Abstract
Introduction
Evidence from epidemiological studies shows a link between food insecurity and diet intake or quality. However, the moderating effect of race in this relation has not yet been studied.
Methods
Food insecurity (USDA Food Security Module) and diet quality (Healthy Eating Index-2010; HEI) were measured in 1,741 participants from the Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS) study. Data were collected from 2004–2009 and analyzed in 2014. Multivariable regression assessed the interaction of race and food insecurity on HEI scores, adjusting for age, sex, poverty status, single parent status, drug, alcohol, and cigarette use, and co-morbid diseases.
Results
The interaction of food insecurity and race was significantly associated with diet quality (p=.001). In the absence of food insecurity, HEI scores were similar across race. However, with each food insecurity item endorsed, HEI scores were substantially lower for Whites compared to Blacks. An ad-hoc analysis revealed that Blacks were more likely than Whites to participate in SNAP (p < .05). Further, race stratified analyses revealed that Blacks participating in SNAP showed diminished associations of food insecurity with diet quality.
Conclusions
Study findings provide the first evidence that the influence of food insecurity on diet quality may be potentiated for Whites, but not Blacks. Additionally, results show that Blacks are more likely to participate in SNAP, and show attendant buffering of the effects of food insecurity on diet quality. These findings may have important implications for understanding how food insecurity affects diet quality differentially by race.
Food insecurity, a lack of access to food due to not enough financial or other resources [1], is not a new problem in the United States. However, due to a struggling economy, rising income inequality, high unemployment, underemployment, and low-wage employment rates, the number of Americans that reduce or skip meals due to insufficient money has increased substantially [1]. Although food insecurity strongly affects those living in poverty, it also affects families across the socioeconomic spectrum who experience job instability, disability or other financial hardships [2]. This may, in part, explain why the overall rate of food insecurity has increased from 11 percent before the Great Recession began in late 2007, to nearly 15 percent in 2008 [1]. Even as the United States has struggled to recover from the Recession, the percentage of families experiencing food insecurity has remained about the same, decreasing only to 14.3% as of 2013 [3]. Groups at the highest risk for food insecurity include families below the poverty line (40.2%), single-parent families (35.1% for families headed by single mothers and 25.4% for those headed by single fathers) and Black (25.1%) and Hispanic (26.2%) households [1].
Evidence from epidemiological studies shows a link between food insecurity and diet intake or quality [4–6]. Tarasuk and Beaton [5] examined food insecurity and nutritional adequacy in 145 Canadian women, finding that food insecurity was associated with inadequate energy, vitamin A, folate, iron, and magnesium intake. Using National Health and Nutrition Examination Survey (NHANES) data, Bhattacharya and colleagues [7] found that for adults, but not children, food insecurity was associated with lower levels of serum nutrients, and a poorer score on the U.S. Healthy Eating Index (HEI), a measure of overall diet quality based on recommended dietary guidelines. Champagne and colleagues [6] similarly found that food-insecure adults scored lower on the HEI than food-secure adults, as well as having lower dietary intake of vitamin A, copper, and zinc.
Little is known regarding the potential moderating role of race in the relations of food insecurity to diet quality has not yet been examined directly. However, recent work suggests that the negative influence of food insecurity may be potentiated among minority groups. In that regard, Rehm and colleagues [8] found that (a) higher HEI scores were associated with a higher food cost; (b) lower SES groups consumed lower cost food and scored lower on the HEI; and (c) this was especially true for Blacks, Hispanics, and single-parent households. The authors concluded that lower income groups, and particularly racial minority groups, may be “priced out” of meeting dietary guidelines that emphasize higher cost foods such as fruit, vegetables, dairy, and whole grains, foods that contain nutrients associated with the essential components of the HEI.
Data from the Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS) study, a community-based, epidemiological investigation of socioeconomically diverse, urban-dwelling adults, were used to examine the interactive relations of food insecurity and race to diet quality. As food insecurity rates are high among minority groups [1] and the high cost of healthy foods may disproportionately impact diet quality among low SES minorities [8], we anticipated the negative association between food insecurity and HEI would be greater among Blacks than Whites.
