Abstract
Objectives
To examine relationships between parental perceptions of child weight and overall health, reported lifestyle behaviors and measured body mass index (BMI).
Methods
Using community-partnered methods, we surveyed families residing in a two census tract area identified for targeted interventions to decrease diabetes related disparities. The survey included demographics, child dietary and physical activity behaviors, and parental perception of child’s health and weight. We measured child BMI using a standardized protocol.
Results
We surveyed parents of 116 children with a mean age of 7 years (range 3–15) with 51 % boys, 74 % Hispanic, and 26 % Black. Over half of the children (55 %) were overweight or obese. Half (50 %) of the parents underestimated their children’s weight. Reported daily hours of walking and/or running trended higher (3.6 vs. 2.6 h, p = 0.08) for children perceived to be of normal weight. Parents who correctly estimated their child’s weight status reported more hours of daily walking/running than parents who underestimated child weight status, 4.5 versus 2.4 h, p = 0.0002. Parents of healthy weight children were more likely to report that children were in excellent or very good health compared to parents of overweight/obese children, 75 versus 56 % respectively (p = 0.04). We found significant racial/ethnic differences in reported diet and physical activity behaviors and perception of overall health.
Conclusions for Practice
Parental perceptions of child health and physical activity level may be related to perceptions of their child’s weight status. Study findings informed community-based initiatives for reducing diabetes risk among children.
Keywords: Children, Parents, Obesity, Diet, Physical activity, Health perception, Weight perception, Race/ethnicity, Community-based participatory research, Diabetes prevention and control, Community health initiative
Introduction
Childhood obesity affects approximately 17 % of children and adolescents in the United States, and there are significant racial/ethnic disparities in obesity rates [25]. Data from New York City public school children demonstrates that the prevalence of obesity in grades K-8 decreased from 21.9 % in 2006–2007 to 20.7 % in 2010–2011 (5.5 % change). However, the decrease was smaller among Black (1.9 %) and Hispanic (3.4 %) children than among Asian/Pacific Islander (7.6 %) and white (12.5 %) children, such that disparities in obesity are widening [7]. Studies have also found racial/ethnic disparities in prevalence of health conditions associated with obesity including metabolic syndrome [5] and diabetes [35].
High rates of childhood obesity and related conditions have led to an abundance of research related to weight loss interventions in children. One Cochrane review showed that combined behavioral lifestyle interventions compared to standard care or self-help can produce a clinically meaningful reduction of weight in overweight children and adolescents [26]. However, such interventions may never be initiated if parents do not correctly identify their children as overweight. Although body mass index (BMI) is the current standard for identifying and monitoring obesity, there are limitations in parents’ understanding of BMI [4]. Parents often incorrectly categorize children as normal weight even when they are considered overweight/obese based on measured BMI [11, 15, 21, 27, 30, 33]. Such misperceptions are more common for younger children and boys, by an overweight or obese parent, and in families that are of minority race/ethnicity and lower socioeconomic status [8, 11–13, 17, 20–22, 30, 33]. Literature is limited regarding how overall perception of a child’s health or reported lifestyle behaviors relate to perception of weight. There is also limited information about racial/ethnic differences in behaviors [34] and weight/health perceptions.
The primary goal of this study was to explore associations between parental perceptions of child weight and general health and reported child health behaviors. A secondary goal was to examine racial/ethnic disparities in these relationships.
Methods
Racial and Ethnic Approaches to Community Health (REACH)
Community and academic partners comprising the Communities Inspired and Motivated to Prevent and Control (IMPACT) Diabetes Center, a CDC Center of Excellence for the Elimination of Health Disparities, chose to focus on contributors to diabetes prevention and control including obesity, healthy eating, and physical activity [6]. The coalition identified a 74 square block geographic area for intensive assessment and targeted health improvement activities, referred to as the Sector of Excellence for Elimination of Disparities (SEED) [9]. After conducting an environmental assessment to explore characteristics of the SEED’s built and food environments [18] and reviewing community health data, partners chose to survey local parents about their children.
Participants
Trained surveyors recruited a convenience sample of 117 parents/guardians from elementary and after-school programs in the SEED from December 2009 to February 2010. Participants had to currently reside in the SEED and were deemed eligible if they were at least 18 years of age, spoke English or Spanish, were the parent or primary guardian of any child 3–17 years of age currently living in their home, and had their child present at the time of the survey. In cases where a parent/guardian had more than one child present, the survey asked about their youngest child present. Those who agreed to participate received a mass transportation voucher on completion of the study. This study was approved by the Icahn School of Medicine at Mount Sinai Institutional Review Board.
