Supplemental Digital Content is available in the text
Abstract
Anxiety and depression are common among patients with cancer, and are often treated with psychological interventions including mindfulness-based therapy.
The aim of the study was to perform a meta-analysis of the effectiveness of mindfulness-based interventions for improving anxiety and depression in patients with cancer.
Medline, the Cochrane Library, EMBASE, and Google Scholar were searched. The randomized controlled trials designed for patients diagnosed with cancer were included. Mindfulness-based interventions were provided.
The outcomes assessed were the changes in anxiety and depression scores from before to after the intervention. The treatment response was determined by calculating the standardized mean difference (SMD) for individual studies and for pooled study results. Subgroup analyses by cancer type, type of therapy, and length of follow-up were performed.
Seven studies, involving 469 participants who received mindfulness-based interventions and 419 participants in a control group, were included in the meta-analysis. Mindfulness-based stress reduction and art therapy were the most common interventions (5/7 studies). All studies reported anxiety and depression scores. The pooled SMD of the change in anxiety significantly favored mindfulness-based therapy over control treatment (−0.75, 95% confidence interval −1.28, −0.22, P = 0.005). Likewise, the pooled SMD of the change in depression also significantly favored mindfulness-based therapy over control (−0.90, 95% confidence interval −1.53, −0.26, P = 0.006). During the length of follow-ups less than 12 weeks, mindfulness-based therapy significantly improved anxiety for follow-up ≤12 weeks after the start of therapy, but not >12 weeks after the start of therapy.
There was a lack of consistency between the studies in the type of mindfulness-based/control intervention implemented. Patients had different forms of cancer. Subgroup analyses included a relatively small number of studies and did not account for factors such as the severity of anxiety and/or depression, the time since diagnosis, and cancer stage.
Mindfulness-based interventions effectively relieved anxiety and depression among patients with cancer. However, additional research is still warranted to determine how long the beneficial effects of mindfulness-based therapy persist.
INTRODUCTION
A diagnosis of cancer can have a significant impact, not only on individuals’ physical well being, but also on their psychological well being. Such a diagnosis, and the ensuing developments/events, can challenge psychological well being in a multitude of manners, particularly through stress, anxiety, and depression related to symptoms, treatment (including potential side effects) and recovery (or potential death), and financial and family concerns.1,2 As such, it is hardly surprising that anxiety and depression are very common among patients with cancer.3,4
Although chemotherapy and radiotherapy can be effective for treating the underlying physical cause(s) of cancer, these treatments do not always affect or improve the psychological well being. Indeed, anxiety, tension, and depression are often experienced before and after, as well as during, treatment.2 Therefore, psychosocial interventions have been developed in an attempt to help manage the psychological manifestations of cancer. These psychological interventions can take a multitude of forms, but ultimately aim to behaviorally reduce stress, tension, and anxiety.2 There is also evidence that improved psychological well being can affect treatment outcomes2 and reduce cancer-related pain.5 Despite the fact that many studies, systematic reviews, and meta-analyses over the years have examined the impact of psychological interventions in patients with various types of cancer, there is a lack of definitive evidence as to whether such interventions are effective.6–8 Further, relatively few published meta-analyses have examined the effect of psychological interventions on anxiety and depression in patients with cancer.
A multitude of psychological interventions have been used in the context of cancer care, including cognitive/behavioral, education, counseling, hypnosis, relaxation, and mindfulness-based interventions.1 In recent meta-analyses, Faller et al9 reported on changes in anxiety and depression after face-to-face psychological interventions, whereas Galway et al,10 in a Cochrane review, reported on changes in anxiety and depression after psychological interventions comprising interpersonal dialog between a trained helper and patients newly diagnosed with cancer. Mindfulness-based therapy revolves around the Buddhist concept of mindfulness, defined as intentional nonjudgmental awareness of present-moment experiences,11 and comprises various forms, including mindfulness-based cognitive therapy, mindfulness-based stress reduction, and mindfulness-based art therapy. Mindfulness-based cognitive therapy targets cognitive processes underlying depression, through a series of group sessions, psychoeducation, and meditation.12 Mindfulness-based stress reduction comprises the presentation of theories related to the body–mind connection, mediation, and relaxation, group and individual meditation, and group activities designed to support the practical application of mindfulness.13 Mindfulness-based art therapy involves the integration of group art therapy and mindfulness meditation.14,15
To our knowledge, only a few recent meta-analyses have examined the effectiveness of mindfulness-based therapy for improving anxiety and depression in patients with cancer; however, 2 of these analyses16,17 were restricted to patients with breast cancer only, whereas the other18 included both patients with cancer and survivors of cancer. To our knowledge, no recent meta-analysis has strictly examined the effect of mindfulness-based therapy on changes in anxiety and depression in patients with cancer. Further, since the publication of the aforementioned meta-analyses, the findings from an important randomized study of mindfulness-based therapy in women with breast cancer has been published.15 Given this information, and that anxiety and depression are common among patients with cancer and that mindfulness-based therapy is a popular approach for managing these afflictions,11 we decided to carry out a meta-analysis in an attempt to obtain definitive, up-to-date information on this relevant aspect of cancer management.
The aim of this meta-analysis of randomized controlled trials (RCTs) published in the peer-reviewed literature was to assess the overall effectiveness of mindfulness-based therapy for relieving anxiety and depression among patients with any form of cancer.
MATERIALS AND METHODS
Eligibility Criteria
Inclusion Criteria
Studies were considered for inclusion in the meta-analysis if they were RCTs that involved adult participants diagnosed with cancer (including stage 0 cancer), who received mindfulness-based interventions with the comparison of usual care and reported outcomes for the change from baseline in anxiety and depression after the intervention.
