Abstract
Objective
The purpose of this scoping review was to identify evidence describing benefits of interventions provided in ICU-survivor follow-up clinics.
Background
Advances in intensive care unit (ICU) treatments have increased the number of survivors who require specialized care for ICU-related sequelae. ICU survivor follow-up clinics exist yet little is known about the nature and impact of interventions provided in such clinics. A scoping review of publications about in-person post-ICU follow-up care was undertaken.
Method
Ten databases were searched yielding one-hundred eleven relevant unique publication titles and abstracts. Sample heterogeneity supported using a scoping review method. After excluding non-related publications, 33 reports were fully reviewed. Twenty international publications were included that described ICU follow-up clinic interventions and/or outcomes.
Results
Authors discussed very diverse interventions in 15 publications, and 9 reported some level of intervention effectiveness. Evidence was strongest that supported the use of prospective diaries as an intervention to prevent or improve psychological symptoms whereas evidence to support implementation of other interventions was weak.
Conclusions
Although ICU follow-up clinics exist, evidence for interventions and effectiveness of treatments in these clinics remains under-explored.
Implications
ICU survivor follow-up clinics provide a venue for further interdisciplinary intervention research that could lead to better health outcomes for ICU survivors.
The Institute of medicine (IOM) has made repeated calls to remodel heath care delivery systems that offer high quality outcomes at a reasonable, sustainable cost (1, 2). Healthcare providers and researchers have been charged to devise innovative processes that target previously ignored gaps in care delivery such as transitions between points of care. (3) One particularly difficult transition is experienced by patients who have been discharged home after surviving an acute, critical illness or injury necessitating care in an intensive care unit (ICU). People who survive their illness or injury and are entering a recovery period post-ICU treatment are known as ICU survivors. The impact of critical illness upon physical and mental health post-ICU has been well demonstrated; however best practices for specialized clinic settings, modes of treatment, and efficacy of follow-up care for prevalent ICU sequelae remain under-explored and under reported. (4)
Problems known as post intensive care syndrome (5) (PICS) that are experienced by ICU survivors after returning home include decreased physical function (6), continuation of pain (4), global cognitive impairment especially for memory and executive function (7), emotional instability (8), and anxiety and depression (9). Often patients face multiple health-related complications that, together or in unique combinations, add significant self-care complexity, diminish quality of life, and decrease their ability to return to work and social activities that subsequently affect long-term health. (4, 5) Even though primary care clinics provide a range of follow-up services, comprehensive specialized support for the unique long-term health problems that are typical of ICU survivors remains lacking.
A healthcare model in the form of specialized clinics could provide the necessary services specific to ICU survivors’ healthcare needs. In 2006, Griffiths and colleagues (10) conducted a survey of 298 ICUs in the United Kingdom (UK) and reported that there were 80 intensive care follow-up clinics existing at that time. No similar comprehensive national surveys are available for other countries. Furthermore, little documented evidence of health outcomes for patients who attend such clinics has been provided (11). An ever-increasing number of ICU survivors and a push from IOM have resulted in the inception of critical care follow-up clinics in the United States (4, 12, 13, 14). Hence, a comprehensive appraisal of published literature regarding the presence and efficacy of existing ICU survivor follow-up clinics was needed to define a future role for such healthcare delivery models (15).
Method
The terms scoping study and scoping review are often used interchangeably (16) and are similarly described in the literature. We have chosen to use the term scoping review for this report and used the scoping method guidelines set out by Arksey and O’Malley (16) and further developed by Levac, Colquhoun, and O’Brian (17) and Daudt, van Mossel, and Scott (18). The goal of a scoping review is to present a comprehensive, broad view of a topic that is represented in the literature by reports about a range of projects that used varied research methods. Arksey and O’Malley (16) and others (17, 18) offer the following four reasons for choosing a scoping method in conducting a review: 1) to describe the extent and nature of existing published research, 2) to evaluate the possibility of conducting a systematic review, 3) to disseminate a summary of extant research, and 4) to point to existing literature gaps (18). The purpose of our scoping review incorporates reasons one and three; to describe and disseminate the extent and range of published literature about ICU survivor follow-up clinic interventions and outcomes. Additionally, consistent with number three, we sought to identify existing gaps in high-quality evidence that supported the interventions.
We followed Arksey and O’Malley’s (16) stepwise process to carry out our scoping review: 1) construct a broad research question(s), 2) conduct a comprehensive literature search, 3) select articles based on inclusion and exclusion criteria, 4) organize the data according to topics or themes, 5) provide a descriptive summary of the findings, and an optional 6) hold a conference with stakeholders to discuss the relevance of the findings (16). We did not formally include the sixth step however we are a multidisciplinary research team with a clinical focus and could be considered stakeholders simply by the nature of our practice settings. The following is a description of our process and a report of our findings and recommendations.
Research Question
Arksey and O’Malley; (16) Levac, Colquhoun, and O’Brian (17); and Daudt, van Mossel, and Scott(18) suggested that when using the scoping method, researchers should follow rigorous procedures beginning with a broad question that guides the process. We defined ICU-survivor follow-up clinic care as events that included at least one in-person clinic encounter with a healthcare professional that occurred in a designated primary care area which specialized in the treatment of ICU survivors. We sought to identify published literature that was consistent with our definition of ICU follow-up clinics and that contributes to the literature about follow-up care for ICU survivors. Our scoping review was conducted to answer the following questions:
Has there been published evidence describing ICU survivor follow-up clinics that included at least one in-person clinic encounter?
What interventions were provided at ICU survivor follow-up clinics and were these interventions beneficial to ICU survivors?
Comprehensive Search Strategy
Globally, primary care practice settings are diverse and tight control over study variables is difficult, so we chose to conduct a scoping review instead of a systematic review because we were willing to decrease internal validity to increase a broader view and, thus, increase generalizability. (49) Given the heterogeneous nature of published research about ICU survivor follow-up clinics, we collectively decided to include all types of research reports such as efficacy trials (randomized controlled trials) and effectiveness studies (other designs). (49, 50) This allowed us to report all measures and outcomes. Accordingly, in keeping with the inclusive nature of scoping reviews, we chose to incorporate all studies that were relevant to answering our second question.
The following search terms were used: Intensive Care Unit, intensive care, critical care, survival, survive, survivor(s), ambulatory care, followup/follow-up clinic, and rehabilitation services. Search terminology included controlled vocabulary terms and keywords as necessary to achieve the best retrieval from each database. The above terms were combined with observational and randomized control trial study design and limited to English speaking human subjects. Studies that enrolled patients under 18 or burn unit survivors or used phone-call-only follow-up, post-ICU home visits, mailed questionnaires, and outpatient primary care clinics were excluded.
