Abstract
Polymyxins, an old class of antibiotics, are currently used as the last resort for the treatment of multidrug-resistant (MDR) Acinetobacter baumannii. However, recent pharmacokinetic and pharmacodynamic data indicate that monotherapy can lead to the development of resistance. Novel approaches are urgently needed to preserve and improve the efficacy of this last-line class of antibiotics. This study examined the antimicrobial activity of novel combination of polymyxin B with anthelmintic closantel against A. baumannii. Closantel monotherapy (16 mg/L) was ineffective against most tested A. baumannii isolates. However, closantel at 4–16 mg/L with a clinically achievable concentration of polymyxin B (2 mg/L) successfully inhibited the development of polymyxin resistance in polymyxin-susceptible isolates, and provided synergistic killing against polymyxin-resistant isolates (MIC ≥4 mg/L). Our findings suggest that the combination of polymyxin B with closantel could be potentially useful for the treatment of MDR, including polymyxin-resistant, A. baumannii infections. The re-positioning of non-antibiotic drugs to treat bacterial infections may significantly expedite discovery of new treatment options for bacterial ‘superbugs’.
Keywords: Polymyxin, combination, non-antibiotic drug, Acinetobacter baumannii
1. Introduction
The past two decades has seen a substantial increase in Gram-negative ‘superbugs’ resistant to almost all clinically available antibiotics.1 This dire situation is exacerbated by a lack of novel antibiotics in the drug discovery pipeline, leaving the world in a vulnerable state against these life-threatening bacteria.1 ‘Old’ polymyxin class of antibiotics, polymyxin B and E (the latter also known as colistin), are now used as a last line of defence against Gram-negative ‘superbugs’.2 Of these pathogens Acinetobacter baumannii is one of the most problematic, causing a range of infections in the nosocomial setting and in injured military personnel.3 Although polymyxins largely remain effective against problematic Gram-negative bacteria such as A. baumannii, recent pharmacokinetic and pharmacodynamic data on polymyxins suggest that caution is required with monotherapy due to emergence of resistance.4,5 Worryingly, there have been increasing reports of infections caused by A. baumannii which are resistant to all available antibiotics, including polymyxins.6,7 The emergence of polymyxin-resistant A. baumannii highlights the urgent need to investigate novel approaches for maintaining and improving the clinical efficacy of polymyxins.
The use of synergistic combinations of non-antibiotic drugs with antibiotics is emerging as a potentially valuable and cost-effective approach to improve the clinical efficacy of currently available antibiotics against problematic MDR bacterial pathogens.8 The aim of the present study was to investigate bacterial killing and the rapid emergence of polymyxin resistance in A. baumannii using clinically relevant concentrations of polymyxin B in combination with the non-antibiotic closantel.
2. Materials and methods
2.1 Bacterial strains and MIC measurements
Eight strains of A. baumannii representing a mixture of polymyxin-susceptible (i.e. MIC ≤2 mg/L) and polymyxin-resistant (i.e. MIC ≥4 mg/L) strains, including MDR strains, were employed in this study (Table 1). Of the 4 polymyxin-susceptible isolates, FADDI-AB009 and 2949 were polymyxin heteroresistant; polymyxin heteroresistance was defined as a polymyxin-susceptible isolate (i.e. MIC ≤2 mg/L) with subpopulations able to grow in the presence of >2 mg/L polymyxin B.9 A. baumannii ATCC 19606 was purchased from the American Type Culture Collection (Rockville, MD) and the polymyxin-resistant variant FADDI-AB065 was from a previous study;10 polymyxin resistance of FADDI-AB065 is conferred by complete loss of lipopolysaccharide (LPS) from the outer membrane.10 FADDI-AB009 was provided by The Alfred Hospital (Melbourne, Australia) and its polymyxin-resistant variant FADDI-AB085 was produced by plating onto Mueller-Hinton agar (Oxoid, Adelaide, Australia) containing 10 mg/L of colistin sulfate (Sigma-Aldrich, Castle Hill, Australia). In addition, two pairs of polymyxin-susceptible and -resistant isolates were obtained from two patients at the University of Pittsburgh Medical Center prior to (susceptible) and following (resistant) colistin treatment: 2382 vs 2384, and 2949 vs 2949A.11 Polymyxin resistance in isolates 2384 and 2949A is conferred by modifications of lipid A.11 All four isolates from the University of Pittsburgh Medical Center are MDR (defined as non-susceptible to ≥1 treating agent in ≥3 antimicrobial categories).12
Table 1.
MICs for polymyxin B and closantel against the A. baumannii strains examined in this study.
| Strain | MDRa | Polymyxin susceptibilityb | MICs (mg/L)
|
||
|---|---|---|---|---|---|
| Polymyxin B | Closantel | Closantel in the presence of 2 mg/L polymyxin Bc | |||
| ATCC 19606 | No | S | 0.5 | >128 | NPd |
| FADDI-AB009e | No | S (HR) | 0.5 | >128 | NP |
| 2382 | Yes | S | 0.5 | >128 | NP |
| 2949e | Yes | S (HR) | 1 | >128 | NP |
| FADDI-AB065 | No | R | 128 | 0.5 | 0.5 |
| FADDI-AB085 | No | R | 32 | 0.5 | 0.5 |
| 2384 | Yes | R | 8 | >128 | 1 |
| 2949A | Yes | R | 64 | >128 | 2 |
Multidrug resistance (MDR) was defined as non-susceptible to ≥1 treating agent in ≥3 antimicrobial categories.12
CLSI breakpoints (S, susceptible; R, resistant): Polymyxin B, S ≤2 mg/L, R ≥4 mg/L; breakpoints are not available for closantel.