Exclusion Criteria
Studies were excluded if they did not evaluate changes in anxiety or depression. Articles published in the form of letters, comments, editorials, and case reports were excluded, as were those published in non-English language journals.
Search Strategy
Medline, the Cochrane Library, EMBASE, and Google Scholar were searched (search date: November 30, 2014) using the following key words: cancer/neoplasm/carcinoma; depression; anxiety; mindfulness/meditation/psychotherapy/behavior therapy. The approval by an institutional review board is not required for this study because humans were not studied.
Study Selection and Data Extraction
Studies were independently identified by 2 reviewers (and data extracted) using the aforementioned search strategy. A third reviewer was consulted to resolve any differences in opinion between these reviewers regarding study eligibility and data extraction.
The following information was extracted from studies that met the eligibility criteria: the name of the first author, year of publication, study design, participant demographics and diagnoses, questionnaires or tools used for evaluation, and outcome measures.
Outcome Measures
The outcomes of interest were the change in measures of anxiety and depression from before to after the intervention.
Quality Assessment
The quality of the studies included in the meta-analysis was assessed by the 2 reviewers using the Cochrane Risk of Bias Tool.19 Again, disagreement between reviewers was resolved by consulting a third reviewer.
Statistical Analysis
The changes from baseline to after the intervention in anxiety and depression were compared between participants who received mindfulness-based therapy and those who received control interventions. Subgroup analysis was also performed, whereby the changes in anxiety and depression were compared on the basis of diagnosis, type of intervention, and the length of follow-up. A change in standardized mean difference (SMD) from before and after intervention, with a corresponding 95% confidence interval (CI), was applied for each outcome measure. An SMD <0 indicated the intervention group might have higher improvement to decrease the anxiety or depression than the control group; an SMD >0 indicated the intervention group might have lower improvement to decrease the anxiety or depression than the control group; an SMD = 0 indicated both intervention and control group have similar change. Cochran Q statistic and I2 were used to carry out a chi-square–based test of homogeneity. I2 represents the level of the total variability in effect estimates among trials caused by heterogeneity rather than chance. If heterogeneity was detected (I2 > 50%), random-effects models of analysis were used. Otherwise, the data were analyzed using fixed-effects models. A 2-sided P value <0.05 was taken to indicate statistical significance for one comparison group over the other. The leave-one-out approach was used to perform the sensitivity analysis for the outcomes of clinical trial. Funnel plots for the outcomes and Egger test were used to assess the publication bias. The data points forming a symmetrical funnel-shaped distribution indicated the absence of publication bias. For Egger test, a 1-tailed significance level >0.05 indicated the absence of publication bias. The software used for all analyses was Comprehensive Meta-Analysis statistical software, version 2.0 (Biostat, Englewood, NJ).
RESULTS
Literature Search
After the removal of duplicates, a total of 293 articles were identified in the literature search (Fig. 1). Of these, the majority was excluded and 52 underwent full-text review. Of the articles that underwent full-text review, 45 were excluded (most commonly because they did not report the outcomes of interest) and 7 RCTs 12–15,20–22 were included in the meta-analysis.
FIGURE 1.
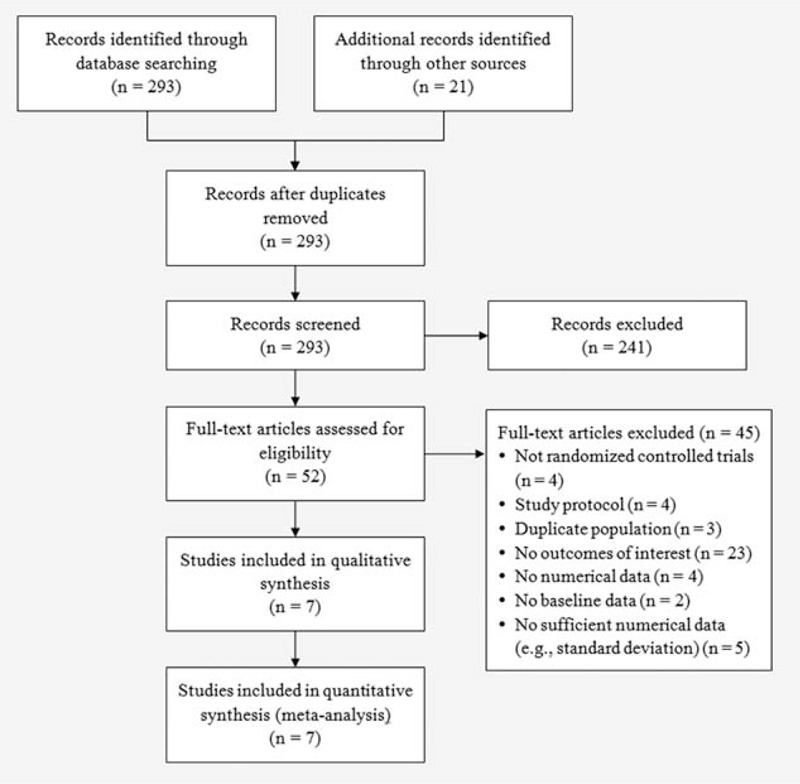
Flowchart of study selection. RCT = randomized controlled trial.
