Abstract
Background
Although infectious diseases (IDs) remain a major public health problem in U.S. children, there have been no recent efforts to examine comprehensively the change in epidemiology of ID hospitalizations.
Methods
A serial cross-sectional analysis using the Kids’ Inpatient Database 2000, 2003, 2006, 2009, and 2012. We identified children ≤19 years of age with a primary diagnosis of IDs. Outcomes were national rate of ID hospitalizations, in-hospital mortality, length-of-stay and hospitalization-related direct costs. Negative binomial and multivariable logistic models were constructed to test the change in hospitalization rate and in-hospital mortality, respectively.
Results
We identified 3,691,672 weighted hospitalizations for IDs, accounting for 24.5% of all pediatric hospitalizations. From 2000 to 2012, the rate of overall ID hospitalizations decreased from 91.0 to 75.8 per 10,000 U.S. children (P<0.001). The most frequently listed ID subgroup was lower respiratory infections (42.8% of all ID hospitalizations in 2012). Although the hospitalization rate for most ID subgroups decreased, the hospitalization rate for skin infections significantly increased (67.6% increase; P<0.001). The multivariable model demonstrated a significant decline in in-hospital mortality (OR for comparison of 2012 with 2000, 0.63; 95%CI, 0.51–0.79). From 2000 to 2012, there was no significant change in the median length-of-stay (2 days in 2000 to 2 days in 2012; Ptrend=0.33). The median direct cost for ID hospitalization increased from $3,452 in 2003 to $3,784 in 2012 (P=0.007), with the nationwide direct cost of $4.4 billion in 2012.
Conclusions
We found a statistically significant decline in overall ID hospitalization rate among U.S. children from 2000 to 2012, whereas skin infections statistically significantly increased. Additionally, the median direct cost per ID hospitalization increased by 10% during the study period.
Keywords: Trend, infectious disease, hospitalization, mortality, cost
INTRODUCTION
Infectious diseases (IDs) are a major cause of morbidity and mortality in the U.S.1, 2 The national estimates indicated that 7.4 million children were hospitalized for IDs from 1997 to 2006.3 In 2003, approximately 300,000 infants were hospitalized for IDs, accounting for 43% of all infant hospitalizations with the total annual direct costs of $690 million.4 In this context, the federal government identified a reduction of ID-related hospitalizations as one of the objectives in Healthy People 2020 through better prevention, surveillance, and treatment.5 To develop and implement these strategies nationally, quantifying and characterizing ID hospitalizations is critical.
To date, most epidemiologic research on IDs have largely focused on specific diseases. Along with the efforts to reduce the burden of IDs, there are many success stories in the field of childhood vaccinations (e.g., pneumonia,6, 7 bacterial meningitis,8, 9 and rotavirus-associated illness10, 11). However, focusing solely on specific IDs provides an incomplete picture of the ID-related public health burden – emerging and re-emerging IDs, as represented by IDs with antimicrobial resistant organisms,12, 13 have threatened the public health. Despite the Healthy People 2020 objective identified by the federal government, there have been no recent studies that comprehensively examine the epidemiology and healthcare utilization of ID hospitalization in U.S. children.
To address the gap in the current literature, we used a nationally-representative database to investigate the change in the rate of ID hospitalizations, in-hospital mortality, and related cost among U.S. children from 2000 through 2012.
METHODS
Study Design and Settings
This is a serial cross-sectional analysis of pediatric hospitalizations in 2000, 2003, 2006, 2009 and 2012 by using the Healthcare Cost and Utilization Project’s (HCUP) Kids’ Inpatient Database (KID). The KID is designed to report hospitalizations and outcomes for children every three years and is the only all-payer inpatient care database for children in the U.S.14 The KID is a stratified sample of all pediatric discharges from states that participate in HCUP. Participating states provide discharge-level data on all inpatient discharges from all “community” hospitals (i.e., non-federal, short-term, general, and specialty hospitals) in that state. KID contains a 10% stratified sample of uncomplicated in-hospital births and an 80% stratified sample of other pediatric cases. In 2012, the KID contained 3.2 million records of pediatric discharges from approximately 4,200 hospitals across 44 states, corresponding to a weighted estimate of 6.7 million pediatric discharges in the U.S.15 Additional information of the KID can be found elsewhere.14 The institutional review board of Massachusetts General Hospital approved this analysis.
Study Population
We identified ID hospitalizations in children aged ≤19 years who had an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for an ID in the primary diagnosis field (i.e., the first listed diagnosis on the record). We defined IDs by using a previously described classification scheme for ICD-9-CM codes.3, 16 We have used only the primary diagnosis to minimize the misclassification from hospitalizations for non-ID conditions and to maintain the consistency of case identification with those already in the literature.3, 4
In addition to the overall ID hospitalizations, we also examined 21 mutually exclusive ID subgroups (data available upon request). The following ID subgroups were used for subgroup-specific analyses: viral central nervous system infections; meningitis due to non-viral organisms; acute otitis media; upper respiratory infections; lower respiratory infections (including pneumonia [ICD-9-CM codes, 486] and bronchiolitis [ICD-9-CM code, 466]); infections of heart; enteric infections; abdominal and rectal infections; hepatobiliary infections; urinary tract infections; infections of female pelvic organs; infections involving bone; skin infections (including soft tissue infections); mycoses; septicemia; HIV/AIDS; tuberculosis; infections due to internal prosthetic device, implant, and graft; postoperative infections; perinatal infections; and viral infections, not otherwise specified.