METHODS
Participants
HANDLS participants were recruited in 2004–2009 as a fixed cohort by household screenings from an area probability sample in 13 pre-selected neighborhoods (contiguous census tracts) in Baltimore City. Neighborhoods were selected because they were likely to yield representative distributions with sufficient individuals to fill the sampling design (based on race, poverty status, sex, and age) based on 2000 census data [9]. Recruitment exclusions were: pregnancy, chemotherapy, radiation, or biological treatments for cancer within 6 months, and AIDS diagnosis. After recruitment, exclusions for physical examinations were: acute intoxication or otherwise medically unfit for participation (e.g., uncontrolled blood pressure > 160/100 mm/Hg or acute alcohol or drug intoxication). A total of 190 participants were excluded for these reasons. The study was approved by our institution’s Institutional Review Board.
Of the 3,720 participants recruited, 2,802 completed an initial medical examination that included measures of diet quality. SES was indexed by poverty status defined as above or below 125% of the 2004 Department of Health and Human Services poverty definition in which household incomes are indexed to household sizes. 1,741 participants were available for analysis after excluding participants with any missing data (listwise deletion) for the primary variables of interest (food insecurity and diet quality).
Procedure
Wave 1 data, examined here, were collected in two phases. In the first phase, field interviewers visited households located in target neighborhoods and recruited one or two eligible adults per household. After providing consent, participants completed an interview about social and educational background, demographic information, racial and cultural identification, educational experience, occupational history, family income, total leisure time physical activity, a 24-hour dietary recall, and a wide range of other information broadly conceived as physiological and psychological chronic exposure.
The second phase was an in-person examination on Mobile Research Vehicles (MRVs) in the participants’ communities up to six weeks after the household survey (depending on availability). After consent on the MRV, a physician or nurse practitioner performed a comprehensive physical examination and medical history. The purpose of the physical examination and medical history was to document any diagnosable conditions, to record medications and their frequencies and dosages, to assess disabilities that might limit independent functional activities, and complete other biomedical and cognitive assessments.
Additionally, each participant was administered the Audio Computer-Assisted Self-Interviewing (ACASI). The ACASI administered a psychiatric screen, psychosocial survey questions and income questionnaire. A second 24h dietary recall interview was also administered. Breakfast and lunch were provided on the MRV, and participants were compensated $120 after completion of the visit.
Measurement
Food Insecurity
Food insecurity was measured using a modified version of the USDA’s Food Security Module (FSM) [10] administered through ACASI. The ACASI did not include the FSM hunger question: “In the last 12 months, were you very hungry but didn’t eat because there wasn’t enough money for food?” This question is used to classify respondents as food insecure with or without hunger. Thus, the present study used the sum of these five items to create a food insecurity score, without classification of hunger. Responses were scored following the standard FSM methodology [10]. Responses were dichotomized to either 0 (no) or 1 (yes). However, rather than classifying responses into categories as is done in the FSM approach, food insecurity was measured as a continuous variable by totaling items endorsed on the FSM scale. Therefore, scores ranged from 0 (high food security) to 5 (low food security).
Diet Quality
Diet recalls were collected in-person with a trained interviewer during both the household interview and MRV session. Participants were asked to recall all foods and beverages consumed during the previous 24 hours (recorded by methods developed by the USDA called the Automated Multiple Pass Method [11]) that is supplemented by Food Model booklet and measurement aids to assist in estimating the accurate quantities. This method asks participants if they use salt in food preparation and add salt at the table. Wave 1 data were adjusted for salt used in preparation of foods but not for salt added at the table which can underestimate sodium intake about 5–6% [12]. The recalls were coded using Survey Net [11], matching foods consumed with 8-digit codes in the Food and Nutrient Database for Dietary Studies version 3.0 [13]. Food and nutrient data from both data collection days were averaged.
