Abstract
Background:
Hospital readmission has been identified as a key quality indicator and a target for reducing health care spending.
Objective:
To evaluate the impact of a pharmacy-facilitated medication reconciliation and patient education model with post discharge follow-up on 30-day readmissions.
Methods:
This prospective, historical control study included all patients admitted during a 6-month period to a general medicine unit with the highest 30-day readmission rate at Yale-New Haven Hospital. Patients were excluded if they expired prior to discharge, transferred, left against medical advice, were discharged to hospice, or were previously enrolled in the study. Upon admission, pharmacy technicians compiled the medication reconciliation information. Interventions were made by the pharmacist communicating with the patient's primary team. Medication and disease state counseling and final medication reconciliation were performed by the pharmacist before discharge. The primary outcome measure was 30-day readmission rates during the intervention period compared to the preceding 6 months and the same time period the previous year. Secondary outcomes included the total number of pharmacist-identified medication reconciliation interventions, total pharmacy resource utilization, and identification of patients at high risk for readmission.
Results:
Study outcomes showed a 27% reduction in readmission during the intervention period. The pharmacist made a total of 546 medication interventions. The average pharmacist and pharmacy technician time per patient were 28.9 and 23.7 minutes, respectively.
Conclusions:
Pharmacy-facilitated medication reconciliation and patient education of medicine patients decreased 30-day readmission rates.
Keywords: medication reconciliation, transitions of care
A 2009 report in the New England Journal of Medicine indicated that approximately one-fifth (19.6%) of Medicare patients are readmitted to the hospital within 30 days of discharge and 34% are readmitted within 90 days. The majority of these hospital readmissions are avoidable, and it is estimated that only 10% of the readmissions are planned. In addition, the annual cost to Medicare of unplanned hospital readmissions exceeds $17 billion.1 As a result, hospital readmission has been identified as a key quality indicator and a target for reducing health care spending. The Centers for Medicare & Medicaid Services (CMS) publicly report 30-day readmission rates as a quality indicator. Additionally, the Patient Protection and Affordable Care Act contains provisions intended to reduce preventable hospital readmissions by reducing Medicare payments to hospitals with relatively high preventable readmissions rates compared to the national average.2
Several strategies have been proposed and trialed to decrease readmission rates including interventions aimed at improving transitions of care and accurate medication reconciliation. Pharmacist-facilitated medication management has demonstrated a reduction in medication errors and readmission rates in several published studies.3,4 In an unpublished study completed at our institution, we evaluated the impact of pharmacist-facilitated discharge education and medication reconciliation on readmission rates in high-risk heart failure and pneumonia patients who had a readmission in the previous 90 days. The study demonstrated a statistically significant 34% reduction in the readmission rate. Pharmacists' interventions were postulated to reduce readmissions by improving the quality of patient care and decreasing the chance of significant medication-related errors.
These outcomes could be further improved by identifying medication-related discrepancies on admission and by close follow-up after discharge. However, one of the barriers to implementing a hospital-wide, pharmacist-facilitated medication reconciliation model at admission and discharge is limited pharmacist resources. One strategy to overcome this barrier, consistent with the beliefs and assumptions of the American Society of Health-System Pharmacists (ASHP) 2010 Pharmacy Practice Model Summit, is to delegate some of the medication reconciliation activities to well-trained pharmacy technicians.5
The goal of this study was to evaluate the impact of instituting a pharmacy-facilitated medication reconciliation, patient education, and post discharge follow-up model on 30-day readmissions.
METHODS
We conducted a prospective, historical control study that included all patients admitted to one general medicine unit from October 2011 through March 2012. This unit was chosen because it had the highest readmission rate for the entire hospital. Patients admitted to this unit are covered by multiple medical teams (hospitalists and academic medical teams), making a change in practice more challenging. The control group consisted of a cohort of patients who were admitted to the same general medicine unit during the 6 months prior to the initiation of our study (April through September 2011) and patients admitted during the same time period a year earlier (October 2010 through March 2011). Patients were excluded if they were transferred to another hospital floor, left against medical advice, expired prior to discharge, or were discharged to hospice. For patients with more than one admission during the study period, only data from the first admission were included in the evaluation. The study was exempt from review by the institutional review board.
