Abstract
Aim:
Diabetes is an emerging health problem, both in developing and developed countries and has an enormous economic and social impact. The objective of our study was to find the impact of insulin pump on the quality of life of patients with type 2 diabetes (T2D) and compare it to the quality of life of patients with T2D using an insulin pen.
Subjects and Methods:
This is a case–control study which was conducted among patients with T2D presenting between November 2014 and November 2015. A total of 83 patients with T2D, using insulin pump were enrolled in the study as cases and 322 patients with T2D not using insulin pump but using insulin pens were enrolled as controls. Short form-36 quality of life questionnaire was used for data collection.
Results:
Mean age of patients using insulin pump was 52.49 ± 9.28 while the mean age of patients not using insulin pump was 54.72 ± 16.87. Mean score of all domains in the questionnaire was found to be higher in patients using insulin pump as compared to patients not using insulin pumps (P < 0.05). In 81.1% of the patients, the insulin pump decreased the frequency of hypoglycemic episodes.
Conclusion:
Insulin pump has significantly improved the quality of life of patients in terms of better self-esteem, decreased stress, and better mood. It has resulted in improved physical health, meal time flexibility, and ease of travel. It allows patient to have more active participation in social and recreational activities improving their personal and family life.
Keywords: Insulin, quality of life, patients with type 2 diabetes
INTRODUCTION
Diabetes is an emerging health problem both in developing and developed countries with an enormous economic and social impact.[1] It has a high age-adjusted prevalence of 9.6% in the North American and Caribbean region.[2] According to the World Health Organization, 347 million people had diabetes as of October 2013.[3,4] It is projected to be the 7th leading cause of death by 2030.[4] Good glycemic control remains an important goal for management of patients with type 2 diabetes (T2D). It significantly reduces the risk of serious long-term complications associated with T2D. One percent reduction in hemoglobin A1c (HbA1c) reduces diabetes-related deaths by 21% while the risk of microvascular complication and myocardial infarction are reduced by 37% and 14%, respectively.[5] Hypoglycemia is one of the major limitations in achieving a good control of T2D. Prevalence of hypoglycemia in T2D has escalated over the past decade with the increasing use of insulin for the treatment of patients with T2D. Hypoglycemia can cause serious morbidity by provoking stroke, acute cardiac failure, myocardial infarction, and ventricular arrhythmia.[6] In such cases, we should keep in mind the importance of quality of life issues as they have a significant impact on an individual's attitude toward managing his or her disease and long-term health. Despite various efforts, good glycemic control remains an elusive goal for most of the patients with T2D. The objective of our study was to find the impact of insulin pump on the quality of life of patients with T2D and compare it to the quality of life of patients with T2D using an insulin pen.
SUBJECTS AND METHODS
Study design, sampling technique, and sample size
This is a case–control study which was conducted among patients T2D using the insulin pump continuously for more than 6 months in a private clinic in New Jersey, the United States of America between November 2014 and November 2015. A total of 83 diagnosed patients with T2D on an insulin pump were included in the study as cases and 322 patients with T2D, not on an insulin pump but using insulin were included as controls. The patient was diagnosed of having T2D if they had HbA1c ≥ 6.5% or fasting plasma glucose ≥ 7.0 mmol/L or having classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥ 11.1 mmol/L.[7] Microvascular complications of diabetes were defined as long-term complications of diabetes because of its effects on small blood vessels resulting in retinopathy, nephropathy, and neuropathy. Macrovascular complications of diabetes included coronary artery disease, stroke, and peripheral vascular disease. The power of the sample size was set at 80% to differentiate quality of life variables between the two groups. Short form-36 (SF-36) quality of life questionnaire was used for data collection.[8] Patients using insulin pump were asked additional questions regarding impact of insulin pump on family relationship, social activities, ease of travel, recreational activities, energy level, the it mood, employment opportunities, intimate relationships, physician-patient relationship, sleep, motivation to achieve a better glycemic control, ease of accomplishing small tasks, frequency of hypoglycemic episodes, and meal time flexibility. They were also asked to list advantages and disadvantages of an insulin pump.