Closantel MICs in the presence of 2 mg/L of polymyxin B.
Not performed (NP) for polymyxin-susceptible isolates.
Polymyxin B heteroresistant (HR). Heteroresistance to polymyxin B was defined as the existence, in an isolate for which the polymyxin B MIC was ≤2 mg/L, of subpopulations able to grow in the presence of >2 mg/L polymyxin B.9
MICs to polymyxin B (Sigma-Aldrich, Castle Hill, Australia; Batch number BCBD1065V) and closantel (Sigma-Aldrich, USA; Batch number SZBC320XV) were determined for all isolates in three replicates on separate days using broth microdilution in cation-adjusted Mueller-Hinton broth (CAMHB; Ca2+ at 23.0 mg/L and Mg2+ at 12.2 mg/L [Oxoid, Hampshire, England]).13 Stock solutions of polymyxin B and closantel were prepared immediately prior to each experiment. Polymyxin B was dissolved in Milli-Q water (Millipore Australia, North Ryde, Australia) and sterilised by passage through a 0.20-μm cellulose acetate syringe filter (Millipore, Bedford, MA). Closantel was first dissolved in dimethyl sulfoxide (DMSO, Sigma-Aldrich) then Milli-Q water to make 10% (v/v). The solution was further serially diluted in filter-sterilised Milli-Q water to the desired final concentration; preliminary studies demonstrated the final concentration of DMSO (2.5%, v/v) to which the bacteria were exposed had no effect on their growth. All assays were performed in 96-well microtiter plates (Techno Plas, Australia) in CAMHB with a bacterial inoculum of approximately 5 × 105 cfu/mL. Plates were incubated at 37°C for 20 h. MICs were determined as the lowest concentrations that inhibited the visible growth of the bacteria. For polymyxin-resistant isolates, MICs of closantel in the presence of 2 mg/L of polymyxin B were also determined (i.e. polymyxin B at the specified concentrations was added to each well of the 96-well plate).
2.2 Baseline polymyxin population analysis profiles
The possible existence of polymyxin-resistant subpopulations at baseline (t = 0 h) was determined with population analysis profiles (PAPs) as described previously.14 Briefly, bacterial cell suspensions (50 μL) of approximately 108 cfu/mL were appropriately diluted with 0.9% saline and plated onto Mueller-Hinton agar plates (Media Preparation Unit, University of Melbourne, Parkville, Australia) containing polymyxin B (0, 0.5, 1, 2, 4 and 8 mg/L) using an automatic spiral plater (WASP, Don Whitley Scientific, West Yorkshire, UK). Colonies were counted after 24-h incubation at 37°C using a ProtoCOL® colony counter (Synbiosis, Cambridge, UK).
2.3 Static time-kill studies
Time-kill studies with polymyxin B and closantel alone, and in combination, were conducted. For monotherapy, polymyxin B was used at 2 mg/L and closantel at 16 mg/L. Three polymyxin B/closantel combinations were investigated using polymyxin B at 2 mg/L combined with closantel at 2, 4, or 16 mg/L (DMSO at 2.5% (v/v) was used for all treatments). Prior to each experiment, isolates were subcultured onto nutrient agar plates (Media Preparation Unit) and incubated overnight at 35°C. One colony was then selected and grown overnight in 20 mL CAMHB at 37°C; from this colony an early log-phase culture was obtained. Each drug was added alone or in combination to 20 mL of a log-phase broth culture of approximately 5 × 105 cfu/mL to yield the desired concentrations. Each 20-mL culture was placed in a sterile 50-mL polypropylene tube (Greiner Bio-One, Germany) containing 20 mL of CAMHB and incubated in a shaking water bath at 37°C (shaking speed, 150 rpm/min). Serial samples (0.5 mL) were removed aseptically at 0, 0.5, 1, 2, 4, 6 and 24 h for viable-cell counting; the samples were appropriately diluted in 0.9% saline and 50 μL of the resultant bacterial cell suspension was spirally plated onto nutrient agar. In order to examine the rapid emergence of polymyxin-resistant subpopulations, samples at 24 h were additionally plated onto Mueller-Hinton agar containing polymyxin B at 4 mg/L. Enumeration was performed after 24 h of incubation as described above. Microbiological responses of combination therapy relative to monotherapy were examined descriptively and via the log change method, i.e. comparing the change in Log10 cfu/mL from 0 h (cfu0) to time t (4 and 24 h; cfut) as shown: log change = Log10(cfut) − Log10(cfu0). Synergy was defined as ≥2 Log10 cfu/mL killing for the combination relative to the most active corresponding monotherapy at a specified time.15
2.4 Quantification of antibacterial activity
The antibacterial activity of polymyxin B and closantel, both individually and in combination, was quantified using a recently reported empirical modeling approach16 which characterizes the rate of bacterial killing in addition to the suppression of bacterial regrowth. An empirical model (Equation 1) was fitted to the time-kill experimental data and estimates were obtained for the parameters A, B, C, Kd and Kr that describe the magnitude of bacterial killing, magnitude of bacterial regrowth, time delay of bacterial regrowth, and the rates of bacterial killing and regrowth, respectively.
| (1) |
Estimation was performed by non-linear regression using the solver add-in in Microsoft Excel® and the parameter estimates were subsequently used to calculate a model-derived time to 2 Log10-killing (T2LK – Equation 2) and time to 3 Log10-regrowth (T3LR – Equation 3). The T2LK was used as a measure of bacterial killing while the T3LR was used as a measure of the suppression of bacterial regrowth. T3LR was constrained to less than 24 h to account for the duration of the time-kill study.