Publications were identified by an experienced librarian using electronic databases and ‘cited by’ and ‘articles citing’ features where available. Databases that were included in the search were Ovid MEDLINE® (1946-March 2015), Ovid MEDLINE® Daily Update, Ovid MEDLINE® In-Process & Other Non-indexed Citations, Cochrane Library (Table 1. Search), PubMed (1947-January 2016), EMBASE™ (1947-March 2015), Cumulative Index of Nursing and Allied health Literature Plus with Full Text (1937-January 2016) and United Kingdom National Health Service Economic Evaluation Database (NHS EED). Unless stated otherwise, all databases were last searched in March 2015. Manual searching was also performed. All references in review articles and cross-referenced studies were hand searched and compared to our review criteria for possible inclusion. Bibliographies and references of relevant articles were further screened for other relevant studies.
Table 1.
Example of one Search Schema
| Search Name: ICUSurvivors | ||
|---|---|---|
| Last Saved: 06/05/2015 | ||
| Description: Cochrane Library | ||
| ID | Search | Results |
| #1 | MeSH descriptor: [Intensive Care Units] explode all trees | 2503 |
| #2 | intensive care survivors | 587 |
| #3 | critical care survivors | 562 |
| #4 | #1 or #2 or #3 | 3416 |
| #5 | MeSH descriptor: [Ambulatory Care] explode all trees | 3451 |
| #6 | followup clinic or follow-up clinic | 10701 |
| #7 | rehabilitation services | 4356 |
| #8 | #5 or #6 or #7 | 17579 |
| #9 | #4 and #8 | 247 |
| #10 | MeSH descriptor: [Observational Study] explode all trees | 0 |
| #11 | MeSH descriptor: [Randomized Controlled Trial] explode all trees | 133 |
| #12 | #10 or #11 | 133 |
| #13 | #12 and (adult or middle aged or aged) | 41 |
| #14 | telephone or home visit or (mail and questionnaire) | |
| or burn unit outpatient clinics or (no intervention) | 74261 | |
| #15 | #13 not #14 | 39 |
Article Selection using Inclusion/Exclusion Criteria
Titles and abstracts were screened for relevancy by all authors. References of included studies were manually evaluated and articles citing these studies were also reviewed. All articles were independently assessed by three authors (SL, SO, JM). Pertinent data were abstracted from publications and organized using a table format with predefined columns labeled authors, method, setting, patient characteristics, interventions, outcomes, and type of follow-up. Although a variety of validated tools exist to evaluate study quality, they are often used to rate the quality of publications in systematic and other types of reviews. Quality evaluation tools are not typically used in scoping reviews (16, 17) because of the broad nature of the included publications so no tools for assessment of quality were used. Any articles that were questioned related to inclusion or exclusion criteria were resolved by author discussion until consensus was reached.
We screened 111 publication titles and abstracts for inclusion in this review of which 78 were excluded because they did not meet inclusion criteria (Fig. 1 Flow Diagram). After thirty-three remaining (4, 5, 12, 19–48) full-text reports were evaluated, 12 were excluded (5, 19, 21, 22, 24, 36, 37, 39, 40, 43, 46, 48) because the subject matter was inconsistent with our aims. One article (33) was excluded because smoking cessation is a public health problem and therefore is not specifically characteristic of ICU survivors’ spectrum of symptoms. We retained articles describing clinics created specifically for treatment of IUC-survivors that reported descriptive statistics about the population and frequency of post-ICU symptoms. We included 20 publications to answer research questions one (Table 2) and 9 for question two (Table 3). We frequently revisited our eligibility criteria to prevent selection bias.
Figure 1.
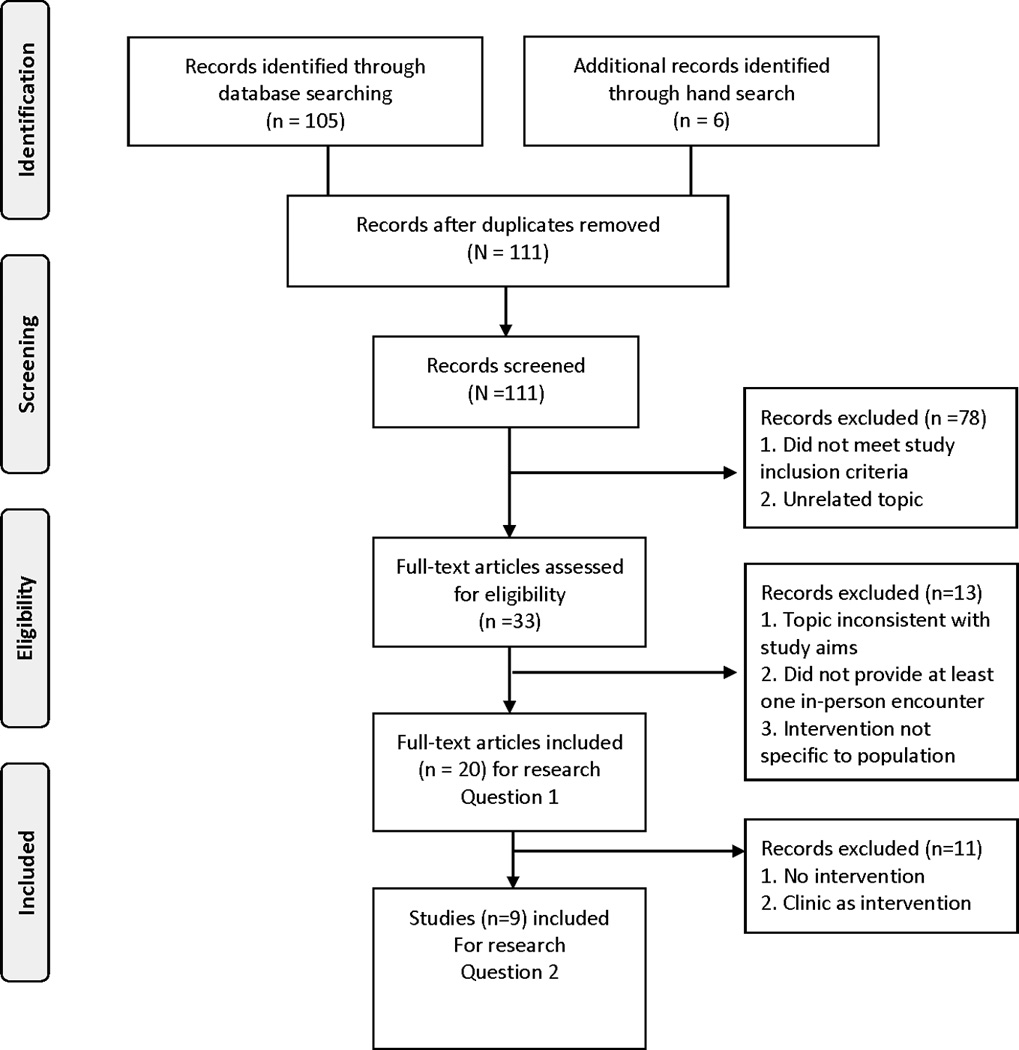
Table 2.