These data were used to calculate HEI-2010 scores using the guidelines from the 2010 USDA HEI Technical Report [14,15]. The HEI-2010 is comprised of 12 components: total fruit; whole fruit; total vegetables; greens and beans; whole grains; dairy; total protein foods; seafood and plant proteins; fatty acids; refined grains; sodium; empty calories. With the exception of fatty acids and empty calories, each component is calculated per 1,000 calories; therefore diets with different caloric intake are transformed on the same scale for comparison. The HEI-2010 score ranges from 0–100, with 0 representing the lowest compliance with the US Dietary guidelines, and 100 representing optimal compliance, which can be interpreted as optimal diet quality. Only the HEI-2010 total score was used for the present analyses.
Covariates
As part of the household survey, demographic characteristics measured included age (years), sex (male/female), self-reported race (Black/White), household characteristics (i.e., single parent status), and poverty status. Data regarding substance use, including cigarette smoking, alcohol use, and illicit drug use (i.e., cocaine, marijuana, opiates) were coded as current user (within past 6 months), former user (use >6 months ago), and never user. Co-morbidity of major diseases was determined by physician interview and examination. Disease categories were metabolic (diabetes, thyroid disorders, and kidney disease), neurological (Alzheimer’s, dementia, Parkinson’s, multiple myeloma, multiple sclerosis, and epilepsy), inflammatory (lupus and hepatitis), and cancer (all types). The disease categories were included as covariates to ensure that any effects of the predictors of interest were not due to diet-related medical conditions.
Data Analyses
Multivariable regression analyses were computed to determine the potential interactive relations of food insecurity and race to diet quality (HEI-2010). The main effects and interaction term for food insecurity and race was regressed on total HEI-2010 score. The model also included model covariates: poverty status, education, age, household composition, sex, alcohol, cigarette and drug use, and history of major medical diseases1. Statistical analyses were conducted using SPSS version 21.0 (IBM Corp., Armonk, NY).
RESULTS
Sample Characteristics
The sample was 57.8% Black, 56.9% female, and 44.2% below poverty (Table 1). The average age of participants was 47.86 years. A greater proportion of Blacks were single parents and living below the poverty line than Whites, and Blacks reported greater food insecurity severity than Whites (all p’s <.005). Although Blacks had a higher overall prevalence of food insecurity (40% vs. 31.8%), the percentage of food-insecure Whites reporting having to skip or reduce the size of meals on a monthly basis was greater than food-insecure Blacks (28% vs. 19%; χ2 (3)=9.02, p=.029). In addition, 37.7% of food-insecure Blacks in the sample reported participating in the Supplemental Nutrition Assistance Program (SNAP), compared to 29.4% of food-insecure Whites (χ2 (2)=6.37, p=.041).