Data Collection
The survey included children’s demographics, past medical history, food intake (school meals, purchased foods, and family meals), types and frequency of physical activity, and amount of screen time. To assess Parental Perception of Weight, we asked, “Do you consider (Child’s name) now to be: Underweight, About the Right Weight, Somewhat Overweight, or Very Overweight?” To assess Parental Perception of Health, we asked: “In general, would you say (Child’s name)’s health is: excellent, very good, good, fair or poor?”
Trained staff verbally administered surveys to the parent/guardian in English or Spanish in a semi-private area, which took approximately 20 min to complete. Staff measured children’s height and weight after removing shoes and heavy clothing using a standard portable stadiometer and the Summit S4600 High Capacity BMI Platform Scale, respectively. BMI was calculated using the digital Tonus PE BMI and Growth Calculator and results were immediately shared with parents/guardians using color-coded standardized BMI tables.
Data Analysis
Out of the 117 children, only one girl was in the underweight category based on her BMI and was excluded from further analysis. All analyses were performed using SAS version 9.3 of SAS System for Windows (Copyright © 2002–2010, SAS Institute Inc., Cary, NC, USA) with the type 1 error rate fixed at 0.05 (2 tailed). Summary statistics including means, standard deviations and proportions were used to describe baseline characteristics. t Tests and Chi square tests were used to compare diet and physical activity behaviors between groups. We derived the variable Parental Misperception of Child Weight Status by comparing measured BMI category and parentally labeled weight category, producing two values (underestimation of weight status or correct estimation of weight status). Logistic regression analyses were performed to assess associations with parental underestimation of child’s weight status. To examine racial/ethnic disparities, we compared behaviors and parental perception of weight and health between Blacks and Hispanics and between Mexicans and non-Mexican Hispanics.
Results
Mothers completed the interview for most participants (83 %). Demographic characteristics of the sample are presented in Table 1. The children ranged in age from 3 to 15 years with most children in elementary school. About half the children were boys with 74 % Hispanic (29 % Puerto Rican, 26 % Mexican and 19 % other/mixed) and 26 % non-Hispanic Black. Although we did not collect information about socioeconomic status, all participants were recruited from the same predominantly low income community in New York City.
Table 1.
Study participant characteristics (N = 116)
| N/Mean (%/SD) | ||||
|---|---|---|---|---|
| Total N = 116 |
Healthy weight N = 52 (45 %) |
Overweight/obese N = 64 (55 %) |
p value | |
| Age | 7.2 (2.2) | 7.1 (2.1) | 7.3 (2.3) | 0.64 |
| Male | 61 (53 %) | 28 (54 %) | 33 (52 %) | 0.81 |
| Race/ethnicity | 0.99 | |||
| Hispanic | ||||
| Puerto Rican | 33 (29 %) | 15 (29 %) | 18 (29 %) | |
| Mexican | 30 (26 %) | 14 (27 %) | 16 (25 %) | |
| Other/Mixed Hispanic | 22 (19 %) | 10 (19 %) | 12 (19 %) | |
| Non-Hispanic Black | 30 (26 %) | 13 (25 %) | 17 (27 %) | |
| Green vegetables (times/day) | 0.4 (0.6) | 0.3 (0.4) | 0.4 (0.7) | 0.18 |
| Fruit (times/day) | 1.1 (1.1) | 1.0 (1.0) | 1.1 (1.1) | 0.60 |
| Fruit Juice (times/day) | 1.7 (1.9) | 1.7 (1.6) | 1.7 (2.1) | 0.94 |
| Sugar sweetened beverages (times/day) | 1.1 (1.9) | 1.2 (2.2) | 1.0 (1.5) | 0.52 |
| TV (hours/day) | 1.8 (1.2) | 1.5 (1.1) | 2.0 (1.3) | 0.04 |
| Computer (hours/day) | 0.9 (1.3) | 0.9 (1.5) | 0.8 (1.0) | 0.85 |
| Reported hours of daily walking/running | 3.3 (3.1) | 4.5 (3.6) | 2.4 (2.4) | 0.0002 |
| Parental weight perception | <0.0001 | |||
| Underestimate | 57 (50 %) | 6 (12 %) | 51 (81 %) | |
| Correct estimation | 58 (50 %) | 46 (88 %) | 12 (19 %) | |
| Parental health perception | 0.03 | |||
| Excellent | 42 (36 %) | 25 (48 %) | 17 (27 %) | |
| Very good | 31 (27 %) | 13 (25 %) | 18 (28 %) | |
| Good | 26 (22 %) | 6 (12 %) | 20 (31 %) | |
| Fair/poor | 17 (15 %) | 8 (15 %) | 9 (14 %) | |
One underweight girl removed from analyses
Reported Dietary Behaviors
Parents reported on several dietary behaviors (see Table 1). Children ate a daily mean of 1 serving of fruit and 0.4 servings of green vegetables, and drank 1 serving of sugar sweetened beverages, 2 servings of milk, 2 servings of fruit juice and 3.5 servings of water. Families had a mean of 4 meals together in the home each week. Parents reported a mean of 1 purchase at a food stand, 2 purchases at bodegas/convenience stores and 1 trip to a fast food restaurant weekly.
