Abstract
Background
We sought to examine the efficacy and safety of chronic total occlusion (CTO) percutaneous coronary intervention (PCI) using the retrograde approach.
Methods and Results
We compared the outcomes of the retrograde vs. antegrade-only approach to CTO PCI among 1,301 procedures performed at 11 experienced US centers between 2012 and 2015. Mean age was 65.5±10 years and 84% of the patients were men with a high prevalence of diabetes mellitus (45%) and prior coronary artery bypass graft surgery (CABG, 34%). Overall technical and procedural success rates were 90% and 89%, respectively, and in-hospital major adverse cardiovascular events (MACE) occurred in 31 patients (2.4%). The retrograde approach was employed in 539 cases (41%), either as the initial strategy (46%) or after a failed antegrade attempt (54%). As compared with antegrade-only cases, retrograde cases were significantly more complex, both clinically (prior CABG prevalence: 48% vs. 24%, p<0.001) and angiographically (mean J-CTO score: 3.1±1.0 vs. 2.1±1.2, p<0.001) and had lower technical success (85% vs. 94%, p<0.001) and higher MACE (4.3% vs. 1.1%, p<0.001) rates. On multivariable analysis, the presence of suitable collaterals, no smoking, no prior CABG and left anterior descending artery target vessel were independently associated with technical success using the retrograde approach.
Conclusions
The retrograde approach is commonly used in contemporary CTO PCI, especially among more challenging lesions and patients. While associated with lower success and higher MACE rates in comparison to antegrade-only crossing, retrograde PCI remains critical for achieving overall high success rates.
Keywords: chronic total occlusion, retrograde approach, percutaneous coronary intervention, outcome, complication
The retrograde approach revolutionized chronic total occlusion (CTO) percutaneous coronary intervention (PCI) and has been one of the main drivers of the increasingly high procedural success rates achieved in many experienced centers. It was developed in Japan,1–5 with rapid subsequent worldwide adoption.6–14 However, the recent development of advanced antegrade crossing options, including antegrade guidewires and antegrade dissection/re-entry, may have affected the utilization and outcomes of the retrograde approach. We, therefore, examined a contemporary, multicenter CTO PCI registry to determine the current role and associated outcomes of the retrograde approach, as compared with cases performed using exclusively antegrade techniques.
Methods
Study population
We examined the clinical and angiographic records of patients who underwent CTO PCI between May 2012 and September 2015 by experienced, high volume operators at 11 CTO PCI centers in the United States: Appleton Cardiology, Appleton, Wisconsin; Columbia University, New York, New York; Henry Ford Hospital, Detroit, Michigan; Massachusetts General Hospital, Boston, Massachusetts; Medical Center of the Rockies, Loveland, Colorado; Piedmont Heart Institute, Atlanta Georgia; PeaceHealth St. Joseph Medical Center, Bellingham Washington; St. Luke's Health System's Mid-America Heart Institute, Kansas City, Missouri; Torrance Memorial Center, Torrance, California; VA North Texas Health Care System, Dallas, Texas, and VA San Diego Healthcare System, San Diego, California. Data collection was performed prospectively and retrospectively and recorded in a CTO database (PROGRESS CTO, Clinicaltrials.gov Identifier: NCT02061436).15–20 Some centers only enrolled patients during part of the study period due to participation in other studies. The study was approved by the institutional review board of each site.
Definitions
Coronary CTOs were defined as coronary lesions with thrombolysis in myocardial infarction (TIMI) grade 0 flow of at least 3 months’ duration. Estimation of the occlusion duration was based on first onset of anginal symptoms, prior history of myocardial infarction in the target vessel territory, or comparison with a prior angiogram. Calcification was assessed by angiography as mild (spots), moderate (involving ≤50% of the reference lesion diameter) and severe (involving >50% of the reference lesion diameter). Moderate proximal vessel tortuosity was defined as the presence of at least 2 bends >70° or 1 bend >90° and severe tortuosity as 2 bends >90° or 1 bend >120° in the CTO vessel. Interventional collaterals were defined as collaterals deemed amenable to crossing by a guidewire and a microcatheter by the operator. A procedure was defined as “retrograde” if an attempt was made to cross the lesion through a collateral vessel supplying the target vessel distal to the lesion; if not, the procedure was classified as “antegrade-only”. A retrograde procedure was classified as “primary” if the retrograde approach was the first approach employed for the target lesion during the index procedure, and as “secondary” if the retrograde approach was used after failure to recanalize the vessel in an antegrade fashion. Technical success of CTO PCI was defined as successful CTO revascularization with achievement of <30% residual diameter stenosis within the treated segment and restoration of TIMI grade 3 antegrade flow. Procedural success was defined as achievement of technical success with no in-hospital major adverse cardiac events (MACE). In-hospital MACE included any of the following adverse events prior to hospital discharge: death, myocardial infarction (MI), recurrent symptoms requiring urgent repeat target vessel revascularization with PCI or coronary artery bypass graft surgery (CABG), tamponade requiring either pericardiocentesis or surgery, and stroke.
Statistical Analysis
Categorical variables were expressed as percentages and compared using Pearson’s chi-square test or Fisher’s exact test. Continuous variables were presented as mean ± standard deviation (normally distributed data) or median (interquartile range) (non-normally distributed data), and were compared using the t-test or Wilcoxon rank-sum test, as appropriate. Logistic regression analysis was performed to identify clinical and angiographic parameters associated with technical success for retrograde CTO PCI. Variables with p<0.10 on univariate analysis (presence of interventional collaterals, degree of proximal vessel tortuosity, target vessel for revascularization, occlusion length and smoking) were included in a multivariable model, along with variables shown by prior studies to be associated with PCI complexity (diabetes mellitus, prior PCI, prior CABG and prior MI). All statistical analyses were performed with JMP 12.0 (SAS Institute; Cary, NC). Two-sided p-values of 0.05 were considered statistically significant.
Results
Baseline clinical and angiographic characteristics
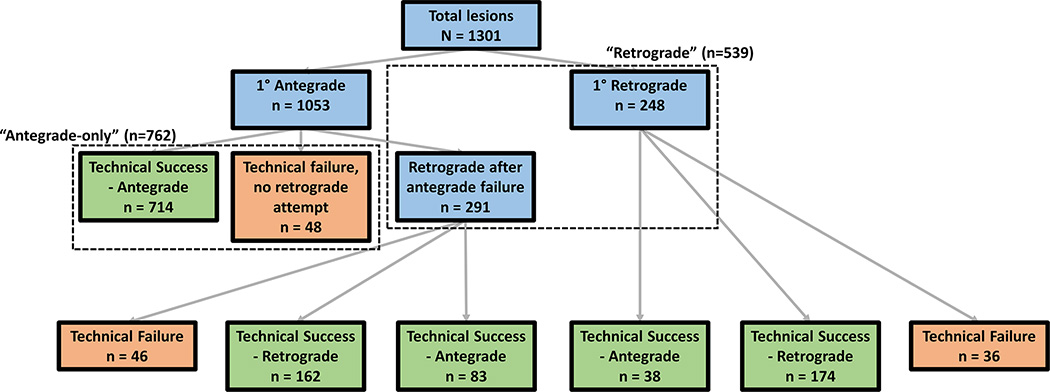
A total of 1,301 CTO PCIs performed in 1,276 patients were included in the present analysis. The retrograde approach was utilized in 539 CTO PCI procedures (41.4%, Figure 1). Mean age of the study patients was 65.5±10.2 years, and 84.1% were men (Table 1). There was a high prevalence of hypertension (89.6%), hyperlipidemia (94.3%) and diabetes mellitus (45.0%). Patients in whom the retrograde approach was used were significantly more likely to be men (87.5% vs. 81.7%, p=0.005), to have a history of heart failure (31.9% vs. 24.8%, p=0.006), prior PCI (70.4% vs. 60.8%, p<0.001), and prior CABG (47.7% vs. 24.1%, p<0.001).
Figure 1.
