Abstract
Aim
To assess the use of anterior segment optical coherence tomography (OCT) as an adjuvant diagnostic tool in primary acquired melanosis (PAM) by correlating clinical, histopathologic and anterior segment OCT findings.
Methods
Twenty-four patients (24 eyes) with PAM of the conjunctiva, cornea or both were imaged with an anterior segment OCT device (RTVue, model-RT100; Optovue Inc., Fremont, Calif., USA).
Results
Histopathologic diagnosis following excisional or incisional biopsy was confirmed in 13 out of 24 patients (54.6%). OCT images showed a characteristic uniformly thick basal epithelial hyperreflective band (about 20 μm thick) and normal thickness of the overlying epithelial layer in all patients (100%). The hyperreflective band on OCT correlated with the basal epithelial melanocytic pigmentation noted on histopathologic examination but did not vary in thickness between cases with or without atypia.
Conclusions
The characteristic basal epithelial hyperreflective band with normal overlying epithelium in the absence of cysts observed in all cases by anterior segment OCT correlated with clinical and histopathologic features of conjunctival and corneal PAM. Anterior segment OCT may be helpful as a noninvasive diagnostic tool for PAM. Improvement in resolution is necessary to detect melanocytic hyperplasia and aytpia suggestive of malignant potential.
Key Words: Corneal epithelium, Correlative microscopy, Immobilization stress, Melanoma, Noninvasive diagnostic tool, Optical coherence tomography
Introduction
Conjunctival primary acquired melanosis (PAM) is an acquired flat, painless noncystic pigmented lesion of the conjunctiva [1,2]. PAM usually occurs unilaterally in middle-aged individuals (mostly Caucasians) and accounts for 11% of all conjunctival tumors and for 21% of all conjunctival melanocytic lesions [2]. It can either be regarded as benign (PAM without atypia) or as a precancerous lesion (PAM with atypia) [3,4,5,6,7]. More recently, the spectrum of histopathologic features within PAM has been emphasized rather than an absolute distinction between PAM without or with atypia [8]. Histopathologically, PAM without atypia is best characterized by melanocytic hyperpigmentation along the basal epithelial layer of the conjunctiva, while atypia refers to melanocytic hyperplasia comprised of isolated or confluent nests of atypical melanocytes [3,5,7].
Anterior segment OCT is a relatively new diagnostic tool that is being investigated for various anterior segment disorders [9]. Spectral domain OCT offers higher resolution of approximately 5 µm compared to time domain OCT, with a resolution of 10-18 µm [10,11,12,13]. Spectral domain OCT has been investigated as adjunct in the management of ocular surface lesions for diagnosis, treatment planning and monitoring of response [9,14,15,16].
As conjunctival or corneal PAM may be subtle and difficult to document on clinical examination and by conventional photography, we have investigated the role of a commercially available spectral domain anterior segment OCT device in detecting PAM by investigating the correlation of clinical, histopathologic and OCT findings.
Patients and Methods
This case series included 24 eyes of 24 consecutive patients with a clinical diagnosis of conjunctival or corneal PAM. All patients underwent complete ophthalmic examination. After the initial clinical diagnosis was made, slit lamp examination and anterior segment OCT imaging were performed with a commercially available device (RTVue, model-RT100; Optovue Inc., Fremont, Calif., USA), with a resolution of 5 µm [26,000 A-scan(s)] and using a wavelength of 840 nm. Horizontal or vertical scans of the lesions were acquired. Thirteen patients out of 24 underwent excisional or incisional biopsy to confirm the diagnosis.
Results
Twenty-four eyes of 24 patients with a clinical diagnosis of conjunctival/corneal PAM were included in this study. There was a female predominance (15 females vs. 9 males). The mean age was 64 years (range 31-94). Clinical findings included a patch of flat, ill-defined pigmented epithelial lesions noticed on slit lamp examination (100%; fig. 1a, 2a). Nineteen patients (79.6%) had only conjunctival involvement, while in 4 patients (16.6%), the pigmentation was extend across the limbus into the adjacent cornea (fig. 3), and 1 patient (4.16%) had isolated corneal PAM. Conjunctival cysts were absent in all patients (100%). Eleven patients (45%) were observed without biopsy or chemotherapy because the lesion was small, stable over follow-up, or the patient was asymptomatic.
