Abstract
A 95-year-old woman was admitted to our hospital for evaluation of bilateral lower-limb edema persisting for 3 months. Serum creatinine was 1.55 mg/dl, and urinary protein excretion was 9.1 g/day. Renal biopsy revealed stage 1 membranous glomerulonephritis (MGN) with immunoglobulin G4-dominant staining. This patient did not have any underlying disease such as infection with hepatitis B or C virus or malignancy, and anti-phospholipase A2 receptor (PLA2R) antibody was detected in the serum. Accordingly, idiopathic MGN was diagnosed. Corticosteroid therapy was avoided, but hemodialysis was required to treat generalized edema. The patient is currently doing well. This is the oldest reported case of idiopathic MGN with positivity for anti-PLA2R antibody.
Key Words: Elderly nephropathy, Anti-phospholipase A2 receptor antibody, Idiopathic membranous glomerulonephritis
Introduction
Membranous glomerulonephritis (MGN) is the most important cause of nephrotic syndrome in adults. Among patients >60 years old, secondary MGN is more common, especially due to underlying malignancy [1]. In 2009, the M-type phospholipase A2 receptor (PLA2R) was identified as the major podocyte antigen involved in idiopathic adult MGN, while anti-PLA2R antibody is not detected in secondary MGN [2]. We encountered a 95-year-old Japanese woman who developed nephrotic-range proteinuria. Renal biopsy revealed stage 1 MGN with immunoglobulin (Ig)G4-dominant staining. This patient did not have any underlying disease that could cause secondary MGN, and anti-PLA2R antibody was detected in her serum, so idiopathic MGN was diagnosed. This is the oldest reported case of idiopathic MGN, and it is discussed with reference to the literature.
Case Presentation
In July 2014, a 95-year-old Japanese woman was admitted to our hospital with a 3-month history of bilateral edema of the lower extremities. When she developed chronic diarrhea at 90 years of age (in 2009), laboratory tests revealed that serum creatinine (Cre) was 1.6 mg/dl, albumin was 3.2 g/dl, and urinary protein excretion was 0.32 g/day.
She had no history of smoking, alcohol intake, or malignancy. On admission, she was 153 cm tall and weighed 56.4 kg. Her blood pressure was 138/70 mm Hg. There were bilateral edema of the lower extremities.
Laboratory tests revealed a white blood cell count of 4,600/μl, a red blood cell count of 3.71×106/μl, hemoglobin of 11.7 g/dl, and platelet count of 21.3×104/μl. In addition, total protein was 6.3 g/dl, albumin was 2.4 g/dl, serum urea nitrogen was 26 mg/dl, serum Cre was 1.55 mg/dl, C-reactive protein was 1.6 mg/dl, and lactate dehydrogenase was 257 IU/l (normal: 119-229 IU/l). Immunological tests showed that antinuclear antibody, anti-double-stranded DNA antibody, and U1-nuclear ribonucleoprotein antibody were all negative. IgG was 1,340 mg/dl, IgA was 427 g/dl, and IgM was 266 mg/dl. The serum level of C3 was 123 mg/dl (normal: >86 mg/dl), C4 was 19 mg/dl (normal: >18 mg/dl), and CH50 was 38 U/ml (normal: >30 U/ml). The patient was negative for hepatitis B virus antibody, hepatitis C virus antibody, and Treponema antigen. Urinary protein excretion was 9.1 g/day, and the sediment contained 5-10 erythrocytes per high-power field. Urinary Bence Jones protein was negative by immunofixation electrophoresis.
No findings suggestive of malignancy were revealed by imaging studies such as computed tomography and ultrasonography. The long axis of the kidney was calculated to be 9.0 cm bilaterally. Serum anti-PLA2R autoantibody was positive according to the method of Akiyama et al. [3]. Renal biopsy was done to evaluate the renal changes in this patient.
