Policy Points:
The International Health Regulations (IHR) are the governing framework for global health security yet require textual and operational reforms to remain effective, particularly as parallel initiatives are developed.
The World Health Organization (WHO) is the agency charged with oversight of the IHR, and its leadership and efficient functioning are prerequisites for the effective implementation of the IHR.
We reviewed the historical origins of the IHR and their performance over the past 10 years and analyzed all of the ongoing reform panel efforts to provide a series of politically feasible recommendations for fundamental reform.
This article offers proposals for fundamental reform—with politically feasible pathways—of the IHR, their operations and implementation, WHO oversight, and State Party conformance.
Context
The International Health Regulations (IHR) have been the governing framework for global health security for the past decade and are a nearly universally recognized World Health Organization (WHO) treaty, with 196 States Parties. In the wake of the Ebola epidemic, major global commissions have cast doubt on the future effectiveness of the IHR and the leadership of the WHO.
Methods
We conducted a review of the historical origins of the IHR and their performance over the past 10 years and analyzed all of the ongoing reform panel efforts to provide a series of politically feasible recommendations for fundamental reform.
Findings
We propose a series of recommendations with realistic pathways for change. These recommendations focus on the development and strengthening of IHR core capacities; independently assessed metrics; new financing mechanisms; harmonization with the Global Health Security Agenda, Performance of Veterinary Services (PVS) Pathways, the Pandemic Influenza Preparedness Framework, and One Health strategies; public health and clinical workforce development; Emergency Committee transparency and governance; tiered public health emergency of international concern (PHEIC) processes; enhanced compliance mechanisms; and an enhanced role for civil society.
Conclusions
Empowering the WHO and realizing the IHR's potential will shore up global health security—a vital investment in human and animal health—while reducing the vast economic consequences of the next global health emergency.
In 2005, the world health assembly (wha) fundamentally revised the International Health Regulations (IHR),1 a treaty meant to herald a new era of global cooperation to make the world more secure. Yet in the aftermath of the West African Ebola epidemic, the IHR face critical scrutiny—the World Health Organization (WHO),2, 3 Harvard and the London School of Hygiene and Tropical Medicine,4 the National Academy of Medicine,5 and the United Nations (UN)6 have all urged major reforms.
Frustration with lack of progress on IHR implementation has led Member States to launch independent programs with strikingly similar aims. The United States established the Global Health Security Agenda (GHSA), partnering with approximately 50 countries to accelerate progress towards global capacity to prevent, detect, and respond to biological threats.7 The United States has committed to support up to 30 countries in developing these capacities,8 and the 2015 G7 Summit pledged to double that number.9 As the IHR face probing questions and parallel initiatives are developed, we review their historical origins, their performance, and their future.
A Brief History
The IHR's origins can be traced to a series of Sanitary Conferences beginning in 1851 to forge an international agreement to curb the spread of infectious diseases (originally cholera, followed by plague and yellow fever) entering Europe from Asia, particularly India and the Levant.10 At that time, the concept of global health security meant protecting Europe without unduly hindering trade. The Sanitary Conferences led to a binding agreement in 1892—the International Sanitary Convention (ISC)—focused on quarantine for cholera. European states subsequently adopted additional conventions, which were incorporated into a single ISC. By 1926, the ISC covered primarily cholera, yellow fever, and plague. The raison d’être of the earliest treaties grew out of a perceived security imperative for powerful countries. Most important was self‐protection against external threats, rather than safeguarding the public's health in every region of the world.
In 1907, the Rome Agreement created the Office International d'Hygiène Publique (OIHP), entrusting this new agency with overseeing the international health agreements.11 At its creation in 1948, the WHO assumed OIHP's mandate and oversight of the ISC as well as a separate convention on air travel. The WHO Constitution empowered the Organization to adopt regulations to prevent the international spread of disease (Articles 21, 22). Its power to adopt regulations is far‐reaching—binding on Member States unless they affirmatively opt out.12 In 1951, the WHA exercised this authority to replace the ISC with the International Sanitary Regulations (ISR), covering 6 diseases. In 1969, the WHA revised the ISR, changed their name to the International Health Regulations, and removed typhus and relapsing fever. The WHA removed smallpox in 1981 after its global eradication. By the time the WHA called for fundamental revision of the IHR in 1995, the treaty applied to the same 3 diseases as the original ISC—cholera, plague, and yellow fever—and no others.
The IHR (2005): International Responsibilities of the WHO and States Parties
With the emergence and pandemic potential of HIV/AIDS, the spread of endemic diseases to new parts of the world, and outbreaks of viral hemorrhagic fever, it became clear that the IHR were insufficiently flexible to respond to new infectious disease threats. The WHA called for the IHR's revision in 1995, and subsequent resolutions in 2001 and 2002 brought critical attention to the early detection of, and rapid response to, public health threats; yet the WHA took little action to shore up the obvious weaknesses in the IHR.13, 14, 15
The imperative for global health governance took on fresh urgency with the advent of severe acute respiratory syndrome (SARS). Although SARS cases emerged in November 2002, China delayed notifying the WHO until February 2003. China took 2 additional months before permitting WHO epidemiologists to enter Guangdong province, where the outbreak originated. Later, Beijing conceded it had experienced hundreds more cases than previously reported.16 Then WHO Director‐General Gro Harlem Brundtland criticized China's delays,17 catalyzing a major political shift toward a global norm of transparency and prompt reporting, further driving IHR reform.18 The WHA adopted the revised IHR in 2005, with the treaty entering into force in 2007. Currently, the IHR have 196 States Parties—every WHO Member plus Lichtenstein and the Holy See.19
Scope
The revised IHR aim “to prevent, protect against, control and provide a public health response to the international spread of disease” (Article 2). The IHR broke from a disease‐specific model, embracing an “all‐hazards” strategy. They define “disease” to include all illnesses or medical conditions, irrespective of origin or source, that could present significant harm to humans (Article 1). The drafters intended to incorporate biological, chemical, and radio‐nuclear events, as well as zoonotic diseases and threats to food safety.
Recognizing the importance of travel and commerce, the IHR contain a “balancing dynamic,” comprising public health, commerce and human rights (Figure 1). This balance informs the health measures a State Party may take for international travelers upon their arrival and departure (eg, medical examinations, vaccinations, observation) and for keeping ships and aircraft free of contamination and disease vectors. States Parties must, though, have sufficient scientific evidence of the risk posed and of whether the measure adopted is likely to ameliorate that risk before taking restrictive travel or trade measures or impinging on human rights. The IHR require States Parties to carefully weigh WHO recommendations in making that threat assessment.
Figure 1.
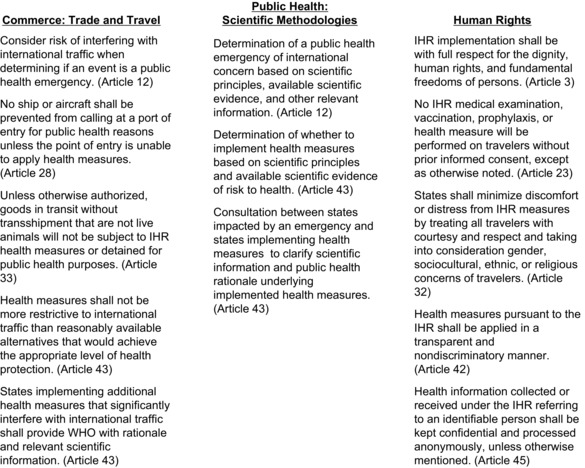
The IHR Balancing Dynamic: Commerce, Public Health, and Human Rights
The IHR obligate States Parties to develop core capacities to detect, assess, report, and respond to potential public health emergencies of international concern. The IHR (Annex 1) prescribe explicit capacities for surveillance and response and for controlling and containing disease at points of entry. The IHR identify minimum core capacities required at the local, intermediate (regional/provincial), and national levels to detect unexpected morbidity and mortality, report essential information, confirm and assess the status of reported events, notify the WHO when required (following the decision algorithm in Annex 2), and respond effectively to contain and mitigate the event.
To guide States Parties in developing IHR core capacities, the WHO published the IHR Core Capacity Monitoring Framework in 2010 (subsequently updated).20 The IHR Monitoring Framework and accompanying IHR Monitoring Tool identified 8 specific core capacities, as well as 5 other capacities concerning points of entry and specific hazards (Figure 2). For each of these 13 core capacities, the WHO identified attributes and actions, asking states to use these attributes to assess their compliance.
Figure 2.
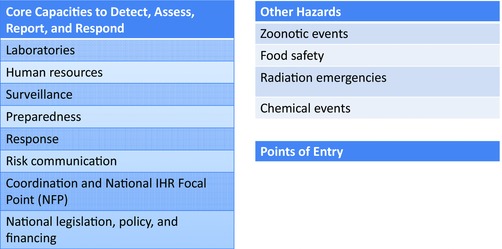
IHR Monitoring Framework: Core Capacities
The concept of core capacities embraced an “upstream” public health strategy to prevent and contain outbreaks at their source. States Parties agreed “to collaborate with each other to the extent possible” to develop and maintain core capacities (Article 44). States Parties were required to develop and maintain core capacities by 2012, with a possible extension to 2014, and an additional extension to 2016. In 2015, the 68th WHA extended the deadline to 2016 for all 81 States Parties that had requested extensions. The WHA also decided to support 60 priority countries, including those in west and central Africa, to meet core capacities by June 20193 (Figure 3). Still, the Organization's pattern has been to accept continual delays in State Party compliance.
