Abstract
To compare the efficacy of simo decoction (SMD) combined with acupuncture at the tsusanli acupoint or chewing gum alone for treating postoperative ileus in patients with hepatocellular carcinoma (HCC) after hepatectomy.
In postoperative ileus, a frequent complication following hepatectomy, bowel function recovery is delayed, which increases length of hospital stay. Studies suggest that chewing gum may reduce postoperative ileus; SMD and acupuncture at the tsusanli acupoint have long been used in China to promote bowel movement.
Patients with primary HCC undergoing hepatectomy between January 2015 and August 2015 were randomized to receive SMD and acupuncture (n = 55) or chewing gum (n = 53) or no intervention (n = 54) starting on postoperative day 1 and continuing for 6 consecutive days or until flatus. Primary endpoints were occurrence of postoperative ileus and length of hospital stay; secondary endpoints were surgical complications.
Groups treated with SMD and acupuncture or with chewing gum experienced significantly shorter time to first peristalsis, flatus, and defecation than the no-intervention group (all P < 0.05). Hospital stay was significantly shorter in the combined SMD and acupuncture group (mean 14.0 d, SD 4.9) than in the no-intervention group (mean 16.5 d, SD 6.8; P = 0.014), while length of stay was similar between the chewing gum group (mean 14.7, SD 6.2) and the no-intervention group (P = 0.147). Incidence of grades I and II complications was slightly lower in both intervention groups than in the no-intervention group.
The combination of SMD and acupuncture may reduce incidence of postoperative ileus and shorten hospital stay in HCC patients after hepatectomy. Chewing gum may also reduce incidence of ileus but does not appear to affect hospital stay. (Clinicaltrials.gov registration number: NCT02438436.)
INTRODUCTION
Hepatectomy is widely used to treat patients with hepatocellular carcinoma (HCC), even those with intermediate and advanced disease.1,2 Despite its well-demonstrated clinical safety and efficacy in many patients, it is associated with postoperative morbidity and mortality.2,3 One complication after hepatectomy is delayed resumption of gastrointestinal function, known as postoperative ileus. This can decrease patient comfort and increase morbidity and mortality, prolonging hospital stay, and raising healthcare costs.4,5 While postoperative ileus usually resolves within approximately 3 days, it can last longer in some cases as a condition termed postoperative paralytic ileus.6 Postoperative use of opioid-based analgesics can increase incidence of postoperative ileus.7,8
No drugs or interventions to prevent or treat postoperative ileus have been approved by the China Drug Administration or the US Food and Drug Administration. Studies suggest that postoperative oral administration of simo decoction (SMD)9 and acupuncture10 can accelerate the return of gastrointestinal function following several types of surgery. Several studies also show that chewing gum, a new and simple modality, can accelerate complication-free recovery of gastrointestinal function following gastrointestinal surgery5,11 and obstetrical–gynecological surgery.12,13 This raises the question whether postoperative SMD, acupuncture, or chewing gum can reduce risk of postoperative ileus following hepatectomy.
To examine this question, we conducted a randomized controlled trial to compare incidence of postoperative ileus and length of hospital stay in HCC patients who received SMD and acupuncture, chewing gum or no intervention following hepatectomy.
METHODS
The protocol for this trial was approved by the Medical Ethics Committee of the Affiliated Tumor Hospital of Guangxi Medical University, and was designed in accordance with the Declaration of Helsinki. The trial was registered at Clinicaltrials.gov (NCT02438436). Data were collected, analyzed, and reported according to the Consolidated Standards of Reporting Trials (CONSORT) statement.
Patients
Patients older than 18 years who underwent open hepatectomy at 1 of the 2 Hepatobiliary Surgery Departments of the Affiliated Tumor Hospital of Guangxi Medical University (Nanning, China) were eligible to participate in the study. Diagnosis of HCC was based on 2 types of clinical imaging, together with a serum level of α-fetoprotein higher than 400 ng/mL; diagnosis was confirmed by histopathological examination of surgical samples. Patients were excluded if they had a history of exploratory laparotomy, laparoscopic surgery, inflammatory bowel disease, abdominal radiation, or substance abuse; if they had psychological or social conditions that might interfere with their participation in the study; if they were allergic to mint; or if they required intensive care more than 24 hours postoperatively or a nasogastric tube beyond the first postoperative morning.