Flow-chart depicting the crossing strategies utilized for recanalization of the study lesions.
Table 1.
Baseline Clinical and Angiographic Characteristics of the Study Patients and Lesions, Classified According to Whether Retrograde Crossing was Attempted or Not
| Clinical Characteristics | Overall N=1276 |
Retrograde n=531 |
Antegrade-only n=745 |
p |
|---|---|---|---|---|
| Age (years)* | 65.5±10.2 | 66.1±10.1 | 65.1±10.3 | 0.096 |
| Men (%) | 84.1 | 87.5 | 81.7 | 0.005 |
| Hypertension (%) | 89.6 | 89.3 | 89.8 | 0.776 |
| Hyperlipidemia (%) | 94.3 | 94.5 | 94.2 | 0.824 |
| Diabetes mellitus (%) | 45.0 | 43.5 | 46.0 | 0.386 |
| Smoking (%) | 28.8 | 27.6 | 29.7 | 0.407 |
| Heart failure (%) | 27.8 | 31.9 | 24.8 | 0.006 |
| History of MI (%) | 41.6 | 44.6 | 39.6 | 0.077 |
| History of CABG (%) | 33.9 | 47.7 | 24.1 | <0.001 |
| History of stroke (%) | 10.9 | 11.4 | 10.5 | 0.587 |
| Prior PCI (%) | 64.8 | 70.4 | 60.8 | <0.001 |
| Prior CTO PCI failure (%) | 17.7 | 20.7 | 15.4 | 0.017 |
| Peripheral arterial disease (%) | 15.7 | 17.5 | 14.4 | 0.135 |
| Angiographic Characteristics | N=1301 | n=539 | n=762 | |
| CTO Target Vessel | ||||
| RCA (%) | 56.8 | 68.2 | 48.8 | |
| LCX (%) | 19.9 | 17.4 | 21.7 | <0.001 |
| LAD (%) | 23.3 | 14.5 | 29.5 | |
| CTO length (mm)* | 30 (20–45) | 38 (25–60) | 28 (16–38) | <0.001 |
| Interventional collaterals (%) | 60.2 | 78.3 | 45.8 | <0.001 |
| Moderate/severe calcification (%) |
58.2 | 69.8 | 49.2 | <0.001 |
| Moderate/severe tortuosity (%) | 35.4 | 41.3 | 30.8 | <0.001 |
| Side branch at proximal Cap (%) | 45.7 | 50.1 | 41.8 | 0.008 |
| Poor distal target vessel (%) | 39.0 | 51.8 | 28.6 | <0.001 |
| Distal cap at bifurcation (%) | 31.3 | 44.6 | 20.7 | <0.001 |
| Proximal cap ambiguity (%) | 31.6 | 47.4 | 18.6 | <0.001 |
| In-stent restenosis (%) | 13.9 | 13.5 | 14.2 | 0.723 |
| J-CTO score* | 2.5±1.2 | 3.1±1 | 2.1±1.2 | <0.001 |
CABG, Coronary artery bypass graft surgery; CTO, chronic total occlusion; LAD, left anterior descending artery; LCX, left circumflex artery; MI, myocardial infarction; PCI, percutaneous coronary intervention; RCA, right coronary artery.