Patient and Hospital Characteristics
The KID contains information on patient characteristics, including age, sex, race/ethnicity, primary insurance type, diagnoses, hospital disposition, and charges for hospital services. Primary insurance types were categorized into public (Medicare and Medicaid), private, self-pay, and others. Hospital characteristics include geographic region, urban-rural status, teaching status, and designation as a children’s hospital. Geographic regions (North, East, South, Midwest, and West) were defined according to Census Bureau boundaries.17 Urban–rural status of the hospital was defined according to the Urban Influence Codes.18 Children’s hospital designation was determined from the National Association of Children’s Hospitals and Related Institutions classification criteria: non–children’s hospital and children’s hospital (children’s general hospital, children’s specialty hospital, and children’s unit in general hospital).19
Outcomes Measures
The primary outcome was the rate of ID hospitalization (overall and ID subgroups). Because the KID database does not contain unique patient identifiers, the rate was estimated as the weighted number of ID hospitalizations per 100,000 U.S. children. Denominators were the population estimates obtained from the U.S. Census Bureau.20 Records for ID hospitalization were examined by age group (i.e., age <1 year, 1–4 years, and 5–19 years), according to the prior literature.3, 16
Other outcomes of interest were in-hospital mortality, length of stay (LOS), and direct cost for the hospital services. In-hospital mortality was defined as the number of inpatient any-cause deaths divided by total number of ID hospitalizations. Direct medical cost was calculated by using hospital-specific cost-charge ratios for 2003, 2006, 2009, and 2012 hospitalizations; cost data were not available in 2000. Cost information was obtained from the hospital accounting reports collected by the Centers for Medicare and Medicaid Services.21 Additionally, cases without hospital-specific cost-charge ratios were excluded, and data were reweighted to analyze cost according to the HCUP recommendations.14
Statistical Analysis
SAS-callable SUDAAN, version 11.0 (Research Triangle Institute, Research Triangle Park, NC) was used to obtain proper variance estimations that accounted for the complex sampling design. If the number of unweighted observations in a stratum was ≤10, the national estimates were considered to be unreliable and were not presented according to the HCUP recommendations.14 Two-sided P<0.05 was considered statistically significant; all data were reported with 95% confidence intervals (CIs).
To investigate the trends in ID hospitalization rates from 2000 to 2012, we constructed negative binominal regression models adjusting for seasonal variation by including the indicator variables for calendar months in addition to calendar years as the independent variables. Negative binomial regression was used to address statistical overdispersion. We reweighted our sample to account for the missingness on hospitalization month data based on the hospitalization year data under the assumption that values were missing at random (<1% of the data of hospitalization month were missing in 2012). We also estimated the number of U.S. population for each month by fitting polynomial (cubic) regression models to the annual population data because monthly population census was not available. In the sensitivity analysis, we fitted ordinary least squares (OLS) model with heteroscedasticity-robust standard errors.22, 23 Analyses for the trends in hospitalization rates were performed with Stata software version 12.1 (StataCorp, College Station, Texas, USA).
To test the change in in-hospital mortality, we fitted two logistic regression models. First, we developed an unadjusted model that included only calendar year as the independent categorical variable. Second, to examine the independent association of calendar year with in-hospital mortality, we constructed multivariable model, adjusting for both patient-level characteristics (i.e., age, sex, race/ethnicity, primary payer) and hospital-level characteristics (region, urban and rural distinction, hospital teaching status, and children’s hospital designation). To test the trend in LOS and direct cost, we fitted unadjusted linear regression model. Because LOS and hospital cost were not normally distributed, we used log-transformed LOS and cost. To facilitate direct comparisons between years, we converted all cost to 2012 U.S. dollars by using the medical care component of the Consumer Price Index.24
RESULTS
We identified 2,278,638 hospitalizations for IDs among U.S. children, corresponding to a weighted estimate of 3,691,672 hospitalizations in the 5 datasets (2000, 2003, 2006, 2009, and 2012; Table 1). This accounted for 24.5% of all hospitalizations being made by U.S. children. The patient and hospital characteristics of children hospitalized for ID are shown in Table 1. Children with ID hospitalization in more recent years were less likely to be aged <1 year and female, and more likely to have public insurance and to be hospitalized in an urban teaching hospital (all Ptrend <0.001).
Table 1.