Data collection methods
A total of 100 patients on Insulin pump were asked to fill the questionnaire SF-36 out of which; 83 filled the form. 350 patients with T2D not using insulin pump were asked to fill the questionnaire SF-36; out of which 322 filled the form. Patients using the insulin pump for more than 6 months were considered as cases in the study. Patient with T1D or with another significant pathology was not included in the study. Informed consent was obtained from every patient and they were assured that their identity would be kept anonymous. The questionnaires were filled over the phone, in the clinic or via E-mail correspondence.
Data analysis
After the forms had been filled, the data were analyzed using the SPSS version 21 (IBM). Frequency and percentages were calculated for all qualitative variables. Welch's test was performed to assess whether difference in scores between the two groups was significant (P < 0.05).
RESULTS
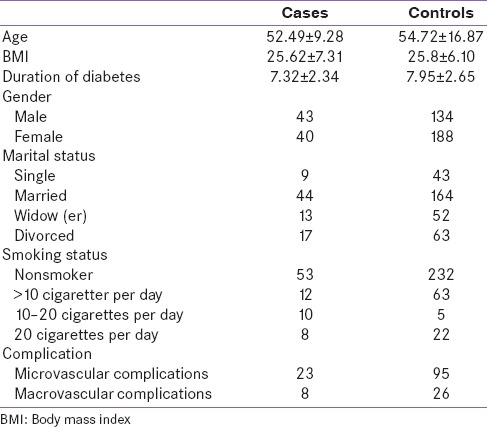
Of the total sample size of 405; 83 were patient with T2D on insulin pump while 322 were patients with T2D not on insulin pump but using insulin. About 177 (43.7%) were male patients while 228 (56.3%) were female patients. Mean age of patients using insulin Pump was 52.49 ± 9.28 while the mean age of patients not using insulin pump was 54.72 ± 16.87 [Table 1].
Table 1.
Characteristics of patients with type 2 diabetes
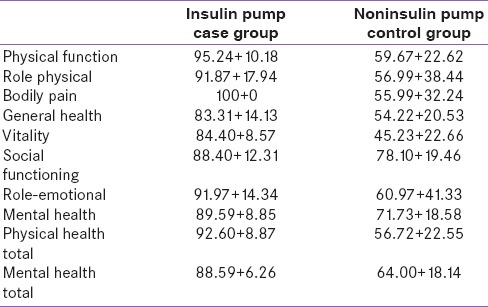
Welch's test was performed to assess whether difference in scores between the two groups was significant or not. Mean score of all domains was found to be higher in patients using insulin pump as compared to patients not using insulin pumps (P < 0.05) [Table 2].
Table 2.
Mean score of case group versus control group
About 100% of the patients found the insulin pump therapy better than their previous treatment with insulin pens or syringes. In 81.1% of the patients, the insulin pump decreased the frequency of hypoglycemic episodes; in 5.4% there was no change in the frequency of hypoglycemic episodes. The remaining 13.5% did not have hypoglycemic episodes before or after starting the insulin pump. 70.3% patients were extremely satisfied with the insulin pump therapy, 21.6% patients were very satisfied with the insulin pump, and 5.4% were satisfied with the insulin pump therapy. Only one patient was unsatisfied with the insulin pump therapy because of its small capacity. About 8.8% patients were troubled by the insulin pump's alarm.
DISCUSSION
Insulin has been the mainstay of treatment in patients with T2D after oral medications fail to control blood glucose level. Insulin was first used as a treatment for diabetes in 1922. Since then, insulin injections have been the golden standard of treatment for patients with T2D. However, injections have their limitations. Compliance is a significant issue with the use of insulin injections. Repeated punctures and calculating the right doses to be taken at specific times prove to be a huge nuisance to users of insulin injections. To counteract these problems, insulin pumps were first introduced in the 1970s in the management of diabetes. The introduction of the insulin pump was a great revolution in the management of diabetes. Dr. Arnold Kadish of Los Angeles devised the first portable insulin pump in 1963, and Dean Kamen designed the first wearable version in 1976. In the late 1970's, for the 1st time, insulin pumps were used in the management of patients with T2D.[9,10] Since then, great advancements in the insulin pump have been made.