Renal Biopsy
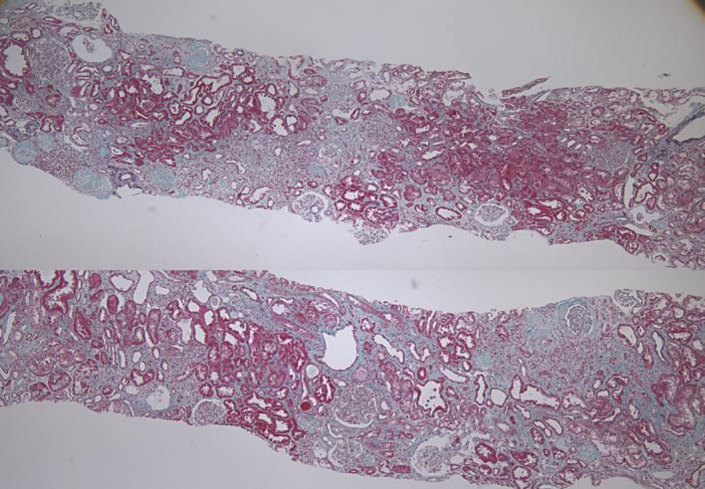
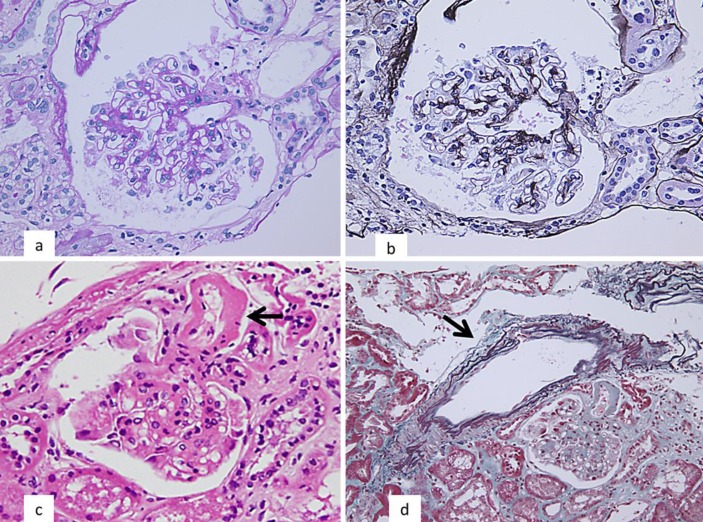
Light microscopy of a renal biopsy specimen containing 36 glomeruli revealed global sclerosis in 22 of them (fig. 1a). The other 13 glomeruli showed mild mesangial matrix expansion (fig. 2a), but there was no definite spike formation, bubbling, or thickening of the glomerular basement membrane (GBM) (fig. 2b). In the tubulointerstitial region, atrophy or fibrosis affected 50-60% of the cortical tissue (fig. 1). The arterioles displayed mild to moderate hyalinosis (fig. 2c), while the interlobular arteries showed mild to moderate fibroelastic intimal thickening (fig. 2d). Immunofluorescence microscopy demonstrated granular deposits of IgG and C3 along the GBM. Analysis of IgG subclasses revealed dominant staining for IgG4 (IgG4 > IgG1 > IgG3 > IgG2; fig. 3), while staining for IgA and IgM was very weak. The anti-PLA2R binding in the biopsy was positive. Congo red staining was negative. Electron microscopy showed subepithelial electron-dense deposits (EDD) in the GBM, but these subepithelial EDD were not associated with spike-like protrusions arising from the basement membrane (fig. 4). Stage 1 MGN was diagnosed due to these findings.
Fig. 1.
Light microscopy of a renal biopsy specimen containing 36 glomeruli revealed global sclerosis in 22. In the tubulointerstitial region, 50-60% of the cortical tissue showed atrophy or fibrosis (Masson's trichrome stain).
Fig. 2.
a The other 13 glomeruli showed mild expansion of the mesangial matrix (periodic acid-Schiff stain). b There was no definite spike formation, bubbling, or thickening of the GBM (periodic acid-methenamine silver stain). c There was mild hyalinosis of the arterioles (arrow) (HE stain). d Interlobular arteries showed mild fibroelastic intimal thickening (arrow) (Masson's trichrome stain).
Fig. 3.