Patient and Hospital Characteristics of U.S. Children Hospitalized for Infectious Diseases, 2000–2012
| Variables | 2000 | 2003 | 2006 | 2009 | 2012 | Ptrend |
|---|---|---|---|---|---|---|
| Unweighted sample, n | 375,668 | 473,031 | 471,454 | 516,485 | 442,000 | - |
| Weighted sample, n | 732,955 | 797,086 | 769,886 | 766,284 | 625,461 | - |
| Patient characteristics* | ||||||
| Age | ||||||
| <1 year | 37.4 (34.1–40.7) | 35.1 (32.4–37.7) | 33.8 (31.1–36.4) | 30.4 (28.0–32.8) | 31.2 (28.7–33.7) | <0.001 |
| 1–4 years | 26.6 (24.4–28.8) | 27.5 (25.6–29.5) | 28.3 (26.2–30.4) | 28.7 (26.5–30.8) | 28.3 (26.1–30.5) | <0.001 |
| 5–19 years | 36.0 (33.4–38.5) | 37.4 (35.1–39.7) | 37.9 (35.4–40.4) | 41.0 (38.3–43.6) | 40.5 (37.7–43.3) | <0.001 |
| Female sex | 45.7 (45.4–45.9) | 45.6 (45.4–45.8) | 46.1 (45.9–46.3) | 46.1 (45.9–46.3) | 46.6 (46.4–46.8) | <0.001 |
| Race/ethnicity | ||||||
| Non-Hispanic white | 45.5 (43.2–47.8) | 36.1 (34.1–38.1) | 37.3 (35.2–39.4) | 42.0 (40.0–44.0) | 45.4 (43.2–47.6) | 0.14 |
| Non-Hispanic black | 12.6 (11.4–13.9) | 10.9 (9.9–12.1) | 11.0 (10.0–12.1) | 13.1 (12.0–14.3) | 14.4 (13.2–15.6) | 0.003 |
| Hispanic | 19.5 (17.3–21.8) | 19.2 (17.1–21.5) | 20.2 (18.0–22.7) | 22.1 (20.1–24.3) | 24.3 (22.0–26.7) | <0.001 |
| Others† | 1.8 (1.5–2.2) | 1.7 (1.3–2.1) | 1.8 (1.5–2.1) | 2.1 (1.8–2.4) | 2.5 (2.2–2.9) | 0.002 |
| Unknown | 20.6 (18.4–23.1) | 32.1 (29.4–35.0) | 29.7 (26.9–32.6) | 20.7 (18.4–23.2) | 13.5 (11.4–15.9) | <0.001 |
| Primary health insurance | ||||||
| Public | 41.5 (40.0–43.0) | 46.3 (45.0–47.6) | 48.7 (47.4–50.1) | 51.9 (50.7–53.1) | 55.0 (53.7–56.2) | <0.001 |
| Private | 50.0 (48.5–51.6) | 45.6 (44.2–47.0) | 42.5 (41.1–43.9) | 40.1 (38.9–41.4) | 37.4 (36.1–38.6) | <0.001 |
| Self-pay | 5.3 (4.8–5.7) | 4.3 (3.9–4.7) | 4.8 (4.4–5.2) | 4.1 (3.8–4.5) | 3.4 (3.1–3.8) | <0.001 |
| Other | 2.9 (2.6–3.3) | 3.6 (3.2–4.2) | 3.8 (3.2–4.4) | 3.6 (3.2–3.9) | 3.9 (3.5–4.5) | 0.004 |
| Hospital characteristics* | ||||||
| Region | ||||||
| Northeast | 18.5 (15.7–21.6) | 16.1 (14.0–18.5) | 16.6 (14.4–19.1) | 17.0 (14.4–19.9) | 17.3 (14.5–20.6) | 0.69 |
| Midwest | 17.7 (14.7–21.2) | 21.5 (18.9–24.5) | 21.5 (18.7–24.7) | 20.1 (17.3–23.2) | 20.4 (17.3–23.9) | 0.40 |
| South | 40.8 (36.8–44.9) | 40.9 (37.2–44.6) | 41.0 (37.1–44.9) | 40.8 (37.0–44.7) | 40.3 (36.3–44.4) | 0.86 |
| West | 23.0 (19.6–26.7) | 21.5 (18.5–24.9) | 20.9 (17.8–24.3) | 22.1 (18.9–25.6) | 22.1 (18.7–25.8) | 0.80 |
| Location/teaching status | ||||||
| Rural | 19.8 (17.8–22.0) | 18.8 (17.1–20.6) | 15.2 (13.7–16.7) | 15.4 (14.0–16.9) | 11.8 (10.7–13.1) | <0.001 |
| Urban nonteaching | 31.0 (28.1–34.1) | 32.4 (29.7–35.2) | 31.4 (28.5–34.5) | 32.9 (29.9–36.0) | 25.1 (22.6–27.9) | <0.001 |
| Urban teaching | 49.2 (45.3–53.2) | 48.8 (45.3–52.3) | 53.5 (49.9–57.0) | 51.7 (48.1–55.2) | 63.0 (59.8–66.1) | <0.001 |
| Hospital designation | 0.38 | |||||
| Non-children's hospital | 71.3 (66.0–76.0) | 70.3 (65.7–74.6) | 63.7 (59.0–68.2) | 63.8 (59.2–68.2) | 78.7 (73.7–83.0) | |
| Children's hospital | 28.8 (24.0–33.9) | 29.7 (25.4–34.0) | 36.3 (31.8–41.0) | 36.1 (31.8–40.8) | 21.3 (17.0–26.3) |
Data are expressed as % (95% CI) unless otherwise indicated.
Percentages may not equal 100 due to rounding.
Asian, Pacific Islander, Native American, and Other.