Study Characteristics
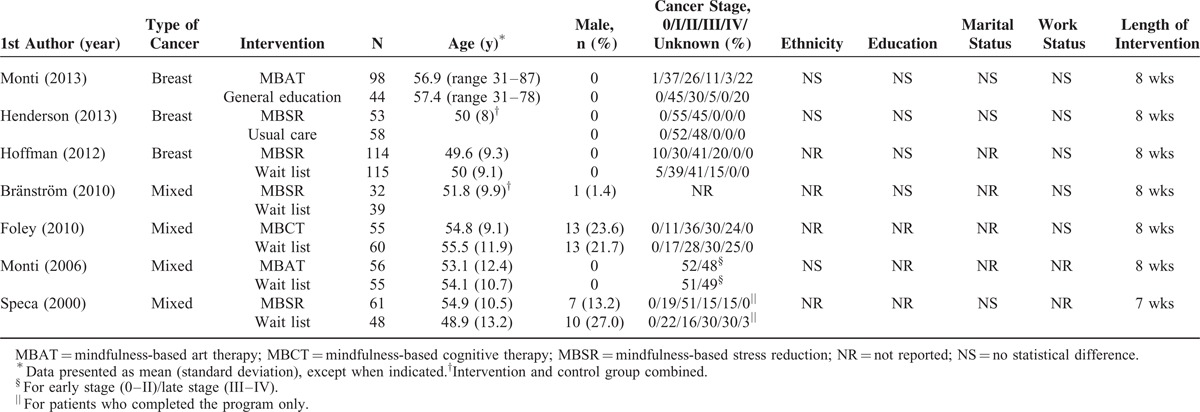
The key characteristics of the studies included in the meta-analysis are summarized in Table 1. Studies involving participants with breast cancer were most common. The type of intervention varied between studies; however, mindfulness-based stress reduction (3 studies) and mindfulness-based art therapy (2 studies) were the most common interventions. Control group participants were typically wait-listed for mindfulness-based therapy (5 studies). The number of participants in each study ranged from 32 to 114 (total = 469) for the mindfulness-based therapy groups, and from 39 to 115 (total = 419) for the control groups. The age of the participants (generally around 50 years) was similar between studies and between groups within studies. As most of the studies involved women with breast cancer, there was a predominance of female participants. In the studies of participants with other types of cancer (apart from prostate and gynecologic cancer), the proportion of participants who were men ranged from 1.4% to 23.6% in the intervention groups, and from 21.7% to 27.0% in the control groups. The majority of patients included patients who had stage I to III cancer, although there was some variability between studies. Where reported, there were no between-group differences within each study with regards to ethnicity, level of education, marital status, or work status. The length of the intervention was 8 weeks in 6 studies and 7 weeks in 1 study.
TABLE 1.
Summary of Key Characteristics of Studies Included in the Meta-analysis
Outcome Measures
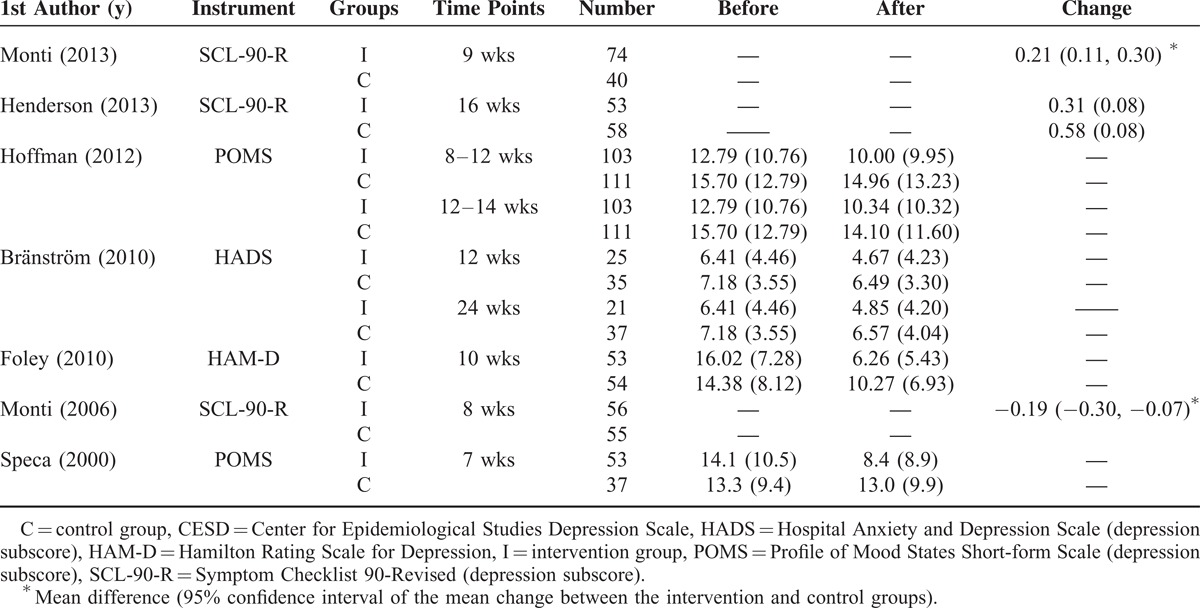
Tables 2 and 3, respectively, summarize anxiety and depression scores before and after the intervention, and the type of instrument used for assessment. The Symptom Checklist 90-Revised and the Profile of Mood States short form scale were the most commonly used instruments for the assessment of anxiety and depression, respectively. Only Hoffman et al21 and Bränström et al22 reported outcomes at different time points.
TABLE 2.