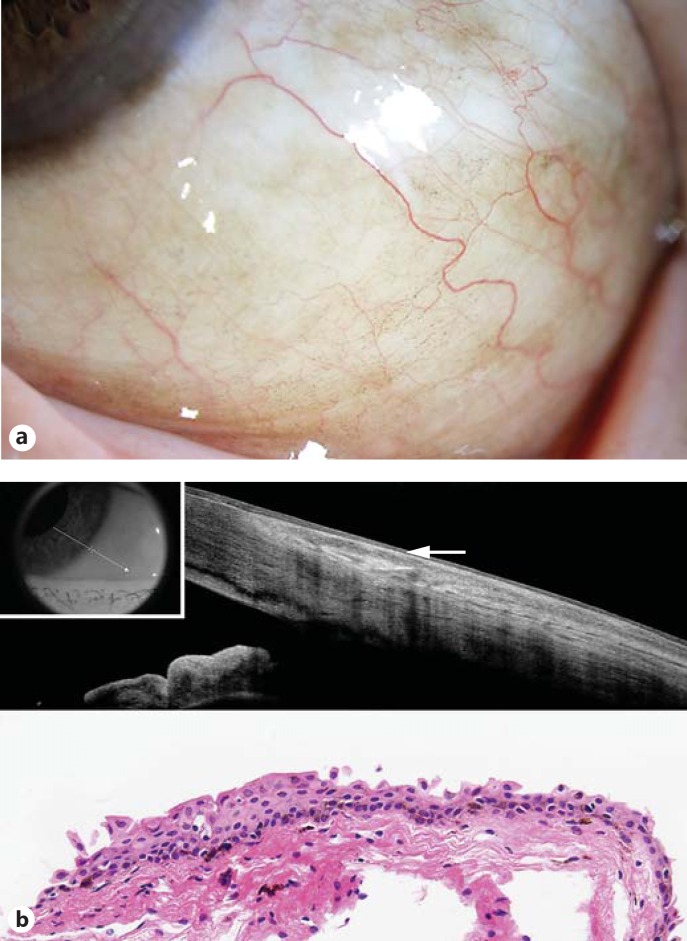
Fig. 1.
a Localized conjunctival PAM without atypia. b Note the basal epithelial hyperreflective band of approximately 20 μm thickness (arrow, above) and the corresponding melanocytic hyperpigmentation that is restricted to the basal layer (below). HE. ×200.
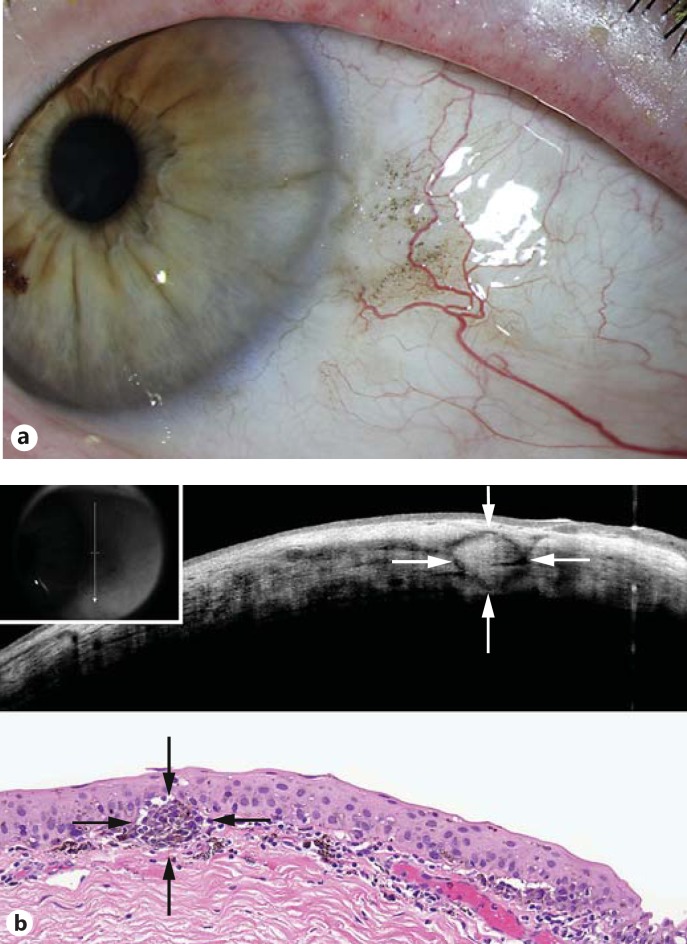
Fig. 2.