The only significant difference in dietary behaviors between Blacks and Hispanics was that Black children had higher daily intake of green vegetables (0.7 vs. 0.2 servings, p = 0.006). Within Hispanic children, Mexican children generally had healthier dietary behaviors with fewer daily servings of sugar-sweetened beverages and fruit juice, more daily servings of milk and fewer weekly purchases at food stands and bodegas than non-Mexican children (Table 2).
Table 2.
Dietary and physical activity variables by Hispanic ethnicity
| Mean values (SD) | Mexican | Non Mexican Hispanic | p |
|---|---|---|---|
| Daily servings of sugar sweetened beverages | 0.4 (1.0) | 1.4 (2.1) | 0.004 |
| Daily servings of milk | 2.2 (1.2) | 1.6 (1.1) | 0.03 |
| Daily servings of fruit juice | 1.2 (1.1) | 2.2 (2.2) | 0.006 |
| Daily servings of fruits | 1.3 (1.1) | 1.0 (1.0) | 0.34 |
| Daily servings of green vegetables | 0.1 (0.3) | 0.3 (0.5) | 0.003 |
| Weekly purchases at food stand | 0.5 (0.8) | 1.0 (1.9) | 0.09 |
| Weekly purchases at bodega | 1.1 (1.2) | 2.1 (2.4) | 0.01 |
| Weekly purchases fast food | 0.5 (0.7) | 0.7 (1.2) | 0.34 |
| Daily television hours | 1.3 (0.8) | 1.9 (1.2) | 0.009 |
| Daily computer hours | 0.2 (0.6) | 1.1 (1.5) | 0.0003 |
Reported Physical Activity Behaviors
On a typical day, children had similar amounts of physical and sedentary activity including an average of 3.3 h “walking or running” and 2.7 h of screen time (combined time spent watching television, playing video games and using a computer). Structured physical activity was less common, with children having an average of only 1 h of physical education per week and just 50 % of parents reporting their children participated in organized physical activity outside of school hours.
There were no overall differences in physical activity behaviors between Blacks and Hispanics, but Mexican children had fewer mean hours of television (1.3) than Black children (2.1), p = 0.02 and participated less frequently in organized after school activities (40 vs. 61 %, p = 0.07), but had less screen time than other Hispanic children (Table 2).
Weight and Related Behaviors
Based on measured BMI, 45 % of children were found to be at a healthy weight, 17 % were overweight and 38 % were obese. While combined rates of overweight/obesity did not vary across racial/ethnic groups, Mexican children were less likely to be obese (30 %) compared to other children (40 %). Demographic and dietary behaviors did not vary significantly by weight category (normal weight vs. overweight/obese). However, overweight/obese children had higher reported hours watching television and lower reported time walking/running daily than normal weight children (Table 1).
Parental Perception of Weight
Parental perceptions of weight differed from measured BMI (Fig. 1). Parents perceived that children were overweight/obese 25 % of the time while 55 % were actually overweight/obese based on measured BMI. No parents reported normal weight children as overweight or obese. Parents of overweight/obese children were more likely to underestimate weight (Table 1). Despite equal rates of overweight/obesity among boys and girls (54 and 56 % respectively), there was more underreporting of obesity for boys than for girls; 33 % of overweight/obese boys compared to 63 % of overweight/obese girls were considered to be “somewhat or very overweight” by their parents, p = 0.02. There were no racial/ethnic differences in parental perception of their child’s weight or in misperception of weight status.
Fig. 1.