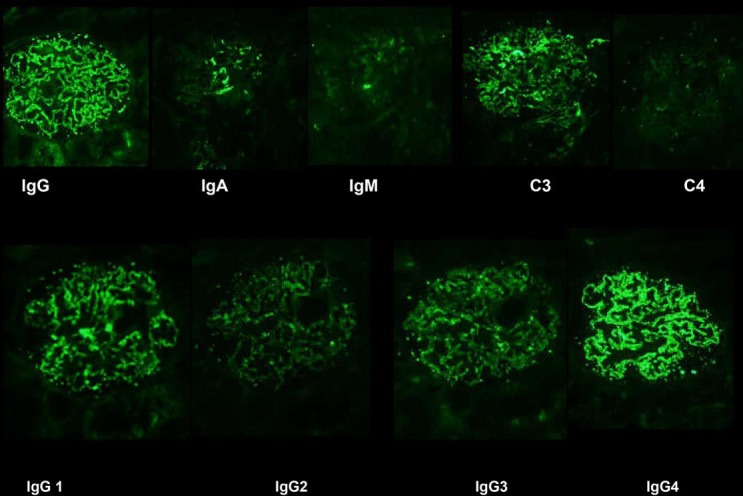
Immunofluorescence microscopy demonstrated granular deposits of IgG and C3 along the GBM. Analysis of IgG subclasses revealed dominance of IgG4 (IgG4 > IgG1 > IgG3 > IgG2).
Fig. 4.

Electron microscopy showed subepithelial EDD (arrows) in the GBM. These subepithelial EDD lacked spike-like protrusions from the basement membrane.
Clinical Course
Anasarca was treated with diuretics (furosemide at 80 mg daily) and dietary restriction (6 g of salt and 700 ml of water daily), achieving weight loss from 56.4 to 51.0 kg. Because the patient did not want steroid therapy due to adverse effects such as bone disease, cyclosporin microemulsion (Neoral at 50 mg daily) was added, and the level at 2 h after administration was titrated in the range of 600-1,000 ng/ml. However, proteinuria persisted, and renal function deteriorated rapidly. Hemodialysis was started when Cre was 6.0 mg/dl and urea nitrogen was 102 mg/dl because of exacerbation of pleural effusion and generalized edema along with an increase in weight to 58 kg at 2 months after diagnosis.
Discussion
In 2009, Beck et al. [2] identified the M-type PLA2R as the major target podocyte antigen in adult idiopathic MGN and showed that it was expressed by podocytes and colocalized with IgG4 in glomerular immune deposits of patients with idiopathic MGN. A PLA2R band was detected in the serum of 26 patients (mean age 48.1 ± 14.9 years; range 21-88) of 37 patients (70%) with idiopathic MGN, while it was not found in 8 patients with secondary MGN, 22 patients with other diseases, and 30 healthy controls. Qin et al. [4] evaluated Chinese MGN patients with the method of Beck et al. [2], and they detected anti-PLA2R autoantibodies in the serum of 49 patients (mean age 49.2 ± 14.9 years; range 18-77) of 60 patients (82%) with idiopathic MGN, in 1 of 20 patients with lupus-associated MGN, in 1 of 16 patients with hepatitis B-associated MGN, and in 3 of 10 patients with tumor-associated MGN.
Akiyama et al. [3] investigated circulating anti-PLA2R antibodies in Japanese MGN patients using a highly sensitive Western blotting method under nonreducing conditions with human glomerular extract (at dilutions of 1:25, 1:10, and 1) as the primary antibody. Anti-PLA2R antibodies were detected in 53 of 100 patients (aged 67 ± 9 years at diagnosis) with idiopathic MGN compared to 0 of 31 patients (aged 61 ± 12 years) with secondary MGN.