a Diffuse conjunctival PAM without atypia. b Note the basal epithelial hyperreflective band of approximately 20 μm thickness (arrow, above) and the corresponding melanocytic hyperpigmentation that is restricted to the basal layer (below). HE. ×200.
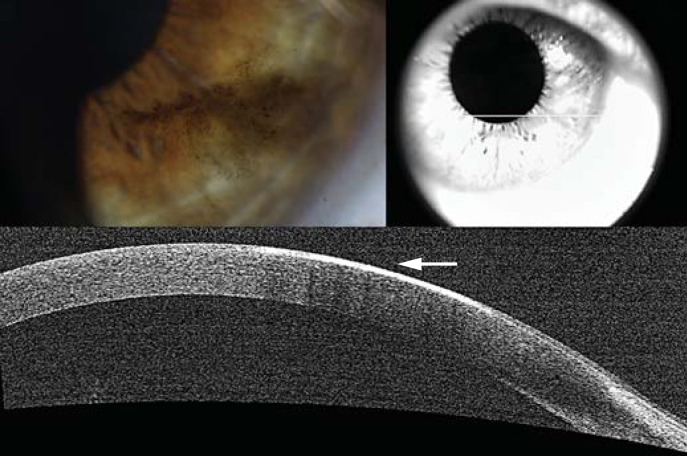
Fig. 3.
Corneal PAM. a Clinical appearance. b Note the corresponding epithelial hyperreflective band (arrow).
Histopathologic specimens of 13 patients (55%) who underwent excisional or incisional biopsy were studied. The specimens showed melanocytic hyperpigmentation within the basal layer of the epithelium in all cases (fig. 1b, 2b). Nine out of 13 patients (69%) additionally showed melanocytic hyperplasia which is compatible with the diagnosis of PAM with atypia (fig. 4b), characterized by cytological (nuclear enlargement, prominent nucleoli and abundant cytoplasm) and architectural atypia (melanocytic extension of the basal layer and nesting of cytologically atypical melanocytes), while 4 patients (31%) showed only melanocytic hyperpigmentation without cytologic or architectural atypia, indicative of PAM without atypia (fig. 1b, 2b). Stromal extension or invasive melanoma and conjunctival cysts were absent in all histopathologic samples (100%).
Fig. 4.
a Localized conjunctival and corneal PAM with atypia. b Note the round stromal hyperreflective zone (arrows, above) with similar appearance of an atypical melanocytic nest (arrows, below). HE. ×200. Without point-to-point correlation between the OCT and the histopathologic image, no definite correlation can be derived.
Anterior segment OCT demonstrated a uniformly thick basal epithelial hyperreflective band in all cases (100%; fig. 2b, 3, 4b). The overlying epithelium was normal in all patients (100%). Optical shadowing (partial or total) of subepithelial layers was observed in 6 patients (25%). Conjunctival cysts were absent in all patients (100%).
The histopathology of examined specimens showed a high correlation with the OCT findings. Cases of PAM sine pigmento were not observed in this series. The melanocytic hyperpigmentation within the basal layer of the epithelium correlated with the hyperreflective band observed on anterior segment OCT (fig. 1b, 2b). Also, normal overlying epithelium and the absence of conjunctival cysts, observed on clinical and histopathologic evaluation, correlated with the OCT findings (100%). Optical shadowing noted on OCT correlated with the amount of melanocytic pigmentation observed on the histopathologic sample. It was not possible to differentiate cases of PAM with atypia from those without atypia by OCT as the hyperreflective band did not vary in thickness between the cases with or without atypia. However, in 1 case with melanoma in situ (PAM with atypia), an atypical melanocytic nest observed on histopathology showed a similar appearance on OCT (fig. 4b).