Adult’s perception of child’s weight versus actual weight category
Weight Perception and Behaviors
There were no differences in reported dietary behaviors between children perceived to be of normal weight and children perceived to be “somewhat overweight” or “very overweight”. However, parents who perceived their children to be of normal weight reported higher daily hours of walking and/or running as compared to children perceived to be “somewhat overweight” or “very overweight”(3.6 vs. 2.6 h, p = 0.08). Parents who more accurately estimated their child’s weight status reported more hours of daily walking/running than parents who underestimated weight status, 4.5 h (SD 3.4) versus 2.4 h (SD 2.6), p = 0.0002. After controlling for child’s age, gender, race/ethnicity, and parental perception of overall health, logistic regression analyses found that higher activity time was associated with less underestimation of child’s weight: for every active hour reported, parents had 9 % lower risk of underestimation of their child’s weight (RR = 0.91, 95 % CI 0.84–0.99).
Parental Perception of Overall Health
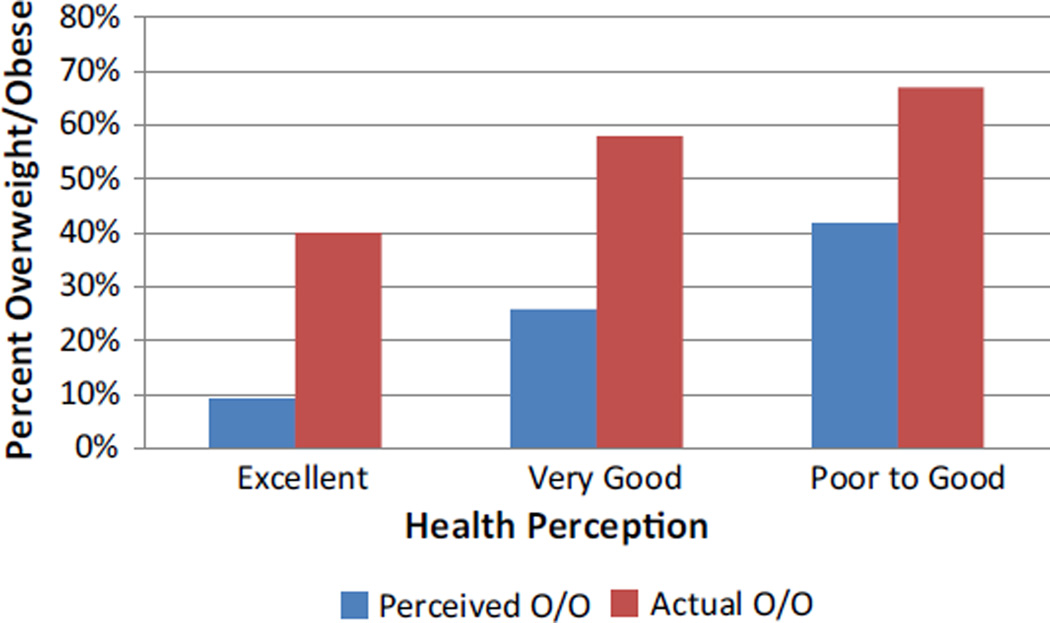
Parents rated their child’s general health as excellent (36 %), very good (27 %), good (22 %), or fair/poor (15 %). Parental perception of overall health varied based on perception of child’s weight and on actual measured BMI. Among children parents perceived to be at a healthy weight, 72 % were reported to be in excellent or very good health but among children perceived as overweight or very overweight, only 40 % were reported to be in excellent or very good health. Similarly, based on measured BMI, children at a healthy weight were reported to be in excellent or very good health 75 % of the time while overweight/obese children were reported to be in excellent or very good health only 56 % of the time, p = 0.04. Parental perception of overweight/very overweight and actual prevalence of overweight/obesity by measured BMI increased as perception of overall health worsened (Fig. 2). Parents correctly identified as overweight/obese 27 % of children in excellent health, 47 % of children in very good health and 62 % of children in good, fair or poor health (p = 0.03) Thus concordance of parental perception of weight with measured BMI increased as perceived health status decreased.
Fig. 2.
Perceived overweight/obese versus actual overweight/obese by health perception
While there were no differences in overall health perception between Blacks and Hispanics, there were differences among Hispanic subgroups. Only 20 % of Mexican parents reported their child’s health as excellent compared to 43 % of non-Mexican Hispanic parents, p = 0.049. On the other hand, 27 % of Mexican parents rated their child’s health as fair or poor compared to only 7 % of non-Mexican Hispanic parents, p = 0.03.
