among secondary outcomes, a moderate between-group effect size favored physical activity on hyperactivity / impulsivity (d = 0.47), while small between-group effects favored physical activity on verbal working memory (d = 0.26) and controls on visuospatial working memory (d = -0.21) and ODD severity (d = -0.37). Figure 3 presents a significant group × time × attendance interaction which emerged on visuospatial working memory (F[1,33] = 7.4, p < .01) such that attendance to the control program was related to improvements in visuospatial working memory (r = .72, p < .01) while attendance to the exercise program was not (r = -.25, p = .34) (Figure 3). Within-group effect sizes were moderate to large on most outcomes across groups (d = 0.67 to 1.60) (Table 3).
Figure 2. Group × time interactions on parent reported executive function, attention-deficit/hyperactivity disorder symptom severity, and functional impairment.
Table 3. Means & Standard Deviations, Effect Sizes (Cohen's d), and Linear Mixed Effects Model.
| Attention Control | Physical Activity | Group × Time | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Baseline M (SD) | Posttest M (SD) | WG Effect Size | Baseline M (SD) | Posttest M (SD) | WG Effect Size | Mean Difference | Mean Difference (95% CI) | BG Effect Size | |
| Neuropsychological Tasks | |||||||||
|
| |||||||||
| (n = 16) | (n = 18) | ||||||||
|
| |||||||||
| STOPIT Inhibition (ms) | 450 (246) | 292 (153) | 0.77 | 550 (285) | 370 (247) | 0.67 | -22a | (-101, 57.3) | -0.09 |
| AWMA Verbal | 92 (16) | 92 (14) | -0.01 | 90 (14) | 93 (8.1) | 0.29 | 3.5 | (-1.0, 7.9) | 0.26 |
| AWMA Visuospatial | 91 (13) | 96 (15) | 0.36 | 93 (16) | 95 (17) | 0.11 | -3.2 | (-8.2, 1.8) | -0.21 |
|
| |||||||||
| Parent Report | |||||||||
|
| |||||||||
| (n = 13) | (n = 14) | ||||||||
|
| |||||||||
| BRIEF GEC T-score | 65 (10) | 54 (12) | 1.00 | 65 (12) | 54 (13) | 0.90 | -0.11 | (-4.0, 3.8) | -0.01 |
| Inattention Severity (0-3) | 1.6 (0.7) | 1.0 (0.6) | 0.95 | 1.5 (0.7) | 1.0 (0.5) | 0.81 | 0.10 | (-0.1, 0.3) | -0.16 |
| Hyperactivity Severity (0-3) | 1.3 (0.7) | 0.8 (0.5) | 0.80 | 1.7 (0.7) | 0.9 (0.6) | 1.16 | -0.30 | (-0.5, -0.1) | 0.47 |
| ODD Severity (0-3) | 1.3 (0.6) | 0.6 (0.2) | 1.60 | 1.4 (0.5) | 0.9 (0.7) | 0.79 | 0.20 | (0.02, 0.4) | -0.37 |
| Impaired Domains (0-6) | 3.6 (1.6) | 1.1 (2.3) | 1.26 | 3.9 (1.3) | 1.4 (2.4) | 1.37 | 0.00a | (-0.6, 0.6) | 0.00 |
| Social Skills | 86 (14) | 92 (15) | 0.45 | 91 (12) | 97 (15) | 0.47 | -0.20 | (-4.7, 4.3) | 0.01 |
| Problem Behaviors | 120 (14) | 104 (12) | 1.23 | 120 (23) | 103 (20) | 0.77 | -0.53a | (-6.5, 5.4) | -0.03 |
Note: Effect Size = Cohen's d, small = ≥ 0.20, moderate = ≥ 0.50, large = ≥ 0.80; there were no significance differences between groups in baseline (independent samples t-tests) and no significant group × time interactions. STOPIT = Stop-Signal Inhibition Task, BRIEF GEC = Behavior Rating Inventory of Executive Function Global Executive Composite, AWMA = Automated Working Memory Assessment System, ODD = Oppositional Defiant Disorder, WG = within group, BG = between group. 1 child in the physical activity group did not complete neuropsychological testing at baseline, 3 parents in the control group and 5 parents in the physical activity group did not complete parent report measures at baseline, these values were removed from analyses (Figure 1).