The pharmacist covering the floor was assigned to the project with assistance from postgraduate year 1 (PGY1) pharmacy residents during their Medicine rotation and on weekends. Technicians with 3 or more years of retail pharmacy experience were selected for this study to assume the role of Medication Reconciliation Technicians (MRTs) after undergoing a structured training program. The MRTs used computer census lists to identify newly admitted patients on a daily basis. Once identified, each patient and/or family member was interviewed by an MRT to obtain medication history, including herbal and over-the-counter products. All information gathered was cross-referenced with outpatient pharmacies, primary physicians' offices, and/or insurance companies. The pharmacist then performed admission medication reconciliation utilizing the medication history provided by the pharmacy technicians. Discrepancies and drug-related issues noted by the pharmacist were communicated to the physician covering the patient for resolution.
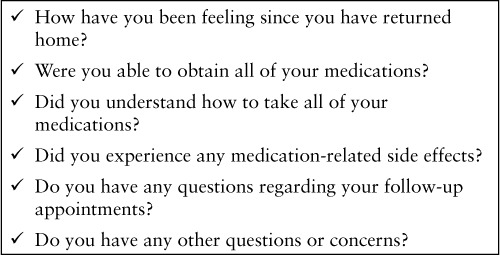
The pharmacist attended the daily interdisciplinary discharge rounds. In addition, the care coordinator assigned to the unit would inform the pharmacist of possible daily patient discharges. When discharge patients were identified, the pharmacist would then perform final medication reconciliation and patient education. Again, discrepancies noted by the pharmacist were communicated to the physician covering the patient. Twenty-four to 72 hours after discharge, the PGY1 pharmacy resident made a follow-up phone call to patients discharged to home or to home with health services to identify any medication-related issues. The phone call also ensured that the patients were reminded of their upcoming follow-up appointments. We used a standard script, adapted from the one used by Boston University's Project RED, to ensure consistency (Table 1).6
Table 1.
Postdischarge phone call standard script for the pharmacist
Data collected from patients' medical records and clinical and administrative databases included demographic information, discharge disposition, discharge diagnoses, length of hospital stay, and 30-day hospital readmissions.
STUDY OUTCOMES
The primary objective was to evaluate the impact of pharmacy-facilitated medication reconciliation and patient education on 30-day readmission. Secondary outcomes included total number of pharmacist-identified interventions, total pharmacy resource utilization, and identification of patients at high risk for readmission.
Descriptive statistics were calculated and chi-square analyses were conducted to assess the difference in readmission rates between the intervention arm and the control group (all patients admitted from October 2011 through March 2012 vs patients admitted to the same general medicine unit the 6 months prior). To account for seasonal variations, we compared the readmission rate in the intervention group to the rate in patients admitted during same time period the previous year (October 2010 through March 2011). The goal was to detect a 20% difference in readmission rates.
RESULTS
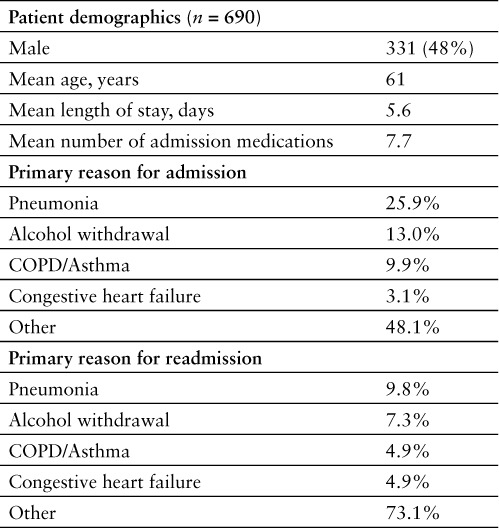
A total of 761 patients were admitted during the study period. Of these patients, 71 met one of the exclusion criteria and 690 patients were eligible for the study (Figure 1). Of these patients, 465 of patients (67%) received pharmacy intervention. Patient demographics, reason for admission, and reason for readmission of the intervention group are listed in Table 2.
Figure 1.