In one of the largest randomized controlled trial was done on 1441 insulin-dependent diabetes mellitus patients, it was found that intensive care therapy was associated with reduced cardiovascular risk, neuropathy, and nephropathy and also caused favorable changes in lipid profiles.[11,12] A comparison study between multiple injection regimens and insulin pump showed that insulin pump provided a better control and was safe and convenient to use.[13] A systemic review of 74 studies concluded that the insulin pump provided better glycemic control and quality of life in both children and adults as compared to multiple daily injections of insulin.[14] Hence, it is no surprise that the percentage of patients with T2D using insulin pump has progressively increased with the passage of time. The obstacles in using pump therapy include the high cost, the high level of commitment with regular blood glucose monitoring, hardware problems, and pump failure. The risk of hypoglycemia and diabetic ketoacidosis still remains, though decreased on insulin pump therapy. All in all, there are disagreements about which is more beneficial for patients; injections or pumps.
The insulin pump is a relatively new modality in the treatment of patients with T2D. A number of studies have proven that insulin pump therapy has improved the glycemic control in patients with T1D and T2D.[15,16,17] Furthermore, with better glycemic control, the risk for the development of complications can be reduced.[18,19] According to a study, about 68.5%, 56.1%, and 31.4% of patients with poorly controlled T2D had neuropathy, nephropathy, and retinopathy, respectively.[18] Hence, an insulin pump is effective not only in the immediate management of T2D but also in preventing the long-term complications associated with T2D.[20]
The most important and common adverse effect of insulin therapy is hypoglycemia. It is the main limitation in the execution of intensive insulin therapy. In a study done in 2013, under diabetes control and complications trial, it was found that the rate of hypoglycemia increased by 300% upon escalating the glycemic control.[21] It has been proven by various studies that insulin pump significantly reduces the hypoglycemic episode and is a good alternative to the ineffective multiple drug injection (MDI).[22,23] A meta-analysis showed that insulin pump was superior in reducing hypoglycemic episodes as compared to MDI with an odds ratio of 0.48 for severe hypoglycemia.[24] According to a randomized parallel group study, patients with T2D using insulin pump has 0.8 episodes of hypoglycemia per month as compared to 1.2 episodes per month in patients with T2D using MDI.[25] In our study, there was a decrease in hypoglycemic episodes in 81.1% of the patients, in 5.4% there was no change in the frequency of hypoglycemic episodes while the remaining 13.5% did not experience hypoglycemic episodes before or after starting the insulin pump. According to a study, a patient who shifted from MDI to insulin pump showed a significant (P < 0.005) decrease in insulin requirement from 1.7 ± 0.9 to 1.1 ± 0.6 U/kg/day.[26] This might be the reason of decreased hypoglycemic episodes in patients using insulin pumps.
The insulin pump offers the patient ease of travel without having to worry about the availability of insulin in different places and whether a specific amount of insulin would last them during the journey or not. This fact was highlighted in our study, as 56.7% of the patients felt “much better,” 21.6% felt “better,” and 18.9% felt the “same as before starting insulin pumps” in their ease of travel. No patient felt worse with the insulin pump in this domain.
A big issue in diabetics is that they need to maintain a pretty stable meal schedule so as to be able to calculate the right dose of the insulin. Insulin pump, however, offers flexibility in meal eating times and also broadens food choice.[27,28] A case–control study showed that people on MDI had greater diet limitations than those on insulin pumps.[29] Patients using injectable insulin have to follow strict schedules for their meal times and the need for administration of injections prior to meals is cumbersome. This indirectly limits their social activity. In fact, it was revealed upon an interview with many of our patients that they were taken as drug addicts by the onlookers in public gatherings while they were administering their premeal dose of insulin. They had anxiety and fear of glycemic excursions after meals and hence abstained from participating in social activities. A systematic literature search showed that insulin pump provided a greater flexibility in lifestyle with regard to meals and socialization.[30] Our research showed that in terms of mealtime flexibility; 67.6% patients felt “much better” after starting the insulin pump, 16.21% patient felt “better” after starting the insulin pump, and 13.5% patient felt same as they did on the previous therapy. Around 72.9% patients felt “much better” and 16.2% “better” in term of social/leisure activity after starting the insulin pump while the remainder felt same as before.