mean±standard deviation or median (interquartile range).
As compared with antegrade-only cases, the retrograde approach was used more frequently for CTOs in the right coronary artery (68.2% vs. 48.8%, p<0.001), lesions with longer length (median length: 38 [25–60] mm vs. 28 [16–38] mm, p<0.001), moderate or severe calcification (69.8% vs. 49.2%, p<0.001), moderate or severe tortuosity (41.3% vs. 30.8%, p<0.001), and proximal cap ambiguity (47.4% vs. 18.6%, p<0.001). Lesions attempted with the retrograde approach were also more likely to have interventional collaterals (78.3% vs. 45.8%, p<0.001) and a higher J-CTO score (3.1±1 vs. 2.1±1.2, p<0.001).21
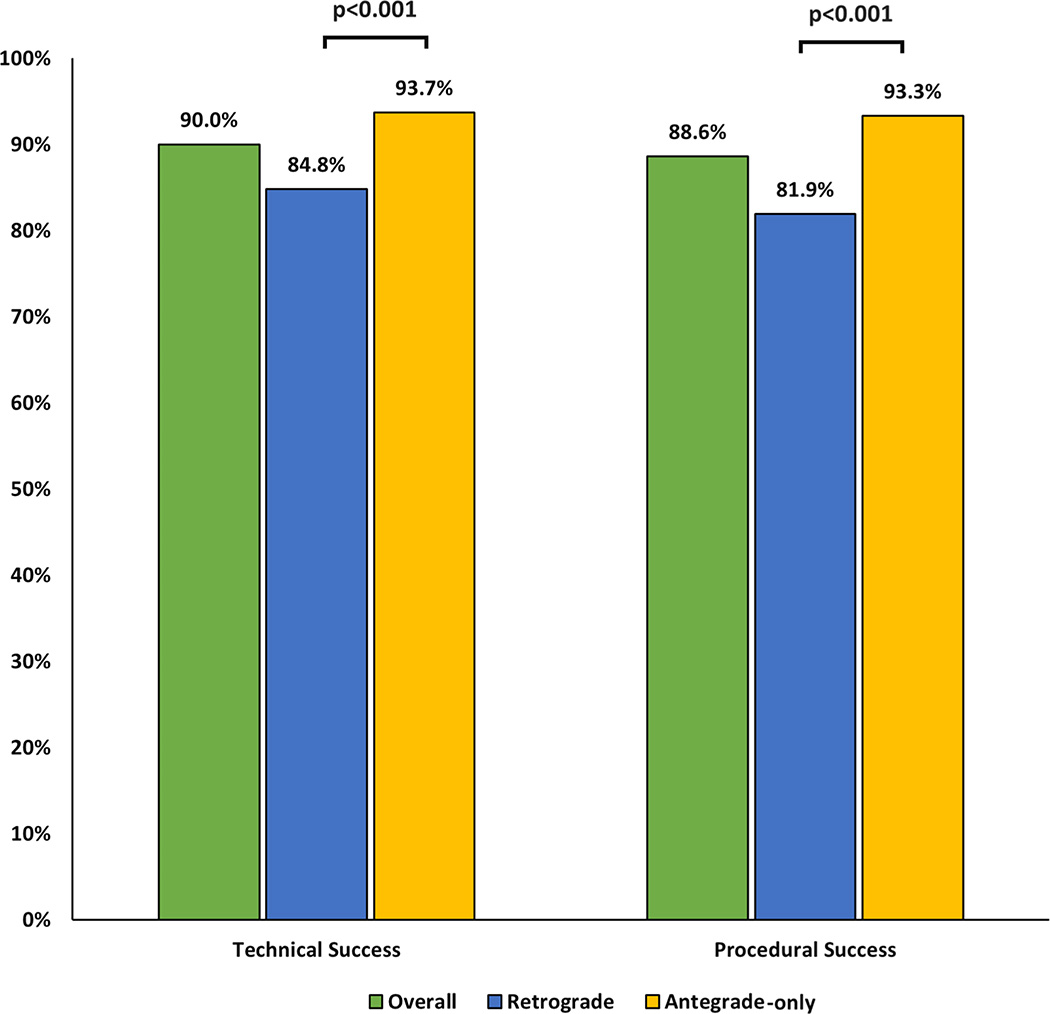
Procedural outcomes
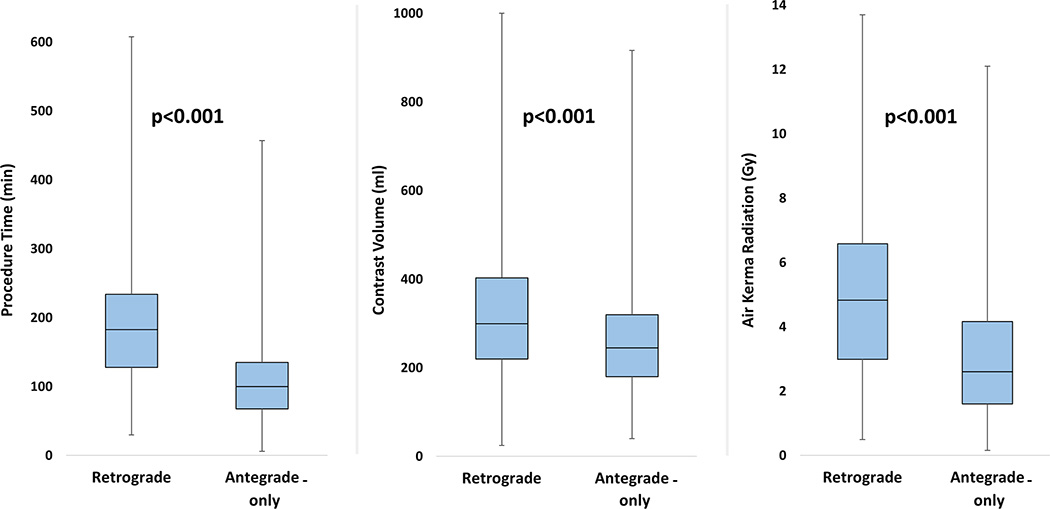
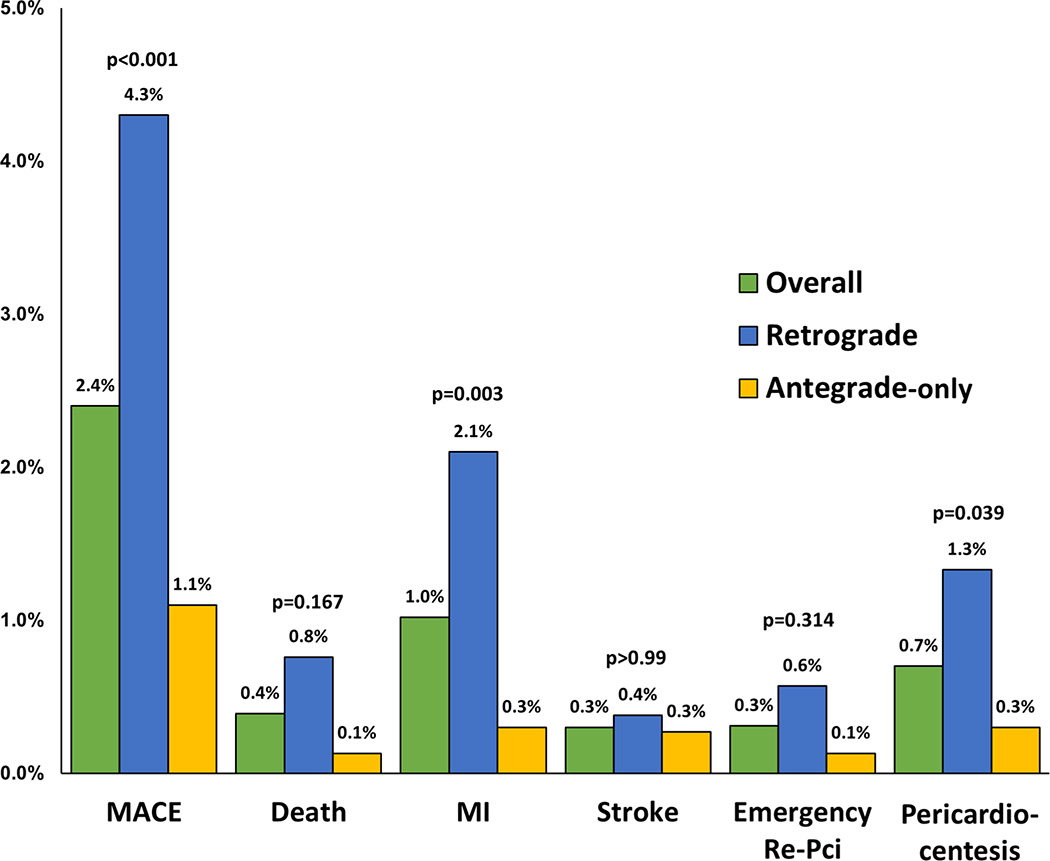
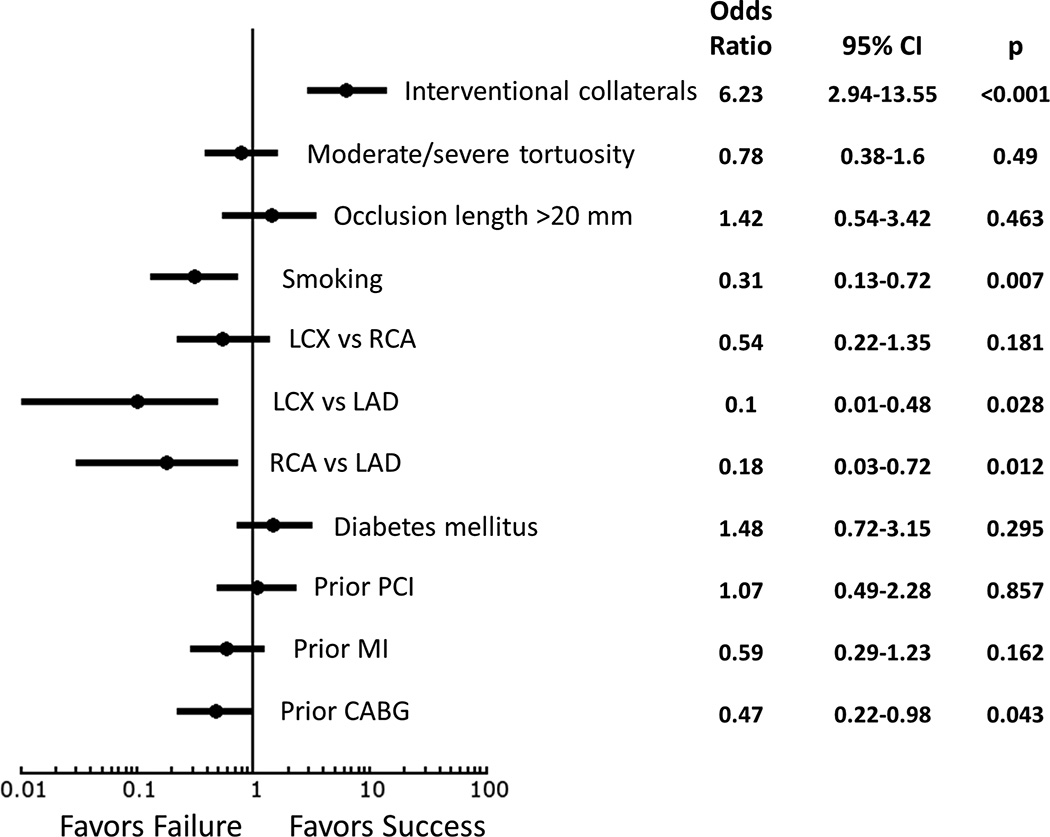
Technical and procedural success among all 1,301 cases was 90.0% and 88.6%, respectively. As compared with antegrade-only cases, retrograde cases were associated with lower technical (84.8% vs. 93.7%, p<0.001) and procedural (81.9% vs. 93.3%, p<0.001) success (Table 2, Figure 2) and required more contrast (300 [220–404] vs. 245 [180–320] ml, p<0.001), higher air kerma radiation dose (4.8 [3.0–6.6] vs. 2.6 [1.6–4.2] Gray, p<0.001), and longer procedure time (183 [128–234] vs. 100 [68–135] min, p<0.001) (Figure 3). They also more frequently required use of a hemodynamic support device (6.5% vs. 2.1%, p<0.001). In-hospital MACE occurred in 31 patients (2.4%), and were more common among retrograde cases (4.3% vs. 1.1%, p <0.001), mostly due to higher incidence of myocardial infarction (2.1% vs. 0.3%, p=0.003) (Figure 4). Patients without interventional collaterals had lower success rates as compared with those with interventional collaterals (Supplemental Table 1). On multivariable analysis, the presence of interventional collaterals, left anterior descending artery as target vessel, no smoking and no prior CABG were independently associated with technical success (Figure 5).