Discussion
To our knowledge, this is the first study to examine parental perceptions of overall child health and relationships with perception of child weight, lifestyle behaviors, and measured BMI, as well as racial/ethnic differences in these factors. Similar to other studies, we found that children in our community engaged in unhealthy dietary and physical activity behaviors and that parental perception of weight differed from actual measures of BMI. Novel findings from our work include that: parents of overweight/obese children rated overall child health lower; parents who viewed their children as less healthy were more likely to correctly characterize their children as overweight; and among children who were overweight, those who were more active were more likely to be seen as healthy and less likely to be seen as overweight. Mexican parents rated their children’s health lower compared to non-Mexican Hispanic parents despite report of healthier behaviors and a trend towards lower rates of obesity.
We found that 55 % of school age children in this low income, urban, racial/ethnic minority community were overweight or obese by measured BMI. Dietary and physical activity behaviors were similar to those reported for other New York City school age children [10] with inadequate intake of fruits and vegetables, excessive intake of sugar sweetened beverages and more time spent in sedentary activities than is recommended [2]. Parents of overweight/obese children reported less daily activity time and more time spent watching television. In addition, similar to other studies, we found that parents often underestimated their child’s weight, especially when children were overweight or obese [11, 21, 27, 30, 33], and that there were gender differences in parental perception of child weight, with a tendency for parents to underestimate weight more in boys than in girls [17, 20, 21, 33]. Interestingly, we found a larger difference between parent perception of child’s weight and measured weight status in obese children than in overweight children. These findings were in contrast to those from a recent meta analysis of parental underestimates of child weight, which found that parents were less likely to underestimate weight in the heaviest children [21]. Our study findings may be partly explained by parents’ unwillingness to label obese children as “very overweight”. Regardless, so long as parents under-recognize their children’s overweight status, interventions targeted to overweight children will have a ceiling on their potential effectiveness. In addition to assessment of BMI and modification of diet and activity for weight management, we also need to address parents’ understanding of overweight/obesity [4]
Previous studies have not examined how parents’ rating of their child’s overall health relates to perception of weight. We found that rates of overweight (both as perceived by parents and by actual measurements) increased as perception of overall health worsened. These findings suggest that parents factor in how healthy they think their children are when they assess the appropriateness of their weight (or vice versa). Agreement between parental weight perception and actual BMI also improved as perception of overall health status decreased, suggesting improved accuracy of weight perception when parents have more concerns about children’s’ overall health status. Previous studies have found that parents may not consider their child to be overweight if he/she has no obvious threatening health problems [16] and are more concerned about weight if they perceive their children to have lower health related quality of life [19]. Other studies have found that parental perception of their child’s weight as a health problem and higher level of parental concern about weight are associated with a higher likelihood of implementing behavioral changes such as limiting screen and improving diet [23, 29]. Therefore, asking parents about overall perception of health may be important since parents may be more likely to implement such changes if they feel that their children’s overall health could be improved.
One important caveat to consider is that there may be cultural or other factors which impact how parents judge their child’s health. For example in our study, Mexican parents rated their children’s overall health less favorably than non-Mexican Hispanic parents despite the trend toward healthier weight and overall report of healthier dietary and physical activity behaviors. While we were not able to find previous studies examining racial/ethnic differences in parental perception of child health, other studies have found racial/ethnic differences in self-rated health in adults, including lower self-rated health among less acculturated Hispanics [3]. We are unable to assess with our data whether Mexican parents are judging their children’s health by different standards or whether these children are in fact less healthy. In either case this finding bears further research.
We note with interest that parent-reported daily hours of walking and/or running trended to be higher in overweight children perceived to be of normal weight. These data suggest that parents may correctly incorporate a sense of fitness level into assessment of child adiposity (children who are active are more likely to be categorized as having a normal weight). One qualitative study found that parents may not consider their children to be overweight if they are active [16]. Previous studies have also found that children’s functional limitations are a key predictor of child health ratings among Latino parents [1] and that parents are more likely to be concerned about their child’s weight if they perceive their child as less active/slower than other children [12, 32]. These perceptions are not without merit as fitness level is an independent predictor of morbidity and longevity and moderates the impact of overweight on health. Thus discussions of perceived child fitness level may provide a fruitful way to engage families in discussions about weight.