Different questionnaires have been developed to assess the quality of life of patients with T2D. A randomized controlled, cross-over trial conducted in 11 European centers showed that diabetes quality of life questionnaire scores for people using insulin pumps are higher than those on other types of therapies.[31] A number of other studies deduced similar results in terms of better sense of well-being, lesser anxiety due to fear of glycemic excursions, and fewer episodes of ketoacidosis.[29] With better quality of life, people have better self-esteem, and better physical health. In our study, mean physical health score of patients using insulin pump was 92.42 as compared to 56.72 in patients in the control groups. Results of the control group were similar to a study done on patients with T2D not using insulin pump. Patients in that study had a mean physical function score of 41.46.[8] About 59% of patients on insulin pump felt “much better,” 21% “better” and 16% felt “same” as before, in addition, 89% people feel “more independent” and “less strained.” There was also improvement in family relations; 37% people reported them to be “much better,” 16.2% “better,” and 40.5% “same” as before.
Many studies have shown that people on insulin pump are more satisfied with their treatment as compared with other therapies.[32] Our research showed that 97% people found the insulin pump to be “more convenient,” with “less pricking,” and reported a “better diabetic control.” With better satisfaction with therapy, patients develop more trust in their doctor, and it improves the doctor-patient relationship. This improvement in physician-patient relationship was seen in our study as 51.35% reported that it got “much better,” 8% reported it got “better,” and 32% reported that it remained “same.” According to a study, 93% of the patient preferred insulin pump over their previous MDI regimen because of increased flexibility, ease of use, convenience, and overall improvement in quality of life.[32]
Patient with diabetes suffer from depression and anxiety.[33] A cross-sectional study done on patients admitted to Cardiac Intensive Care Units showed a strong association between impaired glucose levels and depression.[34] It was found in a case–control study, that the prevalence of depression and anxiety is higher among patients with diabetes as compared to controls.[35] Mean total mental health score was found to be 88.59 in patients on insulin pump as compared to 64.00 in patients in the control group. Other studies done on patient with T2D, not on insulin pump had a mean mental score of 46.63,[8]60.1,[36] and 55.4.[37] In our research, it was found that in terms of mood and feeling happy, 75% people felt “much better,” 11% felt “better,” and 13% felt the “same” as before. In terms of self-esteem and stress; 54% of patients had reported “much better,” 16% “better,” and 29% “same” as before.
Many disadvantages of insulin pump have been raised over the past. One issue is the cost-effectiveness. Different studies have shown that although insulin pump is not economical initially, it becomes more cost-effective in the long run by preventing diabetic complications and thus reducing the hospitalization associated costs.[38,39] Another problem encountered is the weight gain associated with insulin pump. In our research, 91.8% of patients reported no increase in weight. This could be due to the more appropriate insulin dosing done in our study. No significant difference in weight change was found in other studies comparing insulin pump with MDI in patients with T2D.[32,40,41]
Other problems which could be encountered are the alarms associated in an insulin pump. It was found in a retrospective study done on adolescents that one of the chief problems was the alarm.[40] In our study, 8.8% of patients were troubled by them.