Data log10(x) or log10(x+1) transformed in t-tests and mixed models
Figure 3. Significant group × time × attendance interaction with correlations between attendance and change scores for each group.
Discussion
Results revealed substantial improvements in both groups with a near-zero effect size difference between groups on the primary executive function outcome, the BRIEF GEC. The sample demonstrated low executive function at baseline (e.g., 12th to 28th percentile on the BRIEF, 19th to 36th on AWMA). The majority of children were overweight or obese, with those tested at low fitness levels. Despite apparent behavioral problems, very few participants had ever been evaluated by a mental health professional or taken medication, which is typical for the low levels of parental income, employment, and education reported. Thus, there was room for improvement on the dependent variable with low exposure to the independent variable.
Despite implementation in a challenging high poverty environment, the trial met or exceeded its feasibility goals. Two students withdrew from the physical activity group in the program's first week, while two others were expelled from the attention control group and one from the physical activity group for repeated serious infractions (e.g., cursing, hitting, throwing furniture) over the course of the program. Previous studies of physical activity for children with ADHD have reported retention rates between 86% and 90% (7, 8, 21), which is in line with the rate observed in the current study. Few after-school alternatives were available in the participating neighborhood, however, roughly 1 in 5 children enrolled in other after-school programs on one or two days per week. These factors along with school suspensions, program suspensions, hospitalizations, and arrests all decreased attendance rates. While no previous studies of physical activity for ADHD have reported attendance as a continuous variable, Smith et al., reported that 86% of children in their study attended at least 75% of sessions, only 37% of children met this criterion in the current study, potentially reflecting differences in program characteristics and sample studied (47). Nevertheless, 71% of children attended the majority of days, and, on average, children attended 3 days per week, which is an acceptable frequency of physical activity intervention in this age group (55). This success was likely due to the convenience for families to leave their child (and siblings) at the school until 6:00pm without charge. The number of positive reinforcements for good behavior far exceeded punishments for misbehavior, reflecting effective implementation of behavior management strategies by undergraduate and graduate students with training and supervision from the PI (EEB) and study child psychologists (SLF & DR).
Observed heart rates during the 60 minute structured play session in the physical activity group fell above the 60% of maximum heart rate goal stated in two previous studies (8, 21) but below the 154-beats per minute average reported in a third study (55). Unfortunately, on over a quarter of days that children were present and participated their heart rate was not recorded. This could have been due to children not beginning heart rate recording when prompted, the chest strap having been placed incorrectly, the watch malfunctioning, or the designated staff member not collecting the watch from the child (e.g., occasionally we found watches simply thrown on the gym floor or children would forget to take them off and wear them home). The low rate of parents correctly identifying their child's group assignment, at posttest, despite being informed after randomization, may be due to the effectiveness with which the study blinded parents to study hypotheses and emphasized equipoise in presentation of study aims.
Despite the overall null effect on the BRIEF, a moderate effect size favored physical activity over the sedentary attention control condition on hyperactivity symptoms, suggesting a potentially unique benefit of aerobic activity on hyperactivity above and beyond features associated with quality after-school programs generally. Additional investigation in a trial powered for this outcome is warranted. In contrast, a small effect size favored the attention control condition on visuospatial working memory, and attendance to the attention control program was related to greater increases on this outcome.
In a review of the executive function intervention literature, Diamond et al. observed that diverse activities, both active and sedentary, generate executive function adaptations specific to the dimension that is stressed (11). The visuospatial working memory finding corresponds with this training specificity theory, and likely reflects overlap between the arts and crafts activities and the spatial recall measure (1). Between-group effects on other secondary outcomes were small or near zero. Concurrently, most within-group effect sizes reflected moderate to large beneficial effects, including reductions in symptom severity between one-third and one-half, functional impairment by more than half, and problem behaviors by a standard deviation. This pattern of results is similar to those of other recent trials utilizing sedentary attention control conditions, encouraging within-group effects over time but null between-group effects (20, 25, 46). This highlights the utilization of a comparable but sedentary attention control comparison group, which rules out alternative explanations for program benefits, including consistent routines, engaging activities, prosocial interaction, adult attention, and behavior management strategies.