Studies Included in Final Analysis
| Study | Country | Participants (N) | Inclusion Criteria |
Study Type | Clinic | Intervention |
|---|---|---|---|---|---|---|
| Combe D. (2005). (22) | UK | N=35 | ICU LOS≥4 days |
Prospective cohort study | Yes | Patients were given diaries at the first follow up clinic appointments. An informal meeting was held to answer questions. |
| Cuthbertson BH et al. (2009). (23) | Scotland | N=286 n=143 intervention n=143 standard care control 192 completed one year follow-up |
Patients discharged from ICU |
RCT, non-randomized | Yes | Clinic follow-up compared to standard hospital care. |
| Eddleston JM et al (2000). (25) | UK | N=143 | Patients discharged from ICU |
Prospective study | Yes | No. |
| Flaatten H. (2005). (27) | Norway | N/R | N/R | Editorial and descriptive population statistics |
Yes | A regular out-patient clinic for former ICU patients. |
| Fletcher SA et al. (2003) (28) | UK | N=22 | ICU LOS ≥28 days |
Prospective follow-up study | Yes | No |
| Granja C et al. (2003) (29) | Portugal | N=29 | Acute respiratory distress syndrome (ARDS) |
Prospective, matched, parallel cohort study |
Yes | No |
| Griffiths, J. et al. (2006) (30) | UK | N=127 | ICU LOS ≥ 3 days |
Observational | Yes | No |
| Hall-Smith, J. et al. (1997) (31) | UK | N=26 | ICU LOS ≥5 days |
Unstructured client-led interviews | Yes | No |
| Jones C et al. (2003) (35) | UK | N= 126 | ICU LOS ≥ 48 hours and mechanically ventilated |
RCT, | Yes | Control patients receiving ward visits, three telephone calls at home, and clinical appointments at 8 weeks and 6 months Intervention group received the same plus a 6-week self-help rehabilitation manual. |
| Jones C et al. (2008) (34) | UK | N=39 | ICU patients | prospective audit of new ICU counseling service |
Yes | Nurse counseling. |
| Jones C et al. et al. (2010) (32) | Denmark, Italy, Norway, Portugal, Sweden, UK |
N=352 n= 177 intervention n=175 control |
ICU LOS≥72 hours and mechanically ventilated ≥ 24 hours |
RCT | Yes | Intervention patients received their ICU diary at 1 month following critical care discharge and assessment of development of acute PTSD was made at 3 months. |
| Khan BA et al. (2015) (12) | United States |
N=53 | ≥48 hours on mechanical ventilation or ≥ 48 hours of delirium |
Descriptive | Yes | Clinic visit, multidisciplinary care plan, cognitive exercises, physical exercises |
| Knowles RE et al. (2009) (36) | UK | N=36 n=18 control n=18 intervention |
ICU LOS ≥48 hours | RCT | Yes | Compared the effect of having access to an ICU diary accompanied by verbal feedback from an ICU nurse on psychological well-being in a no-treatment control condition. |
| Kvåle R et al. (2003) (37) | Norway | N=346 | ICU LOS ≥24 hours |
Prospective cohort study | Yes | Responders to the survey were offered follow-up outpatient consultations. |
| Modrykamien, AM. (2014) (4) | United States | N/R | N/R | Descriptive | Yes | Clinic follow-up and referral. |
| Petersson CG et al. (2011). (40) |
Sweden | N=96 | ICU LOS ≥72 hours |
Exploratory | Yes | Ward visit, clinic visit, and follow-up call or clinic visit. |
| Samuelson KAM et al. (2009). (43) | Sweden | N=170 | ICU LOS ≥48 hours |
Descriptive and Evaluative | Yes | Acute care ward visits 1–3 days after ICU discharge, a patient information pamphlet and a telephone number for an after-care nurse, follow-up letter to provide information, and a follow-up consultation 2–3 months after ICU discharge, |
| Schandl AR et al. (2011). (44) |
Sweden | N=61 | ICU LOS ≥4 days |
Descriptive | Yes | Ward visit, ICU diary and offer for follow-up in the clinic at 3, 6, 12 months post ICU discharge. |
| Sukantarat K. et al. (2007). (46) |
UK | N=51 45 patients completed the study |
ICU LOS ≥3 days |
Prospective Descriptive, Correlational | Yes | Patients were recruited in a follow-up clinic at 3 and 9 mos. No report about the clinic was included. Psychologist discussed survey findings. |
| Waldmann CS. (1998). (47) | UK | N/R | N/R | Theoretical paper with descriptive statistics |
Yes | Treatment and referral to specialists. |
LOS = Length of stay; all patients were age ≥ 18 years; N/R = not reported; RCT: Randomized Controlled Trial
Table 3.