Summary of Anxiety Outcomes Before and After Mindfulness-based Therapy
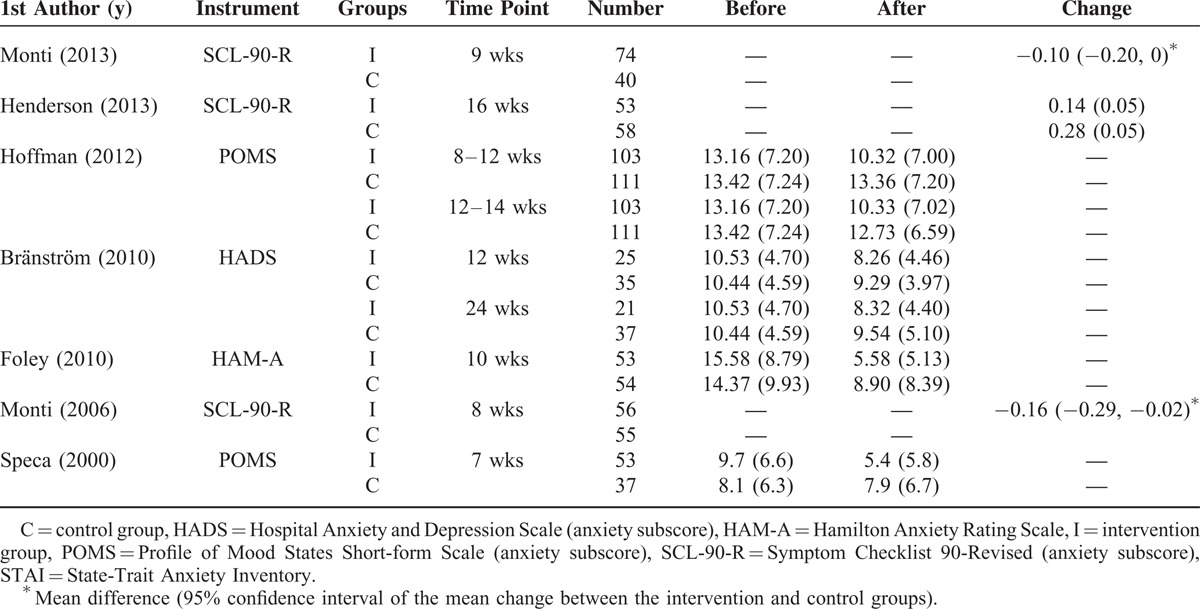
TABLE 3.
Summary of Depression Outcomes Before and After Mindfulness-based Therapy
Meta-analysis of Anxiety
All 7 studies were included in the meta-analysis of the change in anxiety (Fig. 2A). As there was evidence of significant heterogeneity among the studies, a random-effects model of analysis was used (Q statistic = 76.30, I2 = 92.14%, P < 0.001). The pooled SMD indicated anxiety was improved to a significantly greater extent in the mindfulness-based therapy group compared with the control group (pooled SMD = −0.75, 95% CI −1.28 to −0.22, P = 0.005).
FIGURE 2.
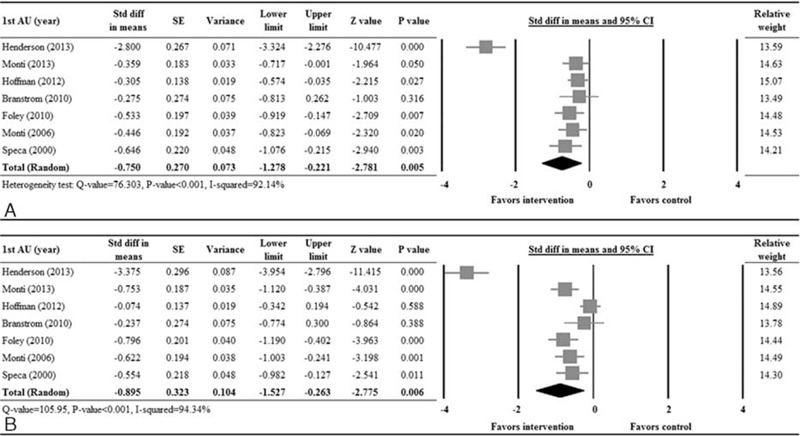
Forest plot of intervention versus control for the change in anxiety (A) and depression (B). CI = confidence interval, lower limit = lower bound of the 95% CI, SE = standard error of mean, SMD = standardized mean difference, upper limit = upper bound of the 95% CI.
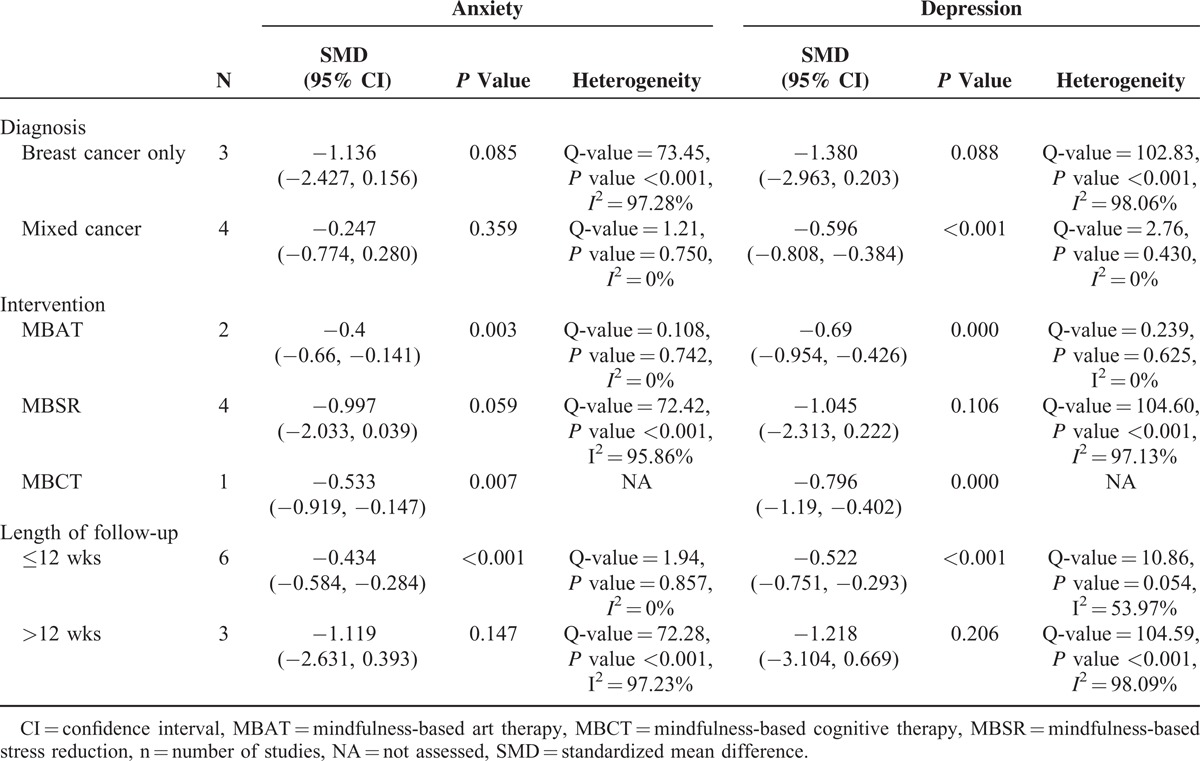
For the subgroup analysis, the pooled SMD revealed that there were significant differences between the mindfulness-based therapy and control groups with respect to the type of intervention (Table 4, supplementary Figure 2A, http://links.lww.com/MD/A506) and length of follow-up (≤12 weeks and >12 weeks; Table 4, Supplementary Figure 3A, http://links.lww.com/MD/A506). Specifically, mindfulness-based art therapy (pooled SMD = −0.40, 95% CI −0.66 to −0.14, P = 0.003) and mindfulness-based cognitive therapy (pooled SMD = −0.53, 95% CI −0.92 to −0.15, P = 0.007) were associated with significant improvement in anxiety. Regarding the duration of follow-up, mindfulness-based therapy was associated with significantly improved anxiety for follow-up ≤12 weeks after the start of the intervention (pooled SMD = −0.43, 95% CI −0.58 to −0.28, P < 0.001), but not for follow-up >12 weeks after the start of the intervention (pooled SMD = −1.119, 95% CI −2.63 to 0.393, P = 0.147). There were no significant effects of treatment when the data were stratified by cancer type (breast and mixed; Table 4, Supplementary Figure 1A, http://links.lww.com/MD/A506).
TABLE 4.
Subgroup Analysis