Discussion
Anterior segment OCT imaging technology provides a noninvasive adjunct diagnostic tool to the gold standard histopathology specimen in ocular surface lesions such as ocular surface squamous neoplasia [14,15,16,17,18]. Limited studies have investigated other conjunctival lesions such as nevi and melanoma [17,18]. We have analyzed the correlation of clinical, histopathologic and OCT findings of conjunctival and corneal PAM using a commercially available spectral domain anterior segment OCT device.
The characteristic features of PAM (with or without atypia) observed in our series include a uniform basal hyperreflective band of approximately 20 μm thickness (100%) with normal overlying epithelium and absence of cysts in all cases (100%). Our observations are similar to those reported by Abou Shousha et al. [14] and Nanji et al. [18] who reported an epithelium of normal thickness and a regular hyperreflectivity of the basal epithelium with the use of ultra-high- and high-resolution OCT in 8 and 8 cases, respectively [14,18]. Cases of PAM sine pigmento were not observed in this series. In such rare cases, there would be no hyperreflective band on OCT, with or without epithelial thickening.
In contrast to PAM, conjunctival nevi characteristically have a high likelihood of conjunctival cysts (77-100%) [17] with normal epithelium [17,18]. Both PAM and nevi have an epithelial layer of normal thickness on OCT [14,18]. In contrast, conjunctival melanoma appears as a hyperreflective, thickened epithelium with extension of hyperreflectivity into the subepithelial layer and significant optical shadowing which may obscure the underlying tissue [14,18]. Characteristically, cysts are absent in melanoma on OCT [18]. Comparative OCT findings of conjunctival and corneal melanocytic lesions are summarized in table 1.
Table 1.
Conjunctival melanocytic lesions: comparison of typical anterior segment OCT features
| Diagnosis | Epithelial hyperreflective band | Stroma | Shadowing | Cyst |
|---|---|---|---|---|
| PAM | +++ | normal | +/− | absent |
| Nevus | ++ | normal/abnornal | ++ | present |
| Melanoma | + | abnormal | +++ | absent |
Optical shadowing is a major limitation of anterior segment OCT. The identification of the posterior extent of the lesion can be obscured by optical shadowing, which is directly influenced by the extent of melanocytic pigmentation and the thickness of the lesion, and hence, limits the use of OCT for full characterization of the nevus or melanoma, as they tend to thicken. The corneal epithelium [17] PAM, which tends to be flat by clinical criteria, is less susceptible to this limitation, as observed in this study. An additional limitation of the anterior segment OCT device used in this study was its inability to differentiate cases of PAM with atypia from those without atypia, as the hyperreflective band did not vary in thickness between the cases with and those without atypia. Meticulous studies with point-to-point correlation between the OCT and histopathologic images are required before any definite conclusions regarding the ability of OCT to detect histopathologic atypia can be reached (fig. 4). Nevertheless, anterior segment OCT is an excellent tool for imaging the anterior surface and lateral extent of the lesions.
In summary, the characteristic basal epithelial hyperreflective band with a normal overlying epithelium in the absence of cysts observed in all cases by anterior segment OCT correlated with clinical and histopathologic features of conjunctival and corneal PAM. Anterior segment OCT may be helpful as a noninvasive diagnostic tool for PAM. Improvement in resolution is necessary to detect intraepithelial melanocytic hyperplasia (atypia) suggestive of malignant potential.
Statement of Ethics
The study protocol has been approved by the Institute's Committee on Human Research. The study application was approved as Exempt Research by the Institutional Review Board for the collection of data in an anonymous manner in which participants were not identifiable.
Disclosure Statement
The authors declare no conflicts of interest.