Table 2.
Procedural Characteristics and Outcomes of the Study Lesions, Classified According to Whether Retrograde Crossing was Attempted or Not
| Variable | Overall | Retrograde | Antegrade-only | p |
|---|---|---|---|---|
| IVUS used (%)† | 37.2 | 48.5 | 30.5 | <0.001 |
| Stent optimization (%) | 46.2 | 42.6 | 49.6 | 0.283 |
| To guide rCART (%) | 11.4 | 23.5 | - | - |
| To determine appropriate stent size (%) |
36.9 | 37.4 | 36.4 | 0.870 |
| To assist wiring (%) | 25.9 | 30.4 | 21.5 | 0.117 |
| To guide antegrade cap puncture (%) |
13.1 | 14.8 | 11.6 | 0.465 |
| Stenting (%) | 88.6 | 84.2 | 91.6 | <0.001 |
| Number of stents* | 2.5±1.1 | 2.9±1.2 | 2.3±1 | <0.001 |
| Stent length (mm)* | 52.3±45.6 | 59.5±51.9 | 47.7±40.2 | <0.001 |
| Hemodynamic support (%) | 4.0 | 6.7 | 2.1 | <0.001 |
| Fluoroscopy time (min)* | 45.6 (27.2–75.1) | 73.8 (53.1– 101.4) |
31.8 (20.2–46.4) | <0.001 |
| Patient air kerma radiation dose (Gray)* |
3.5 (2.0–5.4) | 4.8 (3.0–6.6) | 2.6 (1.6–4.2) | <0.001 |
| Procedure time (min)* | 125 (85–185) | 183 (128–234) | 100 (68–135) | <0.001 |
| Contrast volume (ml)* | 260 (200 – 360) | 300 (220 – 404) | 245 (180 – 320) | <0.001 |
| Technical success (%) | 90.0 | 84.8 | 93.7 | <0.001 |
| Antegrade wire escalation (%) |
46.7 | 8.8 | 71.0 | <0.001 |
| Antegrade dissection/re- entry (%) |
24.6 | 17.7 | 29.0 | |
| Retrograde (%) | 28.7 | 73.5 | - | |
| Procedural success (%) | 88.6 | 81.9 | 93.3 | <0.001 |
| MACE (%) | 2.4 | 4.3 | 1.1 | <0.001 |
| Death (%) | 0.4 | 0.8 | 0.1 | 0.167 |
| Myocardial infarction (%) | 1.0 | 2.1 | 0.3 | 0.003 |
| Stroke (%) | 0.3 | 0.4 | 0.3 | 0.999 |
| Emergency re-PCI (%) | 0.3 | 0.6 | 0.1 | 0.314 |
| Emergency CABG (%) | - | - | - | - |
| Emergency | 0.7 | 1.3 | 0.3 | 0.039 |
| Pericardiocentesis (%) | ||||
| Coronary perforation (%) | 3.4 | 5.5 | 1.9 | <0.001 |
CABG, coronary artery bypass graft surgery; IVUS, intravascular ultrasound; MACE, major adverse cardiovascular events; PCI, percutaneous coronary intervention; rCART, reverse controlled antegrade and retrograde subintimal tracking
mean±standard deviation or median (interquartile range).
In some procedures IVUS was used for multiple indications.
Figure 2.
Technical and procedural success rates overall, for retrograde and for antegrade-only cases.
Figure 3.
Box plots for contrast, radiation and procedure time of the study procedures, classified according to whether retrograde techniques were used or not.
Lines represent minimum, 25th centile, median, 75th centile and maximum values.
Figure 4.
Incidence of in-hospital major adverse cardiovascular events of the study procedures, classified according to whether retrograde techniques were used or not.
(MACE, major adverse cardiovascular events; MI, myocardial infarction; PCI, percutaneous coronary intervention)
Figure 5.
Predictors of technical success for retrograde CTO PCI
(CABG, coronary artery bypass graft; CTO, chronic total occlusion; LAD, left anterior descending; LCX, left circumflex; MACE, major adverse cardiovascular events; MI, myocardial infarction; PCI, percutaneous coronary intervention; RCA, right coronary artery)
Retrograde sequence and outcomes
A primary retrograde approach was utilized in 248 cases (46%), whereas in the remaining 291 (54%) retrograde cases the retrograde approach was used after antegrade crossing failure during the index procedure (Figure 1). As compared with secondary use of the retrograde approach, primary retrograde cases involved longer lesions (42.5 [30–70] mm vs. 30.0 [20–50] mm, p<0.001), with more frequent proximal cap ambiguity (58.3% vs. 38.1%, p<0.001) and prior failed attempts (25.6% vs. 16.1%, p=0.007) (Table 3). They also had a higher J-CTO score (3.3 ± 0.9 vs. 2.9 ± 1.1, p<0.001), and were more likely to have suitable interventional collaterals (84.5% vs 73.3%, p=0.007).
Table 3.
Angiographic Characteristics and Outcomes According to Retrograde Sequence
| Variable | Primary retrograde n = 248 (46%) |
Retrograde after antegrade failure n =291 (54%) |
p |
|---|---|---|---|
| Target Vessel | |||
| RCA (%) | 73.0 | 64.0 | 0.088 |
| LCX (%) | 15.2 | 19.3 | |
| LAD (%) | 11.8 | 16.7 | |
| CTO length (mm)* | 42.5 (30–70) | 30.0 (20–50) | <0.001 |
| Interventional collaterals (%) | 84.5 | 73.3 | 0.007 |
| Proximal cap ambiguity (%) | 58.3 | 38.1 | <0.001 |
| Moderate/severe tortuosity (%) | 40.3 | 42.1 | 0.677 |
| Moderate/severe calcification (%) | 69.2 | 70.2 | 0.802 |
| Poor distal target vessel (%) | 56.8 | 47.8 | 0.069 |
| In-stent restenosis (%) | 12.8 | 14.0 | 0.681 |
| Prior-failed CTO PCI (%) | 25.6 | 16.1 | 0.007 |
| J-CTO score* | 3.3±0.9 | 2.9±1.1 | <0.001 |
| Collaterals used | |||
| Septal (%) | 57.3 | 53.3 | 0.353 |
| Epicardial (%) | 34.7 | 30.6 | 0.312 |
| LIMA (%) | 2.4 | 2.1 | 0.779 |
| SVG (%) | 13.3 | 13.8 | 0.882 |
| Collateral crossing | |||
| Wire (%) | 82.5 | 68.7 | <0.001 |
| Sion† (%) | 65.3 | 71.5 | |
| Fielder FC/XT† (%) | 17.8 | 19.5 | 0.179 |
| Other (%) | 17.0 | 8.9 | |
| Microcatheter (%) | 78.7 | 66.9 | 0.004 |
| Corsair† (%) | 93.5 | 82.4 | |
| Other (%) | 6.5 | 17.6 | |
| Externalization (%) | 66.1 | 54.9 | 0.030 |
| CTO wiring technique | |||
| Reverse CART (%) | 66.1 | 58.0 | |
| Retrograde true lumen crossing (%) |
17.8 | 20.4 | 0.313 |
| Retrograde wire as marker (%) | 1.7 | 4.9 | |
| CART (%) | 1.7 | 3.7 | |
| Guideliner‡ rCART (%) | 1.2 | 2.5 | |
| Other/missing (%) | 11.5 | 10.5 | |
| Procedure time (mins)* | 170 (112 –236) | 187 (142–234) | 0.023 |
| Contrast volume (ml)* | 260 (200–375) | 343 (250–440) | <0.001 |
| Patient air kerma radiation dose (Gray)* |
4.7 (2.5–6.2) | 5.0 (3.2–6.9) | 0.089 |
| Technical success (%) | 85.5 | 84.2 | 0.677 |
| Retrograde (%) | 82.1 | 66.1 | |
| Antegrade wire escalation (%) | 6.1 | 11.0 | <0.001 |
| Antegrade dissection/re-entry (%) | 11.8 | 22.9 | |
| Procedural success (%) | |||
| MACE (%) | 84.4 | 79.9 | 0.179 |
| 3.6 | 4.8 | 0.499 | |
CART, controlled antegrade and retrograde tracking; CTO, chronic total occlusion; LAD, left anterior descending artery; LCX, left circumflex artery; LIMA, left internal mammary artery; MACE, major adverse cardiovascular events; MI, myocardial infarction; PCI, percutaneous coronary intervention; RCA, right coronary artery; SVG, saphenous vein graft.
mean±standard deviation or median (interquartile range).