Meta-analysis of Depression
A total of 7 studies were included in the meta-analysis of the change in depression scores (Fig. 2B). As there was evidence of significant heterogeneity among the studies, a random-effects model of analysis was used (Q statistic = 105.95, I2 = 94.34%, P < 0.001). The pooled SMD indicated that depression was improved to a significantly greater extent in the mindfulness-based therapy group compared with the control group (pooled SMD = −0.90, 95% CI −1.53 to −0.26, P = 0.006).
For the subgroup analysis, mindfulness-based stress reduction was not associated with a significant change in depression for patients with breast cancer (Table 4, Supplementary Figure 1B, http://links.lww.com/MD/A506), but was associated with a significant improvement in depression for patients with the other cancer types (pooled SMD = −0.60, 95% CI −0.81 to −0.38, P < 0.001). Mindfulness-based art therapy (pooled SMD = −0.69, 95% CI −0.954 to −0.426, P < 0.001) and mindfulness-based cognitive therapy (pooled SMD = −0.80, 95% CI −1.19 to −0.40, P < 0.001) were associated with significantly decreased depression. Regarding the duration of follow-up, mindfulness-based therapy was associated with significantly decreased depression for follow-up ≤12 weeks after the start of the intervention (pooled SMD = −0.52, 95% CI −0.75 to −0.29, P < 0.001), but not for follow-up >12 weeks after the start of the intervention.
Sensitivity Analysis
Figure 3 shows forest plots of the SMD for anxiety (Fig. 3A) and depression (Fig. 3B), with individual studies removed, in turn, for the mindfulness-based versus control treatments. The direction and magnitude of the combined estimates did not change markedly with the exclusion of individual studies, indicating that the meta-analyses had good reliability.
FIGURE 3.
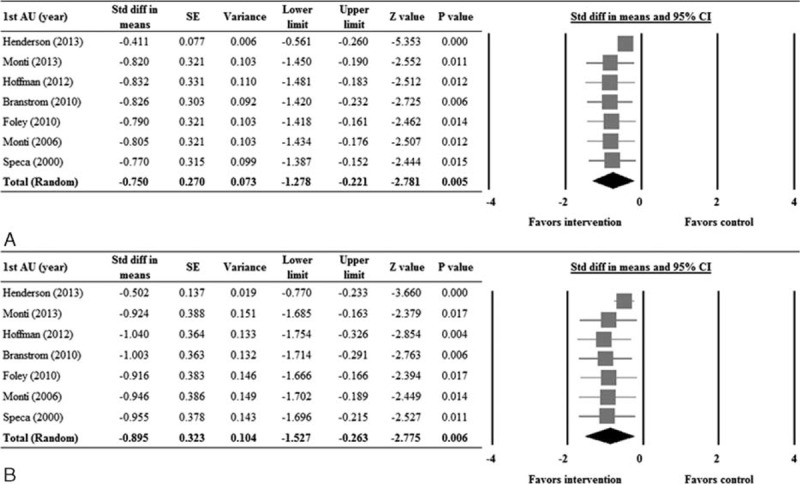
Forest plots of sensitivity analysis examining the influence of each study on the pooled estimate for anxiety (A) and depression (B). The leave-one-out approach was used. CI = confidence interval, lower limit = lower bound of the 95% CI, SE = standard error of mean, SMD = standardized mean difference, upper limit = upper bound of the 95% CI.