Interventions with Patient Outcomes (Question 2)
| Interventions | Outcomes |
|---|---|
| ICU Diary provided at two month follow-up clinic visit followed by informal meeting (22) |
Primary Outcomes: Improved understanding of patient experience Patients reported that the diary was helpful in recovery goal-setting and improved family communication. |
| Self-monitored physical rehabilitation program initiated before hospital discharge, nurse led clinic assessment at 3, 9 & 12 mos., discussion of ICU experiences, ICU visit, medication review, referral based on HADS (Hospital Anxiety and Depression Scale)score. Cost analysis. (23) |
Primary outcome: No statistical difference in the physical or mental components of the Short Form-36 (SF-36) Increased cost. Secondary outcome: No statistical difference in quality of life scores on SF-36 and EuroQol EQ-5D. |
| Ward visits, three telephone calls at home, and clinic appointments at 8 weeks and 6 months plus a 6-week self- help rehabilitation manual. (35) |
Primary outcomes: Improved SF-36 physical function scores at 8 weeks and 12 months. Trending improvement but not significant in depression at 8 weeks (HADS) No difference in anxiety and PTSD symptoms. |
| Nurse counseling (34) | Primary outcomes: Patients required fewer counselling sessions No difference in Psychological Outcome Profiles No difference in treatment between the two sites and counselors as measured by the Clinical Outcomes in Routine Evaluation Outcome Measure. |
| Intervention group patients received their prospective ICU diary at 1 month following ICU discharge. A final assessment of the development of acute PTSD was made during a meeting at 3 months. (32) |
Primary outcome: Incidence of new onset PTSD was significantly reduced (p = 0.02) using the Posttraumatic Stress Symptom-14). Secondary outcome: Patients with very high scores in the intervention group showed the largest reduction of symptoms. |
| Interdisciplinary team assessment (critical care physician, nurse, social worker) and creation of a personalized care plan including cognitive exercises, self-management training manuals, pharmacologic and non-pharmacologic prescriptions, and proactive referrals to community resources, neuropsychologists and physical rehabilitative services. (12) |
Longitudinal improvement between visits 1 and (average 2.5 months later) 2 in cognitive, functional, and behavioral symptoms (p < .01) as measured by the HABC-M |
| Access to a prospective ICU diary kept by ICU nurses about events, treatments, procedures, and condition accompanied by verbal feedback from an ICU nurse on psychological well-being compared to a no-treatment control condition. (36) |
Prospective diaries designed to assist patients in understanding what happened to them in ICU significantly decreased anxiety and depression scores almost 2 months after patients' discharge from intensive care unit. |
| Ward visits 1–3 days after discharge from ICU Patient information pamphlet including a number for after- care nurse and follow-up information letter. Consultation 2–3 months after discharge including discussing and explaining the ICU experiences using hospital records. Patients’ diaries with photographs were handed over. Rehabilitation counselling about long-term health including identification of existing problems. A visit to the ICU if desired. A return clinic visit for 1–2 months later if needed. (43) |
Primary outcomes: 82% factual and delusional memories of the ICU 51% remembered aftercare nurse ward visit 60% remembered the information pamphlet Those who remembered, rated the ward visit experience 9.3 and 9.7 (out of 10). The 2-month follow-up consultation achieved a median VAS rating of 9.8 from both patients and kin. Some patients described in detail how the information, explanations and support had enabled them to complete ‘the intensive care stay puzzle’ and had helped them move on. |
| ICU nurse ward visit, ICU diary, and invitation to follow- up in the clinic at 3, 6, and 12 months post ICU discharge. Clinic: TST, Grip strength and 6 min walk with referrals to PT or home instructions as necessary. Nurse: ICU diary discussion and ICUM results used to understand ICU events, the patient’s current status (including work status), and cognitive and/or social problems. Referral to a counsellor if necessary. Six-month visit included a visit to the ICU to help patients understand surreal ICU memories. Physician: Summary of medical tests and treatments during ICU stay; discussed Impact of Events Score (IES), HADS and SF-36 scores; psychiatrist or pain specialist referral if needed. (44) |
Primary outcomes: n=61 Physical: Patients attending three consultations showed improved physical performance in 6 Minute Walk Test and leg strength over time. Psychological: 34 scored high in the psychological screening: 20 had isolated IES scores >25 six patients had an isolated HADS subscale score >10 8 patients had a combined high score on both. Of five patients evaluated by a psychiatrist 1 was diagnosed with PTSD 3 with depression 1 height phobia caused by the fall leading to ICU admission 1 generalized anxiety disorder Patients who completed three follow-up visits demonstrated an improvement in their HADS anxiety score. |
VAS = visual analog scale; PTSD=post-traumatic stress disorder: HABC-M = Healthy Aging Brain Center Monitor; ICUM=Intensive Care Unit Memory tool.
Organization of the Data
To answer question one, we identified 20 publications (Table 2) that described outpatient clinic settings which provided at least one in-person encounter with any healthcare provider. The follow-up clinics for ICU survivors were mainly offered in European countries; 10 were located in the UK, three in Sweden, two in Norway, two in the United States, one in Scotland, one in Portugal, and one multi-nation report.
Study authors described ICU follow-up clinics using varying degrees of detail. In publications where clinic healthcare providers were identified, they were either nurses or physicians who worked alone or as leaders of a team. Of these clinics, there were five that were nurse-led clinics (23, 34, 36, 40, 42), four physician run clinics (25, 27, 32, 35); six multidisciplinary clinics (4, 12, 22, 31, 44, 47); and five reports did not specify the providers’ discipline (29, 30, 37, 46).
Of the 20 publications that met inclusion criteria for question one, we excluded five reports for question two because, although descriptive statistics and characteristics of clinic patients were provided, little or no detail about the clinics was discussed and no interventions were offered. In 6 of the remaining 15 publications (4, 27, 37, 40, 46, 47) the clinic was assumed to be the intervention for ICU survivors and, thus, were also excluded. To answer question two, the remaining 9 articles provided some detail about clinic-provided intervention(s) and are displayed in Table 3. Although study designs were not always randomized controlled trials (RCT), we included publications where authors reported some level of evidence for the effectiveness of an intervention (12, 22, 23, 32, 34–36, 43, 44).
Results
Topics and Themes
Interventions provided at the ICU-survivor follow-up clinic for treatment of common complications following an ICU stay and published evidence of treatment effectiveness.
Self-monitored interventions
Jones et al. (35) tested the effectiveness of a 6 week manual-based, self-help rehabilitation exercise intervention on post-ICU physical and psychological recovery. Hospitalized patients were recruited and randomized to either routine follow-up consisting of a ward visit (hospital room visit), a series of three telephone calls, and clinic appointments at 2 and 6 month or a routine follow-up plus a 6-week self-help rehabilitation manual intervention. Subjects were responsible for carrying out and self-monitoring their own progress followed with an in-person clinic visit at 8 weeks and 6 months. The manual, which contained 93 pages of instructions and illustrations that focused on a broad range of common post-ICU symptoms, was presented to intervention patients and family members by a nurse. Phone calls were made that targeted reinforcing use of the manual. Recovery was measured by comparing state-trait anxiety, social support, anxiety and depression, PTSD, memory of the ICU experience, and premorbid quality of life scores at recruitment to scores at 6 months. Researchers reported significant improvement in physical function (p= 0.006) and a trend toward lower levels of depression. However, levels of anxiety and PTSD were not significantly different between the two groups. Evaluation of the intervention effect relied upon self-report and self-monitoring of the intervention which might have been influenced by patients’ recall of their own pre-morbid state and assessment of their success at executing the instructions in the rehabilitation manual.