Zent et al. [5] studied 309 patients with idiopathic MGN and reported that 74 were elderly (≥60 years old), with the oldest subject being 83 years old. The incidence of chronic renal insufficiency was significantly higher in elderly patients than in younger patients (<60 years old). Only 33 of 74 elderly patients (46%) received treatment, which was steroids alone in 76%, immunosuppressants alone in 9%, or a combination in 16% of patients. The authors found no benefit of treatment in terms of the complete remission rate and the incidence of chronic renal insufficiency, so they suggested that steroid therapy should not be routinely offered to these elderly patients. O'Callaghan et al. [6] compared the clinical features and outcomes of MGN between 95 younger patients and 60 older patients aged >60 years, including 2 patients aged 80 and 85 years. There was a higher incidence of an identifiable cause for the nephropathy among the older patients, who were also more likely to have hypertension and more severe renal impairment than the younger patients. Abrass [7] reported on the treatment of elderly patients with MGN, stating that the only consistent recommendation is to avoid high-dose corticosteroids. She also mentioned that drug dosages should be modified and monitored carefully and that elderly patients may be particularly prone to the side effects and infectious complications of immunosuppressants.
When we investigated positivity for anti-PLA2R antibodies at the diagnosis of idiopathic MGN among patients attending our hospital, we identified 7 patients aged 75.1 ± 10.2 years (range 65-95) including the present case. Our patient was older than those reported by previous authors, such as Beck et al. [2] (48.1 ± 14.9 years; range 21-88), Akiyama et al. [3] (67 ± 9 years), and Qin et al. [4] (49.2 ± 14.9 years; range 18-77). If nephrologists performed renal biopsy more frequently in elderly patients over 90 years of age with nephrotic range proteinuria, other such cases might be discovered.
In conclusion, we encountered a 95-year-old Japanese woman with nephrotic-range proteinuria, and renal biopsy revealed stage 1 MGN with IgG4 dominance. This patient did not have any underlying disease that could have caused secondary MGN, and anti-PLA2R antibody was positive, so idiopathic MGN was diagnosed. Corticosteroid therapy was avoided, but hemodialysis was required for generalized edema, and the patient is currently doing well on hemodialysis. This case reminds us that idiopathic MGN with anti-PLA2R antibodies can occur even at the very advanced age of 95 years.
Statement of Ethics
The present report adhered to the Declaration of Helsinki and these patients have given their consent for the case report to be published.
Disclosure Statement
All authors report no conflicts of interest.
Acknowledgements
This study was funded by the Okinaka Memorial Institute for Medical Research.
References
- 1.Hofstra JM, Wetzels JF. Management of patients with membranous nephropathy. Nephrol Dial Transplant. 2012;27:6–9. doi: 10.1093/ndt/gfr371. [DOI] [PubMed] [Google Scholar]
- 2.Beck LH Jr, Bonegio RG, Lambeau G, Beck DM, Powell DW, Cummins TD, Klein JB, Salant DJ. M-type phospholipase A2 receptor as target antigen in idiopathic membranous nephropathy. N Engl J Med. 2009;361:11–21. doi: 10.1056/NEJMoa0810457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akiyama S, Akiyama M, Imai E, Ozaki T, Matsuo S, Maruyama S. Prevalence of anti-phospholipase A2 receptor antibodies in Japanese patients with membranous nephropathy. Clin Exp Nephrol. 2015;19:653–660. doi: 10.1007/s10157-014-1054-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qin W, Beck LH Jr, Zeng C, Chen Z, Li S, Zuo K, Salant DJ, Liu Z. Anti-phospholipase A2 receptor antibody in membranous nephropathy. J Am Soc Nephrol. 2011;22:1137–1143. doi: 10.1681/ASN.2010090967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zent R, Nagai R, Cattran DC. Idiopathic membranous nephropathy in the elderly: a comparative study. Am J Kidney Dis. 1997;29:200–206. doi: 10.1016/s0272-6386(97)90030-5. [DOI] [PubMed] [Google Scholar]
- 6.O'Callaghan CA, Hicks J, Doll H, Sacks SH, Cameron JS. Characteristics and outcome of membranous nephropathy in older patients. Int Urol Nephrol. 2002;33:157–165. doi: 10.1023/a:1014404006045. [DOI] [PubMed] [Google Scholar]
- 7.Abrass C. Treatment of membranous nephropathy in the elderly. Semin Nephrol. 2003;23:373–378. doi: 10.1016/s0270-9295(03)00053-6. [DOI] [PubMed] [Google Scholar]