Quality Assessment
Figure 4 summarizes the results of the quality assessment. The vast majority of the studies were considered to have inadequate blinding of participants. Other study characteristics were generally considered to be associated with a low risk of bias.
FIGURE 4.
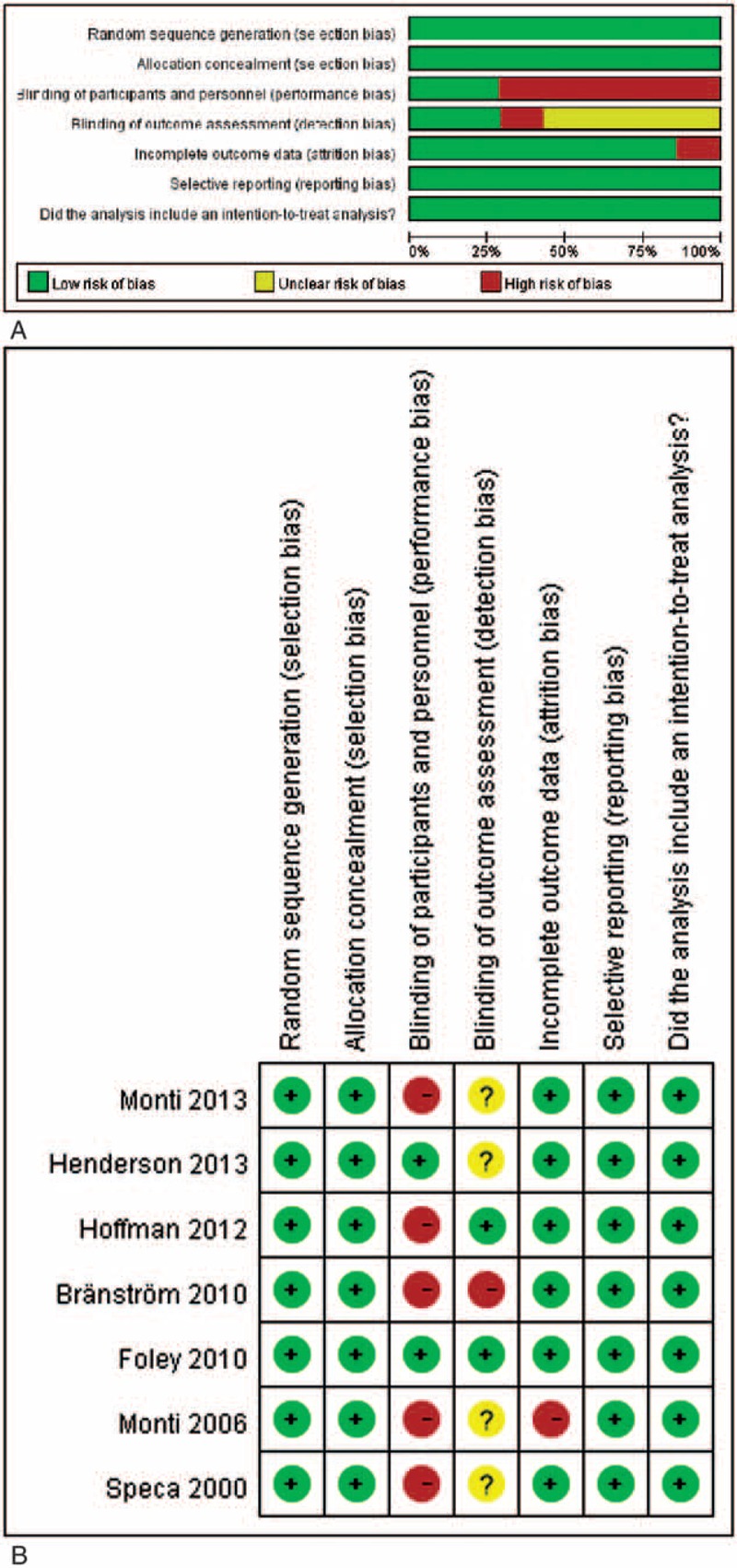
Quality assessment of studies: A, risk of bias graph; B, risk of bias summary.
Publication Bias
Figure 5 shows the Funnel plots for the studies reporting anxiety and depression scores. There was no evidence of publication bias among the studies reporting anxiety (P = 0.093) or depression (P = 0.043).
FIGURE 5.