In a multicenter, RCT of 286 patients age ≥ 18 years, Cuthbertson et al. (23) compared a self-monitored physical therapy program initiated during hospitalization, nurse-led discussions of ICU experiences with optional ICU visit, medication review, referral to a clinic physician, and specialist referral for psychological treatment to usual care. Health related quality of life (HRQOL) outcomes were measured by the SF-36. Investigators found no intervention effect on HRQOL (effect size 1.1; 95% CI; 1.9–4.2) or on any comparison measures of anxiety or depression. Furthermore, investigators found that the ICU follow-up services were significantly more expensive than usual care. Important limitations were that the trial was not blinded, data were collected via mail, and few patients were accompanied by caregiver/support persons (which affected reconciliation of ICU experiences).
Diaries
In five publications (22, 32, 36, 43, 44), researchers employed ICU diaries as interventions. Diaries were prospectively constructed in the ICU by nurses, healthcare providers, visitors, and family members and included narratives and photographs that documented daily experiences, events, and observations. Of the five reports, two tested diaries as part of RCTs (32, 36), one as a prospective cohort pilot study (22) and two incorporated diaries into an aftercare program (43, 44). In two studies, an ICU diary was the only intervention tested and both had follow-up appointments; one at 2 months to answer questions about the diary (22) and the other at 3 months to evaluate effects of the diary on development of PTSD (32).
In one of the two RCTs, Jones et al. (32) tested the effect of prospective ICU diaries on new onset PTSD and found that at one month post-discharge, the incidence of acute PTSD in the treatment group was reduced compared to the control (5% vs 13%, p<.002). In the second RCT, Knowles and Tarrier (36) measured the effect of ICU diaries discussed with a nurse on levels of anxiety and depression compared to usual treatment for matched controls. The intervention group experienced significant decrease in anxiety (p ≤ 0.05) and depression (p ≤ 0.005).
In a cohort pilot study, Combe (22) provided a diary at the first follow-up clinic appointment and invited patients to read them and return for a discussion session. Patients who returned for the discussion (100%) reported that the diary helped them understand what had happened and that they were able to “move on.” No descriptive statistics were provided.
Samuelson and Corrigan (43) tested a combination of a prospective diary, ward visits, a patient information packet, a follow-up consultation (2–3 months post ICU discharge), and feedback to the ICU staff. Of 144 patients who were discharged from ICU, 79 participated in the aftercare program; 51 in-person follow-up clinic visits, and 28 phone consultations. After one year, the 51 patients who consulted in the clinic rated service satisfaction by using a visual analog scale that was created specifically to measure study satisfaction (1- poor and 10- excellent). Satisfaction scores for both patients and family members was 9.8. Based on feedback from patients about their ICU experiences, the study team determined that 82% of patients had memories of their ICU stay and 41% of these had delusional memories. Small sample size, large percentage lost to follow-up, and telephone evaluation compromised quality and generalizability. Schandl and colleagues (44) also incorporated ICU diaries into a multicomponent aftercare program. The impact of the diary component of the intervention was neither measured nor mentioned in the analysis.
Experiential interventions
Two publications detailed experiential interventions (12, 34). Authors et al. (12) visited ICU survivors on acute care units to invite them for follow-up care in the Critical Care Recovery Center (CCRC). Patients received a telephone call from the CCRC nurse approximately two weeks after hospital discharge who used a questionnaire to gather baseline data. An in-person appointment was made for comprehensive assessment including physical and cognitive function, and medications. An individualized care plan was created and revised during a multidisciplinary family conference. When indicated, self-monitored cognitive and physical home exercise instructions were given to the ICU survivors and their caregiver/support persons. Follow-up, in-person clinic visits were scheduled during which self-report data were collected. Physical, cognitive, and psychological symptoms were assessed using the Healthy Aging Brain Center Monitor [HABC-M ()] for both patients and caregivers. Patients showed significant improvement in two of three domains measured longitudinally; cognitive (p=0.04), functional (p=0.02), and overall (p=0.01). Behavioral measures improved but did not reach significance (p=0.65). Limitations included self-report data and lack of validation of the HABC-M in an ICU survivor population.
Jones et al. (34) provided nurse counseling as a single intervention for ICU survivors. The purpose of the counselling sessions was to provide assistance for ICU survivors and their families who needed to resolve psychological stress related to their ICU experiences. Former ICU nurses were trained in counselling and psychotherapy and implemented the intervention. No details were described about preparation for nurse counselors other than the former nurses had additional training in counselling. Furthermore, what took place in the counselling sessions was not discussed. Survivors were compared to community patients to evaluate the effectiveness of the service intervention using a pre-post two group comparison design. Data were collected using Psychological Outcomes Profiles and Clinical Outcomes and Routine Evaluation Outcome Measures to determine baseline and post-intervention evaluation. Baseline measures showed ICU survivors more likely to have moderate to severe symptoms of PTSD. Overall, the counseling intervention improved scores of all but two patients who remained in the moderate to severe category. The clinic adopted nurse counselors as part of their usual care with specialist referral for patients with severe symptoms and PTSD.
Discussion
ICU mortality has declined due to advances in critical care treatment resulting in an increased number of ICU survivors requiring follow-up care. (1) Existing literature about in-person, out-patient follow-up services for ICU survivors originates mainly from European countries with one Australian report (10) and two reports from the United States (4, 12). Various methods have been employed for evaluating ICU survivor rehabilitation and recovery including mailed or telephone-delivered questionnaires, interventions conducted during inpatient stays, and telephone-based follow-up to assess health status. (15) In some instances patients were assessed in the hospital and were referred to primary care clinics after discharge. Interventions provided through in-person clinical setting were diverse and we found little evidence of their efficacy with the exception of prospective diaries. Even with minimal evidence, some clinics reported adopting such interventions into practice (33). Also, healthcare utilization was not assessed, measured, or reported as an outcome of clinic interventions. Research focused on interventions to prevent unnecessary use of emergency services and re-hospitalization is needed. While ICU follow-up clinics have had limited yet ongoing global presence, reports of their usefulness and effectiveness as treatment centers is scarce making it difficult to justify their existence as something other than just another primary care office. (51) However, although not unique to this population, ICU survivors have a characteristic group of symptoms which need to be recognized and treated by teams that have expertise in ICU follow-up care. Nurses and physicians who have tested interventions with rigorous trials for feasibility and effectiveness could find ICU survivor clinics to be exceptional settings for implementation, scaling, optimization, and cost effectiveness studies.