Trends in Hospitalization Rates
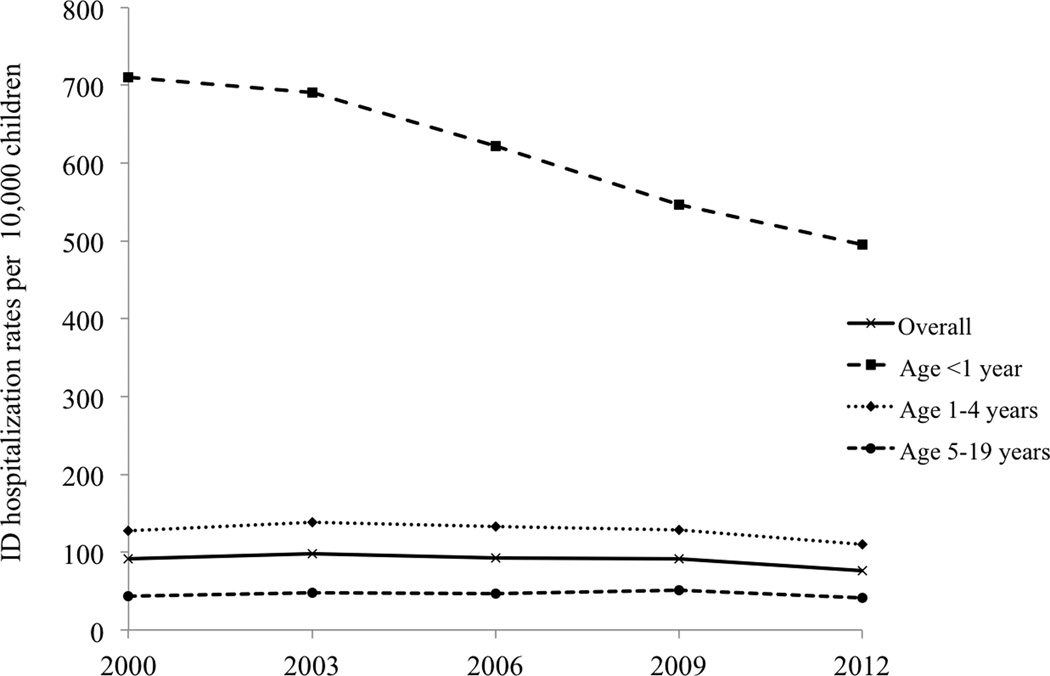
From 2000 to 2012, the rate of overall ID hospitalizations decreased from 91.0 to 75.8 per 10,000 U.S. children (16.5% decrease; Ptrend<0.001; Figure 1). This finding was due largely to the decrease in the rate among children aged <1 year (30.3% decrease; Ptrend<0.001). A similar downward trend was observed in children aged 1–4 years (13.4% decrease, Ptrend=0.002) while the rate was relatively constant in children aged 5–19 years (4.7% decrease, Ptrend=0.53). In the sensitivity analysis using OLS model with heteroscedasticity-robust standard errors, the results did not change materially across the age groups.
Figure 1. Change in infectious disease hospitalization rates per 10,000 U.S. children, 2000–2012.
From 2000 to 2012, the rate of overall ID hospitalizations decreased from 91.0 to 75.8 per 10,000 U.S. children (16.5% decrease; Ptrend<0.001). A similar decreasing trend was observed in children aged <1 year and children aged 1–4 years (both Ptrend=0.002).
Hospitalizations by ID Subgroup
Among the 21 ID subgroups, the most frequently listed subgroup was lower respiratory infection (including pneumonia and bronchiolitis), accounting for 42.8% of all ID hospitalizations in 2012 (Table 2). From 2000 to 2012, the hospitalization rate for lower respiratory infection decreased from 40.1 to 32.5 per 10,000 children (19.1% decrease, P<0.001; data available upon request). In particular, the hospitalization rate for pneumonia decreased more substantially (25.5% decrease; P<0.001) during the same period. The next most commonly listed subgroup was abdominal and rectal infection, accounting for 13.8% of all ID hospitalizations in 2012. The hospitalization rate for abdominal and rectal infection also decreased during the same period (from 11.3 to 10.5 per 10,000 children; 6.9% decrease; P<0.001). The third most frequently listed subgroup changed from upper respiratory infections in 2000 to skin infections in 2012, which accounted for 10.9% of all ID hospitalizations in 2012.
Table 2.
Most Frequently Listed Diagnostic Subgroups in Infectious Disease Hospitalizations in U.S. Children, 2000 and 2012
| 2000 | 2012 | ||||||
|---|---|---|---|---|---|---|---|
| Rank | Infectious disease subgroup |
Weighted sample, n |
Proportion of infectious disease hospitalization, % (95% CI) |
Rank | Infectious disease subgroup |
Weighted sample, n |
Proportion of infectious disease hospitalization, % (95% CI) |
| Overall | Overall | ||||||
| 1 | Lower respiratory infections* |
323,449 | 44.1% (43.4%–44.9%) | 1 | Lower respiratory infections |
267,809 | 42.8% (42.2%–43.4%) |
| 2 | Abdominal and rectal infections |
90,862 | 12.4% (12.0%–12.9%) | 2 | Abdominal and rectal infections |
86,566 | 13.8% (13.3%–14.4%) |
| 3 | Upper respiratory infections |
60,384 | 8.2% (8.0%–8.5%) | 3 | Skin infections | 68,436 | 10.9% (10.7%–11.2%) |
| 4 | Urinary tract infections |
54,930 | 7.5% (7.3%–7.7%) | 4 | Upper respiratory infections |
48,449 | 7.8% (7.5%–8.1%) |
| 5 | Enteric infections | 49,714 | 6.8% (6.5%–7.1%) | 5 | Urinary tract infections |
46,008 | 7.4% (7.2%–7.5%) |
| Age <1 year | Age <1 year | ||||||
| 1 | Lower respiratory infections |
165,982 | 60.5% (59.4%–61.6%) | 1 | Lower respiratory infections |
118,632 | 60.8% (60.0%–61.5%) |