Figure 3.
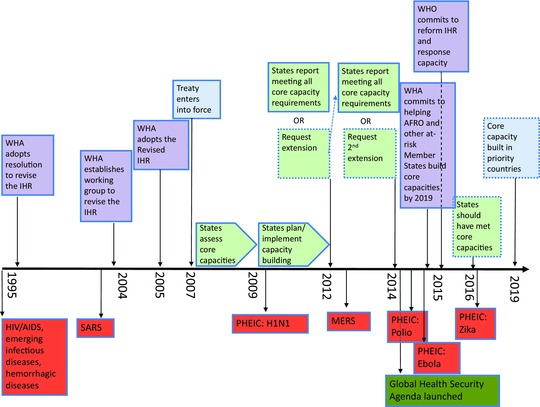
IHR Timeline
In line with their historical origins, the IHR contain rules regarding points of entry at ground, air, and water borders, as well as health measures for conveyances, goods, containers, and travelers. Further, States Parties must apply health measures in a nondiscriminatory manner, justify additional measures, collaborate with other states, and treat personal data confidentially. States Parties must report to the WHO on their IHR implementation and comply with prescribed dispute resolution procedures. Importantly, the IHR also set up new mechanisms for two‐way communication and information sharing between the WHO and States Parties. The IHR mandate that each State Party appoint a National IHR Focal Point (NFP) for routine information sharing and coordination during health crises. All states have NFPs, at least on paper, but many NFPs either are not well trained in IHR implementation or—more often—are not properly tasked to routinely communicate with WHO headquarters.
Notifications and Declarations of PHEICs
The IHR require States Parties to promptly notify the WHO of events that may constitute a public health emergency of international concern (PHEIC) with an ongoing obligation to inform and respond to follow‐up requests (Figure 4). Notifications alert the world to unfolding public health events as well as marshal resources and coordinate global response efforts. To guide notifications, Annex 2 contains a decision instrument requiring States Parties to always notify the WHO of 4 specific diseases: smallpox, wild poliomyelitis, novel human influenza, and SARS. The algorithm also lists pandemic‐prone diseases that trigger further assessment, including cholera, pneumonic plague, yellow fever, and viral hemorrhagic fevers. Beyond listed diseases, States Parties must utilize the instrument to assess any event of potential international public health concern, including from unknown causes, to determine if it is unusual or unexpected, may cross boarders, or may require travel or trade restrictions (Annex 2). Departing from previous international norms, the IHR authorize the WHO to consider reports from unofficial sources, such as scientists, nongovernmental organizations (NGOs), print and broadcasting outlets, and social media platforms. When it receives an unofficial report, the WHO seeks verification from the States Parties in whose territory the event occurs.
Figure 4.
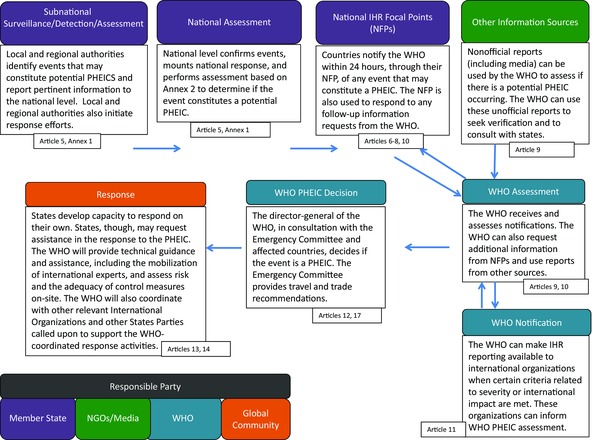
IHR Process for Global Governance of Disease
The director‐general (D‐G) has sole power to declare a PHEIC. In determining whether to declare a PHEIC, the D‐G shall consider: (a) information provided by the State Party; (b) the decision instrument; (c) the advice of the Emergency Committee, which the D‐G also has sole discretion to convene; (d) scientific principles and evidence; and (e) a risk assessment regarding human health, international spread, and interference with international traffic. If the D‐G declares a PHEIC, she must issue temporary, nonbinding recommendations describing health measures States Parties should take. She is also empowered to terminate a PHEIC, which automatically expires after 3 months unless extended, modified, or terminated earlier.
Declared PHEICs
The 2009 H1N1 influenza pandemic put the IHR to the test. The WHO declared the first‐ever PHEIC after consultation with Mexico and the United States.21 The WHO, however, was later criticized for fueling public fear when it became clear the virus was not highly pathogenic (although it still caused more than 200,000 deaths worldwide),22 but that criticism was primarily aimed at WHO's then definition of the pandemic influenza phases, which stood outside the IHR framework. Many States Parties also disregarded the WHO's temporary recommendations against travel and trade restrictions; several states banned pork imports, while others instituted travel restrictions and advisories.23, 24 In 2011, the WHO Review Committee charged with reviewing IHR functioning during the H1N1 pandemic cautioned, “The world is ill‐prepared to respond to a severe influenza pandemic … with tens of millions at risk of dying.”25
In 2014, the D‐G declared 2 further PHEICs, for polio and for Ebola. The designation of polio appeared counterintuitive given there was only a handful of cases. Yet small pockets of polio in Afghanistan, Pakistan, and Nigeria were putting global eradication at risk. The following year, the WHA endorsed extension of the PHEIC given political instability in the regions with ongoing outbreaks.26 The polio PHEIC declaration is untraditional, appearing more to rally political support in targeted states than to alert the world to any large‐scale reemergence of the disease.
In the case of Ebola, the D‐G waited 4 months after announcing an “unprecedented outbreak” in April 2014 before declaring a PHEIC on August 8, 2014.27 The delay only looked worse with time, as leaked WHO documents revealed that the WHO's decisions were highly political and lacked transparency.28 The WHO's Ebola Interim Assessment Panel in July 2015 said that urgent warnings “either did not reach senior leaders or senior leaders did not recognise their significance.”2 The Harvard‐LSHTM Independent Panel on the Global Response to Ebola wrote, “Confidence in the organization's capacity to lead is at an all‐time low.”4 The temporary recommendations also suffered major flaws of their own, asking states with limited infrastructure to ensure health system capacities without adequate international assistance.29
The Ebola PHEIC declaration, though, ultimately rallied the international community to bring the epidemic under control, but not before it had claimed more than 11,300 lives.30 Most notably, President Obama sent in military assets to build treatment facilities and provide logistical support; the UN Security Council (UNSC) adopted a historic resolution calling Ebola a threat to international peace and stability; and the UN Secretary‐General created a UN Mission for Ebola Emergency Response (UNMEER). Although the D‐G continued the PHEIC on December 18, 2015, human‐to‐human transmission has virtually ended in the 3 most affected countries. This robust, albeit delayed, response demonstrates that political resolve and ample financing can bring seemingly intractable health threats under control.
On February 1, 2016, the D‐G declared the fourth, and most recent, declaration of a PHEIC in response to the Zika epidemic.31, 32 Since Brazil reported Zika in May 2015, an estimated 1 million infections have occurred across 25 countries in the Americas. IHR NFPs throughout the Americas have been reporting laboratory‐confirmed cases of Zika to the Pan American Health Organization (PAHO), which has issued recommendations for the region.33 Most concerning is a possible association between Zika virus and neurological disease (Guillain‐Barré syndrome [GBS]) or fetal abnormalities (microcephaly). Curbing the Zika epidemic will require effective vector control, mosquito and human surveillance, and research for reliable diagnostic tests and a vaccine. The US Centers for Disease Control and Prevention advised pregnant women to postpone travel to Zika‐affected countries. Women who are considering becoming pregnant should talk with their doctor.34
This is the first time the D‐G has declared a PHEIC for a mosquito‐borne disease, but the scope of the declaration was narrower than for other PHEICs. Dr. Margaret Chan said, “I am now declaring that the recent cluster of microcephaly cases and other neurological disorders reported in Brazil, following a similar cluster in French Polynesia in 2014, constitutes a Public Health Emergency of International Concern.”35, 36 In other words, the PHEIC was for the cluster of microcephaly and GBS rather than for the Zika virus itself. From a legal perspective, the wording of the PHEIC introduces confusion as neither microcephaly nor GBS is an infectious disease. These neurological and congenital conditions per se do not appear to be hazards that could cross borders under the meaning of Annex 2. It is the Zika virus itself and the mosquito vector that have the potential for international transmission.