CONCLUSION
The insulin pump has significantly improved the quality of life of in terms of better self-esteem, decreased stress, better mood, improved physical health, meal time flexibility, ease of travel, more active participation in social and recreational activities, ease of accomplishing small tasks and family relationships. The satisfaction of patients on treatment with insulin pump shows that it is a simple and convenient way of insulin therapy, providing better diabetic control, with minimal hypoglycemic episodes and weight gain. It is, thus, a new ray of hope to diabetic patients all over the world.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kaul K, Tarr JM, Ahmad SI, Kohner EM, Chibber R. Introduction to diabetes mellitus. Adv Exp Med Biol. 2012;771:1–11. doi: 10.1007/978-1-4614-5441-0_1. [DOI] [PubMed] [Google Scholar]
- 2.Yisahak SF, Beagley J, Hambleton IR, Narayan KM. IDF Diabetes Atlas. Diabetes in North America and the Caribbean: An update. Diabetes Res Clin Pract. 2014;103:223–30. doi: 10.1016/j.diabres.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 4.WHO Diabetes Fact Sheet No. 312. Reviewed October, 2013. [Last accessed on 2015 Dec 28]. Available from: http://www.who.int/mediacentre/factsheets/fs312/en/
- 5.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ. 2000;321:405–12. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zammitt NN, Frier BM. Hypoglycemia in type 2 diabetes: Pathophysiology, frequency, and effects of different treatment modalities. Diabetes Care. 2005;28:2948–61. doi: 10.2337/diacare.28.12.2948. [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association. (2) Classification and diagnosis of diabetes. Diabetes Care. 2015;38(Suppl):S8–16. doi: 10.2337/dc15-S005. [DOI] [PubMed] [Google Scholar]
- 8.Kazemi-Galougahi MH, Ghaziani HN, Ardebili HE, Mahmoudi M. Quality of life in type 2 diabetic patients and related effective factors. Indian J Med Sci. 2012;66:230–7. [PubMed] [Google Scholar]
- 9.Tamborlane WV, Sherwin RS, Genel M, Felig P. Reduction to normal of plasma glucose in juvenile diabetes by subcutaneous administration of insulin with a portable infusion pump. N Engl J Med. 1979;300:573–8. doi: 10.1056/NEJM197903153001101. [DOI] [PubMed] [Google Scholar]
- 10.Pickup JC, Keen H, Parsons JA, Alberti KG. Continuous subcutaneous insulin infusion: An approach to achieving normoglycaemia. Br Med J. 1978;1:204–7. doi: 10.1136/bmj.1.6107.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group. Intensive Diabetes Treatment and Cardiovascular Outcomes in Type 1 Diabetes: The DCCT/EDIC Study 30-Year Follow-up. Diabetes Care. 2016:pii: dc151990. [Epub ahead of print] [Google Scholar]
- 12.Writing Group for the DCCT/EDIC Research Group. Orchard TJ, Nathan DM, Zinman B, Cleary P, Brillon D, et al. Association between 7 years of intensive treatment of type 1 diabetes and long-term mortality. JAMA. 2015;313:45–53. doi: 10.1001/jama.2014.16107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berthe E, Lireux B, Coffin C, Goulet-Salmon B, Houlbert D, Boutreux S, et al. Effectiveness of intensive insulin therapy by multiple daily injections and continuous subcutaneous infusion: A comparison study in type 2 diabetes with conventional insulin regimen failure. Horm Metab Res. 2007;39:224–9. doi: 10.1055/s-2007-970423. [DOI] [PubMed] [Google Scholar]
- 14.Cummins E, Royle P, Snaith A, Greene A, Robertson L, McIntyre L, et al. Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: Systematic review and economic evaluation. Health Technol Assess. 2010;14:iii. doi: 10.3310/hta14110. [DOI] [PubMed] [Google Scholar]
- 15.Monami M, Lamanna C, Marchionni N, Mannucci E. Continuous subcutaneous insulin infusion versus multiple daily insulin injections in type 1 diabetes: A meta-analysis. Acta Diabetol. 2010;47(Suppl 1):77–81. doi: 10.1007/s00592-009-0132-5. [DOI] [PubMed] [Google Scholar]