| 2 | Urinary tract infections |
20,061 | 7.3% (6.9%–7.7%) | 2 | Urinary tract infections |
16,769 | 8.6% (8.3%–8.9%) |
| 3 | Septicemia | 19,545 | 7.1% (6.6%–7.7%) | 3 | Septicemia | 15,920 | 8.2% (7.7%–8.6%) |
| 4 | Upper respiratory infections |
16,466 | 6.0% (5.8%–6.3%) | 4 | Upper respiratory infections |
12,804 | 6.6% (6.2%–7.0%) |
| 5 | Enteric infections | 15,969 | 5.8% (5.5%–6.1%) | 5 | Skin infections | 9,448 | 4.8% (4.6%–5.1%) |
| Age 1–4 years | Age 1–4 years | ||||||
| 1 | Lower respiratory infections |
104,541 | 53.6% (52.5%–54.7%) | 1 | Lower respiratory infections |
95,701 | 54.1% (53.1%–55.1%) |
| 2 | Enteric infections | 21,319 | 10.9% (10.4%–11.5%) | 2 | Skin infections | 34,087 | 14.1% (13.6%–14.6%) |
| 3 | Upper respiratory infections |
21,023 | 10.8% (10.4%–11.2%) | 3 | Upper respiratory infections |
18,492 | 10.5% (10.0%–11.0%) |
| 4 | Skin infections | 11,735 | 6.0% (5.6%–6.4%) | 4 | Enteric infections | 9,062 | 5.1% (4.9%–5.4%) |
| 5 | Urinary tract infections |
10,708 | 5.5% (5.3%–5.7%) | 5 | Urinary tract infections |
9,059 | 5.1% (4.9%–5.3%) |
| Age 5–19 years | Age 5–19 years | ||||||
| 1 | Abdominal and rectal infections |
86,350 | 32.8% (31.8%–33.7%) | 1 | Abdominal and rectal infections |
80,986 | 32.0% (31.1%–32.9%) |
| 2 | Lower respiratory infections |
52,925 | 20.1% (19.5%–20.6%) | 2 | Lower respiratory infections |
53,476 | 21.1% (20.6%–21.6%) |
| 3 | Urinary tract infections |
24,161 | 9.2% (8.9%–9.4%) | 3 | Skin infections | 34,087 | 13.5% (13.1%–13.9%) |
| 4 | Skin infections | 23,961 | 9.1% (8.8%–9.4%) | 4 | Urinary tract infections |
20,180 | 8.0% (7.8%–8.2%) |
| 5 | Upper respiratory infections |
22,895 | 8.7% (8.4%–9.0%) | 5 | Upper respiratory infections |
17,153 | 6.8% (6.5%–7.0%) |
Abbreviation: CI, confidence interval.
Lower respiratory infections include pneumonia and bronchiolitis.
With respect to age groups, there were modest differences in the proportion of ID hospitalization attributable to the disease subgroups. For example, lower respiratory infection was the leading cause of ID hospitalizations both in children aged <1 year and 1–4 years (Table 2). By contrast, in children aged 5–19 years, abdominal and rectal infection was the leading cause, followed by lower respiratory infection (Table 2).
Among the 21 ID subgroups, several subgroups demonstrated a remarkable decline in the rate of hospitalizations from 2000 to 2012 – e.g., HIV/AIDS (81.5% decrease), meningitis due to non-viral organisms (64.9% decrease), infections due to internal prosthetic device, implant, and graft (61.6% decrease), and enteric infections (47.8% decrease; all, P<0.001; data available upon request). By contrast, the rate of hospitalizations increased in 4 ID subgroups: skin infection (67.6% increase), perinatal infection (16.7% increase), septicemia (6.5% increase), and postoperative infections (4.9% increase; all P<0.001).
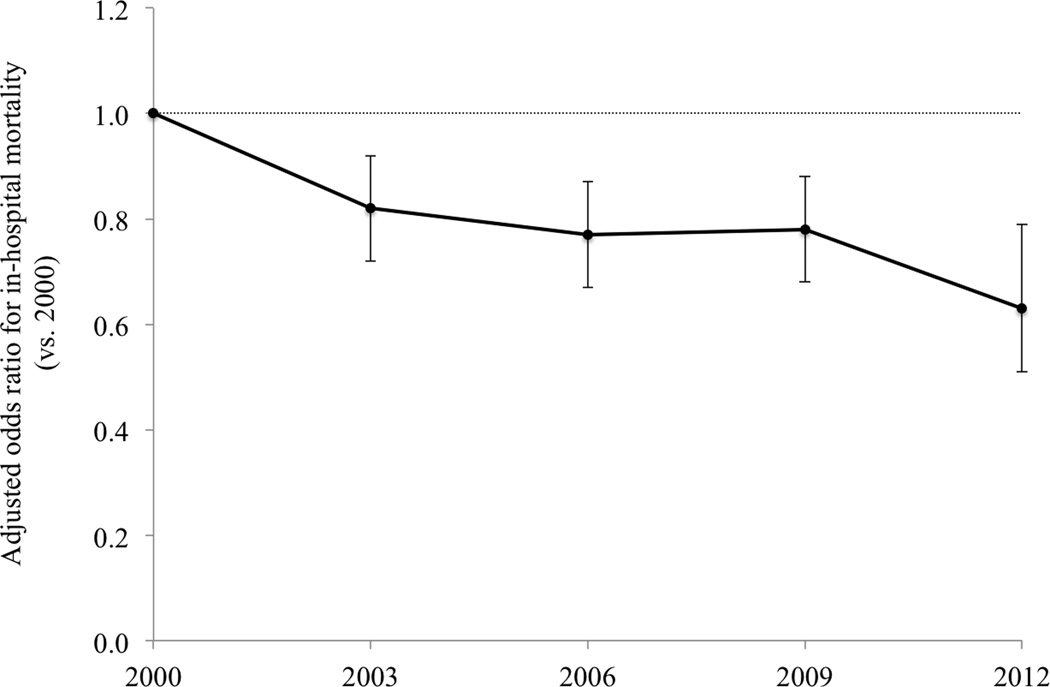
In-hospital Mortality
From 2000 to 2012, the unadjusted in-hospital mortality did not change significantly (odds ratio [OR] for comparison of 2012 with 2000, 0.94; 95%CI: 0.79–1.12). In contrast, the multivariable-adjusted mortality decreased significantly (adjusted OR, 0.63; 95%CI, 0.51–0.79; Figure 2). Similar downward trends were observed in children aged 1–4 years and 5–19 years.