Undeclared and Potential PHEICs
The world is now closely watching outbreaks of Middle East respiratory syndrome (MERS), which originated in Saudi Arabia in 2012. MERS has yet to trigger a PHEIC declaration despite its reaching more than two dozen countries and accounting for at least 1,621 laboratory‐confirmed cases and 584 deaths as of December 2015.37, 38 By September 2015, the D‐G had convened 10 Emergency Committee meetings,39 with the last two occurring during and after the spread of the virus from Saudi Arabia to the Republic of Korea, which sparked a large outbreak.40 The Emergency Committee recommended careful monitoring and strengthened infection prevention and control. Most MERS cases were linked to hospital settings, and in the absence of sustained community transmission, the Committee concluded the conditions to declare a PHEIC had not been met.41
For many global health crises, the D‐G chose not even to convene an Emergency Committee, including cholera in Haiti, the Fukushima nuclear disaster in Japan, and chemical weapons use in Syria. Each event would have required notification under Annex 2, in addition to the several hundred events that have been reported to the WHO as potential PHEICs. Confusion still exists as to what events warrant consideration by an Emergency Committee and a potential PHEIC declaration. What steps can and should the WHO take to ensure prompt notification and information sharing, and how can the D‐G improve the transparency and scientific rigor for declaring a PHEIC?
Operationalizing the IHR: Widespread Noncompliance
The IHR afford a vital governing framework to limit the international spread of disease. Yet, 10 years of experience has shed light on the critical challenges in implementing the IHR, as well as major omissions in the regulations. These challenges and gaps have become politically salient, with deepening concern that the IHR, and the WHO itself, have failed to fulfill the promises of sound governance and leadership. The past decade has revealed an urgent need to improve the IHR's text, but failure to effectively implement the regulations has become far more important. States Parties, in particular, have undermined the IHR's effectiveness by failing to fully comply with their international obligations. Below, we explain the gaps and features of noncompliance that have undermined the IHR's operational viability.
National Core Capacities
National core capacities for preparedness, detection, and response form the bedrock of global health security.42 Yet most States Parties have yet to fully establish core capacities. In 2014, only 64 States Parties reported meeting core capacities, while 48 failed even to respond to the WHO43 (p6) (Figure 5). Governments have not properly funded and implemented required capacities, while international assistance has been limited.43 (p6) Achieving IHR core capacities by all states remains an indisputable baseline for global health security. The more time it takes to detect an event, the slower the response is and the more lives are lost. Every WHO IHR Review Committee and all the major commissions (Table 1) have demanded that States Parties build and strengthen core capacities—all to little avail.2, 43 (p12, 13)
Figure 5.
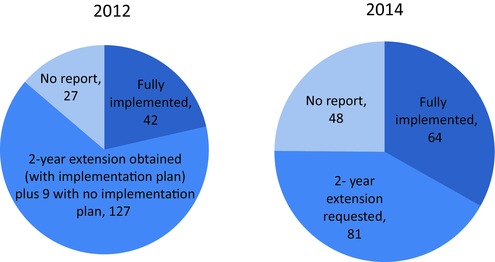
IHR Implementation 2012 and 2014
Table 1.
Commissions on Global Health Security and IHR Reform
| Panels, Committees, and Reports | |
|---|---|
| Related to IHR Reform | Organization |
| Ebola Interim Assessment Panel | WHO |
| Review Committee on the Role of the IHR in the Ebola Outbreak and Response | WHO |
| Roadmap for Action on Ebola | WHO |
| Advisory Group on Reform of WHO's Work in Outbreaks and Emergencies with Health and Humanitarian Consequences | WHO |
| Review Committee on the Functioning of the IHR in Relation to the Pandemic (H1N1) | WHO |
| UN Secretary‐General High‐Level Panel on the Global Response to Health Crises | UN |
| Commission on a Global Health Risk Framework for the Future | National Academy of Medicine (Secretariat) |
| Harvard‐LSHTM Independent Panel on the Global Response to Ebola | Academia |
Finding the resources to support health system capacity building has been challenging. While States Parties committed to providing domestic resources to build core capacities, national budgets often neglect this fundamental commitment under the IHR. Many countries with limited resources have had little bandwidth to prioritize building systems for unknown threats as they have struggled to meet the everyday health needs of their populations—ranging from primary care and essential medicines to safe childbirth and healthy mothers and babies. Similarly, the WHO and higher‐income States Parties agreed to provide technical and financial assistance to countries in need (Article 44), but with some exceptions,44, 45 very few have funded projects explicitly for building IHR core capacities. The bulwark of international financing has been in the form of vertical funding streams, such as for AIDS, tuberculosis, and malaria. All in all, sustainable funding commensurate with the need for IHR core capacities has come neither from national governments nor from donors.
Meaningful Metrics
Through the IHR Monitoring Tool, the WHO expects States Parties to conduct annual self‐assessments on IHR implementation, focusing on the 13 core capacities. States were supposed to issue formal reports in 2012 (with additional reports in 2014 and 2016 for governments that requested extensions) to declare if they had fully implemented the regulations. If not, countries were supposed to submit a concrete plan to reach full implementation.
Even if all States Parties had reported accurately and in a timely manner, national self‐assessments are unacceptable and cannot ensure uniformly high‐quality national preparedness. States Parties have not collected sufficient or the right kinds of data to produce quantitative assessments of what are predominately qualitative questions. Governments, moreover, do not use a consistent set of evidence‐based metrics to measure their compliance. Most importantly, self‐assessments are inherently self‐interested and unreliable, absent rigorous independent validation. These deficiencies undermine the integrity and utility of self‐assessments.43 (p6)
Beyond the failure of political will, country assessments have not been directly linked to robust technical and financial assistance. Lower‐income states, perhaps understandably, express reluctance to upgrade their capacities without such assistance. Overall, responsibility for fulfilling core capacities must be a shared one, requiring dedicated domestic budgets, international financing, and WHO leadership. And absent these political and financial commitments to build core capacities, the world is considerably less secure.
Timely and Full Notification
Although the IHR call for robust information sharing through reporting of potential PHEICs and subsequent requests for follow‐up data, countries continue to delay notifications and/or limit the information reported. Delayed reporting and/or lack of transparency and cooperation, for example, occurred in West Africa during Ebola and in Saudi Arabia during MERS. Additionally, governments have failed to share pertinent information about international travelers, either out of defiance of their international obligations or simply due to confusion about patient privacy—all despite guidance under Article 45.
The extant governance framework reveals an inherent tension, providing a disincentive to transparency and information sharing. The IHR cannot effectively govern global health security unless governments promptly report novel infections. This follows the simple pattern of the epidemiologic curve: the faster health authorities know about a novel event, the faster they can mount an effective response, leading to fewer cases (Figure 6). But governments have economic reasons to withhold or delay transparent information sharing. They fear that once they have disclosed an outbreak of a novel infection, other governments and private parties may impose travel and trade restrictions, with severe economic consequences. For example, once they have disclosed, the IHR Emergency Committee could conclude that travel and trade restrictions are warranted; or, more likely, governments or the private sector may simply take action, disregarding WHO recommendations. The adverse economic impact of early reporting under the IHR can dissuade States Parties from being fully transparent.
Figure 6.
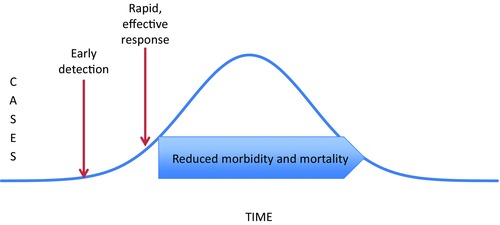
Theoretical Framework: Early Detection Leads to Rapid Response and Reduced Morbidity and Mortality
Given previous patterns, national concern about the economic repercussions of prompt reporting appears fully justified. Guinea, Sierra Leone, and Liberia, for example, experienced aggregate cumulative losses over 10% of GDP due to the Ebola outbreak.46 Canada during SARS as well as Mexico and the United States during H1N1 suffered major losses from precipitous reductions in tourism and trade. Yet, the failure to raise the global alert can ultimately be even more impactful in terms of human life and national treasure. The Commission on a Global Health Risk Framework for the Future concluded, “The global community has massively underestimated the risks that pandemics present to human life and livelihoods.… There are very few risks facing mankind that threaten loss of life on the scale of pandemics … [and] that have the potential for such catastrophic economic impact.” The Commission estimates that a pandemic in the 21st century could cost in excess of US$6 trillion.5
Despite the severe health and economic repercussions of unnecessary travel and trade restrictions, the WHO has not had the political authority or capacity to prevent States Parties from disregarding its recommendations. The WHO is not a policing agency, and the IHR offer scant inducements to ensure consistent State Party compliance. When countries balance their IHR obligation to report against the risk of economic sanctions, they may wait as long as possible before sharing vital information.
WHO Governance
The Ebola epidemic highlighted major deficiencies in mobilizing a large‐scale, coordinated response to health emergencies. The IHR provide a framework for global health security, but that framework functions only if the WHO is an effective leader and governments build strong health systems. The WHO erred at multiple levels during the Ebola epidemic. The D‐G waited 5 months after cross‐border spread before declaring an emergency. The WHO Regional Office for Africa (AFRO) and country offices impeded deployment of international aid workers and equipment. Most importantly, the WHO failed to mobilize adequate fiscal and human resources until the epidemic was spinning out of control. The Organization eventually corrected these mistakes, but its errors probably cost thousands of lives. The fault lies, in fairness, not only with the WHO Secretariat but also with Member States that have starved the agency of resources for many years.