- 16.Pankowska E, Blazik M, Dziechciarz P, Szypowska A, Szajewska H. Continuous subcutaneous insulin infusion vs. Multiple daily injections in children with type 1 diabetes: A systematic review and meta-analysis of randomized control trials. Pediatr Diabetes. 2009;10:52–8. doi: 10.1111/j.1399-5448.2008.00440.x. [DOI] [PubMed] [Google Scholar]
- 17.Weissberg-Benchell J, Antisdel-Lomaglio J, Seshadri R. Insulin pump therapy: A meta-analysis. Diabetes Care. 2003;26:1079–87. doi: 10.2337/diacare.26.4.1079. [DOI] [PubMed] [Google Scholar]
- 18.Ali A, Iqbal F, Taj A, Iqbal Z, Amin MJ, Iqbal QZ. Prevalence of microvascular complications in newly diagnosed patients with type 2 diabetes. Pak J Med Sci. 2013;29:899–902. doi: 10.12669/pjms.294.3704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bash LD, Selvin E, Steffes M, Coresh J, Astor BC. Poor glycemic control in diabetes and the risk of incident chronic kidney disease even in the absence of albuminuria and retinopathy: Atherosclerosis risk in communities (ARIC) Study. Arch Intern Med. 2008;168:2440–7. doi: 10.1001/archinte.168.22.2440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lepore G, Bruttomesso D, Bonomo M, Dodesini AR, Costa S, Meneghini E, et al. Continuous subcutaneous insulin infusion is more effective than multiple daily insulin injections in preventing albumin excretion rate increase in Type 1 diabetic patients. Diabet Med. 2009;26:602–8. doi: 10.1111/j.1464-5491.2009.02736.x. [DOI] [PubMed] [Google Scholar]
- 21.Awoniyi O, Rehman R, Dagogo-Jack S. Hypoglycemia in patients with type 1 diabetes: Epidemiology, pathogenesis, and prevention. Curr Diab Rep. 2013;13:669–78. doi: 10.1007/s11892-013-0411-y. [DOI] [PubMed] [Google Scholar]
- 22.Didangelos T, Iliadis F. Insulin pump therapy in adults. Diabetes Res Clin Pract. 2011;93(Suppl 1):S109–13. doi: 10.1016/S0168-8227(11)70025-0. [DOI] [PubMed] [Google Scholar]
- 23.Pickup JC, Renard E. Long-acting insulin analogs versus insulin pump therapy for the treatment of type 1 and type 2 diabetes. Diabetes Care. 2008;31(Suppl 2):S140–5. doi: 10.2337/dc08-s235. [DOI] [PubMed] [Google Scholar]
- 24.Fatourechi MM, Kudva YC, Murad MH, Elamin MB, Tabini CC, Montori VM. Clinical review: Hypoglycemia with intensive insulin therapy: A systematic review and meta-analyses of randomized trials of continuous subcutaneous insulin infusion versus multiple daily injections. J Clin Endocrinol Metab. 2009;94:729–40. doi: 10.1210/jc.2008-1415. [DOI] [PubMed] [Google Scholar]
- 25.Raskin P, Bode BW, Marks JB, Hirsch IB, Weinstein RL, McGill JB, et al. Continuous subcutaneous insulin infusion and multiple daily injection therapy are equally effective in type 2 diabetes: A randomized, parallel-group, 24-week study. Diabetes Care. 2003;26:2598–603. doi: 10.2337/diacare.26.9.2598. [DOI] [PubMed] [Google Scholar]
- 26.Pouwels MJ, Tack CJ, Hermus AR, Lutterman JA. Treatment with intravenous insulin followed by continuous subcutaneous insulin infusion improves glycaemic control in severely resistant Type 2 diabetic patients. Diabet Med. 2003;20:76–9. doi: 10.1046/j.1464-5491.2003.00848.x. [DOI] [PubMed] [Google Scholar]
- 27.Peters JE, Mount E, Huggins CE, Rodda C, Silvers MA. Insulin pump therapy in children and adolescents: Changes in dietary habits, composition and quality of life. J Paediatr Child Health. 2013;49:E300–5. doi: 10.1111/jpc.12162. [DOI] [PubMed] [Google Scholar]