Referral services for either physical therapy or neuropsychological counselling were incorporated in nearly all publications. Generally speaking, referrals are not true interventions and should not be included or reported as part of a tested intervention. Additionally, for this review of in-person ICU follow-up clinics, referral of patients for specialty services did not set apart the ICU follow-up clinics from other medical services such as primary care clinics, medical homes, or general family physician practices incorporating referrals for specialty care as part of usual care. Traditional clinic-type settings typically focus on pathology which, when delivered as a sole intervention, limits patient-initiated discussions about their ICU experiences. (26)
Patient initiated discussions are valuable to the well-being of patients and caregiver/support persons who prefer interactions with providers who are familiar with contextual details and specifics of ICU treatments. (41) Patients can offer perspective about variances in their experiences of symptoms which is a necessary consideration when providing post-ICU follow-up treatment. There are three recognized domains of post-ICU symptoms: Cognitive, functional, and psychological (anxiety, post-traumatic stress, and depression) and not all survivors experience all symptoms. The results of the studies included in this review could have been impacted by symptom experience variation thus adding to the importance of further research in this area. ICU survivor follow-up clinics provide a venue for the provision of targeted and tailored physical and mental health interventions for post-intensive care symptoms.
Our findings are consistent with Jensen et al. (52) who also demonstrate that, when searching for interventions provided in ICU follow-up clinics, few interventions are detailed in current literature. Also, no clear evidence exists to support the few interventions that are currently used to assist ICU survivors in their quest for maximum post-hospital recovery. The small number of interventions and the inadequate appraisal of the currently provided interventions must be evaluated for effectiveness prior to adoption in practice. New, innovative ideas for treatments targeted at all phases of the ICU patient experience of ICU follow-up clinics are needed.
Additional evidence for outcomes of interventions such as the ABCDEF bundle (Assess, prevent and manage pain; Both spontaneous awakening trials and spontaneous breathing trials; Choice of analgesia and sedation; Delirium, assess, prevent and manage; Early mobility and exercise; Family engagement and empowerment) (53) that are implemented in the ICU and focused on prevention of PICS symptoms related to the ICU stay could be developed and tested. Identification and treatment of symptoms that are experienced after ICU discharge in acute care units is an unexplored area in need of research. Interventions during the phase of care after hospital discharge (in ICU follow-up clinics and at home) needs development as well as primary research regarding interventions that are currently being implemented without adequate evidence. The need for evidence-based ICU survivor interventions during all phases of care is striking and invokes a sense of urgency.
Strengths and Limitations
We found no other published, comprehensive reviews of in-person ICU follow-up clinics. A strength of our review was that our literature search was conducted by an experienced University librarian and guided by authors who are experienced ICU practitioners. Additionally, we included studies that would otherwise be excluded using a systematic review approach.
Limitations for scoping reviews include the possibility of incomplete retrieval of relevant studies. Search terms change over time and ICU survivors and follow-up clinics may have been known by other descriptors thereby escaping inclusion in our search results.
A second limitation of scoping reviews is that using an assessment tool for study quality is not necessary which results in varying levels of quality of the studies that we included in this review. (17) Some research reports had missing or incomplete accounts of interventions which impedes a full synthesis of study findings. (17) These quality limitations raised questions about the use of scoping review results in policy and practice. (17) We used a scoping review approach to identify gaps and to bring forward the need for research in the area of ICU survivor follow-up care interventions. Accordingly, we found a lack of consideration for patient preferences regarding follow-up treatment. The interventions that were tested were generated and initiated by healthcare providers without mention of consultation with patients and families which must be considered when implementing and interpreting intervention outcomes.
Conclusion
Though ICU follow-up clinics have existed for decades, few reports have been published of interventions and the effectiveness of interventions used in these clinics. Published studies are widely diverse in method and focus and lack strong evidence for interventions that are currently employed by ICU survivor follow-up clinics. Rigorous research is needed to establish standardized care for the growing population of ICU survivors.
Acknowledgments
Dr. Khan’s work on the project was supported through a Career Development Award from the National Institute on Aging (NIA K23-AG043476). No additional financial support was provided for this work.
Biographies
Sue Lasiter, PhD, RN, is an Assistant Professor of Nursing at Indiana University School of Nursing and has a practice background in intensive care nursing. Her research focuses on factors occurring in and outside of intensive care units (ICU) that impact the maximum recovery potential of ICU survivors.
Sylwia Oles, BS (Psychology), was a research assistant with Indiana University Center for Aging Research and has worked with ICU survivors in the Critical Care Recovery Center teaching them cognitive rehabilitation. Ms. Oles is currently a graduate student studying Industrial and Organizational Psychology at Eastern Kentucky University.
James Mundell, BA (Psychology), has worked in healthcare research for the past two years at the Regenstrief Institute in Indianapolis, Indiana. He is currently a doctoral student studying Industrial and Organizational Psychology at the University of Missouri, St. Louis, MO.
Sue London, MLS, is an Associate Professor and has been a research librarian at the Indiana University School of Medicine’s Ruth Lilly Medical Library in Indianapolis, Indiana for twenty years. She has expertise in evidence-base literature searching and knowledge management.
Babar Khan, MS, MD, is an Assistant Professor of Medicine, Indiana University School of Medicine, director of the Critical Care Recovery Center, and a researcher at Indiana University center for Aging Research. His research encompasses ICU delirium and long term complications for ICU survivors arising from their ICU stay.
Footnotes
All authors had substantial contributions to the conception, acquisition, analysis, and interpretation of data. All authors were actively involved in writing important intellectual content and revising it critically for final approval of the version to be published. Authors are in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work could be appropriately investigated and resolved.
Contributor Information
Sue Lasiter, 2702 Sandstone Way, Apt. 355, Plainfield, IN 46168, lasiters@iu.edu, Assistant Professor, Indiana University School of Nursing, NUR 433W, Office Phone: 317-274-7912, Cell: 816-726-1179.
Sylwia K. Oles, skoles@umail.iu.edu, Cell: (317) 640-9199.
James Mundell, jtmmt9@mail.umsl.edu, Cell: 317-373-5125.
Susan London, Ruth Lilly Medical Library, IB 319, Indianapolis, IN 46202, slondon@iu.edu, Associate Librarian, Indiana University Libraries, Office: 317-274-2281.
Babar Khan, 1481 West 10th Street, Suite 111-P IU, Indianapolis, IN, bakhan@iu.edu, Assistant Professor, Indiana University School of Medicine, Office: 317-274-9132.