The current study built upon the limited existing literature on regular exercise for children with ADHD and/or DBD through attention to important issues of: (a) sample (exclusion of siblings and typically developing children from analyses, inclusion of children with DBD as well as ADHD), (b) provision of a substantial dose of physical activity sufficient to meet current guidelines (53), which was larger [50 hours of structured and 25 hours of unstructured physical activity vs. 18 hours (21), 27 hours (8), and 30 hours (20)] and more vigorous than previous trials [75% of estimated maximum heart rate during structured activity vs. a 60% goal in previous trials (8, 21)], and (c) clinical trial design and reporting considerations (randomization, intent-to-treat analysis, adherence measures, meeting CONSORT reporting standards, comparison to a sedentary attention control program with similar staff and behavior management systems to isolate the impact of physical activity, exclusion of siblings from analyses, standardized cognitive and behavioral outcomes, blinding of data collectors, and specification of primary and secondary outcomes) (36).
The implementation of the trial in a high poverty African-American community with limited access to safe, structured activities, high rates of childhood behavioral disorders, few available mental health services resources, and no representation in the extant literature is a critical feature of the study. An analysis of three national surveys indicated that nearly 80% of low-income youth, and 90% of uninsured youth, in need of mental health services had not received any in the past year (22). For those who do receive services, attrition rates exceed 50%, especially for low-income, African-American children (23). Hence, for children in urban poor communities there are substantial barriers to affordable, accessible, and high quality mental health care (48). Towards this end, after-school physical activity programs have promise as effective place-based interventions to address multiple health outcomes simultaneously (14).
Limitations
Alternate forms were not utilized on neuropsychological tasks administered in this study and thus practice effects on these outcomes cannot be dismissed, though we would not expect this effect to be different between groups due to randomization. Additionally, it was more challenging to obtain data from parents and teachers than children in this high poverty sample, resulting in a slightly smaller sample for parent report vs. child neuropsychology outcomes (Figure 1) and the decision to limit teacher report to eligibility screening only. Difficulty was also encountered in collection of PACER data, which was originally intended to serve three purposes: 1) to describe the fitness level of the sample, 2) to obtain each child's maximum heart rate in order to individualize each child's daily percentage of maximum heart rate, and 3) as a fidelity check to ensure that fitness improved. On the program's first day we tried to collect the PACER in its standard group format but were unable to do so due to behavioral issues. Therefore, we switched to a one-on-one testing format with a data collector conducting the PACER with children one at a time during the after-school program's first week. This placed a considerable strain on both the intervention and data collection staff, as well as the program, and it was decided that we would not pursue this measure in the attention control group at baseline nor in either group at posttest. Thus, the PACER serves to describe the fitness level and individualize heart rate data in the physical activity group only and was not able to serve as a manipulation check.
Furthermore, without a no-intervention control arm, this study cannot rule out that benefits demonstrated in both interventions were due to other factors (e.g., maturation, Hawthorne effect, regression to the mean, etc.). That said, longitudinal studies conducted with children with ADHD and DBD often demonstrate trajectories of escalating problem severity with regard to inattention, conduct, and oppositional defiance when untreated (2, 4) and quasi-experimental studies in ADHD have shown little to no improvement in no-intervention control groups on cognitive and behavioral symptom outcomes in children (7, 55). Both groups received daily homework support, which may have been responsible for a portion of program benefits. Finally, children assigned to the sedentary attention control condition participated in sedentary play activities (e.g., Dominoes) that may have directly challenged aspects of executive function, and while this can also be true in the physically activity games (e.g., basketball drills) (10, 11, 51), in the current study, activities were selected to maximize heart rate, resulting in a high proportion of tag games, races, and calisthenics, as opposed to skill and strategy based physical activities (e.g., team sports) with longer learning curves and more frequent inactive times. Nevertheless, given the broad nature of executive function, it would be difficult to design an engaging intervention, active or sedentary, that does not challenge executive function.