Figure 2. Adjusted odds ratio of in-hospital mortality in in U.S. children hospitalized for infectious disease, 2000–2012.
Models were adjusted for patient and hospital characteristics. The reference year is 2000. Error bars represent the 95% confidence interval. From 2000 to 2012, the adjusted OR significantly decreased (OR for comparison of 2012 with 2000, 0.63; 95%CI, 0.51–0.79; P<0.001).
Length of Stay and Direct Cost for ID Hospitalizations
From 2000 to 2012, there was no significant change in median LOS (2 days in 2000 to 2 days in 2012; Ptrend=0.33) for all ID hospitalizations. Among the 21 ID subgroups, a half of subgroups demonstrated a decline in the LOS – e.g., abdominal infection (2 days vs. 1 day; Ptrend <0.001). By contrast, the LOS increased in 4 ID subgroups: meningitis (7 days vs. 9 days; Ptrend<0.001 and sepsis (3 days vs. 4 days; Ptrend<0.001). The median direct cost per ID hospitalization increased from $3,452 (IQR, $2,128–$6,033, data available upon request) in 2003 to $3,784 (IQR, $2,201-$6,921) in 2012 (10% increase; Ptrend=0.007) adjusted for inflation. This increasing trend in direct cost for ID hospitalization was observed across the age groups. In 2012, the nationwide direct cost was $4.4 billion (IQR, $4.2–$4.7 billion).
DISCUSSION
In this analysis using a large, nationally-representative database of U.S. pediatric hospitalizations, we found significant downward trends in the rate of overall ID hospitalizations and in-hospital mortality from 2000 to 2012. While the hospitalization rate for most ID subgroups (e.g., lower respiratory infections) decreased over this 13-year period, several ID subgroups (e.g., skin infections) increased. Concurrent with these trends were a significant decline in adjusted mortality associated with ID hospitalization. Our data also demonstrated an increasing trend in the direct cost per hospitalization, with a substantial nationwide financial burden in 2012.
Quantifying the national burden of ID hospitalizations is of great interest to a variety of stakeholders. However, to date, most epidemiologic research on pediatric IDs has focused the specific reasons for hospitalization.6, 8, 10, 25–29 Our data corroborate these previous reports and extend them by comprehensively examining the ID hospitalization rate and mortality among U.S. children. In this study, we found the decreasing trends in the rate of overall ID hospitalization; this decline was largely driven by the decrease in hospitalizations for lower respiratory infections and enteric infections. Indeed, these two ID subgroups accounted for 73% of overall decrease in the number of ID hospitalizations from 2000 to 2012. These observations were paralleled by the studies that demonstrated a decrease in hospitalization for pneumonia and rotavirus-associated illness in U.S. children after the implementation of pneumococcal conjugate vaccine6, 27 and rotavirus vaccine.10, 11
The observed reduction in ID hospitalizations (vaccine-preventable diseases and other IDs) supports a cautious optimism that the ID-related morbidity can be further reduced. However, the burden of ID hospitalization remains substantial – i.e., approximately 625,000 hospitalizations in 2012, contributing to one-fourth of all pediatric hospitalizations in the U.S. In parallel, the literature has documented that the immunization coverage remains suboptimal (e.g., 20% of children did not receive pneumococcal conjugate vaccine5), with reported racial/ethnic and socioeconomic disparities in immunization coverage.30, 31 These findings should facilitate continued efforts, such as bridging the gaps in immunization coverage, to reduce the ID-related morbidity and healthcare utilization nationally. It will require collective efforts of a variety of stakeholders, such as the federal agencies, local public health departments, professional organizations, and clinicians.
The apparent decline in the hospitalization rate for most ID subgroups contrasts sharply with the upward trend in that for several ID subgroups. In particular, we are struck by the substantial increase in hospitalization rates for skin infections over the study period. The reasons for this finding are likely multifactorial – e.g., a shift in population demographics and altered coding practice. Alternatively, this observation was mirrored by the prior studies demonstrating an increasing number of emergency department visits12 and hospitalizations25 for skin infections during the emergence of community-associated methicillin-resistant Staphylococcus aureus. In parallel, other antimicrobial-resistant organisms (e.g., third-generation cephalosporin-resistant and extended-spectrum β-lactamase bacteria) have also emerged among U.S. children in the ambulatory and inpatient settings.32 These data collectively underscore the importance of continued preventive efforts targeting at emerging antimicrobial-resistant organisms.
We are also struck by the substantial nationwide expenditure for ID hospitalizations ($4.4 billion in 2012), with a 10% increase in the cost per hospitalization after adjusting for inflation. Our current investigation is the first to specifically examine the cost of U.S. pediatric hospitalizations for IDs. Although a prior study reported that the hospital charges for pediatric and adult ID hospitalizations during the 1997–2006 periods were $865 billion in the U.S., the use of hospital charges substantially overestimates the actual costs of resources consumed.33 The reasons for increasing direct cost per hospitalization are unclear. The population of ID hospitalization may be similar in severity over the study period, but their inpatient resource use may be increasing.34 Alternatively, the prevalence of children with chronic medical conditions in the study population might be increasing,34, 35 and thereby leading to more intensive resource use. Although our nationwide epidemiologic data are unable to explore the more granular issue of resource use, our observations should facilitate studies that evaluate determinants of the increasing cost for ID hospitalizations.