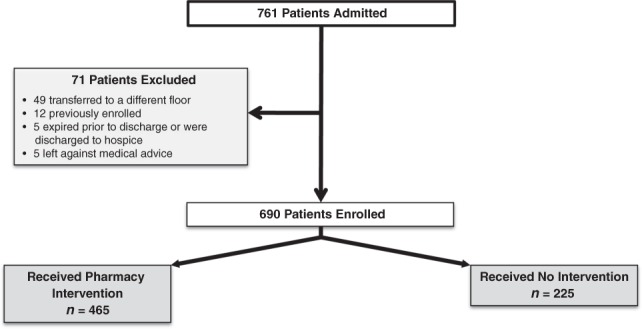
Patient enrollment and disposition.
Table 2.
Intervention group patient demographics, reason for admission, and readmission
The all-cause readmission rate in the intervention period was reduced by 27% compared to the previous 6 months (18% vs 24.7%; p = .009). A larger reduction (31%) was observed when we compared the readmission rate in the intervention period to the same time period the previous year (18% vs 26.2%; p = .002) (Figure 2). Because of logistical problems (time constraints, weekend or after-hours discharges), our pharmacists were not able to see all eligible patients. The greatest reduction in readmission was seen when patients who received pharmacy intervention (n = 465) were compared to patients in the same time period the previous year in a per protocol analysis (15.8% vs 26.2%; p = .0009).
Figure 2.
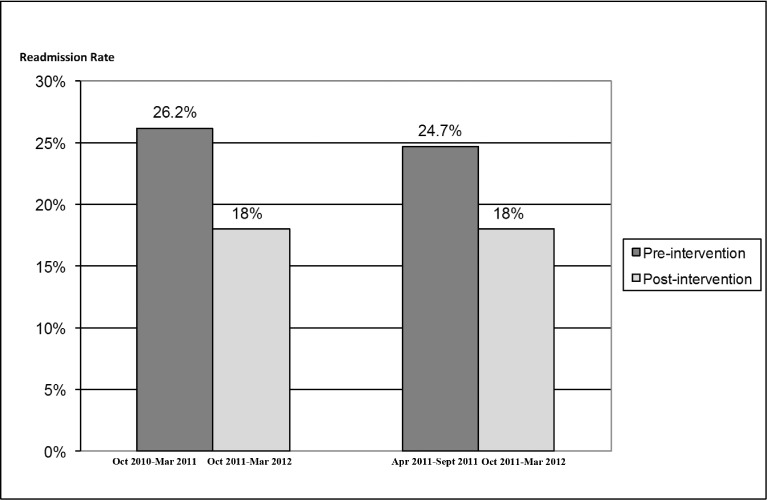
Thirty-day readmission rates: Before and after pharmacy intervention.
A total of 546 pharmacist-identified medication interventions were performed during the study period. Of these interventions, 57% (n = 314) identified chronic medications being omitted on admission or discharge, 29% (n = 157) were making a formulary substitution on admission but not switching back to original agent upon patient discharge, 8% (n = 44) were related to medications with the wrong dose or frequency, and 6% (n = 31) of interventions were classified as others. Although many medication discrepancies do not lead to serious harm, it is postulated that a portion could have led to significant clinical consequences.
The MRTs spent an average of 23.7 minutes per patient. The majority of this time was spent obtaining the medication history from the patient or his/her family (12.2 minutes or 51%). Verifying medication lists with outpatient pharmacies, physicians' offices, or insurance companies required an additional 7.1 minutes (30%). They spent an average of 4.4 minutes (19%) on initial medication reconciliation and reporting to pharmacists. On the other hand, pharmacists spent an average of 28.9 minutes per patient. Pharmacists spent 10.1 minutes (35%) performing medication reconciliation at discharge, 8.8 minutes providing medication education (30%), 6.6 minutes on admission medication reconciliation (23%), and 3.4 minutes (12%) on the postdischarge phone call.
DISCUSSION
Medication errors harm an estimated 1.5 million people each year in the United States, and the majority of these errors occur during times of transition of care.7 Pharmacists are well-suited to detect these errors and to help patients manage drug-related issues during their transitions of care. The current study demonstrates that accurate medication reconciliation and medication education can decrease readmission rate, which could potentially improve patient outcomes. Reduction in readmission rate can also have significant financial implications to the health system.
