Abstract
Background
Slum dwellers have poor socio-environmental conditions and less access to medical care, which make them susceptible to illnesses. Studies on urban slums have primarily focused on communicable diseases and less on lifestyle diseases, such as hypertension. Consequently, there is a paucity of prevalence studies of hypertension in slums in different parts of the country. The aim of the study was to provide estimates of the prevalence, awareness, and control of hypertension in an adult population sample of the slums of Kolkata.
Methods
A population-based cross-sectional study was conducted in the slums of Kolkata in collaboration with Kolkata Municipality Corporation. Door-to-door survey was conducted by trained healthcare workers using a structured questionnaire. Age, sex, religion, housing conditions (house/hut), average monthly household income, education status, current use of tobacco, history of hypertension, and whether on antihypertensive treatment were recorded. Blood pressure (BP) was recorded as per standard guidelines. Hypertension was diagnosed by JNC-VII criteria. A total of 10,175 adults aged ≥20 years were enrolled in the study.
Results
Overall prevalence of hypertension was 42%. Hypertension was newly detected in 19% of the population. Fifty-four percent of the hypertensive subjects were aware of their hypertension status, 38% were on antihypertensive treatment, and 12% had their BP controlled to target level. Subgroup analysis showed that the prevalence of hypertension was higher in men, above 60 years age, in the minority community, in those with a higher household income, and among the tobacco users.
Conclusion
There is a high prevalence of hypertension in the slums of Kolkata. Although the awareness of the condition is high, the control of hypertension is poor.
Keywords: Hypertension, Slums, Kolkata, Kolkata Municipal Corporation
1. Introduction
Hypertension is an important public health problem. Worldwide, more than one billion adults have hypertension and this is predicted to increase to 1.56 billion by 2025.1 Those with hypertension have higher risk of coronary artery disease, heart failure, and stroke. Hypertension accounts for 57% of all deaths from stroke and 24% of all deaths from coronary heart disease in India.2
Although the prevalence of hypertension has remained stable or has decreased in economically developed countries, it has increased in developing countries including India.3, 4 Existing data show that even within our country, the prevalence of hypertension varies considerably from one region to another, and between rural and urban populations.2 Over a period of 55 years, there has been a 10-fold increase in prevalence in the rural population, but in the urban population, the increase is almost 30 times.5 Various factors, such as diet, change in lifestyle, stress, and paucity of employment might have contributed to this rising trend.6
A considerable proportion of the urban population in India lives in slums, which are characterized by poor socioenvironmental conditions and poverty. Slum dwellers tend to neglect the importance of health and social advancement, which make them more prone to lifestyle diseases. Lack of regular employment, threat of eviction, overcrowding, alcoholism, and other social issues contribute to poor health in the slums and make the provision of health services in these areas more difficult. The growth rate of the slum population in India has been much higher than the growth rate of the nonslum population.7
Field-based studies on the prevalence of hypertension in different regions of India are still scarce.8 Moreover, research in the urban slums has primarily focused on child health, and reproductive and communicable diseases.9 Only a few reports are available on the prevalence of lifestyle diseases, such as hypertension, in the slums.
For planning effective strategies for preventing and controlling hypertension among the slum dwellers, the magnitude of the problem needs to be determined.
The aim of the study was to provide estimates of the prevalence, awareness, and control of hypertension in a population sample of the slums of Kolkata.
2. Methods
The study was approved by the local Institutional ethics committee and informed verbal consent was obtained from all participants.