Our study is limited in its scope. Our small sample size includes children from a broad age range confined to a small geographic area with demographics that concentrate poverty and minority race/ethnicity. Still it may be applicable to other communities with which it shares sociodemographic characteristics. Also, parental reports are imperfect, which is both a key finding and a limitation of this study. This limitation is moderated because other than the reported one directional error regarding assessment of weight status, errors are likely to be non-differential and hence bias to the null [31]. Social desirability bias is another important limitation as parents may know the “correct” responses to questions and may modify answers to fit these perceptions. In addition, there are limitations in the cross sectional study design in not being able to determine the directionality of associations or make conclusions about cause and effect relationships.
Study Findings in Context of Larger Study/Implication on Community-Based Health Initiatives
Data presented in this manuscript were collected through surveys administered to parents as part of multifaceted assessment and health improvement activities for reduction of diabetes-related disparities among Black and Latino residents of a small geographic area in East Harlem, New York. Intensive assessment of this area identified several reasons why East Harlem may be a diabetogenic environment [18]. Structured community observation revealed limited availability of produce in food stores and the preponderance of restaurants serving inexpensive, calorie dense foods. Suboptimal sidewalks, relatively few parks/playgrounds in a densely populated residential area, and variable crosswalk times for pedestrians highlighted barriers to walking and other types of activity. Survey of adult community residents revealed high levels of concern about neighborhood safety and identified several individual barriers that correlated with lower physical activity levels [14].
Study findings informed several targeted health improvement initiatives to address diabetes prevention and control, including the development of protocols for selecting, funding, and supporting grants to community organizations, including youth-serving organizations [28] and studying and improving health care providers’ use of information collected from the New York City Fitnessgram, an annual fitness assessment conducted in public schools [24].
Conclusion
In summary, we found that parents often underestimate their child’s weight and that parental perception of child weight appears to integrate both actual weight status and their rating of their child’s health. Fitness or activity level may influence these perceptions. In addition, we found racial/ethnic differences in behaviors and general perception of health that should stimulate timely follow up. Parents who do not recognize that their child is at risk for poor health outcomes are less likely to implement healthy lifestyle changes. In addition, parents from communities with limited resources face considerable challenges in making these changes. Some strategies to aid parents include increasing awareness and utilization of existing healthy food and physical activity resources in the community and encouraging parents to advocate for access to more affordable, healthy foods and safe spaces for physical activity (for example supervised walking groups or keeping school gyms open on evenings and weekends).
Another important implication of bias in parental report of child weight is increasing reliance on parent-reported data by organizations such as the Maternal Child Health Bureau, which monitors National Performance Measures and other child health outcomes. Directional bias in these parent-reported data may impact interpretation of changes in these measures over time, and ultimately may affect policies and programs relying on these data.
Finally, there are several important implications of study findings for child health care providers. First, despite potential provider or parental discomfort in discussing weight, it is imperative that pediatricians identify child weight status during well child visits, ascertain parents’ understanding, and provide clear, family focused suggestions for behavior modification. Given limitations in parental understanding and interpretation of child BMI, pediatricians should consider incorporating additional factors such as parental perception of overall health and fitness/activity levels into clinical discussions about weight. For example, clinicians caring for children might collaborate with schools conducting fitness assessments or ask about parents’ perceptions of child fitness during medical visits. Pediatric health care professionals may become better informed about and more actively collaborate with local community based organizations as a way to engage families. Finally, pediatricians might frame discussions about medical complications of obesity in the context of a child’s overall health, rather than focusing solely on behavior modification for weight loss.
Significance.
What is already known on this subject?
Parental perception of weight differs from actual measures of body mass index (BMI).
What this study adds?
Novel findings from our work include that: parents of overweight/obese children rated overall child health lower; parents who viewed their children as less healthy were more likely to correctly characterize their children as overweight; and among children who were overweight, those who were more active were more likely to be seen as healthy and less likely to be seen as overweight. There may be important racial/ethnic differences in behaviors and general perception of health.
Acknowledgments
This publication was supported by REACH U.S. Cooperative Agreement 5U58DP001010 from the Centers for Disease Control and Prevention, and Grants UL1TR000067 from the National Center for Advancing Translational Sciences, National Institutes of Health (NIH) and 7002024 from the New York State Department of Health (NYSDOH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC, NIH or NYSDOH. We thank the many community partners and staff who were involved in the development of the survey including, Barbara Brenner, Mischka Garel, Helen Looker, Devin Mann, Thalia MacMillan and Judy Wylie-Rosett, as well as staff and interns who participated in the data collection phase of this project including, Alison Chaikittirattana, Maria Fernanda Espinoza, Janice Lam, Yemisi Okusanya, Gregory Tull and Amanda Wiggins.