Table 1.
Descriptive statistics for full sample and by race.
| Full Sample (n = 1,741) | Blacks (n = 1,006) | Whites (n = 735) | |
|---|---|---|---|
| Variable | n (%) / Mean (SD) | n (%) / Mean (SD) | n (%) / Mean (SD) |
| Black | 1006 (57.8%) | - | - |
| Female | 990 (56.9%) | 564 (56.1%) | 426 (58.0%) |
| Poverty Status (Below 125% FPL)* | 770 (44.2%) | 539 (53.6%) | 231 (31.4%) |
| Age (in years) | 47.86 (9.16) | 47.91 (9.09) | 47.80 (9.26) |
| Education (in years)* | 12.54 (3.01) | 12.29 (2.53) | 12.88 (3.56) |
| Single Parent* | 347 (24.3%) | 250 (30.3%) | 97 (16.1%) |
| Food Insecurity* | 1.09 (1.65) | 1.20 (1.69) | 0.95 (1.59) |
| HEI-2010 | 42.96 (11.46) | 42.90 (10.36) | 43.04 (12.82) |
Significant differences by race (p<.005)
Multivariable Regression
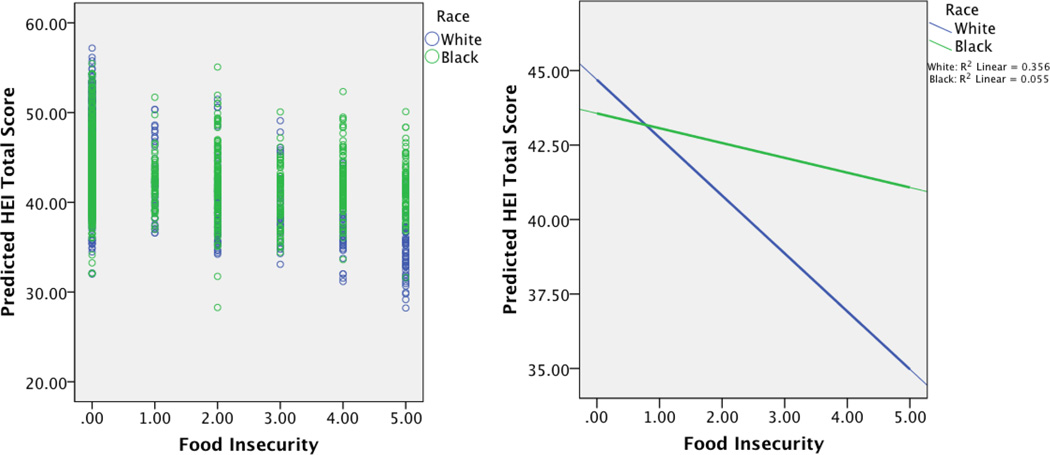
The interaction of food insecurity and race was significantly associated with diet quality (b=1.06, p=.001; Table 2). The interaction plot (Figure 1) showed that at the lowest level of food insecurity (i.e., no endorsements of the food insecurity items), HEI-2010 scores were roughly similar across race. However, with each additional food insecurity item endorsed, HEI-2010 scores were substantially lower for Whites compared to Blacks. The difference between Blacks and Whites was most extreme at the most severe level of food insecurity (i.e., endorsement of all five items), where Blacks had a mean HEI-2010 score of 41.2 and Whites had a mean HEI-2010 score of 36.5. Additionally, poverty status, age, sex, and education were independent predictors of diet quality (all p’s < .05). Furthermore, poverty was associated with lower diet quality, while older age, female sex, and higher education levels were associated with increased diet quality.
Table 2.
Linear regression model predicting diet quality from food insecurity and race.
| Predictor | ba | S.E.a | t | p | |
|---|---|---|---|---|---|
| Food Insecurity | −1.33 | 0.26 | −5.05 | <.001 | |
| Race | 0.02 | 0.63 | 0.24 | .98 | |
| Food Insecurity * Race | 1.06 | 0.33 | 3.25 | .001 | |
| Covariates | |||||
| Poverty Status | −1.14 | 0.57 | −2.01 | .044 | |
| Age | −0.12 | 0.03 | 4.21 | <.001 | |
| Single Parent | 0.25 | 0.58 | 0.43 | .70 | |
| Sex | −2.10 | 0.54 | −2.93 | <.001 | |
| Education | 1.08 | 0.09 | 12.21 | <.001 | |
| Alcohol & Drug Use | −0.87 | 0.47 | −1.86 | .06 | |
| Diabetes/Metabolic | 0.88 | 0.56 | 1.57 | .12 | |
| Neurological | 1.27 | 3.10 | 0.41 | .68 | |
| Inflammatory | 0.91 | 0.84 | 1.08 | .28 | |
| Cancer | 1.77 | 1.10 | 1.61 | .11 | |
| Constant | 25.44 | 1.94 | 13.10 | <.001 | |
Unstandardized regression coefficients.
Figure 1.
Interaction and scatter plot of food insecurity and race predicting HEI total score.