Asahi Intecc, Nagoya, Japan,
Vascular Solutions, Minneapolis, MN
The most common collaterals used were septal (55.1%) followed by epicardial (32.5%), saphenous vein grafts (13.5%) and left internal mammary artery grafts (2.2%) (more than one types of collateral were used in some procedures). The use of epicardial collaterals was not associated with an increase in MACE or coronary perforation (Supplemental Table 2). Collateral wiring success was significantly higher in the primary retrograde group (82.5% vs. 68.7%, p<0.001), as was the microcatheter crossing rate (78.7% vs. 66.9%, p=0.004). Technical success was similar in the two groups (85.5% vs. 84.2%, p=0.677), but was achieved significantly more often via a retrograde approach in the primary retrograde group (70.2% vs. 55.7%, p<0.001) and an antegrade approach in the secondary retrograde group (15.3% vs. 28.5%, p<0.001). Overall, the retrograde approach was the final successful crossing strategy in 336 PCIs, accounting for 28.7% of all technical success.
Retrograde crossing was most often achieved using reverse controlled antegrade and retrograde tracking (62.2%), followed by retrograde true lumen puncture (19.1%). Primary retrograde cases required significantly less time (170 [112–236] vs. 187 [142–234] min, p=0.023) and contrast (260 [200–375] vs. 343 [250–440] ml, p<0.001) to complete. Procedural success rate as well as the incidence of MACE were similar among primary and secondary retrograde cases.
Discussion
The major finding of our study is that the retrograde approach to CTO PCI is commonly utilized (in 41.4% of cases), especially in more complex lesions. While retrograde CTO PCI carries lower success and higher complication rates as compared with antegrade-only cases, it was a key contributor to the overall high success rates observed in this contemporary multicenter registry.
Table 4 summarizes the largest published retrograde CTO PCI series to date.7, 12, 22–25 Utilization of the retrograde approach has been highly variable ranging from 11.8% to 41.4% in the present study. This may in part reflect the increasing familiarity with and refinement of the technique, but also the extensive experience of the participating operators in our study, as well as implementation of the hybrid algorithm for CTO PCI which encourages early strategy change if the initial strategy fails to achieve progress.26, 27 According to this algorithm, a primary retrograde approach is favored in case of proximal cap ambiguity (e.g. due to side branches near the proximal cap or aorto-ostial occlusion) or poor distal target vessel (e.g. small luminal diameter, diffusely diseased segment), especially in the presence of interventional collaterals, and/or when a prior antegrade attempt during a previous procedure has failed. Of all primary retrograde procedures in our study, 97% had at least one angiographic parameter favoring a primary retrograde approach, and 77% had two or more. Although use of the retrograde approach has been proposed as a means to reduce contrast administration, contrast utilization in primary retrograde procedures was higher than the inherently simpler, antegrade-only procedures in our study (median: 260 ml vs. 245 ml), likely due to higher angiographic complexity of primary retrograde cases and the need of contrast injections to cross the collateral.
Table 4.
Largest Published CTO PCI Series to Date Including >200 Retrograde PCIs.
| Study | Year | Retrograde PCI n, (%) |
Primary retrograde* (%) |
Prior failed CTO PCI in retrograde group (%) |
Overall technical success in retrograde group† (%) |
MACE in retrograde group† (%) |
|---|---|---|---|---|---|---|
| Kimura et al.22 | 2009 | 224 | 100 | 65 | 92 | 1.8 |
| Galassi et al.23 | 2011 | 234 (12) | 76 | U | 65 | 3.0 |
| Karmpaliotis et al.12 | 2012 | 462 (34) | 46 | 18 | 81 | 2.6 |
| Yamane et al.24 | 2013 | 378 (25) | 75 | 32 | 84 | 0.5 |
| Tsutchikane et al.25 | 2013 | 801 (27) | 67 | 29 | 85 | 1.6 |
| Galassi et al.7 | 2015 | 1582 (16) | 76 | 43 | 75 | 0.8 |
| Present Study | 2015 | 539 (41) | 46 | 21 | 85 | 4.3 |
Retrograde as first crossing strategy during index procedure.
Definition varies according to study.
CTO, chronic total occlusion; MACE, major adverse cardiovascular events; PCI, percutaneous coronary intervention; U, unknown
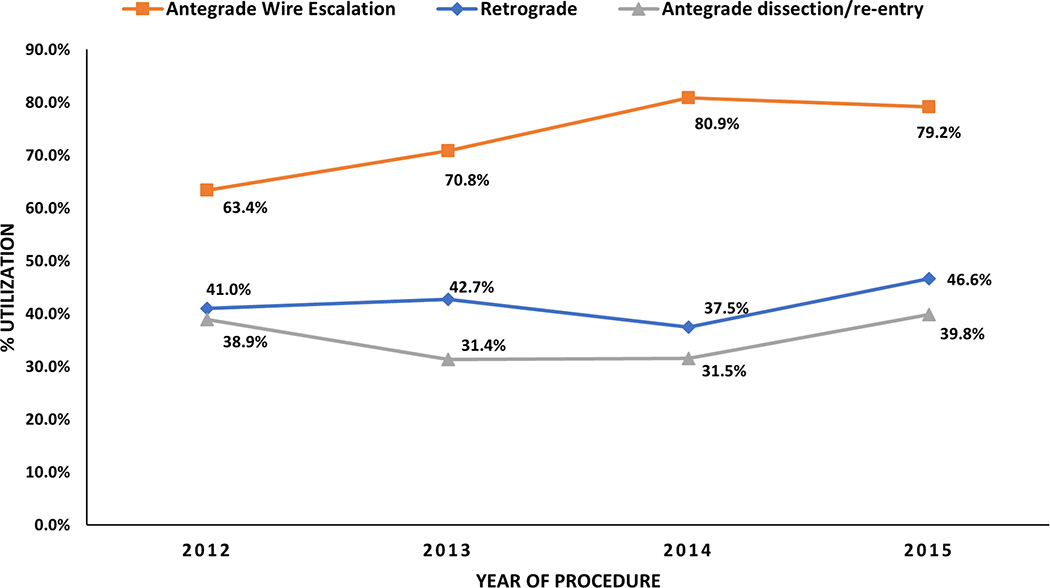
Although the success of retrograde CTO PCI cases was lower than antegrade-only cases in our series, use of the retrograde approach likely contributed to the overall high success rate in this registry, as many of the retrograde patients would likely have failed antegrade crossing. Indeed, retrograde crossing was the final successful strategy in 25.8% of all CTO PCIs in our registry. Similarly, Thompson et al. previously demonstrated that operators who adopted the retrograde approach had increasing success rates, whereas operators who did not had declining success rates,14 a finding that was subsequently replicated by Michael et al.28 In our registry, we observed a numerical increase in retrograde utilization with time (Figure 6), concordant with a significant increase in the average number of strategies utilized per case (1.4±0.7 in 2012 to 1.7± 0.8 in 2015, p<0.001).This may be partly attributed to increased familiarity with retrograde techniques and their utilization for increasingly complex lesions (J-CTO score: 2.5±1.2 vs. 2.8±1.2, p=0.024).
Figure 6.