References
- 1.Gloor P, Alexandrakis G. Clinical characterization of primary acquired melanosis. Invest Ophthalmol Vis Sci. 1995;36:1721–1729. [PubMed] [Google Scholar]
- 2.Shields JA, Shields CL, Mashayekhi A, et al. Primary acquired melanosis of the conjunctiva: experience with 311 eyes. Trans Am Ophthalmol Soc. 2007;105:61–72. [PMC free article] [PubMed] [Google Scholar]
- 3.Folberg R, Jakobiec FA, Bernardino VB, Iwamoto T. Benign conjunctival melanocytic lesions. Clinicopathologic features. Ophthalmology. 1989;96:436–461. doi: 10.1016/s0161-6420(89)32878-8. [DOI] [PubMed] [Google Scholar]
- 4.Griffith WR, Green WR, Weinstein GW. Conjunctival malignant melanoma originating in acquired melanosis sine pigmento. Am J Ophthalmol. 1971;72:595–599. doi: 10.1016/0002-9394(71)90857-9. [DOI] [PubMed] [Google Scholar]
- 5.Folberg R, McLean IW, Zimmerman LE. Primary acquired melanosis of the conjunctiva. Hum Pathol. 1985;16:129–135. doi: 10.1016/s0046-8177(85)80061-7. [DOI] [PubMed] [Google Scholar]
- 6.Folberg R, McLean IW. Primary acquired melanosis and melanoma of the conjunctiva: terminology, classification, and biologic behavior. Hum Pathol. 1986;17:652–654. doi: 10.1016/s0046-8177(86)80175-7. [DOI] [PubMed] [Google Scholar]
- 7.Grossniklaus HE, Green WR, Luckenbach M, Chan CC. Conjunctival lesions in adults. A clinical and histopathologic review. Cornea. 1987;6:78–116. doi: 10.1097/00003226-198706020-00002. [DOI] [PubMed] [Google Scholar]
- 8.Damato B, Coupland SE. Conjunctival melanoma and melanosis: a reappraisal of terminology, classification and staging. Clin Experiment Ophthalmol. 2008;36:786–795. doi: 10.1111/j.1442-9071.2008.01888.x. [DOI] [PubMed] [Google Scholar]
- 9.Medina CA, Plesec T, Singh AD. Optical coherence tomography imaging of ocular and periocular tumours. Br J Ophthalmol. 2014;98:1140–1146. doi: 10.1136/bjophthalmol-2013-304299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ackerman AB, Sood R, Koenig M. Primary acquired melanosis of the conjunctiva is melanoma in situ. Mod Pathol. 1991;4:253–263. [PubMed] [Google Scholar]
- 11.Wang M, Luo R, Liu Y. Optical coherence tomography and its application in ophthalmology. Yan Ke Xue Bao. 1998;14:116–120. [PubMed] [Google Scholar]
- 12.Jancevski M, Foster CS. Anterior segment optical coherence tomography. Semin Ophthalmol. 2010;25:317–323. doi: 10.3109/08820538.2010.518473. [DOI] [PubMed] [Google Scholar]
- 13.Radhakrishnan S, Rollins AM, Roth JE, et al. Real-time optical coherence tomography of the anterior segment at 1310 nm. Arch Ophthalmol. 2001;119:1179–1185. doi: 10.1001/archopht.119.8.1179. [DOI] [PubMed] [Google Scholar]
- 14.Shousha MA, Karp CL, Canto AP, et al. Diagnosis of ocular surface lesions using ultra-high-resolution optical coherence tomography. Ophthalmology. 2013;120:883–891. doi: 10.1016/j.ophtha.2012.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kieval JZ, Karp CL, Abou Shousha M, et al. Ultra-high resolution optical coherence tomography for differentiation of ocular surface squamous neoplasia and pterygia. Ophthalmology. 2012;119:481–486. doi: 10.1016/j.ophtha.2011.08.028. [DOI] [PubMed] [Google Scholar]
- 16.Shousha MA, Karp CL, Perez VL, et al. Diagnosis and management of conjunctival and corneal intraepithelial neoplasia using ultra high-resolution optical coherence tomography. Ophthalmology. 2011;118:1531–1537. doi: 10.1016/j.ophtha.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 17.Shields CL, Belinsky I, Romanelli-Gobbi M, et al. Anterior segment optical coherence tomography of conjunctival nevus. Ophthalmology. 2011;118:915–919. doi: 10.1016/j.ophtha.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 18.Nanji AA, Sayyad FE, Galor A, Dubovy S, Karp CL. High-resolution optical coherence tomography as an adjunctive tool in the diagnosis of corneal and conjunctival pathology. Ocul Surf. 2015;13:226–235. doi: 10.1016/j.jtos.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]