The reasons for the WHO's failures are well understood but remain resistant to change. In 2011, the agency cut its budget by nearly US$600 million due to a severe fiscal deficit, notably its epidemic response capabilities.47 Its regional structures have also been longstanding problems, with major variability in regional organizations. The D‐G has called on governments and donors to build core capacities and has asked for State Party compliance with the IHR, but without impact.48 All the Ebola commissions have exhibited an implicit distrust in the Organization to make the necessary reforms. Instead, each panel has proposed a well‐funded and accountable WHO Centre for Emergency Preparedness and Response. The Harvard‐LSHTM Independent Panel on the Global Response to Ebola, for example, insisted that a new center be quasi‐independent, with a separate governing board (Table 2).
Table 2.
Four Global Health Security Panels: Select Recommendations
| National Academy | UN | |||
|---|---|---|---|---|
| WHO | Harvard‐LSHTM | of Medicine | secretary‐general | |
| Commission on a | High‐Level Panel | |||
| Independent Panel on | Global Health Risk | on the Global | ||
| Ebola Interim | the Global Response to | Framework for the | Response to Health | |
| Recommendation | Assessment Panel | Ebola | Future | Crises |
| Building IHR Core Capacities Linked to Funding and Independent Assessments | There should be a costed planbased on independently assessed information and financed in close partnership with the World Bank. | The plan should be supported by a transparent system for tracking and monitoring results through an Accountability Commission for Disease Outbreak Prevention and Response. Governments should agree to regular independent, external assessments. | Clear metrics to be independently assessed should be developed. Governments should agree to participate in external assessments. The World Bank and other donors should declare that funding is conditional on independent assessments. | All countries must develop IHR core capacities by 2020. The WHO should conduct independent, field‐based assessments of IHR compliance every 4 years to supplement annual self‐assessments. The WHO Secretariat should develop a costed action plan for each country. Independent assessments should be tied to guarantees of financial and technical assistance. |
| Incentives for Reporting and Disincentives for Not Reporting and for Taking Unwarranted Actions | There should be incentives, like insurance triggers, for encouraging countries to notify public health risks to the WHO. There should be disincentives to discourage countries from taking independent travel and trade measures. | The WHO should commend countries that rapidly and publically share information and publish lists of countries that delay reporting or do not follow WHO travel and trade guidance. There should be economic incentives for early warning reporting. | The WHA should agree on protocols both for avoiding suppression/delays in data/alerts and for avoiding unnecessary restrictions on trade or travel. | The IHR Review Committee should develop mechanisms to address actions by states that act contrary to WHO travel and trade recommendations. |
| Tiered PHEIC | The WHO should establish an intermediate‐level PHEIC. | The WHO should establish a graded system of warnings through a Standing Emergency Committee. | The WHO should establish a mechanism to generate a daily high‐priority watch list of outbreaks with PHEIC potential to encourage necessary preparedness activities. | |
| WHO Contingency Fund | Member States and partners should contribute to the WHO Contingency Fund, with a target capitalization of US$100 million fully funded by voluntary contributions. | The WHO Executive Board should mandate good governance reforms and in return governments should finance most of the budget with untied funds. | The WHO should create and fund a sustainable contingency fund of US$100 million through contributions determined pro rata with assessed contributions from Member States. | The Centre for Emergency Preparedness and Response should manage the WHO Contingency Fund. Member States should finance the Contingency Fund with at least US$300 million by the end of 2016. |
| WHO Center for Emergency Preparedness and Response | The WHO should establish the Centre for Emergency Preparedness and Response. | The WHO should have a dedicated Centre for Emergency Preparedness and Response. | The WHO should create a WHO Center for Health Emergency Preparedness and Response (CHEPR). | The WHO should build a new Centre for Emergency Preparedness and Response funded by 10% of all voluntary contributions to the WHO. |
| United Nations | There should be procedures for taking health matters to the UN Security Council (UNSC). The UNSC should have incentives and disincentives for improving global health security. The UN should appoint a Special Representative of the Secretary‐General or a UN Special Envoy for major global health events. | A global health committee should be created as part of the UNSC. An Independent UN Accountability Commission should conduct system‐wide assessments of worldwide response to major disease outbreaks. | The UN and the WHO should establish clear mechanisms for coordination and escalation of health crises. | A High‐level Council on Global Public Health Crises should be established within the UN General Assembly. The UN should hold a Summit on Global Public Health Crises in 2018. The secretary‐general should initiate the integration of health and humanitarian crises trigger systems. |
| IHR Emergency Committee | The WHO should establish a transparent and politically protected Standing Emergency Committee. | |||
| Research and Development (R&D) and Medical Countermeasures | The WHO should help accelerate, through a convening role, the development of appropriate diagnostics, vaccines, therapeutics, and medical and information technology. | There must be a framework of norms and rules to accelerate research, govern conduct of research, and ensure access to findings. There is a need to establish a worldwide R&D financing facility for outbreak‐relevant medical countermeasures and other nonpharmaceutical interventions, including personal protective equipment. | The WHO should galvanize acceleration of relevant R&D by establishing a Pandemic Product Development Committee (PPDC) to define priorities and mobilize and allocate resources. The WHO should work with the global R&D stakeholders to catalyze commitment of US$1 billion per year to maintain a portfolio of projects in drugs, vaccines, diagnostics, personal protective equipment, and medical devices coordinated under the PPDC. | The WHO should oversee the establishment and management of a fund of at least US$1 billion to support R&D for vaccines, therapeutics, and diagnostics. The WHO should coordinate the prioritization of global R&D efforts for neglected diseases. |
| Financing, Including the International Monetary Fund (IMF) and the World Bank | The financing of core capacities should be done in close partnership with the World Bank. | The World Bank and other regional banks should create economic incentives for early reporting by committing to disburse emergency funds rapidly. Additionally, regional banks should invest directly in the development of core capacities. A global financing facility for R&D should be established. | The IMF should include pandemic preparedness in its country economic and policy assessments based on outcomes of the external assessments of IHR core capacities. The World Bank and development partners should put in place financial support for lower‐ middle‐income and low‐income countries in delivering the core capacity plans. The World Bank should establish the Pandemic Emergency Facility (PEF). | The WHO should lead urgent efforts to mobilize resources to build IHR core capacities in partnership with the World Bank, regional development banks, and other partners. WHO Member States should increase assessed contributions by at least 10%. The World Bank should rapidly operationalize the PEF. |
| Failed States | The UN Secretary‐General should work with the WHO and other parts of the UN system to develop strategies for sustaining health system capabilities and infrastructure in fragile and failed states and in warzones to the extent possible. |
The WHO is the agency charged with overseeing the IHR. Without effective leadership, the IHR's security framework breaks down. In other words, a strong treaty text is insufficient without a well‐funded and robust operational response.
Major Gaps in the IHR
When the revised IHR were negotiated, Member States aimed to be as inclusive of all public health threats as possible. However, there remained major omissions in the text, notably sample sharing and zoonotic threats.
Sample Sharing and Inequitable Distribution of Benefits
Indonesia sent shock waves around the world in December 2006, when its minister for health, Siti Fadilah Supari, refused to share samples of avian influenza A (H5N1) with the WHO. Indonesia's decision revealed fissures within the international community. Developing countries backed Indonesia's claim that it was unfair to require sharing viruses without any reciprocal obligation to make vaccines and medicines affordable.
The WHO led a 5‐year negotiation resulting in the 2011 Pandemic Influenza Preparedness (PIP) Framework.49 The PIP Framework, however, applies only to pandemic influenza, and not to other novel pathogens such as SARS, MERS, and Zika. The PIP Framework stands entirely outside the IHR. The regulations, furthermore, are mostly silent on the health security issues of sharing biological materials and genetic sequencing data (GSD), as well as equitable access to medical countermeasures. Article 6(2) of the IHR, however, does offer some guidance for information sharing, stating that States Parties shall continue to provide relevant public health information to the WHO following a potential PHEIC notification, including case definitions, laboratory results, source and type of risk, number of cases and deaths, conditions affecting spread, and the health measures that have been deployed. There is no explicit mention of sharing biological materials or GSD, even though one could broadly interpret Article 6(2) to encompass these data. Certainly, biological materials and GSD are pertinent public health information that would shed light on the conditions affecting the spread of disease.
Neither the IHR nor the PIP framework, moreover, addresses a modern biosecurity hazard. In the not‐too‐distant future, scientists will be able to sequence the genetic composition of pathogens, enabling them to re‐create novel viruses and to manipulate their genetic makeup. Although, for example, smallpox has been eradicated, scientists can sequence its genome, synthesize a real smallpox virus using the genetic code, and potentially enhance the virus's ability for airborne transmission. These capabilities pose major biosecurity threats, which the IHR and the PIP Framework do not govern. Harmonizing the IHR and the PIP Framework and closing major coverage gaps would markedly improve health security.
Zoonotic Threats
Approximately 70% of all emerging infectious diseases have a zoological origin, yet negotiators intentionally did not explicitly include animal diseases in the IHR. The drafters were perhaps too deferential to existing regimes, such as the World Organisation for Animal Health (OIE) and the UN Food and Agriculture Organization (FAO). Although the IHR broadly define “disease,” its currently realized scope is narrow, and the regulations do not incorporate a “One Health” approach that fully integrates animal and human health systems. The lack of such an approach could become a particularly salient omission for diseases like Zika with large animal reservoirs and with the primary mode of transmission through an insect source.