Potential Limitations
We acknowledge several potential limitations to the study. First, as with any studies using administrative data, there may be potential for errors in recording diagnoses. We might have under- or overestimated the disease burden in the individual years. However, potential misclassifications should not have varied substantially between years, and therefore these errors likely would have limited impact on the trend analyses. Moreover, the HCUP data are considered accurate and widely used to estimate diagnoses and hospitalization frequency.7, 10, 36 Second, we identified ID hospitalizations with an ID listed as the primary diagnosis to limit potential misclassification, while this would also have led to an underestimation of ID hospitalizations. Third, the KID contains discharge-level records and not patient-level records. Lack of patient identifiers precludes us from examining longer-term outcomes, such as readmissions. Lastly, the present study investigated only hospitalized children; therefore, those who were treated and released in the clinic or emergency department were not examined. Nevertheless, we focused on the population with the highest morbidity and healthcare utilization. Our findings are directly relevant to the hundreds of thousands of US children hospitalized for IDs (and their families) each year.
CONCLUSIONS
By using a nationally-representative database of U.S. pediatric hospitalizations, we found a significant decline in the rate of ID hospitalization and in-hospital mortality among U.S. children from 2000 to 2012. The observed decrease in hospitalizations for vaccine-preventable diseases and other IDs supports prior optimism that ID-related morbidity and healthcare utilizations can be further reduced. By contrast, the observed increase in hospitalization for several diseases (e.g., skin infections) presents an important public health challenge. For researchers, our data underscore the continued importance of preventive and surveillance strategies aiming at reducing these IDs. Finally, because IDs continue to be a major public health problem, the substantial cost for ID hospitalizations call for the development of better approaches to reduce the financial burden in an already-stressed healthcare system.
Acknowledgments
CAC was supported by grant U01 AI-67693 and R01 AI-114552 from the National Institutes of Health (Bethesda, MD). JMM was supported by the grant from R01 AI-108588 from the National Institutes of Health (Bethesda, MD).
REFERENCES
- 1.Centers for Disease Control and Prevention. Control of infectious diseases. MMWR Morb Mortal Wkly Rep. 1999;48(29):621–629. [PubMed] [Google Scholar]
- 2.Armstrong GL, Conn LA, Pinner RW. Trends in infectious disease mortality in the United States during the 20th century. JAMA. 1999;281(1):61–66. doi: 10.1001/jama.281.1.61. [DOI] [PubMed] [Google Scholar]
- 3.Christensen KL, Holman RC, Steiner CA, Sejvar JJ, Stoll BJ, Schonberger LB. Infectious disease hospitalizations in the United States. Clin Infect Dis. 2009;49(7):1025–1035. doi: 10.1086/605562. [DOI] [PubMed] [Google Scholar]
- 4.Yorita KL, Holman RC, Sejvar JJ, Steiner CA, Schonberger LB. Infectious disease hospitalizations among infants in the United States. Pediatrics. 2008;121(2):244–252. doi: 10.1542/peds.2007-1392. [DOI] [PubMed] [Google Scholar]
- 5.Healthy people 2020. [Accessed June 6, 2015];Immunization and Infectious Diseases. Available at: http://www.healthypeople.gov./2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives.
- 6.Griffin MR, Zhu Y, Moore MR, Whitney CG, Grijalva CG. U.S. hospitalizations for pneumonia after a decade of pneumococcal vaccination. N Engl J Med. 2013;369(2):155–163. doi: 10.1056/NEJMoa1209165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee GE, Lorch SA, Sheffler-Collins S, Kronman MP, Shah SS. National hospitalization trends for pediatric pneumonia and associated complications. Pediatrics. 2010;126(2):204–213. doi: 10.1542/peds.2009-3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thigpen MC, Whitney CG, Messonnier NE, et al. Bacterial meningitis in the United States, 1998–2007. N Engl J Med. 2011;364(21):2016–2025. doi: 10.1056/NEJMoa1005384. [DOI] [PubMed] [Google Scholar]
- 9.Tsai CJ, Griffin MR, Nuorti JP, Grijalva CG. Changing epidemiology of pneumococcal meningitis after the introduction of pneumococcal conjugate vaccine in the United States. Clin Infect Dis. 2008;46(11):1664–1672. doi: 10.1086/587897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leshem E, Tate JE, Steiner CA, Curns AT, Lopman BA, Parashar UD. Acute gastroenteritis hospitalizations among US children following implementation of the rotavirus vaccine. JAMA. 2015;313(22):2282–2284. doi: 10.1001/jama.2015.5571. [DOI] [PubMed] [Google Scholar]
- 11.Aliabadi N, Tate JE, Haynes AK, Parashar UD Centers for Disease Control and Prevention. Sustained decrease in laboratory detection of rotavirus after implementation of routine vaccination-United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2015;64(13):337–342. [PMC free article] [PubMed] [Google Scholar]
- 12.Pallin DJ, Egan DJ, Pelletier AJ, Espinola JA, Hooper DC, Camargo CA., Jr Increased US emergency department visits for skin and soft tissue infections, and changes in antibiotic choices, during the emergence of community-associated methicillin-resistant Staphylococcus aureus. Ann Emerg Med. 2008;51(3):291–298. doi: 10.1016/j.annemergmed.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Gerber JS, Coffin SE, Smathers SA, Zaoutis TE. Trends in the incidence of methicillin-resistant Staphylococcus aureus infection in children's hospitals in the United States. Clin Infect Dis. 2009;49(1):65–71. doi: 10.1086/599348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project (HCUP) [Accessed May 22, 2015];Overview of the Kids' Inpatient Database (KID) Available at: http://www.hcup-us.ahrq.gov/kidoverview.jsp.