References
- 1.Committee on the Future Health Care Workforce for Older Americans, Institute of Medicine. Retooling for an Aging America: Building the Health Care Workforce. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- 2.Institute of Medicine (US) Crossing the quality chasm: A new health system for the 21st century. National Academies Press; 2001. Committee on Quality of Health Care in America. [PubMed] [Google Scholar]
- 3.Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, and Society for Academic Emergency Medicine. J. Hosp. Med. 2009;4:364–370. doi: 10.1002/jhm.510. [DOI] [PubMed] [Google Scholar]
- 4.Modrykamien AM. The ICU follow-up clinic: A new paradigm for intensivists. Respiratory Care. 2012;57(4):764–772. doi: 10.4187/respcare.01461. [DOI] [PubMed] [Google Scholar]
- 5.Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012;40(2):502–509. doi: 10.1097/CCM.0b013e318232da75. (2012) [DOI] [PubMed] [Google Scholar]
- 6.Van der Schaaf M, Dettling DS, Beelen A, Lucas C, Dongelmans DA, Nollet F. Poor functional status immediately after discharge from an intensive care unit. Disabil Rehabil. 2008;30(23):1812–1818. doi: 10.1080/09638280701673559. [DOI] [PubMed] [Google Scholar]
- 7.Hopkins RO, Jackson JC. Long term neurocognitive function after critical illness. Chest. 2006;130(3):869–878. doi: 10.1378/chest.130.3.869. [DOI] [PubMed] [Google Scholar]
- 8.Davydow DS, Gifford JM, Desai SV, Needham DM, Bienvenu OJ. Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen Hosp Psychiatry. 2008;30(5):421–434. doi: 10.1016/j.genhosppsych.2008.05.006. (2008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davydow DS, Gifford JM, Desai SV, Bienvenu OJ, Needham DM. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med. 2009;35(5):796–809. doi: 10.1007/s00134-009-1396-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Griffiths JA, Barber VS, Cuthbertson BH, Young JD. A national survey of intensive care follow-up clinics. Anaesthesia. 2006;61(10):950–955. doi: 10.1111/j.1365-2044.2006.04792.x. [DOI] [PubMed] [Google Scholar]
- 11.Williams TA, Leslie GD. Beyond the walls: A review of ICU clinics and their impact on patient oucomes afer leaving hospital. Australian Critical Care. 2008;21(1):6–17. doi: 10.1016/j.aucc.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Authors [Google Scholar]
- 13.Wood W. Wall Street Journal covers VUMC’s post-ICU delirium research. [Accessed March 21, 2015]; https://my.vanderbilt.edu/getthenac/2013/11/wall-street-journal-covers-vumcs-post-icu-delirium-research/ [Google Scholar]
- 14.Burling S. A new frontier in ICU research: Post-intensive care syndrome. [Accessed March 21, 2015]; http://articles.philly.com/2013-03-27/news/38043544_1_icu-patients-delirium-critical-care. [Google Scholar]
- 15.Melhorn J, Freytag A, Schmidt K, et al. Rehabilitation interventions for postintensive care syndrome: A systematic review. Crit Care Med. 2014;42(5):1263–1271. doi: 10.1097/CCM.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 16.Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, Theory and Practice. 2005;8:19–32. [Google Scholar]
- 17.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implementation science. 2010;5:69. doi: 10.1186/1748-5908-5-69. Available at http://www.implementationscience.com/content/5/1/69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: A large, interprofessional team’s experience with Arksey and O’Malley’s framework. BMC Medical Research Methodology. 2013;13(48):1–9. doi: 10.1186/1471-2288-13-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adhikari NKJ, McAndrews MP, Tansey CM, et al. Self-reported symptoms of depression and memory dysfunction in survivors of ARDS. Chest. 2009;35(3):678–687. doi: 10.1378/chest.08-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bashour CA, Yared JP, Ryan TA, et al. Long-term survival and functional capacity in cardiac surgery patients after prolonged intensive care. Crit Care Med. 2000;28(12):3847–3853. doi: 10.1097/00003246-200012000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Boumendil A, Maury E, Reinhard I, Luquel L, Offenstadt G, Guidet B. Prognosis of patients aged 80 years and over admitted in medical intensive care unit. Intensive Care Med. 2004;30:647–654. doi: 10.1007/s00134-003-2150-z. [DOI] [PubMed] [Google Scholar]
- 22.Combe D. The use of patient diaries in an intensive care unit. Nurs Crit Care. 2005;10(1):31–34. doi: 10.1111/j.1362-1017.2005.00093.x. [DOI] [PubMed] [Google Scholar]
- 23.Cuthbertson BH, Rattray J, Gager M, et al. The PRaCTICaL study of nurse led, intensive care follow-up programmes for improving long term outcomes from critical illness: a pragmatic randomised controlled trial. BMJ. 2009;339:b3723. doi: 10.1136/bmj.b3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Miranda S, Pochard F, Chaize M, et al. Postintensive care unit psychological burden in patients with chronic obstructive pulmonary disease and informal caregivers: a multicenter study. Crit Care Med. 2011;39(1):112–118. doi: 10.1097/CCM.0b013e3181feb824. [DOI] [PubMed] [Google Scholar]
- 25.Eddleston JM, White P, Guthrie E. Survival, morbidity, and quality of life after discharge from intensive care. Crit Care Med. 2000;28(7):2293–2299. doi: 10.1097/00003246-200007000-00018. [DOI] [PubMed] [Google Scholar]
- 26.Engström A, Andersson S, Söderberg S. Re-visiting their ICU experiences of follow-up visits to an ICU after discharge: A qualitative study. Intensive Crit Care Nurs. 2008;24:233–241. doi: 10.1016/j.iccn.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Flaatten H. Follow-up after intensive care: another role for the intensivist? Acta Anaesthesiol Scand. 2005;49:919–921. doi: 10.1111/j.1399-6576.2005.00775.x. [DOI] [PubMed] [Google Scholar]
- 28.Fletcher SN, Kennedy DD, Ghosh IR, et al. Persistent neuromuscular and neurophysiologic abnormalities in long-term survivors of prolonged critical illness. Crit Care Med. 2003;31(4):1012–1016. doi: 10.1097/01.CCM.0000053651.38421.D9. [DOI] [PubMed] [Google Scholar]