Temporal trends in utilization of antegrade wire escalation, antegrade dissection/ re-entry and the retrograde approach.
The likelihood for retrograde CTO PCI success was higher among patients with interventional collaterals (i.e. collaterals considered crossable by the operator). Yet, even among patients without interventional collaterals, 71.6% success was achieved with the retrograde approach being the final successful strategy in 31.8% of cases. Therefore, even though the retrograde approach may be best attempted in cases with interventional collaterals (especially early in the learning curve), a retrograde attempt can and should be considered even in patients without interventional collaterals if antegrade crossing attempts fail. Despite similar complication rates with use of septal and epicardial collaterals in our study, epicardial collaterals should be avoided early on due to the potentially catastrophic and difficult to manage complications associated with their perforation.
In the largest retrograde CTO PCI series published to date, Galassi et al. reported the results of 1,582 retrograde out of a total of 9,589 CTO PCIs from the European Registry of Chronic Total Occlusion (ERCTO), with a technical success rate of 75% and an in-hospital MACE rate of 0.8%. While the patients in our study were more likely to have diabetes (45.0% vs. 29.0%) and prior CABG (33.9% vs. 17.6%), the proportion of prior failed attempt for CTO PCI was higher (42.5%) in the European cohort. This may partly explain the difference in sequence selection for the retrograde approach, with 3 out of 4 patients (76%) in ERCTO undergoing a primary retrograde approach, as opposed to 46% in Progress CTO. The high prevalence of prior – usually antegrade – failed CTO PCI in patients undergoing a retrograde recanalization attempt (Table 4) suggests that such patients may be at increased risk for complications, such as radiation skin injury or contrast nephropathy. On the other hand, a prior failed attempt in which the target vessel was favorably modified - usually by balloon dilatation of the proximal cap and/or subintimal space - may facilitate success of subsequent attempt, a concept known as “investment procedure”. To minimize the risk for complications, repeat procedures are usually performed after at least 1–2 months have elapsed to allow healing of coronary dissections and reduce the adverse impact of repeat exposure to radiation.
In 2014 El Sabbagh et al. performed a meta-analysis of 3,482 retrograde CTO PCI patients from 26 studies.29 A primary retrograde attempt was performed in 52.4%, procedural success was 83.3% and the risk of death, urgent CABG, MI, and tamponade were 0.7%, 0.7%, 3.1%, and 1.4%, respectively, suggesting that the retrograde approach may carry increased risk for complications. An increased risk with retrograde crossing was also observed in our study, with a four-fold higher in-hospital major complication rate for retrograde as compared to antegrade-only techniques, primarily driven by myocardial infarction. Several mechanisms may be responsible for this risk, including collateral channel injury which can cause myocardial infarction, as demonstrated by two prior studies.30, 31 Collateral perforation can also result in pericardial tamponade, which contrary to common belief, may carry increased risk among prior CABG patients due to the formation of localized tamponade, and require specialized measures to achieve hemostasis.32–35 Moreover, donor vessel injury could lead to acute, life threatening hemodynamic compromise. Our study demonstrates that the presence of good interventional collaterals is a strong predictor of technical success for CTO PCI. However, given the higher risk for complications with the retrograde approach, an initial antegrade attempt may be preferred, if feasible. This is further supported by the longer procedure times, higher contrast and radiation requirements, larger number of stents, and more frequent use of hemodynamic support with the retrograde approach, although these differences may be partly attributed to the high baseline clinical and angiographic complexity of patients who underwent retrograde CTO PCI. The hybrid algorithm to CTO PCI can serve as a valuable tool to select the best approach sequence, both while planning as well as during the procedure.27
Study limitations
Our study was a retrospective, observational study, subject to selection bias. The comparison of final technical success between antegrade-only and retrograde cases may be biased in favor of antegrade procedures, as many failed antegrade procedures subsequently underwent a retrograde attempt and were, thus, classified as retrograde. Our analysis included procedures performed by highly skilled and experienced CTO operators, and thus our results may not apply to less experienced operators.36 Some of the participating centers enrolled patients during parts of the study period. There was no local monitoring or core laboratory adjudication of the angiograms or centralized clinical event adjudication. Detailed procedural characteristics were not available for previously failed CTO PCI attempts, and some technical characteristics (e.g. collateral “surfing” vs. use of microcatheter tip injection to negotiate collaterals) were not available for the index procedure.
Conclusions
In summary, the retrograde approach is a critical component of CTO PCI and an important contributor to overall high success rates, especially for more complex patients and lesions, yet may carry a higher risk of complications.
Supplementary Material
What is Known
Retrograde intervention through collateral circulation has greatly improved success of chronic total occlusion (CTO) percutaneous coronary intervention (PCI).
However, retrograde intervention has been associated with higher risk for procedural complications.
With the advent of new antegrade techniques and equipment improving antegrade CTO PCI success rates, the role of retrograde CTO PCI may be changing.
What the Study Adds
As compared to an antegrade-only approach, retrograde intervention is utilized for clinically and angiographically challenging cases.
Procedures necessitating use of the retrograde approach have lower technical success, higher risk for adverse events, and are associated with lower procedural efficiency.
Nevertheless, use of the retrograde approach was responsible for successful recanalization of approximately 1 out of 4 lesions in our registry, highlighting its importance in contemporary CTO PCI.
Acknowledgments
Study data were collected and managed using REDCap electronic data capture tools hosted at University of Texas Southwestern Medical Center.37 REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources.
Sources of Funding
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health” under award Number UL1TR001105. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Disclosures
Dr. Karmpaliotis: speaker bureau, Abbott Vascular, Medtronic, and Boston Scientific. Consultant, Bridgepoint Medical
Dr. Karatasakis: none
Dr. Alaswad: consulting fees from Terumo and Boston Scientific; consultant, no financial, Abbott Laboratories
Dr. Jaffer: consultant to Boston Scientific, Siemens, and Merck, nonfinancial research support from Abbott Vascular, research grant from National Institutes of Health (HL-R01-108229).
Dr. Yeh: Career Development Award (1K23HL118138) from the National Heart, Lung, and Blood Institute.
Dr. Wyman: Honoraria/consulting/speaking fees from Boston Scientific, Abbott Vascular, and Asahi.
Dr. Lombardi: equity with Bridgepoint Medical
Dr. Grantham: Speaking fees, consulting, and honoraria from Boston Scientific, Asahi Intecc. Research grants from Boston Scientific, Asahi Intecc, Abbott Vascular, Medtronic.
Dr. Kandzari: research/grant support and consulting honoraria from Boston Scientific and Medtronic Cardiovascular, and research/grant support from Abbott.
Dr. Lembo: speaker bureau: Medtronic; advisory board Abbott Vascular and Medtronic.
Dr. Doing: none
Dr. Moses: consultant for Abbot and Boston Scientific
Dr. Kirtane: Institutional research grants to Columbia University from Boston Scientific, Medtronic, Abbott Vascular, Abiomed, St. Jude Medical, Vascular Dynamics, Glaxo SmithKline, and Eli Lilly.
Dr. Parikh: none
Dr. Patel: none
Dr. Bahadorani: none
Dr. Ali: grant support and is a consultant for St. Jude Medical and InfraRedX
Dr. Kalra: none
Dr. Nguyen-Trong: none
Dr. Danek: none
Dr. Karacsonyi: none
Dr. Rangan: none
Ms. Roesle: none
Dr. Thompson: employee of Boston Scientific
Dr. Banerjee: research grants from Gilead and the Medicines Company; consultant/speaker honoraria from Covidien and Medtronic; ownership in MDCARE Global (spouse); intellectual property in HygeiaTel.
Dr. Brilakis: consulting/speaker honoraria from Abbott Vascular, Asahi, Boston Scientific, Elsevier, Somahlution, St Jude Medical, and Terumo; research support from Boston Scientific and InfraRedx; spouse is employee of Medtronic.