2.1. Sampling site
This was a population-based cross-sectional study conducted in the slums of Kolkata in collaboration with Kolkata Municipality Corporation (KMC). Kolkata is the cosmopolitan capital of West Bengal, located in eastern part of India. It has an approximate resident population of 4.5 million (Census 2011), of which about 1.49 million reside in slums (about one-third of the total population). Kolkata municipality is divided into fifteen boroughs, each borough comprising of several wards. One of the boroughs (Number III) was selected by simple random sampling. Borough III comprises of 9 wards with a population of 401,332, of which about 44.3% are slum dwellers.10
2.2. Methodology
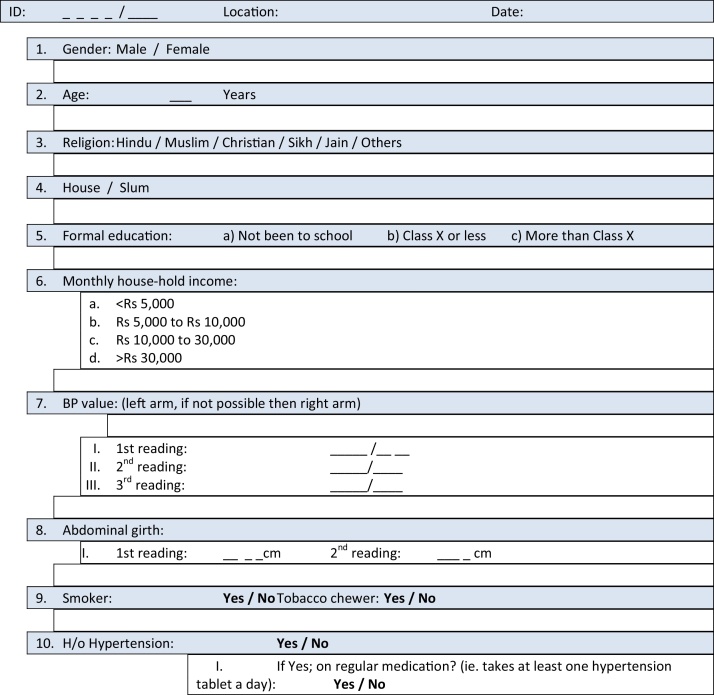
Ten healthcare workers who work in the slums of borough III were given adequate training in blood pressure (BP) measurement by a team of doctors. Door-to-door survey was conducted by these healthcare workers in their respective wards, under the supervision of the team of doctors. All slum residents aged 20 years or more, who were present on the days of the survey and were willing to participate, were included in the study. We planned to interview about 10,000 subjects. In each ward, the first household was randomly selected and then all contiguous households were selected until the target number was reached. A standard structured questionnaire (Fig. 1) was prepared, which comprised of demographics, such as age, sex, religion, housing condition (house/hut), average monthly household income, and education status. History of hypertension and whether on antihypertensive treatment were also noted.
Fig. 1.
Structured questionnaire used for survey.
BP was recorded as per the 2013 ESH/ESC Guidelines for the management of arterial hypertension.11 Korotkoff phase V was taken as the diastolic pressure. Sitting BP was measured by using carefully calibrated hand-held aneroid sphygmomanometers at least twice at 2 min intervals. At the discretion of the surveyor, a third recording was allowed.
2.3. Definitions and diagnostic criteria
Hypertension was defined as per JNC-VII guidelines as systolic blood pressure (SBP) greater or equal to 140 mmHg and/or diastolic blood pressure (DBP) greater or equal to 90 mmHg. The average of two or three readings was taken as the BP value.12
Isolated systolic hypertension was defined as SBP ≥ 140 and DBP < 90 mmHg, and isolated diastolic hypertension as DBP ≥ 90 and SBP < 140 mmHg.
Those who reported that a doctor or a health worker ever told them they had hypertension or those who were already on antihypertensive medications were recorded as ‘known hypertensive’.
Awareness was defined as proportion of persons with known hypertension divided by all hypertension patients (known and newly diagnosed).
Subjects were recorded as on antihypertensive treatment if they confirmed that they were taking at least one antihypertensive medicine every day. Subjects on treatment were expressed as proportion of patients with hypertension on drug treatment divided by all hypertension patients (known and newly diagnosed).
Control of hypertension was defined as hypertensive patients with SBP and DBP less than 140 and 90 mm of Hg, respectively. It was expressed as proportion of patients with BP <140 and <90 mmHg divided by all hypertension patients (known and newly diagnosed).
Slum is described as “residential areas where dwellings are unfit for human habitation” because they are dilapidated, overcrowded, poorly ventilated, unclean, with faulty design of buildings, narrowness of streets, or “any combination of these factors which are detrimental to the safety and health” (Indian Slum Act, 1956). In our study, slum was defined by the criteria set by The Census of India (2001).13 A list of registered slums in borough III was made available by KMC.
For the purpose of defining the housing condition, all dwellings were classified as either houses or huts. A dwelling where the roof was made of concrete was considered as ‘house’. A dwelling where the roof was made with any material other than concrete (such as tiles, wood, bamboo, mud, plastic) was considered as ‘hut’.
As per the level of education, the population was divided into three groups: those who had never been to school; those who went to school but not beyond Class X (the 10th Standard); those who have studied beyond Class X.
The income level was defined by the monthly household income. The population was divided into four categories: those with a monthly household income of INR less than 5000 (about <$81); those with income between INR 5000 to 10,000 ($81 to $162); INR 10,000 to 30,000 ($162 to $485); and above INR 30,000 ($485).
An attempt was made to measure the abdominal girth, but it was later abandoned because of the reluctance of the male health workers to measure the abdominal girth in female subjects.
Only those who currently smoked or chewed tobacco in any form were recorded as smokers or tobacco chewers, respectively. Collectively, they were referred as tobacco users.
2.4. Statistical analysis
For each individual, SBP and DBP were measured two or three times. Average SBP was calculated by taking the arithmetic average of all SBP measurements and average DBP was calculated by taking the arithmetic average of all DBP measurements. Proportions of hypertensive subjects in the different demographic and economic groups were computed and expressed as percentages. Tests of two proportions and goodness-of-fit χ2 tests have been applied to test if proportions of hypertensive subjects are significantly different in the different groups. Confidence intervals (CIs) were calculated using standard errors of binomial proportions and using the standard normal 97.5 percentile point, the numerical value of which is 1.96. 95% CIs are provided corresponding to all prevalence estimations. All prevalence rates and CIs are presented without any places of decimal to keep numbers simple, easy to remember, and help subsequent comparison.