This study also demonstrates the feasibility of incorporating pharmacy technicians in the medication reconciliation process. Expanding technicians' role to include the initial phase of medication reconciliation will free up clinical pharmacist time for other direct patient care activities. We felt that previous pharmacy retail experience and a formal training program were essential to the success in this new pharmacy technician role. Technicians with a background in retail pharmacy are more familiar with outpatient medication names, tablet strengths, and tablet characteristics, such as color and shape, than technicians who have a background in hospital pharmacy. We also felt that they possessed more customer service experience due to the multiple patient interactions in the retail setting. We believe this helped them be successful during patient interviews. The MRT training program consisted of reviewing the brand and generic names and indications of the top 100 outpatient medications prescribed at our institution, interview technique strategies, and shadowing of pharmacists.
The vast majority of hospital readmissions in this study (73%) were related to the index admission. We did not observe any correlation between discharge diagnosis, discharge disposition, or third-party payers and risk for readmission. On the other hand, and consistent with previous findings at our institution, previous readmission within 90 days remains the strongest predictor of future readmissions. Pharmacists and health systems should evaluate their internal data to identify readmission risk factors unique to their local environment and practice setting to determine how to best implement medication reconciliation programs.
Postdischarge phone calls have been previously identified as a key factor in reducing medication-related adverse events after discharge.8 The impact of the follow-up phone calls was not evaluated in the current study, as we did not design it to look at individual components of the intervention.
There were several limitations to the study. Only 67% of eligible patients received the pharmacy intervention mostly due to weekend discharges and short stay admissions. We were able to address this problem by utilizing pharmacy residents on weekends with great success. However, it is still unclear whether any bias was introduced by our inability to reach all eligible patients.
In addition, the control group in this study consists of historical data from 2 different time periods, which may have introduced several biases because patients were neither matched nor prospectively randomized. However, there was no change in the medical teams or admitting policies in all 3 time periods, making significant differences in patients' acuity or diagnoses unlikely.
CONCLUSIONS
Pharmacy-facilitated medication reconciliation and patient education of medicine patients decreased 30-day readmission rates.
ACKNOWLEDGMENTS
None of the authors have any conflicts of interest to report.
Footnotes
Clinical Pharmacist, General Medicine
Clinical Pharmacist, MICU
Pharmacy Manager, Patient Quality Outcomes
Pharmacy Manager, Oncology
Executive Director, Pharmacy Services, Yale-New Haven Hospital, New Haven, Connecticut.
REFERENCES
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2. Public Law 111-148. Patient Protection and Affordable Care Act. March 23, 2010.
- 3.Gillespie U, Alassaad A, Henrohn D et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: A randomized controlled trial. Arch Intern Med. 2009;169:894–900. doi: 10.1001/archinternmed.2009.71. [DOI] [PubMed] [Google Scholar]
- 4.Crotty M, Rowett D, Spurling L et al. Does the addition of a pharmacist transition coordinator improve evidence-based medication management and health outcomes in older adults moving from the hospital to a long-term care facility? Results of a randomized, controlled trial. Am J Geriatr Pharmacother. 2004;2:257–264. doi: 10.1016/j.amjopharm.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 5.The consensus of the Pharmacy Practice Model Summit. Am J Health Syst Pharm. 2011;68:1148–1152. doi: 10.2146/ajhp110060. [DOI] [PubMed] [Google Scholar]
- 6.Sample script for follow-up phone call: Project RED (Re-Engineered Discharge) training program. Rockville, MD: Agency for Healthcare Research and Quality; August 2011. http://archive.ahrq.gov/professionals/systems/hospital/red/callscript.html. [Google Scholar]
- 7.Aspden P, Institute of Medicine, Committee on Identifying and Preventing Medication Errors Preventing Medication Errors. Washington DC: National Academies Press; 2006. [Google Scholar]
- 8.Jack BW, Chetty VK, Anthony D et al. A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Ann Intern Med. 2009;150:178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]