The IHR Monitoring Framework seeks to include zoonotic diseases as “other hazards,” but the regulations fail to govern multisectoral engagement and coordination on zoonotic diseases or the laboratory and surveillance capacities required to identify disease in animals. As the world faces the peril of novel zoonotic diseases and the overuse of antibiotics in both humans and animals (exacerbating the global antimicrobial‐resistance crisis), it appears anomalous that the IHR do not facilitate and guide research and practice at the intersection of human and animal health.
The Future of the IHR: Recommendations for Reform
The IHR are the governing framework for global health security, yet they require textual and operational reforms. The WHO Secretariat is engaged in an internal reform process, ranging from the WHO Roadmap for Action on Ebola3 to the Advisory Group on Reform of WHO's Work in Outbreaks and Emergencies with Health and Humanitarian Consequences.50 In addition to the Ebola Interim Assessment Panel,2 the agency established the WHO Review Committee on the Role of the IHR in the Ebola Outbreak and Response.51 On January 30, 2016, the D‐G announced internal reforms, including a single program and incident management strategy to oversee all health emergencies. The D‐G stressed, however, yet again, that the program required sustainable funding from Member States.52
The proliferation of internal and external reform processes could be transformative. This is “the defining moment for the health of the global community.”2 Yet, it is just as likely that the maze of recommendations will lead to weak or muddled reforms. In the sections that follow we offer proposals for fundamental reform of IHR implementation, WHO oversight, and State Party conformance (Table 3). We propose politically feasible pathways to reform to avoid a long history of bureaucratic stagnation. Thus, our proposals balance the ideal with the politically possible.
Table 3.
Compilation of Our Recommended Reforms of the IHR and Their Implementation
| Recommended | |||
|---|---|---|---|
| Reform | Who and Why | Political Mechanism | |
| IHR Core Capacities | Secure national and global commitment to build, strengthen, and maintain IHR core capacities linked directly to independent assessments and financing. | Who: National governments, international organizations, bilateral donors, and funding organizations Why: Global health security is dependent on every nation having the ability to detect, assess, report, and respond to public health emergencies. | No textual change to IHR required for commitment to core capacities Political and financial commitment to support process required by the WHO and other funding entities, such as the World Bank and regional development banks |
| Independently Assessed Metrics | Utilize rigorous metrics assessed by independent evaluators to identify capacity gaps, develop a road map, and identify funding sources to achieve core capacities. | Who: Independent evaluation teams of domestic and external experts with the participation of the WHO, regional and country offices, and civil society Why: Independently assessed, vigorous metrics will provide accurate analysis of national core capacities that can then be used by funding entities to invest in core capacities or for use in insurance mechanisms. | Amendment of Annex 1 of IHR to include measurable benchmarks Tasking the WHO to work with funding entities to create rigorous metrics and organize assessments |
| Harmonization | Harmonize independent assessments and metrics with the GHSA and the OIE's PVS Pathways. | Who: The WHO in collaboration with the GHSA and the OIE Why: Harmonization will ensure a One Health strategy and reduce redundancies for governments exposed to multiple evaluations. | Harmonization incorporated into Annex 1 amendment WHO, GHSA, and OIE enhanced communication and collaboration |
| New Financing Mechanisms | Obtain robust financing to build core capacities as well as to support the WHO's capacity (including surge capacity in emergencies) and to build human resources. | Who: WHO Member States, the World Bank PEF, the GHSA, the WHO Contingency Fund, and the WHO Global Health Reserve Workforce, including the Global Outbreak Alert and Response Network Why: Core capacities cannot be built or sustained without reliable funding. For funding agencies, the return on investment for building core capacities (as opposed to experiencing a large‐scale, uncontrolled outbreak) is significant. | Existing IHR text under Article 44 Increase in WHO Member States–assessed contributions GHSA Action Packages in support of IHR implementation, World Bank PEF, and/or raising resources support through donors’ conferences modeled on the Global Fund |
| Workforce Development | Create national assessments and career plans for a robust clinical and public health workforce and commit to developing and maintaining the workforce. Build an international emergency workforce ready to respond when national systems are overwhelmed. | Who: National governments with international funding and assistance and WHO coordination for emergency workforce Why: Achieving IHR core capacities, and universal health coverage in general, will require developing (and sustaining) a well‐trained, well‐equipped national workforce. In times of emergency, when even a well‐prepared workforce cannot cope, the international community must provide surge capacity. | Domestic workforce supported through national commitment and assessment with funding assistance from the WHO, the World Bank, and other funding agencies WHO commitment to GOARN, the Global Health Reserve Workforce, and foreign medical teams, including major civil society organizations such as Médecins Sans Frontières |
| Emergency Committee Transparency | Ensure independent and transparent Emergency Committee decision making, supported by civil society shadow reporting. | Who: The WHO in collaboration with civil society Why: Independent and transparent Emergency Committees will build public trust. | Administrative action by WHO |
| Tiered PHEIC Process for Early Action | Institute a tiered process for declarations of a PHEIC. Harmonize diverse WHO global alert frameworks with the IHR. | Who: The WHO Why: A tiered PHEIC declaration process would allow for formal action prior to a full declaration. It could also trigger clear operational and financial strategies, such as access to the Contingency Fund. | WHO development of informal guidelines through Article 11 with WHA understanding or WHA adoption of a new IHR annex illustrating the risk gradient without opening the full text for negotiation |
| Enhanced Compliance | Enhance IHR compliance through a series of carrots and sticks to encourage development of core capacities and to keep Member States from taking action inconsistent with the Emergency Committee travel and trade recommendations. | Who: The WHO in consultation with other arbitration bodies such as the WTO, the FAO, and the ICJ Why: States Parties’ disregard for travel and trade recommendations and insufficient devotion of resources to building core capacity undermine the IHR and weaken global health security. | Public request by the WHO for clear rationales from States Parties that take additional measures outside Emergency Committee recommendations Active pursuit of dispute mediation and arbitration under the IHR, use of the Permanent Court of Arbitration Optional Rules for Arbitrating Disputes, and encouragement of challenges through the World Trade Organization or the International Court of Justice WHA amendment of the IHR to elevate temporary recommendations to a binding status |
| Role of Civil Society Organizations (CSOs) | Engage civil society in IHR governance and implementation activities, including shadow reports, inputs to the Emergency Committee, and participation in independent assessments of core capacities. | Who: CSOs, academics, and other interested partners in collaboration with the WHO Why: Civil society is already deeply engaged in caring for communities, monitoring governments, and holding stakeholders to account. CSOs should be engaged as productive partners. | WHO administrative action |
| Linking the IHR with the PIP Framework and Closing Gaps in the Governance of Sample Sharing and Equitable Access to Vaccines and Treatments | Harmonize the IHR and PIP Framework, enhance governance of sample sharing and equitable access, and integrate mechanisms to address biosecurity challenges associated with genomic sequencing. | Who: WHA Member States Why: The IHR do not address sample sharing, PIP does not apply to any agent beyond novel influenzas, and neither agreement addresses genomic sequencing. This leaves major gaps in the global governance of disease. | WHA understandings or addition of an annex to the IHR |
| One Health Approach | Adapt the IHR to take an explicit One Health approach to addressing global health security challenges. | Who: The WHO and WHA Member States in collaboration with the FAO and the OIE Why: Most emerging infectious disease threats are zoonotic, and effectively addressing them requires a One Health approach that fully integrates animal and human health systems. The benefits include better detection and response and confronting the major challenge of antimicrobial resistance. | WHA understandings and operational guidance from the WHO, OIE, and FAO |
Build Robust IHR Core Capacities and Link Them to Metrics and Financing
Meeting IHR core capacities requires mutual responsibility and accountability. It starts with governments dedicating resources to build and sustain health systems. Every State Party should undergo independent, rigorous review of its implementation of IHR core capacities, using measurable metrics and targets, as explained below. Shared responsibilities also require technical assistance and international financing to close capacity gaps. Collective security is assured only by fulfilling these mutual obligations to sustainably build, measure, and finance health systems (Figure 7).
Figure 7.
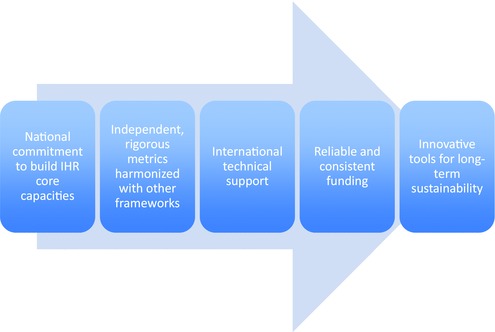
Pathway to Strong, Measured, Funded, and Sustained IHR Core Capacities
Building sustainable core capacities requires fresh thinking by both donors and recipient countries. Too often, countries heavily dependent on external funding follow the priorities of donors, agreeing to erect vertical programs, stove‐piped by disease. Yet, meeting IHR core capacities requires the development of horizontal programs, including diagnostic laboratories that can be used for more than just one pathogen or condition; specimen transport systems that are applicable to all samples; and event‐based surveillance systems designed to pick up unusual or unexpected public health events. Building core capacity also requires integrating these systems into annual budgeting for health system strengthening.