- 15.Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project (HCUP) [Accessed May 22, 2015];Introduction to the HCUP Kids' Inaptient Database (KID) Available at: http://www.hcup-us.ahrq.gov/db/nation/kid/KID_2012_Introduction.pdf.
- 16.Hasegawa K, Tsugawa Y, Cohen A, Camargo CA., Jr Infectious Disease-related Emergency Department Visits Among Children in the United States. Pediatr Infect Dis J. 2015;34(7):681–685. doi: 10.1097/INF.0000000000000704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.United States Bureau of the Census. [Accessed May 22, 2015];Geographic Terms and Concepts - Census Divisions and Census Regions. Available at: http://www.census.gov/geo/www/us_regdiv.pdf.
- 18.United States Department of Agriculture Economic Research Service. [Accessed May 22, 2015];Urban Influence Codes. Available at: http://www.ers.usda.gov/data-products/urban-influence-codes.aspx.
- 19.Children's Hospital Association. [Accessed May 22, 2015];The National Association of Children’s Hospitals and Related Institutions Classification Criteria. Available at: http://www.childrenshospitals.org.
- 20.US Census Bereau. [Accessed May 22, 2015];Population estimates. Available at: http://www.census.gov/popest/
- 21. [Accessed May 22, 2015];Centers for Medicare and Medicaid Services. Available at: http://www.cms.gov. [PubMed]
- 22.Huber PJ. The behavior of maximum likelihood estimates under nonstandard conditions. Proceedings of the fifth Berkeley symposium on mathematical statistics and probability. 1967;1:221–223. [Google Scholar]
- 23.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica: Journal of the Econometric Society. 1980:817–838. [Google Scholar]
- 24. [Accessed May 31, 2015];Consumer Price Index. Available at: http://www.bls.gov/cpi/
- 25.Edelsberg J, Taneja C, Zervos M, et al. Trends in US hospital admissions for skin and soft tissue infections. Emerg Infect Dis. 2009;15(9):1516–1518. doi: 10.3201/eid1509.081228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tate JE, Haynes A, Payne DC, et al. Trends in national rotavirus activity before and after introduction of rotavirus vaccine into the national immunization program in the United States, 2000 to 2012. Pediatr Infect Dis J. 2013;32(7):741–744. doi: 10.1097/INF.0b013e31828d639c. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan SL, Barson WJ, Lin PL, et al. Early trends for invasive pneumococcal infections in children after the introduction of the 13-valent pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2013;32(3):203–207. doi: 10.1097/INF.0b013e318275614b. [DOI] [PubMed] [Google Scholar]
- 28.Bhat N, Wright JG, Broder KR, et al. Influenza-associated deaths among children in the United States, 2003–2004. N Engl J Med. 2005;353(24):2559–2567. doi: 10.1056/NEJMoa051721. [DOI] [PubMed] [Google Scholar]
- 29.Roush SW, Murphy TV Vaccine-Preventable Disease Table Working G. Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007;298(18):2155–2163. doi: 10.1001/jama.298.18.2155. [DOI] [PubMed] [Google Scholar]
- 30.Spicer JO, Thomas S, Holst A, Baughman W, Farley MM. Socioeconomic and racial disparities of pediatric invasive pneumococcal disease after the introduction of the 7-valent pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2014;33(2):158–164. doi: 10.1097/INF.0000000000000025. [DOI] [PubMed] [Google Scholar]
- 31.Flannery B, Schrag S, Bennett NM, et al. Impact of childhood vaccination on racial disparities in invasive Streptococcus pneumoniae infections. JAMA. 2004;291(18):2197–2203. doi: 10.1001/jama.291.18.2197. [DOI] [PubMed] [Google Scholar]
- 32.Logan LK, Braykov NP, Weinstein RA Ramanan Laxminarayan ftCEPP. Extended-Spectrum β-Lactamase–Producing and Third-Generation Cephalosporin-Resistant Enterobacteriaceae in Children: Trends in the United States, 1999–2011. J Ped Infect Dis. 2014;3(4):320–328. doi: 10.1093/jpids/piu010. [DOI] [PubMed] [Google Scholar]
- 33.Dor A, Farley DE. Payment source and the cost of hospital care: evidence from a multiproduct cost function with multiple payers. J Health Econ. 1996;15(1):1–21. doi: 10.1016/0167-6296(95)00029-1. [DOI] [PubMed] [Google Scholar]
- 34.Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA., Jr Trends in bronchiolitis hospitalizations in the United States, 2000–2009. Pediatrics. 2013;132(1):28–36. doi: 10.1542/peds.2012-3877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107(6):E99. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- 36.Hasegawa K, Tsugawa Y, Camargo CA, Jr, Brown DF. Frequent utilization of the emergency department for acute heart failure syndrome: a population-based study. Circ Cardiovasc Qual Outcomes. 2014;7(5):735–742. doi: 10.1161/CIRCOUTCOMES.114.000949. [DOI] [PubMed] [Google Scholar]