Conclusion
The trial demonstrated that, with proper training and support, undergraduate and graduate students can implement high quality after-school physical activity programs for children with behavioral disorders in a high poverty community. Children in both groups improved on clinically relevant outcomes, though there were few differences between groups. Given finite resources, and in the midst of an unwavering obesity epidemic, it is critical to identify interventions that generate the greatest value for societal investment. To this end, physical activity provides myriad physical health benefits related to prevention of obesity and chronic disease, as well as reduction of risk for mood and anxiety disorders, for all of which children with ADHD and DBD are at risk (4). Physically active games and sports are among the most popular leisure activities in childhood, are cheaply and broadly available, and provide a space that can be engaging, emotionally charged, and ripe with opportunities for learning and forming emotional bonds with prosocial peers and adults (14). This study aligns with an emerging literature on after-school programs with benefits for mental health and social adjustment [e.g., (14)] and suggests that integration of structured behavior management (i.e., clear expectation, reward opportunities, peer reinforcement) into after-school programs, active or sedentary, can maximize participation and benefits for children with ADHD and DBD even in challenging circumstances.
Acknowledgments
The authors would like to acknowledge the graduate and undergraduate students that staffed the program, the school staff, teachers, and administrators that supported it and the children and families that participated, as well as Drs. Adele Diamond, Donald Hellison, and William Pelham for their consultation. Funding was provided by the UIC Department of Kinesiology and Nutrition, NIH grants R01 HL087923 (PI: Davis) and R36 MH093152 (PI: Bustamante). The authors declare no conflict of interest.
The results of the present study do not constitute an endorsement by the American College of Sports Medicine.
Funding was provided by the UIC Department of Kinesiology and Nutrition, NIH grants R01 HL087923 (PI: Davis) and R36 MH093152 (PI: Bustamante). The authors declare no conflict of interest. The results of the present study do not constitute an endorsement by the American College of Sports Medicine.
Footnotes
Medicine & Science in Sports & Exercise® Published ahead of Print contains articles in unedited manuscript form that have been peer reviewed and accepted for publication. This manuscript will undergo copyediting, page composition, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered that could affect the content.
References
- 1.Alloway TP. Automated Working Memory Assessment Manual. London (UK): Pearson Assessment; 2007. p. 87. [Google Scholar]
- 2.Armstrong D, Lycett K, Hiscock H, Care E, Sciberras E. Longitudinal Associations Between Internalizing and Externalizing Comorbidities and Functional Outcomes for Children with ADHD. Child Psychiatry Hum Dev. 2014;45(5):1–13. doi: 10.1007/s10578-014-0515-x. [DOI] [PubMed] [Google Scholar]
- 3.Barkley R. Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. 2. New York (NY): Guilford Press; 1998. p. 628. [Google Scholar]
- 4.Barkley R. Major life activity and health outcomes associated with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2002;63:10–5. [PubMed] [Google Scholar]
- 5.Castro-Piñero J, Artero EG, España-Romero V, et al. Criterion-related validity of field-based fitness tests in youth: a systematic review. Br J Sports Med. 2010;44:934–43. doi: 10.1136/bjsm.2009.058321. [DOI] [PubMed] [Google Scholar]