- 29.Granja C, Morujão E, Costa-Pereira A. Quality of life in acute respiratory distress syndrome survivors may be no worst than in other ICU survivors. Intensive Care Med. 2003;29:1744–1750. doi: 10.1007/s00134-003-1808-x. [DOI] [PubMed] [Google Scholar]
- 30.Griffiths J, Gager M, Alder N, Fawcett D, Waldmann C, Quinlan J. A self-report-based study of the incidence and associations of sexual dysfunction in survivors of intensive care treatment. Intensive Care Med. 2006;32:445–451. doi: 10.1007/s00134-005-0048-7. [DOI] [PubMed] [Google Scholar]
- 31.Hall-Smith J, Ball C, Coakley J. Follow-up services and the development of a clinical nurse specialist in intensive care. Intensive Crit Care Nurs. 1997;13:243–248. doi: 10.1016/s0964-3397(97)80374-6. [DOI] [PubMed] [Google Scholar]
- 32.Jones C, Backman C, Capuzzo M, et al. Intensive care diaries reduce new onset post traumatic stress disorder following critical illness: a randomised, controlled trial. Critical Care. 2010;14:R168. doi: 10.1186/cc9260. http://ccforum.com/content/14/5/R168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jones C, Griffiths RD, Skirrow P, Humphris G. Smoking cessation through comprehensive critical care. Intensive Care Med. 2001;27:1547–1549. doi: 10.1007/s001340101051. [DOI] [PubMed] [Google Scholar]
- 34.Jones C, Hall S, Jackson S. Benchmarking a nurse-led ICU counseling initiative. Nurs Times. 2008;104(38):32–34. [PubMed] [Google Scholar]
- 35.Jones C, Skirrow P, Griffiths RD, et al. Rehabilitation after critical illness: A randomized, controlled trial. Crit Care Med. 2003;31(10):2456–2461. doi: 10.1097/01.CCM.0000089938.56725.33. [DOI] [PubMed] [Google Scholar]
- 36.Knowles RE, Tarrier N. Evaluation of the effect of prospective patient diaries on emotional well-being in intensive care unit survivors: A randomized controlled trial. Crit Care Med. 2009;37(1):184–191. doi: 10.1097/CCM.0b013e31819287f7. [DOI] [PubMed] [Google Scholar]
- 37.Kvåle R, Ulvik A, Flaatten H. Follow-up after intensive care: A single center study. Intensive Care Med. 2003;29:2149–2156. doi: 10.1007/s00134-003-2034-2. [DOI] [PubMed] [Google Scholar]
- 38.Mundt DJ, Gage RW, Lemeshow S, Pastides H, Teres D, Avrunin JS. Mortality, functional status, and return to work at six months. Arch Intern Med. 1989;149:68–72. doi: 10.1001/archinte.149.1.68. [DOI] [PubMed] [Google Scholar]
- 39.Peskett M, Gibb P. Developing and setting up a patient and relatives intensive care. Nurs Crit Care. 2009;14(1):4–10. doi: 10.1111/j.1478-5153.2008.00302.x. [DOI] [PubMed] [Google Scholar]
- 40.Petersson CG, Bergbom I, Brodersen K, Ringdal M. Patients' participation in and evaluation of a follow-up program following intensive care. Acta Anaesthesiol Scand. 2011;55:827–834. doi: 10.1111/j.1399-6576.2011.02474.x. [DOI] [PubMed] [Google Scholar]
- 41.Prinjha S, Field K, Rowan K. What patients think about ICU follow-up services: a qualitative study. Critical Care. 2009;13(2):R46. doi: 10.1186/cc7769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Samuelson KAM, Lundberg D, Fridlund B. Stressful memories and psychological distress in adult mechanically ventilated intensive care patients – a 2-month follow-up study. Acta Anaesthesiol Scand. 2007;51:671–678. doi: 10.1111/j.1399-6576.2007.01292.x. [DOI] [PubMed] [Google Scholar]
- 43.Samuelson KAM, Corrigan I. A nurse-led intensive care after-care programme – development, experiences and preliminary evaluation. Nurs Crit Care. 2009;14(5):254–263. doi: 10.1111/j.1478-5153.2009.00336.x. [DOI] [PubMed] [Google Scholar]
- 44.Schandl AR, Brattström OR, Svensson-Raskh A, Hellgren EM, Falkenhav MD, Sackey PV. Screening and treatment of problems after intensive care: A descriptive study of multidisciplinary follow-up. Intensive Crit Care Nurs. 2007;27:94–101. doi: 10.1016/j.iccn.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 45.Strahan E, McCormick J, Uprichard E, Nixon S, Lavery G. Immediate follow-up after ICU discharge: establishment of a service and initial experiences. Nurs Crit Care. 2003;8(2):49–55. doi: 10.1046/j.1478-5153.2003.00007.x. [DOI] [PubMed] [Google Scholar]
- 46.Sukantarat K, Greer S, Brett S, Williamson R. Physical and psychological sequelae of critical illness. Br J Health Psychol. 2007;12:65–74. doi: 10.1348/135910706X94096. [DOI] [PubMed] [Google Scholar]
- 47.Waldmann CS. Intensive after care after intensive care. Currt Anesth Crit Care. 1998;9:134–139. [Google Scholar]
- 48.Zetterlund P, Plos K, Bergbom I, Ringdal M. Memories from intensive care unit persist for several years–a longitudinal prospective multi-centre study. Intensive Crit Care Nurs. 2012;28:159–167. doi: 10.1016/j.iccn.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 49.Gartlehner G, Hansen RA, Nissman D, Lohr KN, Carey TS. Technical Review 12 (Prepared by the RTI-International–University of North Carolina Evidence-based Practice Center under Contract No. 290-02-0016.) AHRQ Publication No. 06-0046. Rockville, MD: Agency for Healthcare Research and Quality; 2006. Apr, Criteria for distinguishing effectiveness from efficacy trials in systematic reviews. [PubMed] [Google Scholar]
- 50.Compher C. Efficacy vs effectiveness. J of Parenteral and Enteral Nutrition. 2010;34(6):598–599. doi: 10.1177/0148607110381906. [DOI] [PubMed] [Google Scholar]
- 51.Connolly B, Douiri A, Steier J, Moxham J, Denehy L, Hart N. A UK survey of rehabilitation following critical illness: Implementation of NICE Clinical Guidance 83 (GCG83) following hospital discharge. BMJ open. 2014;4:e004963. doi: 10.1136/bmjopen-2014-004963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jensen JF, Thomsen T, Overgaard D, Bestle MH, Christensen D, Egerod I. Impact of follow-up consultation for IUC survivior on post-ICU syndrome: A systematic review and meta-analysis. Intensive Care Med. 2015;41:763–775. doi: 10.1007/s00134-015-3689-1. [DOI] [PubMed] [Google Scholar]
- 53.Balas MC, Vasilevskis EE, Burke WJ, et al. Critical Care Nurses’ Role in Implementing the “ABCDE Bundle” Into Practice. Crit Care Nurse. 2012;32(2):35–47. doi: 10.4037/ccn2012229. [DOI] [PMC free article] [PubMed] [Google Scholar]