Develop Metrics and Rigorous Assessments
For IHR metrics to be meaningful, valued, and utilized, they must undergo rigorous external evaluations. The WHO should establish an independent evaluation system with a feedback loop and continuous quality improvement. Independent assessments would use evidence‐based metrics and indicators. Unless assessment criteria are clear, transparent, and valid, they will not be fully trusted. The measurable benchmarks for the external assessment process, moreover, should be integrated directly into Annex 1 of the IHR, which contains the core capacity requirements for surveillance and response. It may be necessary either to amend Annex 1 or to operationalize it to incorporate more granular indicators.
Parallel initiatives such as the GHSA and OIE's Performance of Veterinary Services (PVS) Pathways (measuring compliance with OIE standards on veterinary services) should be harmonized with the IHR. The IHR are the only agreement with the international legal and political legitimacy to set global security standards. Harmonizing extant multiple standards within the IHR would be more holistic, ensuring a One Health strategy and reducing redundancies for governments exposed to multiple evaluations.
States often resist external assessment due to sovereignty concerns, but the new system could be designed to foster cooperation. Evaluation teams would comprise both domestic and external experts, so national governments would be fully involved in the process. WHO, regional, and country offices would all play a strategic role. Civil society should be fully engaged, much like in UNAIDS monitoring mechanisms. Expert panels would work constructively and collaboratively to identify capacity gaps, develop a road map, and identify funding sources to achieve measurable benchmarks for success. The mandate, therefore, would not be to give a passing or failing grade but to continuously improve health infrastructure with strategic plans and adequate financing.
The World Bank's Pandemic Emergency Facility (PEF) should tie funding to country cooperation with IHR assessments. Additionally, international donors such as regional development banks, the Global Fund, and philanthropies could create funding streams for national IHR core capacities, also conditioned upon rigorous assessments. All of these measures would reinforce national commitments to build robust health systems, which align well with the UN Sustainable Development Goal of Universal Health Coverage (UHC).53
“What gets measured gets done.” But Laud Boateng, a GHSA Next Generation Fellow from Ghana, shifts this discourse to better reflect national experiences noting, “what gets measured gets done, but only what gets political support gets measured, and only that which is funded gets political support.”54 Thus, tying independent evaluations to external funding would foster cooperation and marshal resources for building core capacities.
Create Reliable and Consistent Financing Mechanisms
Robust financing is required not only to build national health systems but also to support the WHO's own capacities and to ensure a surge in resources in a health emergency. Several financing models could operate separately or in concert. Increasing WHO Member State–assessed contributions would be the most logical funding source. Mandatory dues are more predictable and sustainable than discretionary funding for targeted projects. Moreover, as the treaty oversight agency, the WHO holds the legal obligation to implement the regulations, including securing adequate financing.
Assessed dues, however, are politically fraught. Several high‐income Member States do not have sufficient confidence in the agency to justify an increase in their dues. They also want the discretion to direct where their international assistance is going. Consequentially, it will be necessary to create alternative financing mechanisms. The GHSA Action Packages and the PEF are realistic funding sources, but they should be synchronized with the IHR. The Global Fund offers another model, whereby the WHO and the World Bank could host a donors’ conference to boost international support and cooperation.2, 55 Irrespective of the funding mechanism, ensuring sustainable resources to develop and maintain core capacities would benefit both low‐ and high‐income countries by strengthening security for all.
Invest in Human Resources
Ebola demonstrated that a well‐trained, well‐equipped health workforce is crucial to an effective response, including doctors, nurses, community health workers, lab technicians, infection control practitioners, and public health experts. If there are insufficient health personnel and their numbers are depleted even further by exposure to infection, the health system will fail to control outbreaks. Educating, training, supporting, and protecting health workers is a defining issue for global health security.
Even a well‐prepared workforce may not be able to cope in a public health emergency. In such cases, the WHO must make provision for a surge in human resources, such as through the Global Outbreak Alert and Response Network (GOARN). The 2015 WHA endorsed a Global Health Reserve Workforce but failed to guarantee funding.
Engage Civil Society to Hold States Parties to Account
AIDS advocates demonstrated the power of civil society to demand global health equity.56 Civil society organizations (CSOs) care for their communities, monitor governments, and hold stakeholders to account. As with other spheres of international law, such as in human rights or climate change, civil society could offer “shadow” reports and advocate for funding national capacities and fulfilling IHR and human rights obligations. Harnessing the power of CSOs requires more than incorporating them into existing or new IHR functions. Borrowing from the Framework Convention on Tobacco Control, the WHO could regularly host a Conference of the Parties where civil society could meet with governments to advance IHR implementation. The Framework Convention Alliance (CSOs committed to effective implementation of the Framework Convention on Tobacco Control) has propelled tobacco control reforms. A similar CSO network for IHR implementation could be transformative.
Convene Transparent, Independent Emergency Committee Meetings
After facing criticism for disclosing Emergency Committee members only after the H1N1 PHEIC was terminated, the WHO improved public trust by releasing member names for subsequent Emergency and Review Committees.25 (p16) The WHO also pledged transparency on expert committee members’ conflicts of interest.57 Concerns still persist, however, that Emergency Committees are influenced by politics rather than strictly scientific evidence. For example, the D‐G and Emergency Committee offered no evidence for their decisions regarding H1N1,25 very little for the first Emergency Committee meeting on Ebola,29 and little during the initial meetings on MERS.58 They did give more transparent explanations for polio59 and recent MERS and Zika Emergency Committees.60 The D‐G and Emergency Committee should routinely publicly disclose their evidence and decision‐making processes. Transparency would include full minutes of Emergency Committee meetings, web access to relevant documents, and live updates through social media platforms.
Independent and transparent Emergency Committee decision making would build public confidence, but these reforms are of little value if the D‐G fails to convene an Emergency Committee. Outside the WHO's governing structure and drawing on civil society shadow reports, a committee of independent experts, particularly from academia and civil society, could coalesce to regularly review data on disease outbreaks and propose actions, including recommending that the D‐G convene an Emergency Committee.
Institute a Reliable and Timely PHEIC Declaration Process
The declaration of a PHEIC is the public face of the WHO's outbreak response, but the agency must respond long before an outbreak becomes an international emergency. Beyond the IHR, the WHO has multiple instruments supporting early action. For example, the WHO utilizes the Emergency Response Framework (ERF) to measure the level of risk and to inform the international community of an outbreak's severity in a graduated manner.61 As evidenced during the Ebola epidemic, using 2 distinct sets of governing rules (the ERF and the IHR) confused first responders and the public. Similar confusion arose during the H1N1 pandemic, in which the WHO did not coordinate the 6 pandemic phases in the Pandemic Influenza Preparedness and Response Framework62 (since revised) with the PHEIC. Given the public symbolism of a PHEIC, multiple emergency response frameworks must be integrated with IHR processes.
The WHO Ebola Interim Assessment Panel recommended introducing an intermediate‐level emergency—allowing gradation while retaining the power of a PHEIC.2 A gradient system would not necessarily require a textual amendment to the IHR, as many diplomats fear. The WHO could develop informal guidelines through Article 11, which allows the agency to share information with States Parties, alerting them to potential emergencies in a graduated fashion. Alternatively, the WHA could adopt a new IHR annex that illustrates the risk gradient, limiting negotiations only to the new annex. To maintain credibility, different grades should trigger clear operational and financial strategies. For example, an intermediate‐level emergency could allow the WHO to access resources from the Contingency Fund. Similarly, the World Bank could release PEF funds based on graded emergency declarations by the WHO.63 The promise of international assistance with adequate funding, even at an early stage, could provide additional incentives for States Parties to report a potential PHEIC through the Annex 2 algorithm. A full PHEIC declaration, however, would still be needed to raise the global alert, stiffen political resolve, and mobilize major resources.
Enhance Compliance Through Carrots and Sticks
State disregard for Article 43's “Additional Health Measures” and Emergency Committee temporary recommendations (eg, state travel and trade restrictions and injudicious quarantines) undermines the IHR. For example, during H1N1 and Ebola, States Parties ignored WHO recommendations and imposed additional measures, impeding deployment of critical medical supplies and health workers. Regional and international carriers suspended flights; States Parties banned travel to and from, or trade with, affected countries; and quarantines of health workers returning from the region dampened the charitable instinct to help.
The WHO is not a policing agency that can readily impose sanctions on States Parties for noncompliance with their legal obligations. But it does have various means at its disposal to enhance compliance, which it has failed to use. The D‐G should publicly request clear rationales for and reconsideration of additional measures, while working with States Parties to dismantle harmful policies. The D‐G could more actively encourage States Parties to pursue available dispute mediation and arbitration under Article 56(3). She could similarly steer States Parties toward the Permanent Court of Arbitration Optional Rules for Arbitrating Disputes Between Two States. The WHO and the World Trade Organization (WTO) could similarly encourage use of the WTO Dispute Resolution procedures by States Parties harmed by additional measures. Although the WTO is primarily constituted to adjudicate WTO treaties, it could intervene in cases where state action adversely impacts both public health and international trade—such as a poultry ban during H5N1 outbreaks.