| (2) |
| (3) |
3. Results
3.1 MICs and PAPs
MICs of each drug alone plus MICs to closantel in the presence of polymyxin B (2 mg/L), as well as results for baseline PAPs, are shown in the Table 1. Closantel alone was inactive (MIC >128 mg/L) against the majority of isolates. However, an MIC of closantel of 0.5 mg/L was achieved against two polymyxin-resistant strains (FADDI-AB065 and FADDI-AB085); for these two strains, closantel MICs were unaffected by the addition of polymyxin B (2 mg/L). The addition of polymyxin B substantially reduced closantel MICs in the two remaining polymyxin-resistant isolates (2384 and 2949A; Table 1). The varying susceptibility to polymyxin B of subpopulations within the polymyxin-susceptible isolates prior to polymyxin B treatment was evident in the PAPs. Two isolates (2949 and FADDI-AB009) considered susceptible based upon polymyxin B MIC results were heteroresistant, containing subpopulations able to grow in the presence of >2 mg/L polymyxin B (Table 1). For the polymyxin-resistant isolates, virtually the entire bacterial population was highly resistant to polymyxin B and grew in the presence of 8 mg/L polymyxin B.
3.2 Time-kill studies and rapid emergence of polymyxin resistance
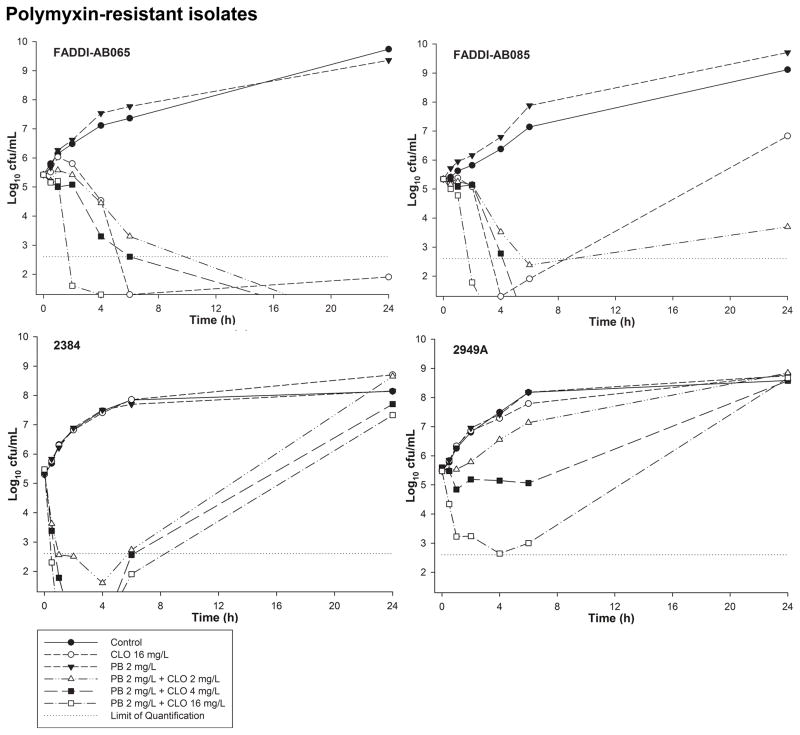
Time-kill profiles for polymyxin B and closantel monotherapy and combination therapy against polymyxin-resistant isolates are shown in Figure 1. Against the closantel-susceptible isolates FADDI-AB065 and FADDI-AB085, polymyxin B monotherapy (2 mg/L) resulted in no bacterial killing while closantel monotherapy (16 mg/L) resulted in rapid killing between 2 – 4 h (T2LK: 178 and 113 min for FADDI-AB065 and FADDI-AB085, respectively). Minimal regrowth was observed at 24 h for FADDI-AB065 (<2-Log10 cfu/mL), although substantial regrowth occurred for FADDI-AB085 (>6-Log10 cfu/mL, T3LR = 19.3 h) (Figure 1). Despite subsequent regrowth at 24 h, the polymyxin-resistant subpopulations of FADDI-AB085 treated with closantel monotherapy (16 mg/L) were approximately 1:100 compared with control, treatment with polymyxin B monotherapy (2 mg/L), and treatment with polymyxin B/closantel 2 mg/L combination (Table 2). Against the remaining polymyxin-resistant isolates 2384 and 2949A, no bacterial killing was observed with either polymyxin B or closantel monotherapy, with growth mirroring that of the controls over 24 h (Figure 1). Combination therapy of polymyxin B and closantel was highly effective against isolates FADDI-AB065 and FADDI-AB085. For FADDI-AB065, all combinations of polymyxin B and closantel resulted in complete inhibition, with no viable colonies detected at 24 h. For FADDI-AB085, complete inhibition was achieved with combinations of polymyxin B and closantel at concentration 4 and 16 mg/L. Against the isolates 2384 and 2949A, even though regrowth was at or close to control values by 24 h with all polymyxin B/closantel combinations, rapid and extensive bacterial killing was observed soon after the commencement of the combination therapy. Against isolate 2949A, polymyxin B plus closantel at 16 mg/L was synergistic at 4 h (T2LK: 80.7 min), with an additional ~4.5-Log10 kill compared with polymyxin B monotherapy observed with the highest closantel concentration (Figure 1). For isolates 2384, rapid and extensive bacterial killing was observed with all polymyxin B/closantel combinations with a minimum of ~5-Log10 greater killing compared to monotherapy at 4 h (T2LK: 46.7, 20.1 and 11.7 min for polymyxin B 2 mg/L plus closantel 2, 4 and 16 mg/L, respectively) (Figure 1). Within 2 h of initiation of therapy, no viable bacteria were detected with the polymyxin B/closantel (4 mg/L and 16 mg/L) combinations; the killing at 4 h in these cases was ~7.5-Log10 more than with equivalent monotherapy.