- 6.Castro-Piñero J, González-Montesinos JL, Mora J, Keating XD, Sjöström M, Ruiz JR. Percentile values for running sprint field tests in children ages 6–17 years: Influence of weight status. Res Q Exerc Sport. 2010;81(2):143–51. doi: 10.1080/02701367.2010.10599661. [DOI] [PubMed] [Google Scholar]
- 7.Chang Y-K, Hung C-L, Huang C-J, Hatfield BD, Hung T-M. Effects of an Aquatic Exercise Program on Inhibitory Control in Children with ADHD: A Preliminary Study. Arch Clin Neuropsych. 2014;29(3):217–23. doi: 10.1093/arclin/acu003. [DOI] [PubMed] [Google Scholar]
- 8.Choi JW, Han DH, Kang KD, Jung HY, Renshaw PF. Aerobic exercise and attention deficit hyperactivity disorder: brain research. Med Sci Sports Exerc. 2015;47(1):33–9. doi: 10.1249/MSS.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen J. Statistical Power for the Behavioral Sciences. 2. Hillsdale (NJ): Lawrence Erlbaum Associates; 1988. p. 590. [Google Scholar]
- 10.Crova C, Struzzolino I, Marchetti R, et al. Cognitively challenging physical activity benefits executive function in overweight children. J Sports Sci. 2014;32(3):201–11. doi: 10.1080/02640414.2013.828849. [DOI] [PubMed] [Google Scholar]
- 11.Diamond A, Lee K. Interventions Shown to Aid Executive Function Development in Children 4 to 12 Years Old. Science. 2011;333(6045):959–64. doi: 10.1126/science.1204529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fabiano GA, Pelham WE, Waschbusch DA, et al. A practical measure of impairment: Psychometric properties of the impairment rating scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. J Clin Child Adolesc. 2006;35(3):369–85. doi: 10.1207/s15374424jccp3503_3. [DOI] [PubMed] [Google Scholar]
- 13.Fisher P, Lucas L, Lucas C, Sarsfield J, Shaffer D. Interviewer Manual. Columbia University DISC Development Group; 2006. [Google Scholar]
- 14.Frazier SL, Chacko A, Van Gessel C, O'Boyle C, Pelham WE. The Summer Treatment Program Meets the South Side of Chicago: Bridging Science and Service in Urban After-School Programs. Child Adolesc Ment Health. 2012;17(2):86–92. doi: 10.1111/j.1475-3588.2011.00614.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gadbury G, Coffey C, Allison D. Modern statistical methods for handling missing repeated measurements in obesity trial data: beyond LOCF. Obes Rev. 2003;4(3):175–84. doi: 10.1046/j.1467-789x.2003.00109.x. [DOI] [PubMed] [Google Scholar]
- 16.Gapin J, Etnier JL. The relationship between physical activity and executive function performance in children with attention-deficit hyperactivity disorder. J Sport Exerc Psychol. 2010;32(6):753–63. doi: 10.1123/jsep.32.6.753. [DOI] [PubMed] [Google Scholar]
- 17.Gioia GA, Isquith PK, Guy SC, Kenworthy L. Test review behavior rating inventory of executive function. Child Neuropsychol. 2000;6(3):235–8. doi: 10.1076/chin.6.3.235.3152. [DOI] [PubMed] [Google Scholar]
- 18.Gresham FM, Elliott SN. Rating Scales Manual: Social Skills Improvement System. Bloomington (MN): Pearson Assessments; 2009. p. 216. [Google Scholar]
- 19.Halperin JM, Marks DJ, Bedard AC, et al. Training Executive, Attention, and Motor Skills: A Proof-of-Concept Study in Preschool Children With ADHD. J Atten Disord. 2012;17(8):711–21. doi: 10.1177/1087054711435681. [DOI] [PubMed] [Google Scholar]
- 20.Hoza B, Smith AL, Shoulberg EK, et al. A Randomized Trial Examining the Effects of Aerobic Physical Activity on Attention-Deficit/Hyperactivity Disorder Symptoms in Young Children. J Abnorm Child Psychol. 2014;43(4):1–13. doi: 10.1007/s10802-014-9929-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kang KD, Choi JW, Kang SG, Han DH. Sports therapy for attention, cognitions and sociality. Int J Sports Med. 2011;32(12):953–9. doi: 10.1055/s-0031-1283175. [DOI] [PubMed] [Google Scholar]