Beyond the WTO, other institutions could encourage IHR compliance. For example, at various points during the H1N1 pandemic, the FAO, OIE, and WTO together with the WHO issued joint statements discouraging trade restrictions on pork and pigs.64, 65 It may also be possible to look to the International Court of Justice (ICJ) when one country's active violation of the IHR causes specific damage to either the population or the economy of a second country.
There is still more the WHO could do to signal strong political commitment to IHR compliance. The WHA, for example, could amend Article 48 to elevate temporary recommendations from the Emergency Committee during a PHEIC to a binding status. Even though States Parties could still disregard their international obligations, more binding treaty language could increase pressure to comply.
Realpolitik: Making IHR Reform Politically Possible
Textual reforms are more difficult to achieve than operational reforms. Reopening the full text of the IHR for revision would result in a multi‐year negotiating process and require considerable resources and could weaken IHR norms and human rights safeguards. Our proposals for reform, therefore, should be achieved, whenever possible, by textual interpretation, understandings, and amendments to specific annexes, rather than the main text.
There is a precedent for amending an IHR annex without reopening the entire text to negotiation (2014 Resolution regarding Annex 7 and Yellow Fever).66 States Parties could find consensus on new language or understandings focused only on particular annexes. Revisions to the main text through textual interpretations or understandings would be politically feasible. In arms control treaties, for example, States Parties use the mechanism of Review Conferences to agree on a series of understandings to guide treaty implementation and State Party compliance. The States Parties decide specifically not to reopen the original text to revision. IHR States Parties could adopt similarly effective political strategies, fully consistent with international law. “Smart” global health diplomacy could enhance IHR functioning without bureaucratic hurdles standing in the way of sensible reform.
The Way Forward
Ten years after the adoption of the IHR, it is time to realize their promise. The unconscionable Ebola epidemic in West Africa opened a window of opportunity for fundamental reform—for both the IHR and the Organization that oversees the treaty. That political window, however, is rapidly closing. Donor fatigue, fading memories, and competing priorities (eg, climate change, the Paris bombings, and fighting the Islamic State) are diverting political attention. The promising results of the vaccine trial Ebola ça Suffit (“Ebola that's enough”),67 although transformative, could further weaken political resolve. Empowering the WHO and realizing the IHR's potential would shore up global health security—a vital investment in human and animal health, while reducing the vast economic consequences of the next global health emergency.
Funding/Support
None.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. No disclosures were reported.
Acknowledgments: The authors thank Eric A. Friedman and Mary C. DeBartolo of the O'Neill Institute for National and Global Health Law, Georgetown University Law Center.
References
- 1. WHO. International Health Regulations (2005) . 2nd edition. Geneva, Switzerland: World Health Organization; 2008. http://whqlibdoc.who.int/publications/2008/9789241580410_eng.pdf. Accessed June 29, 2015.
- 2. WHO. Report of the Ebola Interim Assessment Panel. July 2015. http://who.int/csr/resources/publications/ebola/report‐by‐panel.pdf. Accessed July 30, 2015.
- 3. WHO. 2014 Ebola virus disease outbreak and follow‐up to the Special Session of the Executive Board on Ebola. May 23, 2015. http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_ACONF5‐en.pdf. Accessed June 29, 2015.
- 4. Moon S, Sridhar D, Pate MA, et al. Will Ebola change the game? Ten essential reforms before the next pandemic. The report of the Harvard‐LSHTM Independent Panel on the Global Response to Ebola. Lancet. 2015;386(10009):2204‐2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Commission on a Global Health Risk Framework for the Future. The Neglected Dimension of Global Security: A Framework to Counter Infectious Disease Crises. Washington, DC: National Academy of Medicine; 2016. www.nam.edu/GHRF. Accessed January 30, 2016. [PubMed] [Google Scholar]
- 6. UN Secretary‐General. Press release: Secretary‐General appoints high‐level panel on global response to health crises. April 2015. http://www.un.org/press/en/2015/sga1558.doc.htm. Accessed December 10, 2015.
- 7. White House. Global Health Security Agenda: toward a world safe and secure from infectious disease threats. 2014. http://www.globalhealth.gov/global‐health‐topics/global‐health‐security/GHS%20Agenda.pdf. Accessed February 25, 2016.
- 8. White House. Fact sheet: the U.S. commitment to the Global Health Security Agenda. November 16, 2015. https://www.whitehouse.gov/the‐press‐office/2015/11/16/fact‐sheet‐us‐commitment‐global‐health‐security‐agenda. Accessed December 4, 2015.
- 9. G7. G7 Leaders’ Declaration. June 8, 2015. http://www.interaction.org/document/2015‐g7‐leaders‐declaration. Accessed June 30, 2015.
- 10. Howard‐Jones N. The scientific background of the International Sanitary Conferences, 1851–1938. Geneva, Switzerland: WHO; 1975. http://whqlibdoc.who.int/publications/1975/14549_eng.pdf. Accessed June 30, 2015. [Google Scholar]
- 11. Gostin LO. Global Health Law. Cambridge, MA, and London, UK: Harvard University Press; 2014. [Google Scholar]
- 12. WHO. WHO Constitution. 1946. http://whqlibdoc.who.int/hist/official_records/constitution.pdf. Accessed June 30, 2015.
- 13. WHA. Revision and updating of the International Health Regulations. WHA48.7. 1995.
- 14. WHA. Global health security: epidemic alert and response. WHA54.14 2001.
- 15. WHA. Global public health response to natural occurrence, accidental release or deliberate use of biological and chemical agents or radionuclear material that affect health. WHA55.16. 2002.
- 16. Heymann DL. The international response to the outbreak of SARS in 2003. Phil Trans R Soc Lond B. 2004;359(1447):1127‐1129. http://rstb.royalsocietypublishing.org/content/royptb/359/1447/1127.full.pdf. Accessed June 30, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fleck F. How SARS changed the world in less than six months. Bull World Health Organ. 2003;81(8):625‐626. http://www.who.int/bulletin/volumes/81/8/News0803.pdf?ua=1. Accessed June 30, 2015. [PMC free article] [PubMed] [Google Scholar]
- 18. Heymann DL, Mackenzie JS, Peiris M. SARS legacy: outbreak reporting is expected and respected. Lancet. 2013;381(9869):779‐781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. WHO. States Parties to the International Health Regulations (2005). http://www.who.int/ihr/legal_issues/states_parties/en/. Accessed June 30, 2015.
- 20. WHO. IHR Core Capacity Monitoring Framework: Checklist and Indicators for Monitoring Progress in the Development of IHR Core Capacities in States Parties. Geneva, Switzerland: WHO; 2013. http://www.who.int/ihr/checklist/en/. Accessed April 2014. [Google Scholar]
- 21. Katz R. Use of revised International Health Regulations during influenza A (H1N1) epidemic, 2009. Emerg Infect Dis. 2009;15(8):1165‐1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McNeil DG Jr. W.H.O. estimate of swine flu deaths in 2009 rises sharply. New York Times. November 27, 2013. http://www.nytimes.com/2013/11/27/health/who‐revises‐estimate‐of‐swine‐flu‐deaths.html. Accessed June 30, 2015. [Google Scholar]
- 23. WHO. Swine influenza: statement by WHO Director‐General, Dr Margaret Chan. April 27, 2009. http://www.who.int/mediacentre/news/statements/2009/h1n1_20090427/en/. Accessed July 1, 2015.
- 24. WHO. Implementation of the International Health Regulations (2005): responding to public health emergencies: report by the Director‐General. May 15, 2015: para. 10. http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_22‐en.pdf. Accessed July 1, 2015.
- 25. WHO. Implementation of the International Health Regulations (2005): report of the Review Committee on the Functioning of the International Health Regulations (2005) in Relation to Pandemic (H1N1) 2009. Doc. A64/10. May 5, 2011. http://apps.who.int/gb/ebwha/pdf_files/WHA64/A64_10‐en.pdf. Accessed Aug 3, 2015.
- 26. WHO. Statement on the 5th IHR Emergency Committee meeting regarding the international spread of wild poliovirus. May 5, 2015. http://www.who.int/mediacentre/news/statements/2015/polio‐5th‐statement/en/. Accessed July 1, 2015.
- 27. Horton R. A plan to protect the world—and save WHO. Lancet. 2015; 386(9989):103. [DOI] [PubMed] [Google Scholar]
- 28. Associated Press. Emails: UN health agency resisted declaring Ebola emergency. New York Times . March 20, 2015. http://www.nytimes.com/aponline/2015/03/20/world/ap‐un‐who‐bungling‐ebola.html. Accessed June 30, 2015.
- 29. WHO. Statement on the meeting of the International Health Regulations Emergency Committee regarding the 2014 Ebola outbreak in West Africa. August 8, 2014. http://www.who.int/mediacentre/news/statements/2014/ebola‐20140808/en/. Accessed August 3, 2015.
- 30. WHO. Ebola virus disease outbreak. www.who.int/csr/disease/ebola/en/. Accessed December 10, 2015.