Figure 1.
Time-kill curves for polymyxin B (PB) and closantel (CLO) monotherapy and combination therapy against polymyxin-resistant A. baumannii isolates FADDI-AB065, FADDI-AB085, 2384 and 2949A. The y-axis starts from the limit of detection and the limit of quantification is indicated by the horizontal dotted line.
Table 2.
Proportion of polymyxin-resistant subpopulations of examined isolates before and after 24 hours treatment with polymyxin B (PB) alone, closantel (CLO) alone, and polymyxin B plus closantel.
| A. baumannii strains | Proportion of polymyxin B-resistant subpopulations able to grow on agar supplemented with 4 mg/L polymyxin B
|
||||||
|---|---|---|---|---|---|---|---|
| Baseline | After 24 hours treatment
|
||||||
| Control | PB 2.0 mg/L | CLO 16 mg/L | PB 2.0 mg/L + CLO 2.0 mg/L | PB 2.0 mg/L + CLO 4.0 mg/L | PB 2.0 mg/L + CLO 16 mg/L | ||
| Polymyxin-susceptible | |||||||
| ATCC 19606 | NDa | 3.33 × 10−8 | ND | ND | ND | NGb | NG |
| FADDI-AB009c | 5.00 × 10−7 | 5.00 × 10−6 | NG | 1.00 × 10−6 | NG | NG | NG |
| 2382 | ND | ND | NG | ND | NG | NG | NG |
| 2949c | 3.33 × 10−5 | 1.67 × 10−5 | 9.17 × 10−1 | 4.17 × 10−6 | 5.91 × 10−3 | NG | NG |
| Polymyxin-resistant | |||||||
| FADDI-AB065 | 8.96 × 10−1 | 7.46 × 10−1 | 1.86 | 1.00 | NG | NG | NG |
| FADDI-AB085 | 1.52 | 1.29 | 2.14 | 1.12 × 10−2 | 1.77 | NG | NG |
| 2384 | 4.75 × 10−1 | 2.90 × 10−1 | 1.97 × 10−1 | 5.95 × 10−1 | 4.82 × 10−1 | 4.89 × 10−1 | 2.55 ×s 10−2 |
| 2949A | 1.01 | 1.74 | 1.62 | 1.38 | 1.13 | 1.42 | 1.31 |
No polymyxin-resistant subpopulations detected (ND)
No growth detected after 24 hours (NG)
Polymyxin B heteroresistant isolates
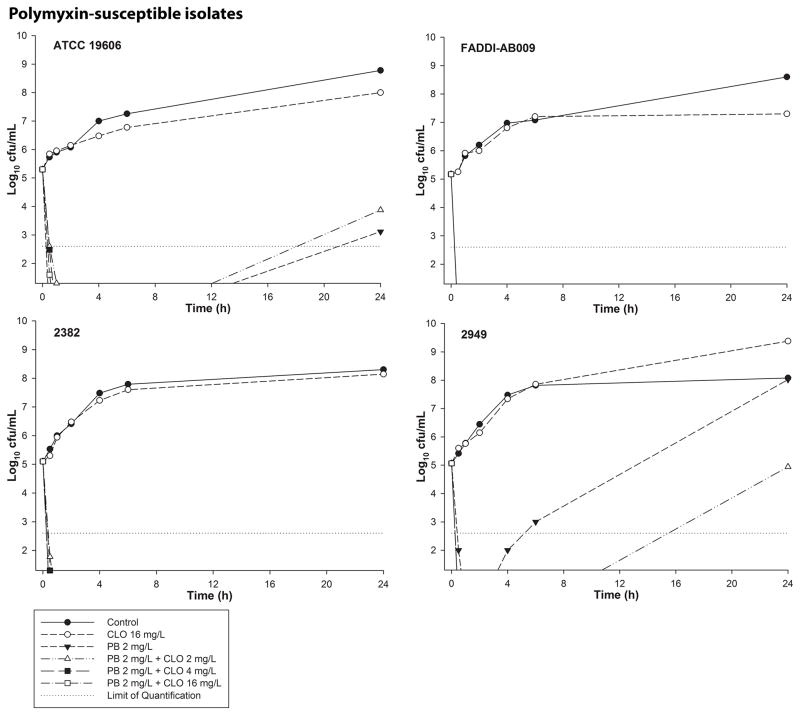
Time-kill profiles for polymyxin B and closantel monotherapy and combination therapy against polymyxin-susceptible isolates are shown in Figure 2. The proportions of polymyxin-resistant isolates before and after 24 h of treatment with each regimen are shown in Table 2. Against all polymyxin-susceptible isolates, polymyxin B monotherapy (2 mg/L) resulted in rapid bacterial killing to below the limit of detection within 0.5 – 1 h, with no viable colonies detected up to 6 h. For FADDI-AB009 and 2382, no regrowth was observed at 24 h. However, regrowth occurred at 24 h with the remaining two isolates (Figure 2). For heteroresistant isolate 2949, the proportion of polymyxin-resistant subpopulations dramatically increased at 24 h following polymyxin B monotherapy, with virtually the entire population able to grow on Mueller-Hinton agar containing 4 mg/L polymyxin B (Table 2); the substantial bacterial killing observed at this time with all other susceptible isolates precludes meaningful comparison of polymyxin-susceptible and -resistant subpopulations. For isolates ATCC 19606 and 2949 (the isolates where regrowth at 24 h was observed), the addition of closantel at 4 and 16 mg/L to polymyxin B was synergistic at 24 h, preventing regrowth despite closantel having no discernible antibacterial activity as monotherapy against any polymyxin-susceptible isolate (i.e. growth with closantel monotherapy was essentially indistinguishable from that of the control). Regrowth similar to that which occurred with polymyxin B monotherapy was observed with the polymyxin B/closantel 2 mg/L combination against isolates ATCC 19606 and 2949. However, with this combination the rapid emergence of polymyxin-resistant subpopulations was approximately 100 times lower than polymyxin B monotherapy for isolate 2949 (Table 2). Antimicrobial activity for the combination of polymyxin B and closantel against polymyxin-susceptible isolates, quantified by the model-derived T2LK, did not differ significantly compared to polymyxin B alone (mean ± SD: 11.5 ± 2.60 vs. 10.5 ± 0.73 min, p = 0.47). Notably, against isolate 2949 bacterial regrowth was markedly suppressed following combination therapy with closantel (2, 4 and 16 mg/L) compared to polymyxin B alone (T3LR: >22 h vs. 6.08 h).