- 22.Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among US children: Variation by ethnicity and insurance status. Am J Psychiatry. 2002;159(9):1548–55. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- 23.Kazdin A. Dropping out of child psychotherapy: Issues for research and implications for practice. Clin Child Psychol Psychiatry. 1996;1(1):133–56. [Google Scholar]
- 24.Kent KM, Pelham WE, Jr, Molina BS, et al. The academic experience of male high school students with ADHD. J Abnorm Child Psychol. 2011;39(3):451–62. doi: 10.1007/s10802-010-9472-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krafft CE, Schaeffer DJ, Schwarz NF, et al. Improved frontoparietal white matter integrity in overweight children is associated with attendance at an after-school exercise program. Dev Neurosci. 2014;36(1):1–9. doi: 10.1159/000356219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krafft CE, Schwarz NF, Chi L, et al. An 8-month randomized controlled exercise trial alters brain activation during cognitive tasks in overweight children. Obesity. 2014;22(1):232–42. doi: 10.1002/oby.20518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lachin JM. Fallacies of last observation carried forward analyses. Clinical Trials. 2015 doi: 10.1177/1740774515602688. 1740774515602688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lijffijt M, Kenemans JL, Verbaten MN, van Engeland H. A meta-analytic review of stopping performance in attention-deficit/hyperactivity disorder: deficient inhibitory motor control? J Abnorm Psychol. 2005;114(2):216. doi: 10.1037/0021-843X.114.2.216. [DOI] [PubMed] [Google Scholar]
- 29.Loeber R, Dishion TJ, Patterson GR. Multiple Gating - a Multistage Assessment Procedure for Identifying Youths at Risk for Delinquency. J Res Crime Delinq. 1984;21(1):7–32. [Google Scholar]
- 30.Mahar MT, Rowe DA, Parker CR, Mahar FJ, Dawson DM, Holt JE. Criterion-referenced and norm-referenced agreement between the mile run/walk and PACER. Meas Phys Educ Exerc Sci. 1997;1(4):245–58. [Google Scholar]
- 31.Maughan B, Rowe R, Messer J, Goodman R, Meltzer H. Conduct disorder and oppositional defiant disorder in a national sample: developmental epidemiology. J Child Psychol and Psyc. 2004;45(3):609–21. doi: 10.1111/j.1469-7610.2004.00250.x. [DOI] [PubMed] [Google Scholar]
- 32.McClain JJ, Welk GJ, Ihmels M, Schaben J. Comparison of two versions of the PACER aerobic fitness test. Journal of Physical Activity & Health. 2006;3:S47. [Google Scholar]
- 33.McKune A, Pautz J, Lomjbard J. Behavioural response to exercise in children with attention-deficit/hyperactivity disorder. South African Journal of Sports Medicine. 2004;15(3):17–21. [Google Scholar]
- 34.Medina JA, Netto TL, Muszkat M, et al. Exercise impact on sustained attention of ADHD children, methylphenidate effects. Atten Defic Hyperact Disord. 2010;2(1):49–58. doi: 10.1007/s12402-009-0018-y. [DOI] [PubMed] [Google Scholar]
- 35.Mélard G. On the accuracy of statistical procedures in Microsoft Excel 2010. Comput Stat. 2014;29(5):1095–128. [Google Scholar]
- 36.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63(8):e1–e37. doi: 10.1016/j.jclinepi.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 37.Nolan EE, Gadow KD, Sprafkin J. Teacher reports of DSM-IV ADHD, ODD, and CD symptoms in schoolchildren. J Am Acad Child Adolesc Psychiatry. 2001;40(2):241–9. doi: 10.1097/00004583-200102000-00020. [DOI] [PubMed] [Google Scholar]
- 38.Pelham WE, Jr, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry. 1992;31(2):210–8. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Piepmeier AT, Shih C-H, Whedon M, et al. The effect of acute exercise on cognitive performance in children with and without ADHD. J Sport Health Sci. 2015;4(1):97–104. [Google Scholar]
