Supplemental Digital Content is available in the text
Abstract
In this study, we describe a patient in whom tigecycline-induced drug fever and leukemoid reaction (LR) after 3 weeks of therapy for pneumonia.
A 62-year-old man developed aspiration pneumonia on February 1, 2015. He had received multiple antibiotics at another hospital, but did not respond well. Disease rapidly progressed, and he was referred to our department on February 14. We adjusted the antibiotic therapy to tigecycline + vancomycin, and added voriconazole to empiric antifungal therapy. Pneumonia largely improved, and we discontinued vancomycin and voriconazole on February 28. With tigecycline monotherapy, his clinical status remained stable.
On March 7, he developed high fever and LR (white blood cell count: 38.25 × 109/L). Erythrocyte sedimentation rate and C-reactive protein were elevated, and CD8+ T cells had been abnormally activated. After a careful physical examination and laboratory investigation, we confirmed that primary infection did not progress and no other cause was evident. So we figured fever and LR might be induced by tigecycline. After discontinuing tigecycline and adding low-dose steroid, fever and LR totally resolved in 3 days, which further confirmed our diagnosis.
According to this case and literature review, drug-induced hypersensitivity should be considered in the differential diagnosis of fever and LR when the therapeutic duration of tetracycline approximates 3 weeks. Monitoring T-cell subsets may facilitate early diagnosis. When necessary, we should discontinue the suspected drug to confirm diagnosis.
INTRODUCTION
Tigecycline, the first-in-class glycylcycline tetracycline antimicrobial agent, is the 9-t-butylglycylamido derivative of minocycline. With glycyl-amino substitutions at position 9, tigecycline has more broad-spectrum, anti-infective activities (Figure S1, http://links.lww.com/MD/A492). Clinically, adverse events of tetracycline antimicrobial agents commonly include gastrointestinal discomfort (nausea and vomiting), liver dysfunction, impairment of renal function, and so on. Drug fever and leukemoid reaction (LR) are rarely caused by tetracycline antibiotics, with only several cases reported to be associated with minocycline.1–4 Here, we describe a case in which fever and LR developed 3 weeks after initiation of tigecycline therapy for pneumonia. To the best of our knowledge, this is the first case report of tigecycline-induced drug fever and LR in the world. This study was approved by the Institutional Review Board of Peking Union Medical College Hospital. Informed consent has been obtained from the patient for publication of this case report.
CASE
A 62-year-old man developed pneumonia after vomiting and aspirating on February 1, 2015. Sputum culture was positive for Klebsiella pneumoniae (multidrug-resistant, sensitive to tetracycline). Chest computed tomography (CT) scan showed effusions in bilateral lower lobes, with the right side more significant, and bilateral pleural effusions (Figure S2A, http://links.lww.com/MD/A492). He had received piperacillin, tienam, teicoplanin, and sulperazone monotherapy or combination at another hospital, but did not respond well. Disease rapidly progressed. He developed type I respiratory failure and underwent tracheotomy on February 11, and was referred to our department 3 days later. Medical, family, and psychosocial history was not significant. On physical examination, he was weak and unconscious, with hyperthermic (38.7°C), hypertension (149/75 mm Hg), and tachypnea (30 beats per minute). Auscultation revealed that bilateral breath sounds were rough, and bilateral lower breath sounds were weak. We adjusted the antibiotic therapy to 50 mg tigecycline + 1 g vancomycin q12 h. Meanwhile, we added voriconazole 0.2 g q12 h to empiric antifungal therapy. He gradually came back to consciousness and his temperature normalized (37.3°C). Signs and symptoms of pneumonia largely improved. Repeat chest CT scan showed bilateral pleural effusions were less than before, but the remaining was unchanged (Figure S2B, http://links.lww.com/MD/A492). Vancomycin and voriconazole were discontinued on February 28. With tigecycline monotherapy, his clinical status remained stable.
On March 7, our patient developed scattered rash on both lower extremities, and his temperature reached 39.0°C on the same night (Fig. 1). His general status was well, and signs and symptoms of pneumonia did not worsen. His white blood cell (WBC) count was 38.25 x 109/L (from 13.34 × 109/L 1 d earlier), with 83.2% neutrophils, 0.2% eosinophils, and 9.8% lymphocytes (Fig. 1). Blood smear did not identify naïve blood cells. Erythrocyte sedimentation rate (ESR) was 58 mm/h and C-reactive protein (CRP) was 108 mg/L. Blood culture and T-SPOT.TB were both negative. G-test was <100 pg/mL. T-cell subsets showed CD8+ T cells were abnormally activated (CD8-DR 73.8%, CD8+CD38+ 94.0%). Repeat chest CT scan did not indicate any progression of the primary infection (Figure S2C, http://links.lww.com/MD/A492). Since fever and LR cannot be explained by primary infection and no other cause was evident after a careful physical examination and laboratory investigation, we figured fever and LR were induced by tigecycline, which was the only agent he was receiving at that time.
FIGURE 1.