3. Results
3.1. Subjects
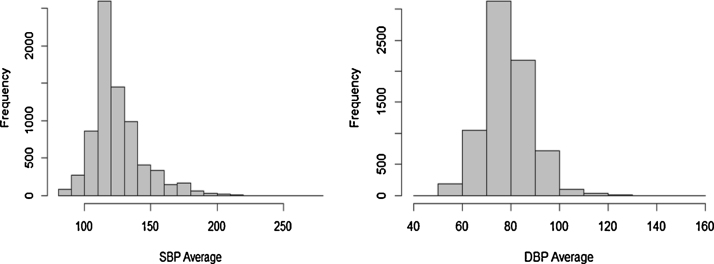
We enrolled 10,175 individuals but analyzable data were available for 10,167 subjects, 4079 males (40.1%) and 6088 females (59.9%). All proportions calculated were based on 10,167 subjects. The characteristics of the population surveyed are given in Table 1. The mean systolic BP of the population was 128 ± 10 (SD) mmHg and mean diastolic BP was 82 ± 10 (SD) mmHg. The 25th percentiles, the 75th percentiles, and the 90th percentiles for systolic BP were 120 mmHg, 139 mmHg, and 153 mmHg, respectively. For diastolic BP, the 25th percentiles, 75th percentiles, and 90th percentiles were, respectively, 77 mmHg, 90 mmHg, and 93 mmHg (Fig. 2).
Table 1.
Sociodemographic characteristics of the study population.
| Categories | Sample size |
|---|---|
| Number (%) | |
| Gender (n = 10,167) | |
| Male | 4079 (40) |
| Female | 6088 (60) |
| Age group (n = 10,167) | |
| 20–40 | 3470 (34) |
| 41–60 | 4698 (46) |
| Above 60 | 1999 (20) |
| Religion (n = 10,167) | |
| Hindu | 9388 (92) |
| Minorities | 779 (8) |
| Dwelling (n = 10,167) | |
| House | 4427 (43) |
| Hut | 5740 (57) |
| Education level (n = 9088) | |
| A: Not been to school | 1529 (17) |
| B: Class X or less | 4820 (53) |
| C: More than Class X | 2739 (30) |
| Monthly household income (n = 9678) | |
| A: <Rs 5000 | 2567 (26) |
| B: Rs 5000–10,000 | 4032 (42) |
| C: Rs 10,000–30,000 | 2703 (28) |
| D: Above Rs 30,000 | 376 (4) |
| Tobacco users: smokers and/or tobacco chewers (n = 10,167) | |
| Yes | 3425 (34) |
| No | 6742 (66) |
Fig. 2.
Histograms for the distribution of SBP and DBP in the study population.
3.2. Prevalence of hypertension
Overall prevalence of hypertension (known and newly detected) in the study population was 42% (4304 out of 10,167). The prevalence was higher in men than in women (men: 47%, women: 39%, p ≤ 0.001). Of the study population, 2340 (23%) were known hypertensive. Hypertension was newly detected in 1964 (19%) subjects during the survey. Out of the total population of hypertensive subjects (4304), 857 (20%) had isolated systolic hypertension, and 1280 (30%) had isolated diastolic hypertension.
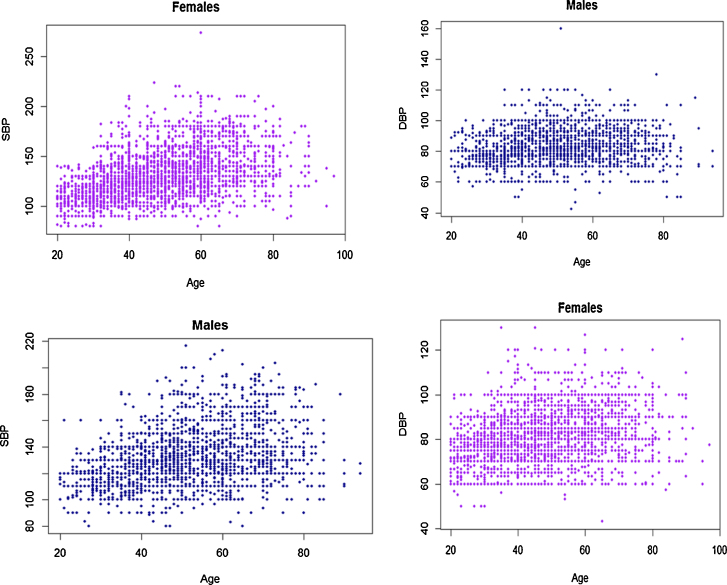
The prevalence of hypertension increased with age. Prevalence was higher in men than in women (men: 47%, women: 39%, p ≤ 0.001). Highest prevalence for men was seen in the seventh decade and for women in the eighth decade (Table 2). Prevalence of hypertension among women was less than that among males till about sixty years of age. Thereafter, it was greater in women than in men. Although the SBP increased with age, no such correlation was evident with DBP, both in men and women (Fig. 3).