Randomization
The study information was explained to all enrolled patients. After written informed consent was obtained, patients were assigned randomly to groups that would receive SMD combined with acupuncture or chewing gum or no intervention. Randomization was performed the day before hepatectomy using TenAlea software (http://nl.tenalea.net). The fundamentally different characteristics of SMD or chewing gum meant that no blinding was used after randomization. Patients were informed that the ability of SMD, acupuncture, or chewing gum to promote recovery of gastrointestinal function after hepatectomy was not known, and that none of these measures was expected to cause obvious side effects.
Interventions
The same surgical team performed all hepatectomies using general anesthesia, the same evidence-based protocol of perioperative management and standardized postoperative care plans.3,14,15 An abdominal cavity drainage tube was placed in each patient. The nasogastric drainage tube was removed on the first postoperative morning. Enteral or nasogastric feeding was not provided until after passage of first flatus. All patients were mobilized as soon as possible in the postoperative period. Additional opioid or nonsteroidal analgesia was prescribed for pain when required and their use carefully documented. Then nursing ward staff administered the following interventions to the randomized groups, recording their actions in patient records.
One group of patients received oral SMD decoction (Hansen Co., Ltd, Yiyang, Hunan Province, China, 10 mL/dose) 3 times per day beginning on the first day after hepatectomy. They also received bilateral injections of vitamin B1 (50 mg × 2) at the tsusanli acupoint 1 time per day after the skin was swabbed with 75% alcohol. This intervention was performed for a total of 6 consecutive days or until flatus.
Another group of patients was instructed to chew commercially available sugarless chewing gum (Extra & Reg, Wm. Wrigley Jr. Co., Ltd, Shanghai, China) 3 times daily starting on postoperative day 1. They were instructed to chew the piece of gum for 30 minutes. This intervention was performed for a total of 6 consecutive days or until flatus.
A third group did not receive any postoperative intervention, including SMD, acupuncture, chewing gum, or adjuvant drugs that might influence recovery of bowel function.
Outcomes
Primary endpoints were time to first flatus and time to defecation, which were recorded daily by nursing staff. Secondary endpoints were length of hospital stay and postoperative complications such as fever, pneumonia, wound infection, and bleeding. Length of hospital stay was defined as the number of days from hepatectomy to discharge. Criteria for hospital discharge included stability of vital signs with no fever, achievement of flatus or defecation, ability to tolerate solid food without vomiting, control of postoperative pain, absence of other postoperative complications, and ability to function at home independently or with the home care provided. Postoperative complications were classified and graded according to the Clavien–Dindo scheme.16
Sample Size Calculation
Sample size calculation was based on our previous retrospective study17 performed in patients with HCC after hepatectomy. Mean time to first flatus was assumed to be 73 and 51 hours between SMD combined with acupuncture and no-intervention group. The minimum detectable difference was 22. Assuming that the common standard deviation is 24 hours, the sample size was calculated to be a total of 171 participants applying statistical power of 90% at a 2-sided significance level of 5%. We recruited an additional 10 subjects to offset potential attrition.
Statistical Analysis
SPSS 19.0 (IBM, USA) was used for all statistical analyses, with the threshold of significance defined as a two-tailed P < 0.05. Data for continuous variables were expressed as median (range), while data for categorical variables were expressed as number (percentage). Intergroup differences in continuous variables were assessed for significance using Student t test (if data were normally distributed) or the Mann–Whitney U test (if data were skewed). Intergroup differences in categorical data were assessed using the χ2 test or Fisher exact tests (2-tailed), as appropriate. Length of hospital stay was calculated using Kaplan–Meier analysis and compared between groups using the log-rank test.
RESULTS
Patient Characteristics
From January 1, 2015 to August 31, 2015, 245 patients with HCC were assessed for eligibility. Of these, 43 were excluded because they did not meet the inclusion criteria, 16 refused to participate, 3 were unwilling to receive SMD and 2 were unwilling to receive chewing gum. The remaining 181 patients were randomly assigned to receive SMD with acupuncture (n = 62), chewing gum (n = 60), or no intervention (n = 59). After randomization, 7 patients diagnosed with cholangiocellular carcinoma were excluded. Another 5 patients were excluded because they had a prolonged stay in the intensive care unit and so could not receive SMD or chewing gum. Four patients discontinued the study and three received the incorrect intervention, so these 7 were excluded from the final analysis. In the end, 162 patients completed the study, comprising 55 in the SMD with acupuncture group, 53 in the chewing gum group, and 54 in the control group (Fig. 1).