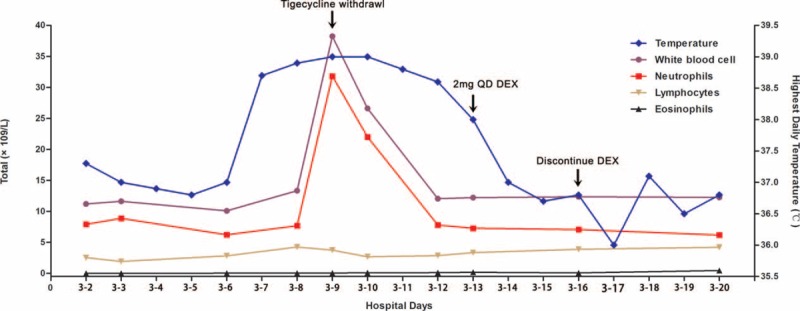
Highest daily temperature, white blood cell, total neutrophil, eosinophil, and lymphocyte counts during hospital stay. With tigecycline monotherapy, the clinical status of our patient remained stable for 1 week. On March 7, his temperature reached 39.0°C and he developed leukemoid reaction (LR) the next day. Since fever and LR cannot be explained by primary infection and no other cause was evident, drug hypersensitivity was suspected. We discontinued tigecycline and added dexamethasone 2 mg QD for 3 days. After that, his temperature and WBC count gradually normalized. QD = quaque die, WBC = white blood cell.
After discontinuing tigecycline on March 9, rash recessed, WBC count came down, and his temperature gradually came down in 48 hours, which is appropriate to the t1/2 of tigecycline (42.4 h); this helped to demonstrate that fever and LR were induced by tigecycline. Dexamethasone (DEX) 2 mg quaque die (QD) was added on March 13 for 3 days, and his temperature, WBC count, as well as inflammatory indexes, normalized a step further. High-resolution chest CT scan showed infiltrates of the right lung and right pleural effusion largely improved; pleural effusion on the left side was almost absent (Figure S2D, http://links.lww.com/MD/A492). He recovered and discharged on March 31. To this end, our patient fulfilled the criteria for drug fever and LR, which were induced by tigecycline. The patient was reported asymptomatic in our 3-month follow-up by telephone.
DISCUSSION
We report what we believe to be the first case report of tigecycline-induced drug fever and LR in the world. By literature review, we found several previous case reports of drug fever and LR induced by minocycline. It is reported that minocycline serves as a cytokine which induces neutrophil movement from bone marrow into the circulation and results in LR.1,3–5 In minocycline-related case reports, systemic reactions can be severe. Apart from high fever and LR, minocycline can also cause generalized eruption, exfoliative dermatitis, and severe hepatitis, which can be even fatal without timely and proper intervention.5 Since tigecycline and minocycline are both tetracycline derivatives and are similar in constructions (Figure S1, http://links.lww.com/MD/A492), it is reasonable to figure that they can induce similar hypersensitivities.
According to the characteristics of our patient and previous reported cases, when the therapeutic duration of tetracycline approximates 3 weeks, drug-induced hypersensitivity should be considered in the differential diagnosis of fever and LR. Those who are old in age and receive multiple drugs during the course of disease are at higher risk of developing hypersensitivity. Meanwhile, T-cell activation is related to tetracycline-induced hypersensitivity. Therefore, monitoring T-cell subsets may help to recognize hypersensitivity in early stage and facilitate the next diagnosis.4,6 When necessary, an attempt should be made to discontinue the suspected drug to confirm the diagnosis. It is also an option to add short-term low-dose steroid to facilitate inflammation recession, especially when the adverse event is severe and fatal.
Acknowledgments
Contributors: Q-QS, LQ, G-RR, and X-JM looked after the patient, and R-XC and Z-JL collected the data. All authors contributed to the report. Written consent to publication was obtained.
Footnotes
Abbreviations: CRP = C-reactive protein, CT = computed tomography, DEX = dexamethasone, ESR = erythrocyte sedimentation rate, LR = leukemoid reaction, WBC = white blood cell.
Q-QS and LQ contributed equally to this work.
Grant support: The Clinical Research Special Fund of Wu Jieping Medical Foundation (NO. 320.6750.14339), China.
Declaration of interests: All authors state that there is no conflict of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.Chatham WW, Ross DW. Leukemoid blood reaction to tetracycline. South Med J 1983; 76:1195–1196. [DOI] [PubMed] [Google Scholar]
- 2.Kaufmann D, Pichler W, Beer JH. Severe episode of high fever with rash, lymphadenopathy, neutropenia, and eosinophilia after minocycline therapy for ache. Arch Intern Med 1994; 154:1983–1984. [PubMed] [Google Scholar]
- 3.Parneix-Spake A, Bastuji-Garin S, Lobut J-B, et al. Minocycline as possible cause of severe and protracted hypersensitivity drug reaction. Arch Dermatol 1995; 131:490–491. [DOI] [PubMed] [Google Scholar]
- 4.MacNeil M1, Haase DA, Tremaine R, et al. Fever, lymphadenopathy, eosinophilia, lymphocytosis, hepatitis, and dermatitis: a severe adverse reaction to minocycline. J Am Acad Dermatol 1997; 36 (2 Pt 2):347–350. [DOI] [PubMed] [Google Scholar]
- 5.MacNeil M, Haase DA, Tremaine R, et al. Fever, lymphadenopathy, eosinophilia, lymphocytosis, hepatitis, and dermatitis: a severe adverse reaction to minocycline. J Am Acad Dermatol 1997; 36:347–350.(2 Pt 2). [DOI] [PubMed] [Google Scholar]
- 6.Guillon J-M, Joly P, Autran B, et al. Minocycline-induced cell-mediated hypersensitivity pneumonitis. Ann Intern Med 1992; 117:476–481. [DOI] [PubMed] [Google Scholar]