Table 2.
Age-related prevalence of hypertension in men and women.
| Age | Males | Hypertensive males | 95% CI (%) | Females | Hypertensive females | 95% CI (%) | All | All hypertensive | 95% CI (%) |
|---|---|---|---|---|---|---|---|---|---|
| Number (%) | Number (%) | Number (%) | |||||||
| 20–30 | 337 | 40 (12) | 8–15 | 826 | 57 (7) | 5–9 | 1163 | 97 (8) | 7–10 |
| 31–40 | 807 | 267 (33) | 30–36 | 1455 | 393 (27) | 25–29 | 2262 | 660 (29) | 27–31 |
| 41–50 | 1130 | 555 (49) | 46–52 | 1468 | 622 (42) | 40–45 | 2598 | 1177 (45) | 43–47 |
| 51–60 | 899 | 493 (55) | 52–58 | 1201 | 637 (53) | 50–56 | 2100 | 1130 (54) | 52–56 |
| 61–70 | 640 | 388 (61) | 57–64 | 798 | 502 (63) | 60–66 | 1438 | 890 (62) | 59–64 |
| 71–80 | 232 | 129 (56) | 49–62 | 244 | 164 (67) | 61–73 | 476 | 293 (62) | 57–66 |
| >80 | 39 | 19 (49) | 33–64 | 46 | 28 (61) | 47–75 | 85 | 47 (55) | 45–66 |
Fig. 3.
Scatter diagram showing relation of SBP and DBP with age in men and women.
The prevalence of hypertension among different categories is given in Table 3. Forty-two percent Hindus and 48% from minority communities had hypertension (p < 0.001). No significant difference in prevalence of hypertension was seen between those residing in house or those in huts (43% huts, 42% house; p = 0.6). The prevalence of hypertension in those who have never been to school, those who have not studied beyond class X, and those who have studied beyond class X were 43%, 42%, and 44%, respectively, which were not statistically significant (p = 0.5%). The prevalence of hypertension increased with monthly household income. It was 35%, 46%, and 51% in those with monthly household income of less than rupees 5000, 5000–30,000, and above 30,000, respectively (p < 0.001). Tobacco users had higher prevalence (56%) of hypertension than nonusers (36%), (p < 0.001).
Table 3.
Prevalence of hypertension among various categories.
| Categories | Sample size | Hypertensive | 95% CI (%) |
|---|---|---|---|
| Number | Number (%) | ||
| Gender | |||
| Male | 4079 | 1900 (47) | 45–48 |
| Female | 6088 | 2404 (39) | 38–41 |
| Religion | |||
| Hindu | 9388 | 3929 (42) | 41–43 |
| Minorities | 779 | 375 (48) | 45–52 |
| Dwelling | |||
| House | 4427 | 1861 (42) | 41–43 |
| Hut | 5740 | 2443 (43) | 41–44 |
| Education level | |||
| A: Not been to school | 1529 | 659 (43) | 41–46 |
| B: Class X or less | 4820 | 2046 (42) | 41–44 |
| C: More than Class X | 2739 | 1198 (44) | 42–46 |
| Income | |||
| A: <Rs 5000 | 2567 | 886 (35) | 33–36 |
| B: Rs 5000–10,000 | 4032 | 1846 (46) | 44–47 |
| C: Rs 10,000–30,000 | 2703 | 1240 (46) | 44–48 |
| D: Above Rs 30,000 | 376 | 193 (51) | 46–56 |
| Tobacco users: smokers and/or tobacco chewers | |||
| Yes | 3425 | 1909 (56) | 54–57 |
| No | 6742 | 2395 (36) | 34–37 |
3.3. Awareness, treatment, and control of hypertension
Of the total hypertensive subjects, 54% (2340 out of 4304) were aware of their condition. In the remaining 46%, hypertension was detected during the survey. Of the total hypertensive subjects, 38% (1648 of 4304) were on antihypertensive treatment and 12% (499 of 4304) had their BP controlled (lowered to less than 140/90 mmHg) (Table 4). Seventy-one percent (1648 of 2340) of hypertensive subjects, who were aware of their hypertensive status, were on treatment. Among those who were on treatment for hypertension, only 26% (426 of 1648) had their BP controlled. Although the prevalence of hypertension was higher in men than women, the awareness, treatment, and control of hypertension was higher in women.
Table 4.