References
- 1.Rathore S, Matsuo H, Terashima M, Kinoshita Y, Kimura M, Tsuchikane E, Nasu K, Ehara M, Asakura Y, Katoh O, Suzuki T. Procedural and in-hospital outcomes after percutaneous coronary intervention for chronic total occlusions of coronary arteries 2002 to 2008: Impact of novel guidewire techniques. JACC Cardiovasc Interv. 2009;2:489–497. doi: 10.1016/j.jcin.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 2.Saito S. Different strategies of retrograde approach in coronary angioplasty for chronic total occlusion. Catheter Cardiovasc Interv. 2008;71:8–19. doi: 10.1002/ccd.21316. [DOI] [PubMed] [Google Scholar]
- 3.Surmely JF, Katoh O, Tsuchikane E, Nasu K, Suzuki T. Coronary septal collaterals as an access for the retrograde approach in the percutaneous treatment of coronary chronic total occlusions. Catheter Cardiovasc Interv. 2007;69:826–832. doi: 10.1002/ccd.20816. [DOI] [PubMed] [Google Scholar]
- 4.Surmely JF, Tsuchikane E, Katoh O, Nishida Y, Nakayama M, Nakamura S, Oida A, Hattori E, Suzuki T. New concept for cto recanalization using controlled antegrade and retrograde subintimal tracking: The cart technique. J Invasive Cardiol. 2006;18:334–338. [PubMed] [Google Scholar]
- 5.Tsuchikane E, Katoh O, Kimura M, Nasu K, Kinoshita Y, Suzuki T. The first clinical experience with a novel catheter for collateral channel tracking in retrograde approach for chronic coronary total occlusions. JACC Cardiovasc Interv. 2010;3:165–171. doi: 10.1016/j.jcin.2009.10.026. [DOI] [PubMed] [Google Scholar]
- 6.Tomasello SD, Marza F, Giubilato S, Galassi AR. Retrograde approach for revascularization of coronary chronic total occlusion. Minerva Cardioangiol. 2012;60:461–472. [PubMed] [Google Scholar]
- 7.Galassi AR, Sianos G, Werner GS, Escaned J, Tomasello SD, Boukhris M, Castaing M, Buttner JH, Bufe A, Kalnins A, Spratt JC, Garbo R, Hildick-Smith D, Elhadad S, Gagnor A, Lauer B, Bryniarski L, Christiansen EH, Thuesen L, Meyer-Gessner M, Goktekin O, Carlino M, Louvard Y, Lefevre T, Lismanis A, Gelev VL, Serra A, Marza F, Di Mario C, Reifart N Euro CTOC. Retrograde recanalization of chronic total occlusions in europe: Procedural, in-hospital, and long-term outcomes from the multicenter ercto registry. J Am Coll Cardiol. 2015;65:2388–2400. doi: 10.1016/j.jacc.2015.03.566. [DOI] [PubMed] [Google Scholar]
- 8.Sianos G, Barlis P, Di Mario C, Papafaklis MI, Buttner J, Galassi AR, Schofer J, Werner G, Lefevre T, Louvard Y, Serruys PW, Reifart N Euro CTOC. European experience with the retrograde approach for the recanalisation of coronary artery chronic total occlusions. A report on behalf of the eurocto club. EuroIntervention. 2008;4:84–92. doi: 10.4244/eijv4i1a15. [DOI] [PubMed] [Google Scholar]
- 9.Stojkovic S, Sianos G, Katoh O, Galassi AR, Beleslin B, Vukcevic V, Nedeljkovic M, Stankovic G, Orlic D, Dobric M, Tomasevic M, Ostojic M. Efficiency, safety, and long-term follow-up of retrograde approach for cto recanalization: Initial (belgrade) experience with international proctorship. J Interv Cardiol. 2012;25:540–548. doi: 10.1111/j.1540-8183.2012.00754.x. [DOI] [PubMed] [Google Scholar]
- 10.Rinfret S, Joyal D, Nguyen CM, Bagur R, Hui W, Leung R, Larose E, Love MP, Mansour S. Retrograde recanalization of chronic total occlusions from the transradial approach; early canadian experience. Catheter Cardiovasc Interv. 2011;78:366–374. doi: 10.1002/ccd.23140. [DOI] [PubMed] [Google Scholar]
- 11.Brilakis ES, Grantham JA, Thompson CA, DeMartini TJ, Prasad A, Sandhu GS, Banerjee S, Lombardi WL. The retrograde approach to coronary artery chronic total occlusions: A practical approach. Catheter Cardiovasc Interv. 2012;79:3–19. doi: 10.1002/ccd.23004. [DOI] [PubMed] [Google Scholar]
- 12.Karmpaliotis D, Michael TT, Brilakis ES, Papayannis AC, Tran DL, Kirkland BL, Lembo N, Kalynych A, Carlson H, Banerjee S, Lombardi W, Kandzari DE. Retrograde coronary chronic total occlusion revascularization: Procedural and in-hospital outcomes from a multicenter registry in the united states. JACC Cardiovasc Interv. 2012;5:1273–1279. doi: 10.1016/j.jcin.2012.06.025. [DOI] [PubMed] [Google Scholar]
- 13.Michael TT, Mogabgab O, Alomar M, Kotsia A, Christopoulos G, Rangan BV, Abdullah S, Grodin J, Banerjee S, Brilakis ES. Long-term outcomes of successful chronic total occlusion percutaneous coronary interventions using the antegrade and retrograde approach. J Interv Cardiol. 2014;27:465–471. doi: 10.1111/joic.12149. [DOI] [PubMed] [Google Scholar]
- 14.Thompson CA, Jayne JE, Robb JF, Friedman BJ, Kaplan AV, Hettleman BD, Niles NW, Lombardi WL. Retrograde techniques and the impact of operator volume on percutaneous intervention for coronary chronic total occlusions an early u.S. Experience. JACC Cardiovasc Interv. 2009;2:834–842. doi: 10.1016/j.jcin.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 15.Alaswad K, Menon RV, Christopoulos G, Lombardi WL, Karmpaliotis D, Grantham JA, Marso SP, Wyman MR, Pokala NR, Patel SM, Kotsia AP, Rangan BV, Lembo N, Kandzari D, Lee J, Kalynych A, Carlson H, Garcia SA, Thompson CA, Banerjee S, Brilakis ES. Transradial approach for coronary chronic total occlusion interventions: Insights from a contemporary multicenter registry. Catheter Cardiovasc Interv. 2015;85:1123–1129. doi: 10.1002/ccd.25827. [DOI] [PubMed] [Google Scholar]
- 16.Christopoulos G, Karmpaliotis D, Alaswad K, Lombardi WL, Grantham JA, Rangan BV, Kotsia AP, Lembo N, Kandzari DE, Lee J, Kalynych A, Carlson H, Garcia S, Banerjee S, Thompson CA, Brilakis ES. The efficacy of "hybrid" percutaneous coronary intervention in chronic total occlusions caused by in-stent restenosis: Insights from a us multicenter registry. Catheter Cardiovasc Interv. 2014;84:646–651. doi: 10.1002/ccd.25465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christopoulos G, Karmpaliotis D, Wyman MR, Alaswad K, McCabe J, Lombardi WL, Grantham JA, Marso SP, Kotsia AP, Rangan BV, Garcia SA, Lembo N, Kandzari D, Lee J, Kalynych A, Carlson H, Thompson CA, Banerjee S, Brilakis ES. Percutaneous intervention of circumflex chronic total occlusions is associated with worse procedural outcomes: Insights from a multicentre us registry. Can J Cardiol. 2014;30:1588–1594. doi: 10.1016/j.cjca.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Christopoulos G, Menon RV, Karmpaliotis D, Alaswad K, Lombardi W, Grantham A, Patel VG, Rangan BV, Kotsia AP, Lembo N, Kandzari D, Carlson H, Garcia S, Banerjee S, Thompson CA, Brilakis ES. The efficacy and safety of the "hybrid" approach to coronary chronic total occlusions: Insights from a contemporary multicenter us registry and comparison with prior studies. J Invasive Cardiol. 2014;26:427–432. [PMC free article] [PubMed] [Google Scholar]