Footnotes
Compliance with Ethical Standards
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Arcia E. Latino parents’ perception of their children’s health status. Social Science & Medicine (1982) 1998;46(10):1271–1274. doi: 10.1016/s0277-9536(97)10055-7. [DOI] [PubMed] [Google Scholar]
- 2.Barlow SE Committee, Expert. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 3.Benjamins MR, Hirschman J, Hirschtick J, Whitman S. Exploring differences in self-rated health among Blacks, Whites, Mexicans, and Puerto Ricans. Ethnicity & Health. 2012;17(5):463–476. doi: 10.1080/13557858.2012.654769. [DOI] [PubMed] [Google Scholar]
- 4.Ben-Joseph EP, Dowshen SA, Izenberg N. Do parents understand growth charts? A national, internet-based survey. Pediatrics. 2009;124(4):1100–1109. doi: 10.1542/peds.2008-0797. [DOI] [PubMed] [Google Scholar]
- 5.Casazza K, Dulin-Keita A, Gower BA, Fernandez JR. Differential influence of diet and physical activity on components of metabolic syndrome in a multiethnic sample of children. Journal of the American Dietetic Association. 2009;109(2):236–244. doi: 10.1016/j.jada.2008.10.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Racial and ethnic approaches to community health (REACH) 2015 Retrieved from http://www.cdc.gov/nccdphp/dch/programs/reach/index.htm.
- 7.Centers for Disease Control and Prevention (CDC) Obesity in K-8 students—New York City, 2006–07 to 2010–11 school years. MMWR Morbidity and Mortality Weekly Report. 2011;60(49):1673–1678. [PubMed] [Google Scholar]
- 8.Chaparro MP, Langellier BA, Kim LP, Whaley SE. Predictors of accurate maternal perception of their preschool child’s weight status among hispanic WIC participants. Obesity (Silver Spring, Md.) 2011;19(10):2026–2030. doi: 10.1038/oby.2011.105. [DOI] [PubMed] [Google Scholar]
- 9.Cromley E, Kleinman LC, Ramos MA, Arniella G, Viswanathan N, Garel M, Horowitz CR. A community-engaged approach to select geographic areas for interventions to reduce health disparities. Progress in Community Health Partnerships: Research, Education, and Action. 2011;5(3):299–305. doi: 10.1353/cpr.2011.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Day S, Lim S, Olson C, Konty K, Kerker B. Child obesity risk: Nutrition & physical activity (No. 10 (4)) New York, NY: NYC Department of Health and Mental Hygiene; 2011. [Google Scholar]
- 11.Doolen J, Alpert PT, Miller SK. Parental disconnect between perceived and actual weight status of children: A metasynthesis of the current research. Journal of the American Academy of Nurse Practitioners. 2009;21(3):160–166. doi: 10.1111/j.1745-7599.2008.00382.x. [DOI] [PubMed] [Google Scholar]
- 12.Eckstein KC, Mikhail LM, Ariza AJ, Thomson JS, Millard SC, Binns HJ Pediatric Practice Research Group. Parents’ perceptions of their child’s weight and health. Pediatrics. 2006;117(3):681–690. doi: 10.1542/peds.2005-0910. [DOI] [PubMed] [Google Scholar]
- 13.Foster BA, Hale D. Perceptions of weight and health practices in hispanic children: A mixed-methods study. International Journal of Pediatrics. 2015;2015:761515. doi: 10.1155/2015/761515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fox AM, Mann DM, Ramos MA, Kleinman LC, Horowitz CR. Barriers to physical activity in east harlem, new york. Journal of Obesity. 2012;2012:719140. doi: 10.1155/2012/719140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gordon NP, Mellor RG. Accuracy of parent-reported information for estimating prevalence of overweight and obesity in a race-ethnically diverse pediatric clinic population aged 3 to 12. BMC Pediatrics. 2015 doi: 10.1186/s12887-015-0320-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jain A, Sherman SN, Chamberlin LA, Carter Y, Powers SW, Whitaker RC. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics. 2001;107(5):1138–1146. doi: 10.1542/peds.107.5.1138. [DOI] [PubMed] [Google Scholar]
- 17.Jeffery AN, Metcalf BS, Hosking J, Mostazir MB, Voss LD, Wilkin TJ. Awareness of body weight by mothers and their children: Repeated measures in a single cohort (EarlyBird 64) Child: Care, Health and Development. 2015;41(3):434–442. doi: 10.1111/cch.12167. [DOI] [PubMed] [Google Scholar]