Figure 2.
Time-kill curves for polymyxin B (PB) and closantel (CLO) monotherapy and combination therapy against polymyxin-susceptible A. baumannii isolates ATCC 19606, FADDI-AB009, 2382 and 2949. The y-axis starts from the limit of detection and the limit of quantification is indicated by the horizontal dotted line. All isolates start at a similar initial inoculum. For combinations with CLO 2 mg/L (FADDI-AB009 and 2382) and 4 and 16 mg/L (all isolates), regrowth (if present) is below the limit of detection.
4. Discussion
Infections caused by MDR A. baumannii are increasing globally and are already a major burden on the public health care system.17–19 Although polymyxins are increasingly used as a last-line therapy against this very problematic Gram-negative pathogen,20,21 reports of polymyxin-resistant MDR A. baumannii are increasing.22 Additionally, emerging pharmacokinetic and pharmacodynamic data for polymyxins suggest caution with polymyxin monotherapy due to the presence of polymyxin heteroresistant isolates.23,24 Consequently, novel treatment strategies which optimise bacterial killing and minimise the emergence of polymyxin resistance are urgently required.25
In the present study we evaluated the in vitro efficacy of the combination of polymyxin B with the non-antibiotic closantel against a range of clinical isolates (including MDR isolates) of A. baumannii with various susceptibilities to polymyxin B (Table 1). Closantel is a veterinary anthelmintic drug with activity against multiple nematode species.26 The anthelmintic activity of closantel involves the uncoupling of oxidative phosphorylation and inhibition of chitinase.27,28 Our study is the first to demonstrate the synergistic antibacterial activity between polymyxins and closantel against MDR A. baumannii. The re-positioning of veterinary drugs has been successful for drug discoveries for humans. An example is ivermectin,29 a drug that is currently being used to treat river blindness in human but was initially developed for veterinary use. Currently, the pharmacokinetics of closantel is unavailable in humans; hence, multiple concentrations of closantel (2, 4 and 16 mg/L) were employed based on its pharmacokinetics in animals30,31 and to ensure an appropriate concentration range is covered. The concentration of polymyxin B (2 mg/L) employed in this study is clinically achievable as demonstrated by the pharmacokinetics studies in critically-ill patients.32,33
For A. baumannii, regrowth with polymyxin monotherapy (polymyxin B or colistin) is driven in part by the amplification of polymyxin-resistant subpopulations.23,24 Such regrowth was similarly observed here in two of four polymyxin-susceptible isolates (Figure 2). This finding again illustrates that caution is required for treatment of A. baumannii infections with polymyxin monotherapy. For the polymyxin-resistant isolates, rapid and dramatic improvements in bacterial killing were observed with all three combinations against isolates 2384, and with the combination of polymyxin B/closantel 16 mg/L against 2949A. These improvements occurred despite the virtual absence of bacterial killing with each monotherapy. For example, against isolate 2384 improvements in bacterial killing of >5-Log10 cfu/mL compared with each monotherapy were observed within 1 h of the commencement of treatment with the combination containing 4 mg/L closantel. Despite subsequent regrowth, such rapid and extensive initial killing by an antibiotic/non-antibiotic combination against isolates highly resistant to each drug is an important finding. The rapid and extensive reduction in the bacterial load at the commencement of therapy may facilitate clearance of bacteria by the immune system of the host. Interestingly closantel showed antibacterial activity as monotherapy against FADDI-AB065 and FADDI-AB085, but even then the combinations with all concentrations of closantel (2, 4 and 16 mg/L) demonstrated superiority through better regrowth suppression after 24 h. The addition of closantel to polymyxin B had no effect on initial bacterial killing of polymyxin-susceptible isolates due to extensive bacterial killing by polymyxin B alone (Figure 2). However, the additional closantel at 4 or 16 mg/L did suppress the regrowth observed with polymyxin B monotherapy against ATCC 19606 and 2949 (Figure 2). These findings merit further research given increasing reports of polymyxin resistance34–38 and a diminishing arsenal of effective antibiotics.39–41
Similar to previous reports,42–44 our current study shows that the MIC results did not completely mirror that of the results from the time-kill studies (Table 1 and Figure 1). For isolates 2384 and 2949A, closantel MICs were 1 and 2 mg/L, respectively, in the presence of 2 mg/L of polymyxin B (Table 1). However, in the time-kill studies, regrowth was observed for both isolates with 16 mg/L of closantel in the presence of 2 mg/L of polymyxin B (Figure 1). As MICs are obtained after 20-h incubation via visual observation for turbidity and viable counting using agar plates is not part of the MIC measurement, the MIC results do not necessarily indicate lack of viable cells (e.g. in the 24-h time-kill studies).