- 28.Aronson R, Reznik Y, Conget I, Castañeda JA, de Portu S, Runzis S, et al. Sustained efficacy of insulin pump therapy, compared with multiple daily injections, in type 2 diabetes: 12-month data from the OpT2mise randomized trial. Diabetes Obes Metab. 2016 doi: 10.1111/dom.12642. doi: 10.1111/dom.12642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.EQuality Study Group – Evaluation of QUALITY of Life and Costs in Diabetes Type. Nicolucci A, Maione A, Franciosi M, Amoretti R, Busetto E, et al. Quality of life and treatment satisfaction in adults with Type 1 diabetes: A comparison between continuous subcutaneous insulin infusion and multiple daily injections. Diabet Med. 2008;25:213–20. doi: 10.1111/j.1464-5491.2007.02346.x. [DOI] [PubMed] [Google Scholar]
- 30.Hirose M, Beverly EA, Weinger K. Quality of life and technology: impact on children and families with diabetes. Curr Diab Rep. 2012;12:711–20. doi: 10.1007/s11892-012-0313-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoogma RP, Hammond PJ, Gomis R, Kerr D, Bruttomesso D, Bouter KP, et al. Comparison of the effects of continuous subcutaneous insulin infusion (CSII) and NPH-based multiple daily insulin injections (MDI) on glycaemic control and quality of life: Results of the 5-nations trial. Diabet Med. 2006;23:141–7. doi: 10.1111/j.1464-5491.2005.01738.x. [DOI] [PubMed] [Google Scholar]
- 32.Reznik Y, Cohen O. Insulin pump for type 2 diabetes: Use and misuse of continuous subcutaneous insulin infusion in type 2 diabetes. Diabetes Care. 2013;36(Suppl 2):S219–25. doi: 10.2337/dcS13-2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaur G, Tee GH, Ariaratnam S, Krishnapillai AS, China K. Depression, anxiety and stress symptoms among diabetics in Malaysia: A cross sectional study in an urban primary care setting. BMC Fam Pract. 2013;14:69. doi: 10.1186/1471-2296-14-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Azimova K, Rude J, Mallawaarachchi I, Dwivedi A, Sarosiek J, Mukherjee D. Glucose levels and depression in Hispanic patients admitted to the cardiovascular intensive care unit: A cross-sectional study. Angiology. 2015;66:57–64. doi: 10.1177/0003319713513318. [DOI] [PubMed] [Google Scholar]
- 35.Bajaj S, Agarwal SK, Varma A, Singh VK. Association of depression and its relation with complications in newly diagnosed type 2 diabetes. Indian J Endocrinol Metab. 2012;16:759–63. doi: 10.4103/2230-8210.100670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Papadopoulos AA, Kontodimopoulos N, Frydas A, Ikonomakis E, Niakas D. Predictors of health-related quality of life in type II diabetic patients in Greece. BMC Public Health. 2007;7:186. doi: 10.1186/1471-2458-7-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Clouet F, Excler-Cavailher G, Christophe B, Masson F, Fasquel D. Type 2 diabetes and short form 36-items health survey. Diabetes Metab. 2001;27:711–7. [PubMed] [Google Scholar]
- 38.Health Quality Ontario. Continuous Subcutaneous Insulin Infusion (CSII) pumps for type 1 and type 2 adult diabetic populations: An evidence-based analysis. Ont Health Technol Assess Ser. 2009;9:1–58. [PMC free article] [PubMed] [Google Scholar]
- 39.Fendler W, Baranowska AI, Mianowska B, Szadkowska A, Mlynarski W. Three-year comparison of subcutaneous insulin pump treatment with multi-daily injections on HbA1c, its variability and hospital burden of children with type 1 diabetes. Acta Diabetol. 2012;49:363–70. doi: 10.1007/s00592-011-0332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Herman WH, Ilag LL, Johnson SL, Martin CL, Sinding J, Al Harthi A, et al. A clinical trial of continuous subcutaneous insulin infusion versus multiple daily injections in older adults with type 2 diabetes. Diabetes Care. 2005;28:1568–73. doi: 10.2337/diacare.28.7.1568. [DOI] [PubMed] [Google Scholar]
- 41.Low KG, Massa L, Lehman D, Olshan JS. Insulin pump use in young adolescents with type 1 diabetes: A descriptive study. Pediatr Diabetes. 2005;6:22–31. doi: 10.1111/j.1399-543X.2005.00089.x. [DOI] [PubMed] [Google Scholar]