- 19.Christopoulos G, Menon RV, Karmpaliotis D, Alaswad K, Lombardi W, Grantham JA, Michael TT, Patel VG, Rangan BV, Kotsia AP, Lembo N, Kandzari DE, Lee J, Kalynych A, Carlson H, Garcia S, Banerjee S, Thompson CA, Brilakis ES. Application of the "hybrid approach" to chronic total occlusions in patients with previous coronary artery bypass graft surgery (from a contemporary multicenter us registry) Am J Cardiol. 2014;113:1990–1994. doi: 10.1016/j.amjcard.2014.03.039. [DOI] [PubMed] [Google Scholar]
- 20.Sapontis J, Christopoulos G, Grantham JA, Wyman RM, Alaswad K, Karmpaliotis D, Lombardi WL, McCabe JM, Marso SP, Kotsia AP, Rangan BV, Christakopoulos GE, Garcia S, Thompson CA, Banerjee S, Brilakis ES. Procedural failure of chronic total occlusion percutaneous coronary intervention: Insights from a multicenter us registry. Catheter Cardiovasc Interv. 2015;85:1115–1122. doi: 10.1002/ccd.25807. [DOI] [PubMed] [Google Scholar]
- 21.Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, Ochiai M, Noguchi Y, Kato K, Shibata Y, Hiasa Y, Doi O, Yamashita T, Hinohara T, Tanaka H, Mitsudo K, Investigators JCR. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: The j-cto (multicenter cto registry in japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4:213–221. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 22.Kimura M, Katoh O, Tsuchikane E, Nasu K, Kinoshita Y, Ehara M, Terashima M, Matsuo H, Matsubara T, Asakura K, Asakura Y, Nakamura S, Oida A, Takase S, Reifart N, Di Mario C, Suzuki T. The efficacy of a bilateral approach for treating lesions with chronic total occlusions the cart (controlled antegrade and retrograde subintimal tracking) registry. JACC Cardiovasc Interv. 2009;2:1135–1141. doi: 10.1016/j.jcin.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 23.Galassi AR, Tomasello SD, Reifart N, Werner GS, Sianos G, Bonnier H, Sievert H, Ehladad S, Bufe A, Shofer J, Gershlick A, Hildick-Smith D, Escaned J, Erglis A, Sheiban I, Thuesen L, Serra A, Christiansen E, Buettner A, Costanzo L, Barrano G, Di Mario C. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: Insights from the ercto (european registry of chronic total occlusion) registry. EuroIntervention. 2011;7:472–479. doi: 10.4244/EIJV7I4A77. [DOI] [PubMed] [Google Scholar]
- 24.Yamane M, Muto M, Matsubara T, Nakamura S, Muramatsu T, Oida A, Igarashi Y, Nozaki Y, Kijima M, Tuschikane E. Contemporary retrograde approach for the recanalisation of coronary chronic total occlusion: On behalf of the japanese retrograde summit group. EuroIntervention. 2013;9:102–109. doi: 10.4244/EIJV9I1A15. [DOI] [PubMed] [Google Scholar]
- 25.Tsuchikane E, Yamane M, Mutoh M, Matsubara T, Fujita T, Nakamura S, Muramatsu T, Okamura A, Igarashi Y, Oida A. Retrograde Summit I. Japanese multicenter registry evaluating the retrograde approach for chronic coronary total occlusion. Catheter Cardiovasc Interv. 2013;82:E654–E661. doi: 10.1002/ccd.24823. [DOI] [PubMed] [Google Scholar]
- 26.Michael TT, Mogabgab O, Fuh E, Patel VG, El Sabbagh A, Alomar ME, Rangan BV, Abdullah SM, Banerjee S, Brilakis ES. Application of the "hybrid approach" to chronic total occlusion interventions: A detailed procedural analysis. J Interv Cardiol. 2014;27:36–43. doi: 10.1111/joic.12083. [DOI] [PubMed] [Google Scholar]
- 27.Christopoulos G, Karmpaliotis D, Alaswad K, Yeh RW, Jaffer FA, Wyman RM, Lombardi WL, Menon RV, Grantham JA, Kandzari DE, Lembo N, Moses JW, Kirtane AJ, Parikh M, Green P, Finn M, Garcia S, Doing A, Patel M, Bahadorani J, Tarar MN, Christakopoulos GE, Thompson CA, Banerjee S, Brilakis ES. Application and outcomes of a hybrid approach to chronic total occlusion percutaneous coronary intervention in a contemporary multicenter us registry. Int J Cardiol. 2015;198:222–228. doi: 10.1016/j.ijcard.2015.06.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Michael TT, Karmpaliotis D, Brilakis ES, Fuh E, Patel VG, Mogabgab O, Alomar M, Kirkland BL, Lembo N, Kalynych A, Carlson H, Banerjee S, Lombardi W, Kandzari DE. Procedural outcomes of revascularization of chronic total occlusion of native coronary arteries (from a multicenter united states registry) Am J Cardiol. 2013;112:488–492. doi: 10.1016/j.amjcard.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 29.El Sabbagh A, Patel VG, Jeroudi OM, Michael TT, Alomar ME, Mogabgab O, Fuh E, Roesle M, Rangan BV, Abdullah S, Hastings JL, Grodin J, Kumbhani DJ, Alexopoulos D, Fasseas P, Banerjee S, Brilakis ES. Angiographic success and procedural complications in patients undergoing retrograde percutaneous coronary chronic total occlusion interventions: A weighted meta-analysis of 3,482 patients from 26 studies. Int J Cardiol. 2014;174:243–248. doi: 10.1016/j.ijcard.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Lo N, Michael TT, Moin D, Patel VG, Alomar M, Papayannis A, Cipher D, Abdullah SM, Banerjee S, Brilakis ES. Periprocedural myocardial injury in chronic total occlusion percutaneous interventions: A systematic cardiac biomarker evaluation study. JACC Cardiovasc Interv. 2014;7:47–54. doi: 10.1016/j.jcin.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Werner GS, Coenen A, Tischer KH. Periprocedural ischaemia during recanalisation of chronic total coronary occlusions: The influence of the transcollateral retrograde approach. EuroIntervention. 2014;10:799–805. doi: 10.4244/EIJV10I7A139. [DOI] [PubMed] [Google Scholar]
- 32.Kotsia AP, Brilakis ES, Karmpaliotis D. Thrombin injection for sealing epicardial collateral perforation during chronic total occlusion percutaneous coronary interventions. J Invasive Cardiol. 2014;26:E124–E126. [PubMed] [Google Scholar]
- 33.Lowe R, Hammond C, Perry RA. Prior cabg does not prevent pericardial tamponade following saphenous vein graft perforation associated with angioplasty. Heart. 2005;91:1052. doi: 10.1136/hrt.2004.053132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marmagkiolis K, Brilakis ES, Hakeem A, Cilingiroglu M, Bilodeau L. Saphenous vein graft perforation during percutaneous coronary intervention: A case series. J Invasive Cardiol. 2013;25:157–161. [PubMed] [Google Scholar]
- 35.Michael TT, Karmpaliotis D, Brilakis ES, Abdullah SM, Kirkland BL, Mishoe KL, Lembo N, Kalynych A, Carlson H, Banerjee S, Lombardi W, Kandzari DE. Impact of prior coronary artery bypass graft surgery on chronic total occlusion revascularisation: Insights from a multicentre us registry. Heart. 2013;99:1515–1518. doi: 10.1136/heartjnl-2013-303763. [DOI] [PubMed] [Google Scholar]
- 36.Brilakis ES, Banerjee S, Karmpaliotis D, Lombardi WL, Tsai TT, Shunk KA, Kennedy KF, Spertus JA, Holmes DR, Jr, Grantham JA. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: A report from the ncdr (national cardiovascular data registry) JACC Cardiovasc Interv. 2015;8:245–253. doi: 10.1016/j.jcin.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 37.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (redcap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.