Ad-Hoc Analyses
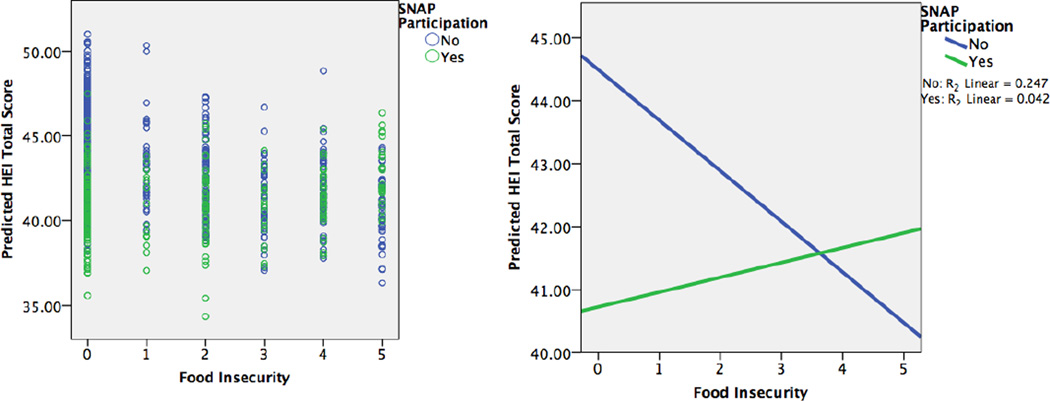
To further explore the race differences in the association of food insecurity on diet quality, and additional ad-hoc analysis was performed to examine the role of SNAP participation. As stated above, Blacks in this sample were significantly more likely to report participating in SNAP (χ2 (2)=6.37, p=.041). Therefore, race-stratified models were run to test the interaction of food insecurity and SNAP participation. Indeed, SNAP participation diminished the effects of food insecurity on diet quality for Blacks only (b=0.80, p=.042; Table 3). The interaction plot (Figure 2) shows that as food insecurity increases, diet quality for Blacks increases for those receiving SNAP participation, and decreases for those who are not.
Table 3.
Linear regression model predicting diet quality from food insecurity and food stamp participation, for Blacks only.
| Predictor | ba | S.E.a | t | p | |
|---|---|---|---|---|---|
| Food Insecurity | −1.44 | 0.57 | −2.55 | .011 | |
| Food Stamps | −2.74 | 0.90 | −3.03 | .002 | |
| Food Insecurity * Food Stamps | 0.80 | 0.39 | 2.03 | .042 | |
| Covariates | |||||
| Poverty Status | −0.31 | 0.69 | −0.45 | .65 | |
| Age | 0.13 | 0.04 | 3.50 | <.001 | |
| Single Parent | 0.43 | 0.68 | 0.62 | .53 | |
| Sex | −1.95 | 0.67 | −2.93 | .003 | |
| Education | 0.53 | 0.13 | 4.05 | <.001 | |
| Alcohol & Drug Use | −0.21 | 0.56 | −0.38 | .71 | |
| Diabetes/Metabolic | 0.74 | 0.70 | 1.05 | .29 | |
| Neurological | 0.85 | 3.07 | 0.28 | .78 | |
| Inflammatory | 1.33 | 1.02 | 1.30 | .19 | |
| Cancer | −1.70 | 1.58 | −1.08 | .283 | |
| Constant | 34.72 | 2.90 | 11.96 | <.001 | |
Unstandardized regression coefficients.
Figure 2.
Scatter and interaction plots of food insecurity and SNAP participation predicting HEI total score, for Blacks only.
DISCUSSION
The researchers posited that greater severity of food insecurity would be associated with lower diet quality, and that this association would be potentiated for Blacks. Although food insecurity indeed interacted with race to predict diet quality, results were contrary to the hypothesized direction. Unexpectedly, Whites had lower HEI scores with greater food insecurity. To our knowledge, this is the first such finding in the literature, as race differences in the relation between food insecurity and diet quality have not been examined previously.
The current findings are inconsistent with prior work that reported an heightened effect of low SES—although not food insecurity specifically—on diet quality among minority groups compared to Whites [8]. Furthermore, the present findings may counterintuitive when viewed in light of the literature on racial disparities in food access that show a lack of access to healthy foods in predominantly Black neighborhoods [16,17]. Given the greater prevalence of food insecurity among Blacks, and the lack of healthy food access in Black neighborhoods, one might have expected to see more pronounced effects of food insecurity on diet quality in Blacks.