Prevalence, awareness, treatment, and control of hypertension.
| Male |
Female |
Total |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Sample size | Number (%) | 95% CI (%) | Sample size | Number (%) | 95% CI (%) | Sample size | Number (%) | 95% CI (%) | |
| Prevalence | 4079 | 1900 (47) | 45–48 | 6088 | 2404 (39) | 38–41 | 10,167 | 4304(42) | 41–43 |
| Awareness | 1900 | 923 (49) | 46–51 | 2404 | 1417(59) | 57–61 | 4304 | 2340 (54) | 53–56 |
| Treatment | 1900 | 669 (35) | 33–37 | 2404 | 979 (41) | 39–43 | 4304 | 1648 (38) | 37–40 |
| Control | 1900 | 185 (10) | 8–11 | 2404 | 314(13) | 12–14 | 4304 | 499 (12) | 11–13 |
Among known hypertensive subjects whose BP was not controlled to target despite medication, the mean SBP was 147.7 ± 13.4 mmHg, and mean DBP was 91.2 ± 8.3 mmHg; 70% of them were in Stage I and 30% had Stage II hypertension.
4. Discussion
The overall prevalence of hypertension in the slums of Kolkata was 42%. This is higher than the previously reported prevalence of 24.9% in the urban population of the district town of Malda, West Bengal6 based on JNC VII criteria, a study not restricted to slums. Using criteria similar to ours, a recent population-based study in the urban slums of North 24 Parganas district of West Bengal estimated the prevalence of hypertension as 35% among males and 33% among females in the age group of 25–64 years.9 Our study population did not have an upper age limit for enrolment, which may have contributed to the higher prevalence of hypertension in our study. A high prevalence of hypertension among urban adults has also been reported from other parts of India: men 44%, women 45% in Mumbai (1999)14; men 31%, women 36% in Thiruvananthapuram (2000)15; men 36%, women 37% in Jaipur (2002)16; 47% among urban people in Kerala (2009).17 A study conducted on adult outdoor patients of an urban health center in Lucknow district found that 44.4% respondents were hypertensive.18 Comparison of results among these studies is difficult because of different populations, cut-off BP values, and different methodologies used in the studies.9 A lower prevalence was noted in some other studies. Mohan et al. reported a prevalence of 20% amongst the urban population of Chennai.19 The study counted only those who were already on antihypertensive medications and was not restricted to a slum population. Also the cut-off value for hypertension was higher at >140/90 mmHg. The high prevalence of hypertension seen in our study may be due to problems inherent and specific to the slums of Kolkata or may be a reflection of the rising trend of hypertension seen in our country because of rapid urbanization, lifestyle changes, dietary changes and the increased life expectancy,18, 20 or a combination of these factors.
Hypertension was newly detected during the survey in about one-fifth of the population studied. This has important implications for public health measures aimed towards diagnosis and treatment of hypertension. However, there is a difference in measurement methodology of BP in epidemiological studies as compared to clinic-based measurements. It has been reported that epidemiological studies relying on single-session measurements overdiagnose hypertension by 20–25%.21
Our study showed a high level of awareness of the hypertensive status among the study subjects. About 54% of hypertensive subjects were aware of their condition. A high level of awareness has been reported in selected populations, such as from Kerala (44.9% of all hypertensives),22 among Parsis in Mumbai (47% of males and 56% of females were aware of hypertensive status),23 and in Chennai (38.2%).19 Most of the studies, however, have shown a lower level of awareness: 11% male and 16% female hypertensives (Jaipur)24; 18.4% (West Bengal),9 and 21.9% of all hypertensives (Himachal Pradesh).25 This shows that within India there is a wide variation in hypertension awareness. The reasons for the high awareness level observed in our study are not clear. The clinics and the camps conducted by the KMC and the various nongovernment organizations might have helped in the detection of hypertension among the slum dwellers and increased awareness of the condition. It is also possible that self-selection bias could have caused more hypertensive subjects, who are aware of their condition, to have agreed to the study.
Seventy-one percent of those known to have hypertension were on antihypertensive treatment. Similar 73% adherence to medication has been reported in urban slum dwellers in Kolkata.26 Our data are also comparable to the data from Jaipur23 and Chennai19, where respectively, 61% and 70.8% of those who were aware of their hypertensive status were on antihypertensive treatment. These figures are high compared to the study in a rural community of Himachal Pradesh, where 47% of known hypertensive subjects were on antihypertensive medications.24
Overall control of hypertension was poor (12%). Among those who were on treatment, only a quarter (26%) had their BP controlled to the target level (<140/90 mmHg). This is lower than what is reported in other studies. The corresponding figures from Chennai,19 Himachal Pradesh,24 and Kerala27 are 45.9%, 42.9%, and 32.1%, respectively. The poor control of BP noted in our study, despite a large proportion of patients being on antihypertensive medications, needs explanation. Probably once medications were initiated, no further follow-ups were done. This notion is supported by the findings from Dakar, Senegal,28 which have shown that the control of BP was related to the frequency of follow-up visits. Partial adherence to prescribed medications is another possibility, as in our study, a subject was considered to be on treatment even if he took only one of all the prescribed medicines.