The antibacterial mechanism of closantel is unclear. However, closantel has been shown to exhibit antimicrobial activity against Gram-positive bacteria in vitro45,46 and against Staphylococcus aureus in a Caenorhabditis elegans infection model.47 For Gram-negative bacteria, the unique structure of the cell envelope creates a permeability barrier to hydrophobic compounds such as closantel (logP 7.2). Lipopolysaccharide (LPS), the principal component of the external leaflet of the Gram-negative outer membrane, is the initial binding target of polymyxins via electrostatic interaction of the cationic L-α,γ-diaminobutyric acid (Dab) side chains present on polymyxins with the negatively charged phosphate groups of the lipid A component of LPS.48 Binding displaces the divalent cations (Ca2+ and Mg2+) that bridge adjacent LPS molecules, disorganising the outer membrane and increasing its permeability.49 While it was originally proposed that bacterial killing by the polymyxins resulted from permeabilisation of the bacterial outer membrane and subsequent leakage of cell contents, the precise mechanism(s) by which polymyxins ultimately kill bacterial cells is still unknown and several alternative mechanisms of action have been reported.50–53 A previous study has demonstrated polymyxin resistance in isolates 2384 and 2949A is conferred by modifications of lipid A with cationic galactosamine.11 It is apparent that this outer membrane modification on its own did not lead to enhanced penetration of closantel as the MIC for both isolates was >128 mg/L and closantel monotherapy produced no bacterial killing. However, the enhanced bacterial killing observed when combined with polymyxin B suggests sufficient permeabilisation of the outer membrane by the polymyxin to allow closantel to enter into the cell and exert an antibacterial effect. Complete loss of LPS in A. baumannii is also known to confer polymyxin resistance, although such resistance comes at the cost of rendering the outer membrane more permeable to hydrophobic compounds that would otherwise be unable to enter the bacterial cell.10 This may explain the antibacterial activity of closantel in its own right (closantel MICs of 0.5 mg/L) against strains FADDI-AB065 (which is LPS-deficient) and FADDI-AB085. This would also be consistent with the previously reported antibacterial activity of closantel against Gram-positive species which do not possess LPS.45,46
5. Conclusions
In an era of declining antibiotic discovery and rapidly emerging antibiotic resistance, novel treatment strategies for MDR Gram-negative organisms such as A. baumannii are urgently needed. The off-label use of non-antibiotic drugs for antibacterial purposes in combination with existing antibiotics is a currently underexplored area with significant potential to expedite discovery of new treatment options for infections caused by MDR pathogens. The findings from the present study demonstrate that the ‘unexpected’ combination of polymyxin B with an anthelmintic, closantel, may substantially increase the antibacterial activity against MDR, including polymyxin-resistant, A. baumannii. Further investigations in animal infection models are required for translation into the clinic.
Supplementary Material
Acknowledgments
This study is supported by a research grant from the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (R01AI111965) awarded to J.L., T.V., J.N.S., A.F., A.W.P., and D.J.C.. Y.D. is supported in part by R01AI104895. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health. J.L. and A.W.P. are Australian National Health and Medical Research Council (NHMRC) Senior Research Fellows. T.V. is an Australian NHMRC Industry Career Development Research Fellow and D.J.C. is an NHMRC Career Development Research Fellow.
Footnotes
Disclosures
All authors declare no conflict of interests. All authors have approved of this article.
References
- 1.Boucher HW, et al. 10 × ′20 Progress--development of new drugs active against gram-negative bacilli: an update from the Infectious Diseases Society of America. Clin Infect Dis. 2013;56:1685–1694. doi: 10.1093/cid/cit152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Velkov T, Roberts KD, Nation RL, Thompson PE, Li J. Pharmacology of polymyxins: new insights into an ‘old’ class of antibiotics. Future Microbiol. 2013;8:711–724. doi: 10.2217/fmb.13.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peleg AY, Seifert H, Paterson DL. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev. 2008;21:538–582. doi: 10.1128/CMR.00058-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dudhani RV, Turnidge JD, Nation RL, Li J. fAUC/MIC is the most predictive pharmacokinetic/pharmacodynamic index of colistin against Acinetobacter baumannii in murine thigh and lung infection models. J Antimicrob Chemother. 2010;65:1984–1990. doi: 10.1093/jac/dkq226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garonzik SM, et al. Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrob Agents Chemother. 2011;55:3284–3294. doi: 10.1128/AAC.01733-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poulikakos P, Tansarli GS, Falagas ME. Combination antibiotic treatment versus monotherapy for multidrug-resistant, extensively drug-resistant, and pandrug-resistant Acinetobacter infections: a systematic review. Eur J Clin Microbiol Infect Dis. 2014 doi: 10.1007/s10096-014-2124-9. [DOI] [PubMed] [Google Scholar]