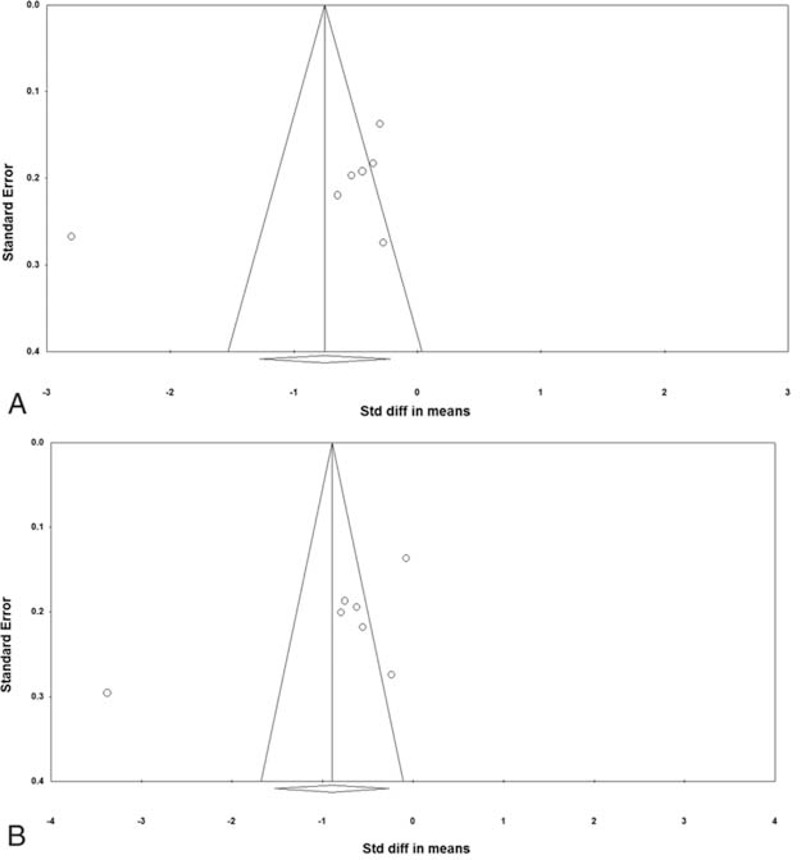
Funnel plots for publication bias: A, anxiety; B, depression.
DISCUSSION
In this meta-analysis, we examined the effects of mindfulness-based interventions on anxiety and depression in patients with cancer. A total of 7 RCTs (involving 888 participants) met the criteria for inclusion in the meta-analyses. Participants in most studies had breast cancer, whereas the type of mindfulness-based intervention varied between studies. However, our meta-analyses were found to be reliable, with no evidence of publication bias or study design biases (apart from the unavoidable lack of double-blinding).
Our overall findings indicated that mindfulness-based therapy is effective for reducing anxiety and depression, whereas our subgroup analysis findings indicated that this may depend on the type of therapy administered and that the effect of treatment may not last longer than 12 weeks.
The overall results of our meta-analyses revealed that mindfulness-based therapy significantly improved measures of anxiety and depression. Our findings are similar to those reported in several other recent meta-analyses on this topic. Specifically, in a meta-analysis of 9 studies, Zainal et al17 found that mindfulness-based stress reduction significantly reduced anxiety and depression in women with breast cancer. Only 2 of the 9 studies in the meta-analysis, however, were RCTs. Cramer et al16 similarly reported that mindfulness-based stress reduction reduced anxiety and depression in women with breast cancer in a meta-analysis of 3 RCTs; however, only postintervention changes, rather than the change from before to after the intervention, were considered. In another meta-analysis of 9 RCTs, Piet et al18 likewise found that mindfulness-based stress reduction or cognitive therapy significantly reduced both anxiety and depression among patients with cancer or survivors of cancer.
The duration of mindfulness-based therapy was 8 weeks in the majority of studies, whereas the timing of postintervention assessment(s) varied considerably. This variation in the timing of the assessment of benefit allowed us to perform subanalysis to assess the persistence of benefit with time. To this end, our subanalysis revealed that the effect of mindfulness-based therapy was significant at ≤12 weeks after the start of intervention, but not at >12 weeks after the start of the intervention. It should be noted, however, that only 2 studies incorporated longer term assessment of benefit. Therefore, we suggest that further studies, with a longer duration of follow-up, are needed to determine how long any beneficial effects of mindfulness-based therapy persist.
In addition to the overall findings, subgroup analysis revealed several significant effects of mindfulness-based therapy, most notably that both anxiety and depression were improved to a greater extent with mindfulness-based art therapy compared with control, whereas the reverse was true for mindfulness-based stress reduction. These findings suggest that the type of mindfulness-based therapy implemented is important and that some therapies may be effective, whereas others may not be effective. Our findings regarding anxiety and depression, and mindfulness-based cognitive therapy are consistent with of a number of other meta-analyses, notably those reported by Faller et al9 and Osborn et al,23 who found that cognitive behavioral therapy was effective for relieving anxiety and depression in participants who had survived cancer. In contrast to our findings, Galway et al10 found no such effects of different psychosocial interventions on anxiety or depression. This lack of an impact may reflect the fact that few studies were included in the analyses and that participants in the studies included in the meta-analysis were newly diagnosed and had not yet had time to develop marked anxiety or depression regarding their cancer. It is unclear why mindfulness-based stress reduction was found to have a negative impact on anxiety and depression in our meta-analysis.
Our meta-analysis has a number of limitations that warrant mention. Firstly, there was a lack of consistency between the studies in terms of the specific type of mindfulness-based intervention implemented and indeed the type of control intervention. This lack of consistency may have affected the overall results of our meta-analysis, and as such, our results must be interpreted with some degree of caution. Indeed, as suggested by the results of our subgroup analyses, it is possible that some mindfulness-based interventions may be effective for relieving anxiety and /or depression among patients with cancer, whereas others may not be effective. Secondly, although we presume that the patients in the studies included in our meta-analysis were not receiving potentially confounding medical or somatic treatment for anxiety or depression during the course of the study, we cannot rule out this possibility as no specific statements to this effect were provided in the reporting articles. Thirdly, we included studies involving patients with different forms of cancer, rather than a single form of cancer. Fourthly, the subgroup analyses only included a relatively small number of studies and thus cannot be considered definitive. Finally, although we carried out subgroup analyses to assess the effects of cancer type, form of therapy, and follow-up duration, we were not able to consider other factors that could impact the severity of anxiety and/or depression, such as time since diagnosis and stage of cancer. Clearly, additional well designed studies would be useful to definitively determine whether certain mindfulness-based therapies may provide some benefit to patients with cancer who are suffering anxiety and/or depression, and the impact of patient factors on treatment responsiveness. Despite these limitations, our study is strengthened by the fact that we restricted our analyses to results from high-quality studies (ie, RCTs). This is in contrast with other similar meta-analyses17,24 on this topic, which have also included non-RCTs. However, it would limit the number of eligible RCTs and total sample size (number of participants).