Wide variations in hypertension prevalence, awareness, treatment, and control have been reported from other developing countries. The overall prevalence of hypertension was 42% in the Federation of Bosnia and Herzegovina.29 Ongeti et al.30 reported 13% prevalence of hypertension in the slums of Kenya. Thirteen percent of these hypertensive subjects knew that they have hypertension and 10% of them were on treatment. The prevalence of hypertension in Astana, Kazakhstan31 was 70%. Among them, 91% were aware of their condition, 77% took antihypertensive medications, and 34% had BP controlled (<140/90 mmHg). Prevalence of hypertension was 65.4% among urban population aged 50 years or older in Senegal, sub-Saharan Africa.28 Half of these hypertensive subjects were aware of their problem and among the latter, 70% were on treatment. However, of these, only 17% had controlled BP.
Traditionally men are thought to have a higher prevalence of hypertension than women, which was also the finding in our study. Similar observations were noted from Chennai19 (men: 23.2%, women: 17.1%), slums of North 24 Parganas district of West Bengal (35% males and 33% females),9 and Himachal Pradesh24 (39.8% in males and 33.15% in females). Some other studies, however, reported a higher prevalence of hypertension in females; 33% women vs 30% males in Jaipur23; and 44% males vs 45% females in Mumbai.14
A significant correlation of age with increasing BP was seen only for SBP, both in men and women. The prevalence of hypertension steadily increased with age. The higher prevalence of hypertension in males was seen up to the sixth decade; thereafter, the prevalence was higher in females. This is contrary to what has been previously reported from West Bengal, where above the age of 60 years, men were more hypertensive than women.32
A higher prevalence of hypertension was seen among the minority communities compared to the Hindus. A similar but nonsignificant trend was seen among adult patients attending out-patient clinic in Lucknow (44.7% of Muslims vs 43% of Hindus).18
There was no significant difference between the prevalence of hypertension in slum dwellers residing in houses and those residing in huts (42% vs 43%, respectively). This is understandable, as perhaps the environment of the slum has a greater impact on health than the type of dwelling.
Conventional wisdom suggests that higher education is associated with greater awareness, which have positive impact on prevalence of lifestyle diseases. Among the rural population of Spiti Valley in Himalayas, Negi et al.33 found that the education level had inverse association with prevalence of hypertension. In our study, the prevalence of hypertension was not related to the level of education. Living in a slum probably attenuated the greater awareness that comes with education. The other possibility is that higher education was perhaps associated with higher incomes and a consequent poorer lifestyle leading to the annulment of the benefits of education. A study conducted in the rural community of West Bengal showed only weak association between the level of education and BP.34 No significant relationship with literacy was seen in a study from Jaipur.23
Our study showed that the prevalence of hypertension increased with monthly household income. Affluence has been shown to be associated with unhealthy diet, obesity, and sedentary habits, which may contribute to hypertension. By taking into account education, occupation, and income, and using modified Kuppuswamy's classification,35 Wasir et al.36 showed that prevalence of hypertension varied directly with socioeconomic status (7.1%, 6.3%, and 5.1% of the upper, middle, and lower socioeconomic status, respectively were hypertensive). Higher prevalence of hypertension among the upper socioeconomic status has also been reported from Rohtak.37 According to the WHO, societies that are in the transitional stages of economic and epidemiological changes have higher prevalence of hypertension among the upper socioeconomic groups.18
The prevalence of tobacco users in our country varies widely from 16% in Kerala to 68% in Mizoram.38 In our study, one-third of the population were current tobacco users and a significantly high prevalence of hypertension was noted among them compared to the nonusers. Direct relation of chronic tobacco consumption with hypertension however is not yet well established,39, 40 although tobacco consumption has been shown to cause an acute elevation of BP.41
5. Limitations of the study
The study has several limitations. Firstly, we assumed that the slums of borough III are representative of the slums of Kolkata, although we have scarce data to substantiate the assumption. Secondly, random sampling of the study population was not done. Only those members of a family were interviewed who were present at that point of time. This may explain the higher number of females in the study. Thirdly, the measure of prevalence of hypertension was based on the measurements of BP on a single day. The possibility of white-coat hypertension in some of these subjects could not be excluded. No attempt was made to assess target organ damage. Fourthly, it is difficult to exclude the possibility of bias in self-reporting. Some of the participants may not have revealed their actual income status. Moreover, no age verification was done for practical reasons. Also, due to the one-off questionnaire nature of the study, and the nature of the population studied, compliance to medications was difficult to ascertain. It was felt that a compliance question in the questionnaire would not be reliably answered. Finally, a lack of information on co-morbidities, such as diabetes, obesity, renal disease, and of lifestyle factors, such as diet and physical activities, limited further interpretation of the data.