FIGURE 1.
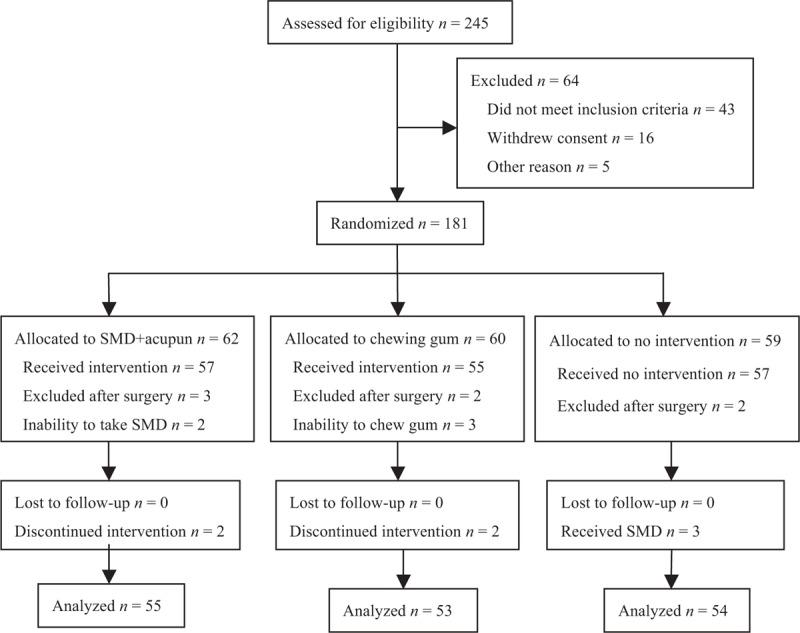
CONSORT diagram for the study. SMD + acupun, simo decoction with acupuncture.
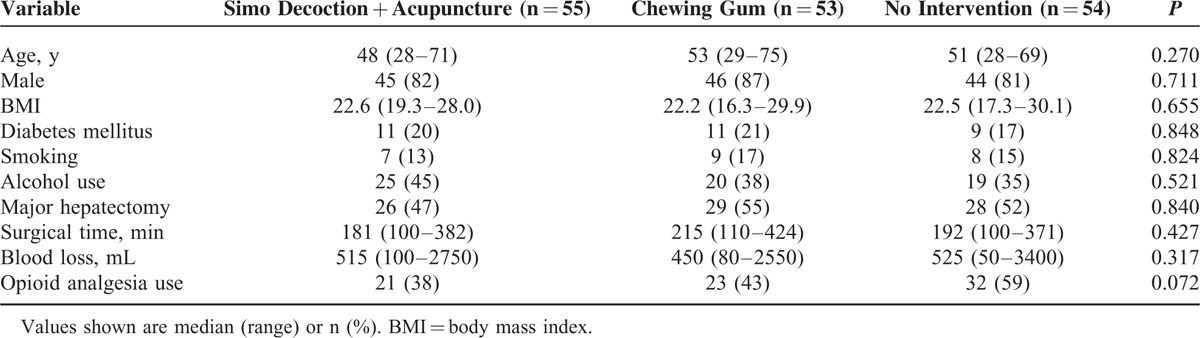
Patients in all 3 groups had similar hepatectomy characteristics, including major or minor hepatectomy, mean duration of surgery and blood loss (Table 1). No intervention-related adverse events more severe than grade I were recorded in any of the groups, based on the Common Terminology Criteria for Adverse Events 3.0.18
TABLE 1.