Nonetheless, there are two possible explanations for the more pronounced association of greater food insecurity to poorer diet quality in Whites noted in the present investigation. One such explanation relates to methodological differences between the present investigation and prior literature. First, the present study used a large, racially- and socioeconomically diverse sample representative of Baltimore, MD. Prior studies have employed small samples [4, 6], national data sets that may not have been as racially-representative as the present study [4,7], or a select sample of participants already seeking food assistance and therefore not representative of the full socioeconomic spectrum [18].
A second possible explanation for a more deleterious impact of food insecurity on diet quality in Whites may be the lesser role of SNAP participation, which was tested in the ad hoc analyses. Indeed, this finding may actually be related to our conceptual rationale for expecting potentiated effects in Blacks. Although food insecurity has been measured consistently only in the last 25 years, it is likely that racial disparities in food insecurity prevalence have been present throughout many generations of Black Americans due to centuries of economic disadvantage [19]. It is possible that this historical contrast yielded greater resiliency or better coping skills in Blacks compared to Whites. Blacks may have passed down knowledge and skills for securing and preparing higher quality foods on a tight budget through the generations (i.e., cultural transmission of food knowledge) [20], and in this case, using food stamps to help make ends meet.
Additionally, it is notable that not only were relations of food insecurity to diet quality diminished for Blacks participating in SNAP, but food-insecure Blacks were also less likely than food-insecure Whites to have skipped or reduced the size of meals in the last month. It is possible that additional coping skills employed by Blacks mitigate the effects of food insecurity on diet quality, including a collectivist approach to caring for the well-being of others in their community [20]. Therefore, the Black participants in this study may have received additional food assistance through their family, friends, church, or community, in addition to government assistance, that contributed to lower rates of meal skipping and buffered effects on diet quality.
It is important to interpret these findings in the context of factors other than food insecurity that may differentially influence dietary choices and ultimately diet quality. These factors include taste, cost, convenience, and food preference. Glanz et al. [21] examined the role of taste, nutrition, cost, convenience, and weight control on personal dietary choices in a national sample of 2,967 adults. The researchers also examined demographic differences in the importance of each decision factor, as well as healthy lifestyle orientation. They found that, although taste, nutrition, and weight control were important considerations across the socioeconomic spectrum, low-income individuals place a priority on cost and convenience. According to Drewnowski & Specter [22], the relative higher cost of a healthy diet (i.e., low energy density) compared to an unhealthy diet (i.e., high energy density) may explain why low income groups choose unhealthy foods to meet their energy needs. That is, in the context of low SES, individuals have to make a choice between food cost and nutritional content, as they cannot afford to place importance on both. Future research should examine whether the above factors differentially influence diet quality as a function of race/ethnicity.
Our study had several strengths and limitations. Strengths include the large, community-based sample size that was both racially- and socioeconomically-representative and diverse. Additionally, examining race interactions in the effect of food insecurity on diet quality is a first in the literature. The HEI-2010 scores were based on two 24-hour recalls administered by trained interviewers. However, there were a number of limitations to the present study. First, the HANDLS sample overall reported HEI-2010 scores (M=42.96) that were about 10 points below the national average of 51.90 reported in NHANES [23]. Second, sodium added to foods at the table was not included in the HEI-2010 calculations, possibly resulting in underestimation of sodium intake. Third, nutrients from supplements such as omega 3 fatty acids and sodium from antacids were not included in the HEI-2010 scores. Therefore, these nutrient intakes may be underestimated here. Fourth, individual HEI-2010 component scores were not examined in the present study. Therefore, different dietary patterns could have resulted in similar HEI-2010 scores. Finally, due to IRB restrictions, participants with uncontrolled blood pressure were excluded from the study; this limits the generalizability of our findings.