In conclusion, the results of our meta-analysis of RCTs suggest that mindfulness-based interventions can relieve anxiety and depression among patients with cancer. However, our subgroup analyses, although clearly limited by the small number of eligible studies, suggest that the effect of mindfulness-based therapy may not persist over the long term and that some forms of mindfulness-based interventions may be less effective for relieving anxiety and depression. Clearly, further research is warranted to more definitively determine which forms of mindfulness-based therapy may be effective in this context and how best to optimize the persistence of benefits obtained.
Footnotes
Abbreviations: CI = confidence interval, SMD = standardized mean difference.
M-FZ, Y-SW, and W-YL contributed equally towards the study.
Funding: This study was supported by grants from the Natural Science Foundation of Guangdong province (Grant No. S2011010003549) and Guangdong Provincial Department of Finance (No. 131171).
Conflicts of interests: The funding bodies played no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to declare.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.Moyer A, Sohl SJ, Knapp-Oliver SK, et al. Characteristics and methodological quality of 25 years of research investigating psychosocial interventions for cancer patients. Cancer Treat Rev 2009; 35:475–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antoni MH. Psychosocial intervention effects on adaptation, disease course and biobehavioral processes in cancer. Brain Behav Immun 2013; 30 Suppl:S88–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stanton AL. Psychosocial concerns and interventions for cancer survivors. J Clin Oncol 2006; 24:5132–5137. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 2011; 12:160–174. [DOI] [PubMed] [Google Scholar]
- 5.Zabora J, BrintzenhofeSzoc K, Curbow B, et al. The prevalence of psychological distress by cancer site. Psychooncology 2001; 10:19–28. [DOI] [PubMed] [Google Scholar]
- 6.Coyne JC, Lepore SJ, Palmer SC. Efficacy of psychosocial interventions in cancer care: evidence is weaker than it first looks. Ann Behav Med 2006; 32:104–110. [DOI] [PubMed] [Google Scholar]
- 7.Lepore SJ, Coyne JC. Psychological interventions for distress in cancer patients: a review of reviews. Ann Behav Med 2006; 32:85–92. [DOI] [PubMed] [Google Scholar]
- 8.Rodin G, Lloyd N, Katz M, et al. The treatment of depression in cancer patients: a systematic review. Support Care Cancer 2007; 15:123–136. [DOI] [PubMed] [Google Scholar]
- 9.Faller H, Schuler M, Richard M, et al. Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: systematic review and meta-analysis. J Clin Oncol 2013; 31:782–793. [DOI] [PubMed] [Google Scholar]
- 10.Galway K, Black A, Cantwell M, et al. Psychosocial interventions to improve quality of life and emotional wellbeing for recently diagnosed cancer patients. Cochrane Database Syst Rev 2012; 11:CD007064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shennan C, Payne S, Fenlon D. What is the evidence for the use of mindfulness-based interventions in cancer care? A review. Psychooncology 2011; 20:681–697. [DOI] [PubMed] [Google Scholar]
- 12.Foley E, Baillie A, Huxter M, et al. Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: a randomized controlled trial. J Consult Clin Psychol 2010; 78:72–79. [DOI] [PubMed] [Google Scholar]
- 13.Speca M, Carlson LE, Goodey E, et al. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med 2000; 62:613–622. [DOI] [PubMed] [Google Scholar]
- 14.Monti DA, Peterson C, Kunkel EJ, et al. A randomized, controlled trial of mindfulness-based art therapy (MBAT) for women with cancer. Psychooncology 2006; 15:363–373. [DOI] [PubMed] [Google Scholar]
- 15.Monti DA, Kash KM, Kunkel EJ, et al. Psychosocial benefits of a novel mindfulness intervention versus standard support in distressed women with breast cancer. Psychooncology 2013; 22:2565–2575. [DOI] [PubMed] [Google Scholar]
- 16.Cramer H, Lauche R, Paul A, et al. Mindfulness-based stress reduction for breast cancer-a systematic review and meta-analysis. Curr Oncol 2012; 19:e343–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zainal NZ, Booth S, Huppert FA. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: a meta-analysis. Psychooncology 2013; 22:1457–1465. [DOI] [PubMed] [Google Scholar]
- 18.Piet J, Wurtzen H, Zachariae R. The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: a systematic review and meta-analysis. J Consult Clin Psychol 2012; 80:1007–1020. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; 343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henderson VP, Massion AO, Clemow L, et al. A randomized controlled trial of mindfulness-based stress reduction for women with early-stage breast cancer receiving radiotherapy. Integr Cancer Ther 2013; 12:404–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoffman CJ, Ersser SJ, Hopkinson JB, et al. Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: a randomized, controlled trial. J Clin Oncol 2012; 30:1335–1342. [DOI] [PubMed] [Google Scholar]
- 22.Bränström R, Kvillemo P, Brandberg Y, et al. Self-report mindfulness as a mediator of psychological well-being in a stress reduction intervention for cancer patients: a randomized study. Ann Behav Med 2010; 39:151–161. [DOI] [PubMed] [Google Scholar]
- 23.Osborn RL, Demoncada AC, Feuerstein M. Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta-analyses. Int J Psychiatry Med 2006; 36:13–34. [DOI] [PubMed] [Google Scholar]
- 24.Ledesma D, Kumano H. Mindfulness-based stress reduction and cancer: a meta-analysis. Psychooncology 2009; 18:571–579. [DOI] [PubMed] [Google Scholar]