- 18.Kleinman LC, Lutz D, Plumb EJ, Barkley P, Nazario HR, Ramos MA, Horowitz CR. A partnered approach for structured observation to assess the environment of a neighborhood with high diabetes rates. Progress in Community Health Partnerships: Research, Education, and Action. 2011;5(3):249–259. doi: 10.1353/cpr.2011.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lampard AM, Byrne SM, Zubrick SR, Davis EA. Parents’ concern about their children’s weight. International Journal of Pediatric Obesity: IJPO: An Official Journal of the International Association for the Study of Obesity. 2008;3(2):84–92. doi: 10.1080/17477160701832552. [DOI] [PubMed] [Google Scholar]
- 20.Li J, Lei J, Wen S, Zhou L. Sex disparity and perception of obesity/overweight by parents and grandparents. Paediatrics & Child Health. 2014;19(7):e113–e116. doi: 10.1093/pch/19.7.e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: A meta-analysis. Pediatrics. 2014 doi: 10.1542/peds.2013-2690. [DOI] [PubMed] [Google Scholar]
- 22.McKee C, Long L, Southward LH, Walker B, McCown J. The role of parental misperception of child’s body weight in childhood obesity. Journal of Pediatric Nursing. 2015 doi: 10.1016/j.pedn.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 23.Moore LC, Harris CV, Bradlyn AS. Exploring the relationship between parental concern and the management of childhood obesity. Maternal and Child Health Journal. 2012;16(4):902–908. doi: 10.1007/s10995-011-0813-x. [DOI] [PubMed] [Google Scholar]
- 24.New York City Department of Education. NYC fitnessgram. Retrieved from http://schools.nyc.gov/Academics/FitnessandHealth/NycFitnessgram/NYCFITNESSGRAM.htm.
- 25.Ogden CL, Carroll ME, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief. 2012;82(82):1–8. [PubMed] [Google Scholar]
- 26.Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O’Malley C, Stolk RP, Summerbell CD. Interventions for treating obesity in children. The Cochrane Database of Systematic Reviews. 2009 doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 27.Parry LL, Netuveli G, Parry J, Saxena S. A systematic review of parental perception of overweight status in children. The Journal of Ambulatory Care Management. 2008;31(3):253–268. doi: 10.1097/01.JAC.0000324671.29272.04. [DOI] [PubMed] [Google Scholar]
- 28.Ramos MA, Fox A, Simon EP, Horowitz CR. A community-academic partnership to address racial/ethnic health disparities through grant-making. Public Health Reports (Washington, D.C.:1974) 2013;128(Suppl 3):61–67. doi: 10.1177/00333549131286S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rhee KE, De Lago CW, Arscott-Mills T, Mehta SD, Davis RK. Factors associated with parental readiness to make changes for overweight children. Pediatrics. 2005;116(1):e94–e101. doi: 10.1542/peds.2004-2479. [DOI] [PubMed] [Google Scholar]
- 30.Rietmeijer-Mentink M, Paulis WD, van Middelkoop M, Bindels PJ, van der Wouden JC. Difference between parental perception and actual weight status of children: A systematic review. Maternal & Child Nutrition. 2013;9(1):3–22. doi: 10.1111/j.1740-8709.2012.00462.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008. [Google Scholar]
- 32.Taylor RW, Williams SM, Dawson AM, Haszard JJ, Brown DA. Parental motivation to change body weight in young overweight children. Public Health Nutrition. 2015;18(10):1807–1814. doi: 10.1017/S1368980014002171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Towns N, D’Auria J. Parental perceptions of their child’s overweight: An integrative review of the literature. Journal of Pediatric Nursing. 2009;24(2):115–130. doi: 10.1016/j.pedn.2008.02.032. [DOI] [PubMed] [Google Scholar]
- 34.Vangeepuram N, Mervish N, Galvez MP, Brenner B, Wolff MS. Dietary and physical activity behaviors of New York City children from different ethnic minority subgroups. Academic Pediatrics. 2012;12(6):481–488. doi: 10.1016/j.acap.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Writing Group for the SEARCH for Diabetes in Youth Study Group. Dabelea D, Bell RA, D’Agostino RB, Jr, Imperatore G, Johansen JM, et al. Incidence of diabetes in youth in the United States. JAMA: The Journal of the American Medical Association. 2007;297(24):2716–2724. doi: 10.1001/jama.297.24.2716. [DOI] [PubMed] [Google Scholar]