- 7.Cai Y, Chai D, Wang R, Liang B, Bai N. Colistin resistance of Acinetobacter baumannii: clinical reports, mechanisms and antimicrobial strategies. J Antimicrob Chemother. 2012;67:1607–1615. doi: 10.1093/jac/dks084. [DOI] [PubMed] [Google Scholar]
- 8.Ejim L, et al. Combinations of antibiotics and nonantibiotic drugs enhance antimicrobial efficacy. Nat Chem Biol. 2011;7:348–350. doi: 10.1038/nchembio.559. [DOI] [PubMed] [Google Scholar]
- 9.Li J, et al. Heteroresistance to colistin in multidrug-resistant Acinetobacter baumannii. Antimicrob Agents Chemother. 2006;50:2946–2950. doi: 10.1128/AAC.00103-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moffatt JH, et al. Colistin resistance in Acinetobacter baumannii is mediated by complete loss of lipopolysaccharide production. Antimicrob Agents Chemother. 2010;54:4971–4977. doi: 10.1128/AAC.00834-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pelletier MR, et al. Unique structural modifications are present in the lipopolysaccharide from colistin-resistant strains of Acinetobacter baumannii. Antimicrob Agents Chemother. 2013;57:4831–4840. doi: 10.1128/AAC.00865-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magiorakos AP, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 13.Clinical and Laboratory Standards Institute (CLSI) Performance Standards for Antimicrobial Susceptibility Testing: Twenty-Second Informational Supplement (M100-S22) CLSI; 2012. [Google Scholar]
- 14.Bergen PJ, et al. Clinically relevant plasma concentrations of colistin in combination with imipenem enhance pharmacodynamic activity against multidrug-resistant Pseudomonas aeruginosa at multiple inocula. Antimicrob Agents Chemother. 2011;55:5134–5142. doi: 10.1128/AAC.05028-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pillai SK, Moellering RC, Eliopoulos GM. In: Antibiotics in Laboratory Medicine. Lorian Victor., editor. Ch. 9. Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 16.Cheah SE, Li J, Nation RL, Bulitta JB. Novel rate-area-shape modeling approach to quantify bacterial killing and regrowth for in vitro static time-kill studies. Antimicrob Agents Chemother. 2015;59:381–388. doi: 10.1128/AAC.04182-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boucher HW, et al. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:1–12. doi: 10.1086/595011. [DOI] [PubMed] [Google Scholar]
- 18.Vincent JL, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302:2323–2329. doi: 10.1001/jama.2009.1754. [DOI] [PubMed] [Google Scholar]
- 19.Kunz AN, Brook I. Emerging resistant Gram-negative aerobic bacilli in hospital-acquired infections. Chemotherapy. 2010;56:492–500. doi: 10.1159/000321018. [DOI] [PubMed] [Google Scholar]
- 20.Li J, et al. Colistin: the re-emerging antibiotic for multidrug-resistant Gram-negative bacterial infections. Lancet Infect Dis. 2006;6:589–601. doi: 10.1016/S1473-3099(06)70580-1. [DOI] [PubMed] [Google Scholar]
- 21.Falagas ME, Kasiakou SK. Colistin: the revival of polymyxins for the management of multidrug-resistant gram-negative bacterial infections. Clin Infect Dis. 2005;40:1333–1341. doi: 10.1086/429323. [DOI] [PubMed] [Google Scholar]
- 22.Ko KS, et al. High rates of resistance to colistin and polymyxin B in subgroups of Acinetobacter baumannii isolates from Korea. J Antimicrob Chemother. 2007;60:1163–1167. doi: 10.1093/jac/dkm305. [DOI] [PubMed] [Google Scholar]
- 23.Owen RJ, Li J, Nation RL, Spelman D. In vitro pharmacodynamics of colistin against Acinetobacter baumannii clinical isolates. J Antimicrob Chemother. 2007;59:473–477. doi: 10.1093/jac/dkl512. [DOI] [PubMed] [Google Scholar]
- 24.Tan CH, Li J, Nation RL. Activity of colistin against heteroresistant Acinetobacter baumannii and emergence of resistance in an in vitro pharmacokinetic/pharmacodynamic model. Antimicrob Agents Chemother. 2007;51:3413–3415. doi: 10.1128/AAC.01571-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nation RL, et al. Framework for optimisation of the clinical use of colistin and polymyxin B: the Prato polymyxin consensus. Lancet Infect Dis. 2015;15:225–234. doi: 10.1016/S1473-3099(14)70850-3. [DOI] [PubMed] [Google Scholar]
- 26.Martin RJ. Modes of action of anthelmintic drugs. Vet J. 1997;154:11–34. doi: 10.1016/s1090-0233(05)80005-x. [DOI] [PubMed] [Google Scholar]
- 27.Gloeckner C, et al. Repositioning of an existing drug for the neglected tropical disease Onchocerciasis. Proc Natl Acad Sci U S A. 2010;107:3424–3429. doi: 10.1073/pnas.0915125107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Williamson RL, Metcalf RL. Salicylanilides: a new group of active uncouplers of oxidative phosphorylation. Science. 1967;158:1694–1695. doi: 10.1126/science.158.3809.1694. [DOI] [PubMed] [Google Scholar]
- 29.Omura S. Ivermectin: 25 years and still going strong. Int J Antimicrob Agents. 2008;31:91–98. doi: 10.1016/j.ijantimicag.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 30.Michiels M, Meuldermans W, Heykants J. The metabolism and fate of closantel (Flukiver) in sheep and cattle. Drug Metab Rev. 1987;18:235–251. doi: 10.3109/03602538708998307. [DOI] [PubMed] [Google Scholar]