6. Conclusion
Our study showed that there is a high prevalence of hypertension in the slums of urban Kolkata. However, more than half of the hypertensive population was aware of their condition and about three-fourth of those who were aware were on antihypertensive medications. Unfortunately, only a quarter of those on antihypertensive medications had their BP controlled to target, implying a high risk of hypertension-related complications and a future major impact on local healthcare resources. There is a need to develop population-based hypertension detection and control strategies incorporating the slums. These could include free hypertension clinics focused on the slum population, enhanced education on the adverse outcomes of hypertension, and encouragement of medical follow-up for monitoring of BP in those who are already diagnosed with hypertension.
Conflicts of interest
The authors have none to declare.
Acknowledgements
The study has been supported by the Department of Clinical Trials and Research, Apollo Gleneagles Hospital, Kolkata and Kolkata Municipal Corporation (IEC/2013/1/06).
References
- 1.Kearney P.M., Whelton M., Reynolds K., Muntner P., Whelton P.K., He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–78. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 3.Kearney P.M., Whelton M., Reynolds K., Whelton P.K., He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22:11–19. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Hypertension Study Group Prevalence, awareness, treatment and control of hypertension among the elderly in Bangladesh and India: a multicentre study. Bull World Health Organ. 2001;79:490–500. [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta R. Meta analysis of prevalence of hypertension in India. Indian Heart J. 1997;49:43–44. [PubMed] [Google Scholar]
- 6.Das S.K., Sanyal K., Basu A. Study of urban community survey in India: growing trend of high prevalence of hypertension in a developing country. Int J Med Sci. 2005;2:70–78. doi: 10.7150/ijms.2.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta K., Arnold F., Lhungdim H. International Institute for Population Sciences; Mumbai, Calverton, Maryland, USA: 2009. Health and Living Conditions in Eight Indian Cities. National Family Health Survey (NFHS-3), India, 2005–06. [Google Scholar]
- 8.Todkar S.S., Gujarathi V.V., Tapare V.S. Period prevalence and sociodemographic factors of hypertension in rural Maharashtra: a cross-sectional study. Indian J Community Med. 2009;34:183–187. doi: 10.4103/0970-0218.55269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acharyya T., Kaur P., Murhekar M.V. Non communicable disease risk factors in urban slum. Indian J Public Health. 2014;58:1–4. doi: 10.4103/0019-557X.138632. [DOI] [PubMed] [Google Scholar]
- 10.Census of India . Series 30. Director of Census Operation; West Bengal, Kolkata: 2011. pp. 245–256. (Provisional Population Totals, West Bengal). [Google Scholar]
- 11.Giuseppe Mancia G., Fagard R., Narkiewicz K. 2013 ESH/ESC Guidelines for the management of arterial hypertension. J Hypertens. 2013;31:1281–1357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 12.Chobanian A.V., Bakris G.L., Black H.R. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC-7) JAMA. 2003;289:2560–2571. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 13.Census of India . Series 20. Director of Census Operation; West Bengal, Kolkata: 2001. pp. 202–308. (Provisional Population Totals, West Bengal). [Google Scholar]
- 14.Gupta P.C., Gupta R. Hypertension prevalence and blood pressure trends among 99,589 subjects in Mumbai, India. Indian Heart J. 1999;51:691. [Abstract] [Google Scholar]
- 15.Joseph A., Kutty V.R., Soman C.R. High risk for coronary heart disease in Thiruvananthapuram city: a study of serum lipids and other risk factors. Indian Heart J. 2000;52:29–35. [PubMed] [Google Scholar]
- 16.Gupta R. Prevalence of coronary heart disease and risk factors in an urban Indian population: Jaipur Heart Watch-2. Indian Heart J. 2002;54:59–66. [PubMed] [Google Scholar]
- 17.Vimala A., Ranji S.A., Thodi J.M. The prevalence risk factors and awareness of hypertension in an urban population of Kerala (South India) Saudi J Kidney Dis Transpl. 2009;20:685–689. [PubMed] [Google Scholar]
- 18.Mahmood S.E., Prakash D., Srivastava J.P. Prevalence of hypertension amongst adult patients attending Out Patient Department of Urban Health Training Centre, Department of Community Medicine, Era's Lucknow Medical College and Hospital, Lucknow. J Clin Diagn Res. 2013;4:652–656. doi: 10.7860/JCDR/2013/4707.2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohan V., Deepa M., Farooq S. Prevalence, awareness and control of hypertension in Chennai – The Chennai Urban Rural Epidemiology Study (CURES – 52) J Assoc Phys Ind. 2007;55:326–332. [PubMed] [Google Scholar]