- 40.Pontifex MB, Saliba BJ, Raine LB, Picchietti DL, Hillman CH. Exercise improves behavioral, neurocognitive, and scholastic performance in children with attention-deficit/hyperactivity disorder. J Pediatr. 2013;162(3):543–51. doi: 10.1016/j.jpeds.2012.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Qian Y, Shuai L, Cao QJ, Chan RCK, Wang YF. Do executive function deficits differentiate between children with Attention Deficit Hyperactivity Disorder (ADHD) and ADHD comorbid with Oppositional Defiant Disorder? A cross-cultural study using performance-based tests and the Behavior Rating Inventory of Executive Function. Clin Neuropsychol. 2010;24(5):793–810. doi: 10.1080/13854041003749342. [DOI] [PubMed] [Google Scholar]
- 42.Saha C, Jones MP. Type I and Type II error rates in the last observation carried forward method under informative dropout. J Appl Statist. 2015:1–15. [Google Scholar]
- 43.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 44.Sibley MH, Evans SW, Serpell ZN. Social cognition and interpersonal impairment in young adolescents with ADHD. J Psychopathol Behav. 2010;32(2):193–202. [Google Scholar]
- 45.Sibley MH, Pelham WE, Molina BS, et al. Inconsistent self-report of delinquency by adolescents and young adults with ADHD. J Abnorm Child Psychol. 2010;38(5):645–56. doi: 10.1007/s10802-010-9404-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sink KM, Espeland MA, Castro CM, et al. Effect of a 24-Month Physical Activity Intervention vs Health Education on Cognitive Outcomes in Sedentary Older Adults: The LIFE Randomized Trial. JAMA. 2015;314(8):781–90. doi: 10.1001/jama.2015.9617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smith AL, Hoza B, Linnea K, et al. Pilot physical activity intervention reduces severity of ADHD symptoms in young children. J Atten Disord. 2013;17(1):70–82. doi: 10.1177/1087054711417395. [DOI] [PubMed] [Google Scholar]
- 48.Sturm R, Ringel JS, Andreyeva T. Geographic disparities in children's mental health care. Pediatrics. 2003;112(4):e308–e. doi: 10.1542/peds.112.4.e308. [DOI] [PubMed] [Google Scholar]
- 49.Tantillo M, Kesick CM, Hynd GW, Dishman RK. The effects of exercise on children with attention-deficit hyperactivity disorder. Med Sci Sports Exerc. 2002;34(2):203–12. doi: 10.1097/00005768-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 50.Tomporowski PD, Davis CL, Miller PH, Naglieri JA. Exercise and children's intelligence, cognition, and academic achievement. Educ Psychol Rev. 2008;20(2):111–31. doi: 10.1007/s10648-007-9057-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tomporowski PD, McCullick B, Pendleton DM, Pesce C. Exercise and children's cognition: The role of exercise characteristics and a place for metacognition. J Sport Health Sci. 2015;4(1):47–55. [Google Scholar]
- 52.United States Centers for Disease Control and Prevention. Attention-Deficity/Hyperactivity Disorder--A Public Health Perspective. Atlanta, GA: National Center on Birth Defects and Developmental Disabilities, United States Centers for Disease Control and Prevention; 2001. p. 76. Available from: National Center on Birth Defects and Developmental Disabilities. [Google Scholar]
- 53.United States Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, D.C.: United States Department of Health and Human Services, Office of Disease Prevention and Health Promotion; 2008. p. 76. Available from: United States Department of Health and Human Services. [Google Scholar]
- 54.Verbruggen F, Logan GD, Stevens MA. STOP IT: Windows executable software for the stop-signal paradigm. Behav Res Methods. 2008;40(2):479–83. doi: 10.3758/brm.40.2.479. [DOI] [PubMed] [Google Scholar]
- 55.Verret C, Guay MC, Berthiaume C, Gardiner P, Beliveau L. A physical activity program improves behavior and cognitive functions in children with ADHD: an exploratory study. J Atten Disord. 2012;16(1):71–80. doi: 10.1177/1087054710379735. [DOI] [PubMed] [Google Scholar]