- 31.Mohammed-Ali NA, Bogan JA. The pharmacodynamics of the flukicidal salicylanilides, rafoxanide, closantel and oxyclosanide. J Vet Pharmacol Ther. 1987;10:127–133. doi: 10.1111/j.1365-2885.1987.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 32.Sandri AM, et al. Pharmacokinetics of polymyxin B in patients on continuous venovenous haemodialysis. J Antimicrob Chemother. 2013;68:674–677. doi: 10.1093/jac/dks437. [DOI] [PubMed] [Google Scholar]
- 33.Zavascki AP, Goldani LZ, Li J, Nation RL. Polymyxin B for the treatment of multidrug-resistant pathogens: a critical review. J Antimicrob Chemother. 2007;60:1206–1215. doi: 10.1093/jac/dkm357. [DOI] [PubMed] [Google Scholar]
- 34.Lean SS, et al. Prevalence and genetic characterization of carbapenem- and polymyxin-resistant Acinetobacter baumannii isolated from a tertiary hospital in Terengganu, Malaysia. ISRN Microbiol. 2014;2014:953417. doi: 10.1155/2014/953417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Freire MP, et al. Polymyxin use as a risk factor for colonization or infection with polymyxin-resistant Acinetobacter baumannii after liver transplantation. Transpl Infect Dis. 2014;16:369–378. doi: 10.1111/tid.12210. [DOI] [PubMed] [Google Scholar]
- 36.Velkov T, et al. Surface changes and polymyxin interactions with a resistant strain of Klebsiella pneumoniae. Innate Immun. 2014;20:350–363. doi: 10.1177/1753425913493337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moskowitz SM, et al. PmrB mutations promote polymyxin resistance of Pseudomonas aeruginosa isolated from colistin-treated cystic fibrosis patients. Antimicrob Agents Chemother. 2012;56:1019–1030. doi: 10.1128/AAC.05829-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Urban C, Tiruvury H, Mariano N, Colon-Urban R, Rahal JJ. Polymyxin-resistant clinical isolates of Escherichia coli. Antimicrob Agents Chemother. 2011;55:388–389. doi: 10.1128/AAC.01088-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Butler MS, Blaskovich MA, Cooper MA. Antibiotics in the clinical pipeline in 2013. J Antibiot (Tokyo) 2013;66:571–591. doi: 10.1038/ja.2013.86. [DOI] [PubMed] [Google Scholar]
- 40.Schaberle TF, Hack IM. Overcoming the current deadlock in antibiotic research. Trends Microbiol. 2014;22:165–167. doi: 10.1016/j.tim.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 41.Conly J, Johnston B. Where are all the new antibiotics? The new antibiotic paradox. Can J Infect Dis Med Microbiol. 2005;16:159–160. doi: 10.1155/2005/892058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Poudyal A, et al. In vitro pharmacodynamics of colistin against multidrug-resistant Klebsiella pneumoniae. J Antimicrob Chemother. 2008;62:1311–1318. doi: 10.1093/jac/dkn425. [DOI] [PubMed] [Google Scholar]
- 43.Keepers TR, Gomez M, Celeri C, Nichols WW, Krause KM. Bactericidal activity, absence of serum effect, and time-kill kinetics of ceftazidime-avibactam against beta-lactamase-producing Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2014;58:5297–5305. doi: 10.1128/AAC.02894-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robin F, et al. In vitro efficiency of the piperacillin/tazobactam combination against inhibitor-resistant TEM- and complex mutant TEM-producing clinical strains of Escherichia coli. J Antimicrob Chemother. 2011;66:1052–1056. doi: 10.1093/jac/dkr045. [DOI] [PubMed] [Google Scholar]
- 45.Hlasta DJ, et al. Novel inhibitors of bacterial two-component systems with gram positive antibacterial activity: pharmacophore identification based on the screening hit closantel. Bioorg Med Chem Lett. 1998;8:1923–1928. doi: 10.1016/s0960-894x(98)00326-6. [DOI] [PubMed] [Google Scholar]
- 46.Macielag MJ, et al. Substituted salicylanilides as inhibitors of two-component regulatory systems in bacteria. J Med Chem. 1998;41:2939–2945. doi: 10.1021/jm9803572. [DOI] [PubMed] [Google Scholar]
- 47.Rajamuthiah R, et al. Whole animal automated platform for drug discovery against multi-drug resistant Staphylococcus aureus. PLoS One. 2014;9:e89189. doi: 10.1371/journal.pone.0089189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Velkov T, Thompson PE, Nation RL, Li J. Structure--activity relationships of polymyxin antibiotics. J Med Chem. 2010;53:1898–1916. doi: 10.1021/jm900999h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hancock RE, Chapple DS. Peptide antibiotics. Antimicrob Agents Chemother. 1999;43:1317–1323. doi: 10.1128/aac.43.6.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brogden KA. Antimicrobial peptides: pore formers or metabolic inhibitors in bacteria? Nat Rev Microbiol. 2005;3:238–250. doi: 10.1038/nrmicro1098. [DOI] [PubMed] [Google Scholar]
- 51.Pristovsek P, Kidric J. Solution structure of polymyxins B and E and effect of binding to lipopolysaccharide: an NMR and molecular modeling study. J Med Chem. 1999;42:4604–4613. doi: 10.1021/jm991031b. [DOI] [PubMed] [Google Scholar]
- 52.Hale JD, Hancock RE. Alternative mechanisms of action of cationic antimicrobial peptides on bacteria. Expert Rev Anti Infect Ther. 2007;5:951–959. doi: 10.1586/14787210.5.6.951. [DOI] [PubMed] [Google Scholar]
- 53.Sampson TR, et al. Rapid killing of Acinetobacter baumannii by polymyxins is mediated by a hydroxyl radical death pathway. Antimicrob Agents Chemother. 2012;56:5642–5649. doi: 10.1128/AAC.00756-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.