- 20.Gupta R., Al-Odat N.A., Gupta V.P. Hypertension epidemiology in India: meta-analysis of fifty year prevalence rates and blood pressure trends. J Hum Hypertens. 1996;10:465–472. [PubMed] [Google Scholar]
- 21.Anand M.P. Prevalence of hypertension amongst Mumbai executives. J Assoc Phys Ind. 2000;48:1200–1201. [PubMed] [Google Scholar]
- 22.Kalavathy M.C., Thankappan K.R., Sarma P.S. Prevalence, awareness, treatment and control of hypertension in an elderly community-based sample in Kerala, India. Natl Med J India. 2000;13:9–15. [PubMed] [Google Scholar]
- 23.Bharucha N.E., Kuruvilla T. Hypertension in the Parsi community of Bombay: a study on prevalence, awareness and compliance to treatment. BMC Public Health. 2003;3:1–5. doi: 10.1186/1471-2458-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta R., Guptha S., Gupta V.P. Prevalence and determinants of hypertension in the urban population of Jaipur in western India. J Hypertens. 1995;13:1193–1200. doi: 10.1097/00004872-199510000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Bhardwaj R., Kandoria A., Marwah R. Prevalence, awareness and control of hypertension in rural communities of Himachal Pradesh. J Assoc Phys Ind. 2010;58 [PubMed] [Google Scholar]
- 26.Subhasis B., Sarma P.S. Adherence to antihypertensive treatment and its determinants among urban slum dwellers in Kolkata, India. Asia Pac J Public Health. 2011 doi: 10.1177/1010539511423568. http://aph.sagepub.com/content/early/.Abstract [DOI] [PubMed] [Google Scholar]
- 27.Thankappan K.R., Shah B., Mathur P. Risk factor profile for chronic non-communicable diseases: results of a community-based study in Kerala, India. Indian J Med Res. 2010;131:53–63. [PubMed] [Google Scholar]
- 28.Macia E., Duboz P., Gueye L. Prevalence, awareness, treatment and control of hypertension among adults 50 years and older in Dakar, Senegal. Cardiovasc J Afr. 2012;23:265–269. doi: 10.5830/CVJA-2011-039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pilav A., Doder V., Branković S. Awareness, treatment, and control of hypertension among adult population in the Federation of Bosnia and Herzegovina over the past decade. J Public Health Res. 2014;3:146–151. doi: 10.4081/jphr.2014.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ongeti K.W., Ogeng’o J.A., Pulei A.N. Blood pressure characteristics among slum dwellers in Kenya. Glob Adv Res J Microbiol. 2013;2:080–085. [Google Scholar]
- 31.Supiyev A., Kossumov A., Utepova L. Prevalence, awareness, treatment and control of arterial hypertension in Astana, Kazakhstan. A cross-sectional study. Public Health. 2015 doi: 10.1016/j.puhe.2015.02.020. [DOI] [PubMed] [Google Scholar]
- 32.Mandal P.K., Sinha Roy A.K., Chatterjee C. Burden of hypertension and its risk factors in an urban community of India: are we aware and concerned? Sudanese J Public Health. 2010;5:130–135. [Google Scholar]
- 33.Negi P.C., Bhardwaj R., Kandoria A. Epidemiological study of hypertension in natives of Spiti Valley in Himalayas and impact of hypobaric hypoxemia; a cross-sectional study. J Assoc Phys Ind. 2012;60 [PubMed] [Google Scholar]
- 34.Sadhukhan S.K., Dan A. Multifactorial analysis of blood pressure variations in a rural community of West Bengal. Indian J Community Med. 2005;30:4–6. [Google Scholar]
- 35.Kuppuswamy: In: Economic Classification, Modified: Textbook of Preventive and Social Medicine. Park J.E., Park K., editors. Messrs Banarsidas Bhanot; Jabalpur: 1979. p. 81. [Google Scholar]
- 36.Wasir H.S., Ramachandran P., Nath L.M. Prevalence of hypertension in a closed urban community. Indian Heart J. 1984;36:250–253. [PubMed] [Google Scholar]
- 37.Gupta S.P., Siwach S.B., Moda C.K. Epidemiology of hypertension based on total community survey in an urban population (Rohtak) Indian Heart J. 1978;30:315. [PubMed] [Google Scholar]
- 38.National Institute of Medical Statistics, Indian Council of Medical Research (ICMR), 2009, IDSP Non-Communicable Disease Risk Factors Survey, Phase-I States of India, 2007–08.
- 39.Primatesta P., Falaschetti E., Gupta S. Association between smoking and blood pressure: evidence from the Health Survey for England. Hypertension. 2001;37:187–193. doi: 10.1161/01.hyp.37.2.187. [DOI] [PubMed] [Google Scholar]
- 40.Abtahi F., Kianpour Z., Zibaeenezhad M.J. Correlation between cigarette smoking and blood pressure and pulse pressure among teachers residing in Shiraz, Southern Iran. Iran Cardiovasc Res J. 2011;5:97–102. [Google Scholar]
- 41.Westman E.C. Does smokeless tobacco cause hypertension? South Med J. 1995;88:716–720. doi: 10.1097/00007611-199507000-00004. [DOI] [PubMed] [Google Scholar]