- 31. Fauci AS, Morens DM. Zika virus in the Americas: yet another arbovirus threat. N Engl J Med. Published online January 13, 2016. doi:10.1056/NEJMp1600297. [DOI] [PubMed] [Google Scholar]
- 32. Lucey DR, Gostin LO. The emerging Zika pandemic: enhancing preparedness. JAMA. Published online January 27, 2016. doi:10.1001/jama.2016.0904. [DOI] [PubMed] [Google Scholar]
- 33. WHO and PAHO. Epidemiological alert: neurological syndrome, congenital malformations, and Zika virus infection: implications for public health in the Americas. December 1, 2015. http://www.paho.org/hq/index.php?option=com_content&view=article&id=11599&Itemid=41691&lang=en. Accessed January 31, 2016.
- 34. Petersen EE, Staples JE, Meaney‐Delman D, et al. Interim guidelines for pregnant women during a Zika virus outbreak—United States, 2016. Morb Mortal Wkly Rep. 2016;65(2):30‐33. [DOI] [PubMed] [Google Scholar]
- 35. WHO. Director‐General summarizes the outcome of the Emergency Committee regarding clusters of microcephaly and Guillain‐Barré syndrome. February 1, 2016. http://www.who.int/mediacentre/news/statements/2016/emergency‐committee‐zika‐microcephaly/en/. Accessed February 25, 2016.
- 36. WHO. Statement on the first meeting of the International Health Regulations (2005) (IHR 2005) Emergency Committee on Zika virus and observed increase in neurological disorders and neonatal malformations. February 1, 2016. http://www.who.int/mediacentre/news/statements/2016/1st‐emergency‐committee‐zika/en/. Accessed February 25, 2016.
- 37. Lucey DR. MERS in Korea: why this outbreak can be stopped soon. Center for Strategic and International Studies. June 7, 2015. http://csis.org/files/publication/150608_MERS%20in%20Korea%20Why%20This%20Outbreak%20Can%20Be%20Stopped%20Soon.pdf. Accessed July 1, 2015.
- 38. WHO. Middle East respiratory syndrome—Saudi Arabia . December 4, 2015. http://www.who.int/csr/don/4‐december‐2015‐mers‐saudi‐arabia/en/. Accessed December 8, 2015.
- 39. WHO. Emergency Committee—9th meeting summary: briefing notes on MERS‐CoV . June 22, 2015. http://www.who.int/mediacentre/news/mers/briefing‐notes/update‐22‐june‐2015/en/. Accessed July 1, 2015.
- 40. Gostin LO, Lucey DR. Middle East respiratory syndrome: a global health challenge. JAMA. Published online June 17, 2015. http://jama.jamanetwork.com/article.aspx?articleID=2338303. Accessed July 1, 2015. [DOI] [PubMed] [Google Scholar]
- 41. WHO. Statement on the eighth meeting of the IHR Emergency Committee regarding MERS‐CoV . February 5, 2015. http://www.who.int/mediacentre/news/statements/2015/8th‐mers‐emergency‐committee/en/. Accessed July 1, 2015.
- 42. Gostin LO, Friedman EA. A retrospective and prospective analysis of the West African Ebola virus disease epidemic: robust national health systems at the foundation and an empowered WHO at the apex. Lancet. 2015;385:1902‐1909. [DOI] [PubMed] [Google Scholar]
- 43. WHO. Implementation of the International Health Regulations (2005): report of the Review Committee on Second Extensions for Establishing National Public Health Capacities and on IHR Implementation: report by the Director‐General. March 27, 2015: para. 17. http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_22Add1‐en.pdf. Accessed June 29, 2015.
- 44. Phu TD, Long VN, Hien NT, et al. Strengthening global health security capacity—Vietnam demonstration project, 2013. Morb Mortal Wkly Rep. 2014;63(4):77‐80. [PMC free article] [PubMed] [Google Scholar]
- 45. Lescano AG, Salmon‐Mulanovich G, Pedroni E, Blazes DL. Outbreak investigation and response training. Science. 2007;318(5850):574‐575. [DOI] [PubMed] [Google Scholar]
- 46. United Nations Development Group (UNDG)—Western and Central Africa. Socio‐Economic Impact of Ebola Virus Disease in West African Countries. Addis Ababa, Ethiopia: UNDG; 2015. http://www.africa.undp.org/content/dam/rba/docs/Reports/ebola‐west‐africa.pdf. Accessed January 31, 2016. [Google Scholar]
- 47. Gostin LO, Friedman EA. Ebola: a crisis in global health leadership. Lancet. 2014;384:1323‐1325. [DOI] [PubMed] [Google Scholar]
- 48. WHO. Report by the Director‐General to the Executive Board at its 138th session. January 25, 2016. EB 138/2.
- 49. Fidler DP, Gostin LO. The WHO Pandemic Influenza Preparedness Framework: a milestone in global governance for health. JAMA. 2011;306(2):200‐201. [DOI] [PubMed] [Google Scholar]
- 50. WHO. Advisory Group on Reform of WHO's Work in Outbreaks and Emergencies with Health and Humanitarian Consequences. http://www.who.int/about/who_reform/emergency‐capacities/advisory‐group/en/. Accessed December 10, 2015.
- 51. WHO. Review Committee on the Role of the International Health Regulations (2005) in the Ebola Outbreak and Response. http://www.who.int/ihr/review‐committee‐2016/en/. Accessed December 10, 2015.
- 52. WHO. Global Policy Group statement on reforms of WHO work in outbreaks and emergencies. January 30, 2016. http://www.who.int/dg/speeches/2016/reform‐statement/en/. Accessed January 31, 2016.
- 53. Jha A, Kickbusch I, Taylor P, Abbasi K. Accelerating achievement of the sustainable development goals: a game changer in global health. BMJ. 2016;352:i409. doi:10.1136/bmj.i409. [DOI] [PubMed] [Google Scholar]
- 54. Boateng L. Perspectives in global health security: effective prevention, detection and response to global pandemics. CRDF Global Sponsored Briefing. Washington, DC: October 2015. [Google Scholar]
- 55. The Lancet. Ebola: what lessons for the International Health Regulations? Lancet. 2014;384(9951):1321. http://www.thelancet.com/journals/lancet/article/PIIS0140‐6736(14)61697‐4/fulltext. Accessed March 6, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Buse K, Gostin LO, Friedman EA. Pathways towards a framework convention on global health: political mobilization for the human right to health In: Freeman M, Hawkes S, Bennett B, eds. Law and Global Health. Current Legal Issues, vol. 16. London, UK: Oxford University Press; 2014. [Google Scholar]
- 57. WHO. Frequently asked questions on IHR Emergency Committee . http://www.who.int/ihr/procedures/en_ihr_ec_faq.pdf. Accessed July 3, 2015.
- 58. WHO. Statement on the second meeting of the IHR Emergency Committee concerning MERS‐CoV . July 17, 2013. http://www.who.int/mediacentre/news/statements/2013/mers_cov_20130717/en/. Accessed July 3, 2015. [PubMed]
- 59. WHO. Statement on the meeting of the International Health Regulations Emergency Committee concerning the international spread of wild poliovirus . May 5, 2014. http://www.who.int/entity/mediacentre/news/statements/2014/polio‐20140505/en/index.html. Accessed July 3, 2015.
- 60. WHO. Statement on the ninth meeting of the IHR Emergency Committee regarding MERS‐CoV . June 17, 2015. http://www.who.int/mediacentre/news/statements/2015/ihr‐ec‐mers/en/. Accessed July 3, 2015.
- 61. WHO. Emergency Response Framework . 2013: p. 19. http://apps.who.int/iris/bitstream/10665/89529/1/9789241504973_eng.pdf?ua=1. Accessed July 2, 2015.
- 62. WHO. Current WHO phases of pandemic alert for Pandemic (H1N1) 2009. http://www.who.int/csr/disease/swineflu/phase/en/. Accessed August 3, 2015.
- 63. Standley CJ, Sorrell EM, Kornblet S, Vaught A, Fischer JE, Katz R. New framework for global public health emergency reporting and response. Science. 2015;348(6236):762‐763. doi:10.1126/science.aaa5521. [DOI] [PubMed] [Google Scholar]
- 64. FAO, WHO, OIE, WTO. Joint FAO/WHO/OIE/WTO statement on influenza A (H1N1) and the safety of pork. May 2, 2009. http://www.who.int/mediacentre/news/statements/2009/h1n1_20090502/en/. Accessed July 1, 2015.
- 65. FAO, WHO, OIE. Joint FAO/WHO/OIE statement on influenza A (H1N1) and the safety of pork . May 7, 2009. http://www.who.int/mediacentre/news/statements/2009/h1n1_20090430/en/. Accessed July 5, 2015.
- 66. WHO. Implementation of the International Health Regulations (2005). May 24, 2014. WHA67.13. http://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_R13‐en.pdf. Accessed December 16, 2015.
- 67. Henao‐Restrepo AM, Longini IM, Egger M, et al. Efficacy and effectiveness of an rVSV‐vectored vaccine expressing Ebola surface glycoprotein: interim results from the Guinea ring vaccination cluster‐randomised trial. Lancet. Published online July 31, 2015. http://dx.doi.org/10.1016/S0140‐6736(15)61117‐5. [DOI] [PubMed] [Google Scholar]