Despite these limitations, the findings from this study have important implications. Overall diet quality and nutrient intakes are associated with many health outcomes, including but not limited to cardiovascular disease risk [24]. Thus, it is necessary to further explore these associations, especially social factors that might mitigate detrimental effects of food insecurity on diet quality.
Future Directions
Future work should examine the potential mechanisms underlying increased resiliency for food-insecure Blacks, compared to greater vulnerability among food-insecure Whites with respect to diet quality. These include cultural transmission of food procurement and preparation techniques that buffer effects of food insecurity on diet quality and increased SNAP participation among Blacks compared to Whites. These coping responses should be investigated further, particularly with respect to cultural and racial differences in strategies. Relatedly, research into why food-insecure Whites are less likely to participate in SNAP than food-insecure Blacks should be investigated. Additionally, future research in this area should also further explore how food insecurity influences food preferences and eating patterns, and examine race differences in these associations. These findings highlight the need for targeted study of poor urban-dwelling Whites as a vulnerable population as well as the more frequently studied low-income Whites of Appalachia or other rural settings.
Policy Implications
These results have important implications for public health and health policy. Aside from development of primary prevention programs and policy changes to reduce food insecurity, the present data suggest intervention points for prevention. Examples include programs and policy changes aimed at mitigating the effects of food insecurity on diet quality. Although the present study did not link these mechanistic pathways to physical health outcomes, there is an abundance of evidence for negative health consequences associated with poor diet quality [24].
Acknowledgments
Funding
This work was supported by the Intramural Research Program, National Institute on Aging, National Institutes of Health (NIH) (A.B.Z. & M.K.E.) and NIH grant 1 RO1AG034161 (S.R.W.).
Footnotes
A model excluding the medical disease variables was also run to ensure that the present model is not only valid for “healthy” individuals, meaning people without major medical problems. However, the reduced model did not effect the interaction terms for the predictors of interest, therefore the disease variables were kept in the model.
COMPLIANCE WITH ETHICAL STANDARDS
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the MedStar Institutional Review Board and NIH’s NIEHS Institutional Review Board, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
There are no conflicts of interest to report for any authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
REFERENCES
- 1.Coleman-Jensen A, Nord M, Andrews M, Carlson S. Household Food Security in the United States in 2010. 2011 [Google Scholar]
- 2.Rose D. Economic determinants and dietary consequences of food insecurity in the United States. J. Nutr. 1999:517–520. doi: 10.1093/jn/129.2.517S. [DOI] [PubMed] [Google Scholar]
- 3.Coleman-Jensen A, Singh A. Econ. Res. Rep. Washington, D.C.: 2014. Household Food Security in the United States in 2013. [Google Scholar]
- 4.Kirkpatrick SI, Tarasuk V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. J. Nutr. [Internet] 2008;138:604–612. doi: 10.1093/jn/138.3.604. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18287374. [DOI] [PubMed] [Google Scholar]
- 5.Tarasuk VS, Beaton GH. Women’s dietary intakes in the context of household food insecurity. J. Nutr. 1999;129:672–679. doi: 10.1093/jn/129.3.672. [DOI] [PubMed] [Google Scholar]
- 6.Champagne CM, Casey PH, Connell CL, Stuff JE, Gossett JM, Harsha DW, et al. Poverty and food intake in rural America: diet quality is lower in food insecure adults in the Mississippi Delta. [cited 2013 Aug 27];J. Am. Diet. Assoc. [Internet] 2007 107:1886–1894. doi: 10.1016/j.jada.2007.08.003. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17964307. [DOI] [PubMed] [Google Scholar]
- 7.Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J. Health Econ. [Internet] 2004;23:839–862. doi: 10.1016/j.jhealeco.2003.12.008. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0167629604000530. [DOI] [PubMed] [Google Scholar]
- 8.Rehm CD, Monsivais P, Drewnowski A. The quality and monetary value of diets consumed by adults in the. Am. J. Clin. Nutr. 2011;94:1333–1339. doi: 10.3945/ajcn.111.015560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Evans MK, Lepkowski JM, Powe NR, LaVeist T, Kuczmarski MF, Zonderman AB. Healthy aging in neighborhoods of diversity across the life span (HANDLS): overcoming barriers to implementing a longitudinal, epidemiologic, urban study of health, race, and socioeconomic status. Ethn. Dis. 2010;20:267–275. [PMC free article] [PubMed] [Google Scholar]
- 10.Bickel G, Nord M, Price C, Hamilton W, Cook J. Alexandria, VA: 2000. Guide to Measuring Household Food Security (Revised 2000) [Internet] Available from: http://www.fns.usda.gov/FSEC/FILES/FSGuide.pdf. [Google Scholar]
- 11.Raper N, Perloff B, Ingwersen L, Steinfeldt L, Anand J. An overview of USDA’s Dietary Intake Data System. [cited 2014 Sep 5];J. Food Compos. Anal. [Internet] 2004 17:545–555. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0889157504000511. [Google Scholar]
- 12.Moshfegh AJ, Holden JM, Cogswell ME, Kuklina EV, Patel SM, Gunn JP, et al. Vital Signs: Food categories contributing the most to sodium consumption--United States, 2007–2008. Morb. Mortal. Wkly. Rep. 2012;61:92–98. [PubMed] [Google Scholar]
- 13.Agricultural Research Service. USDA Food and Nutrient Database for Dietary Studies, 3.0 [Internet] 2014 Available from: http://www.ars.usda.gov/Services/docs.htm?docid=12089.
- 14.Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HA, Kuczynski KJ, et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113:569–580. doi: 10.1016/j.jand.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Institute on Aging. Healthy Eating Index 2010 Calculation [Internet] 2014 Available from: http://handls.nih.gov/06Coll-w01HEI.htm.
- 16.Morland K, Wing S, Diez-Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am. J. Prev. Med. 2002;22:23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- 17.Baltimore Food Policy Task Force. Baltimore City Food Environment Map Methodology Brief [Internet] 2012 Available from: http://www.baltimorecity.gov/Portals/0/agencies/planning/public downloads/Food Desert Methodology Brief.pdf.
- 18.Tarasuk VS, Beaton GH. Women’s dietary intakes in the context of household food insecurity. J. Nutr. [Internet] 1999 doi: 10.1093/jn/129.3.672. Available from: http://jn.nutrition.org/content/129/3/672.short. [DOI] [PubMed] [Google Scholar]
- 19.Airhihenbuwa CO, Kumanyika S, Agurs TD, Lowe a, Saunders D, Morssink CB. Cultural aspects of African American eating patterns. [cited 2013 Dec 6];Ethn. Health [Internet] 1996 1:245–260. doi: 10.1080/13557858.1996.9961793. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9395569. [DOI] [PubMed] [Google Scholar]
- 20.Daly A, Jennings J, Beckett JO, Leashore BR. Effective coping strategies of African Americans. Soc. Work. 1995;40:240–248. [Google Scholar]
- 21.Glanz K, Basil M, Maibach E, Goldberg J, Snyder D. Why Americans eat what they do: Taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J. Am. Diet. Assoc. 1998;98:1118–1126. doi: 10.1016/S0002-8223(98)00260-0. [DOI] [PubMed] [Google Scholar]
- 22.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am. J. Clin. Nutr. [Internet] 2004;79:6–16. doi: 10.1093/ajcn/79.1.6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14684391. [DOI] [PubMed] [Google Scholar]
- 23.Guenther PM, Casavale KO, Kirkpatrick SI, Reedy J, Hiza H, Kuczynski KJ, et al. Alexandria, VA: 2013. Diet quality of americans in 2001–02 and 2007–08 as measured by the healthy eating index-2010 [Internet] Available from: http://www.cnpp.usda.gov/Publications/NutritionInsights/Insight51.pdf. [Google Scholar]
- 24.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch Ha, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. [cited 2013 Aug 7];Circulation [Internet] 2006 114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16785338. [DOI] [PubMed] [Google Scholar]