Clinicopathological Data of Patients With Hepatocellular Carcinoma Treated With Simo Decoction + Acupuncture, Chewing Gum, or No Intervention
Postoperative Ileus
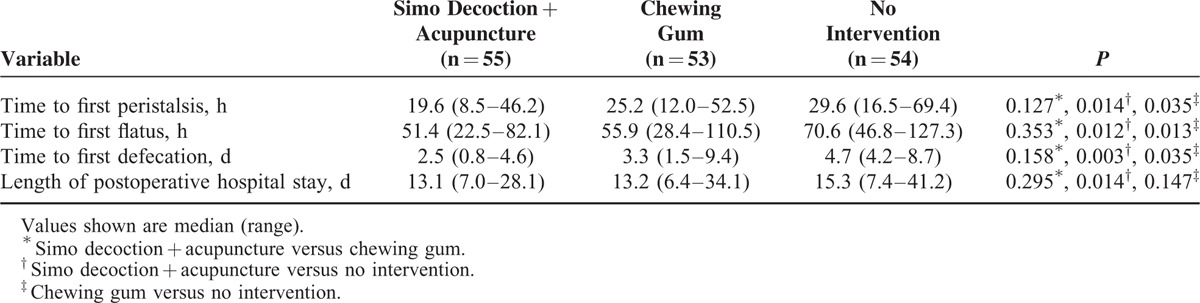
Time to first peristalsis, first flatus, and first defecation was significantly shorter in the 2 intervention groups than in the no-intervention group (all P < 0.05). All 3 time intervals were slightly shorter in the groups receiving SMD with acupuncture than in the group receiving chewing gum (all P > 0.05) (Table 2).
TABLE 2.
Outcomes of Postoperative Simo Decoction + Acupuncture or Chewing Gum in Patients With Hepatocellular Carcinoma
Length of Hospital Stay
Hospital stay lasted a mean of 14.0 d (SD 4.9, median 13) for patients receiving SMD with acupuncture, 14.7 d (SD 6.2, median 13) for patients receiving chewing gum, and 16.5 (SD 6.8, median 15) for no-intervention controls (Table 2). Kaplan–Meier analysis showed that length of stay was significantly shorter for SMD with acupuncture than for no intervention (P = 0.014) (Fig. 2). In contrast, length of stay was slightly shorter for the group receiving SMD with acupuncture than the group receiving chewing gum (P = 0.295), and it was slightly shorter for the group receiving chewing gum than for the group receiving no intervention (P = 0.147).
FIGURE 2.
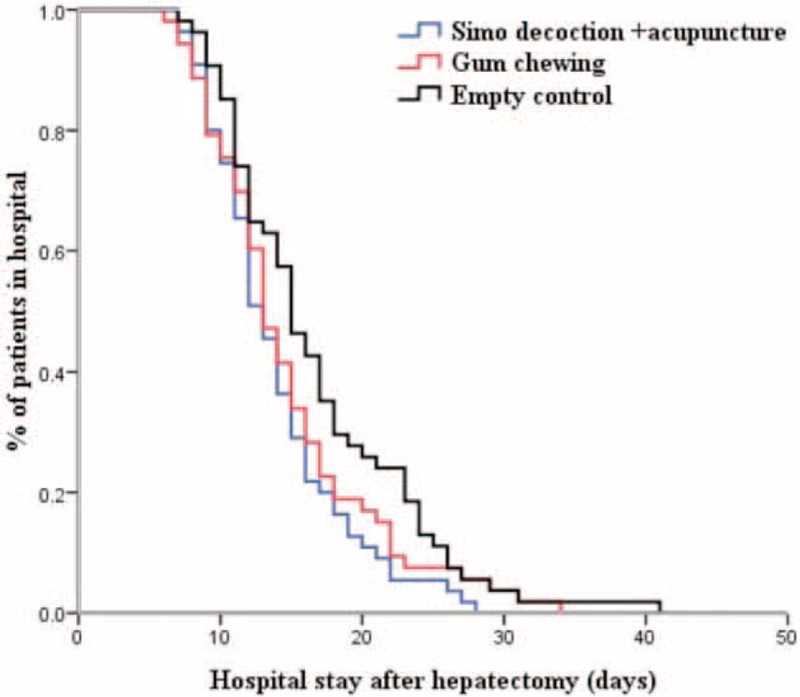
Kaplan–Meier curves showing length of hospital stay in the three groups. Significant differences were observed between the group receiving SMD with acupuncture and the control group receiving no intervention (P = 0.014), but not between the group receiving SMD with acupuncture and the group who chewed gum (P = 0.295), or between the group who chewed gum and the control group (P = 0.147).
Complications
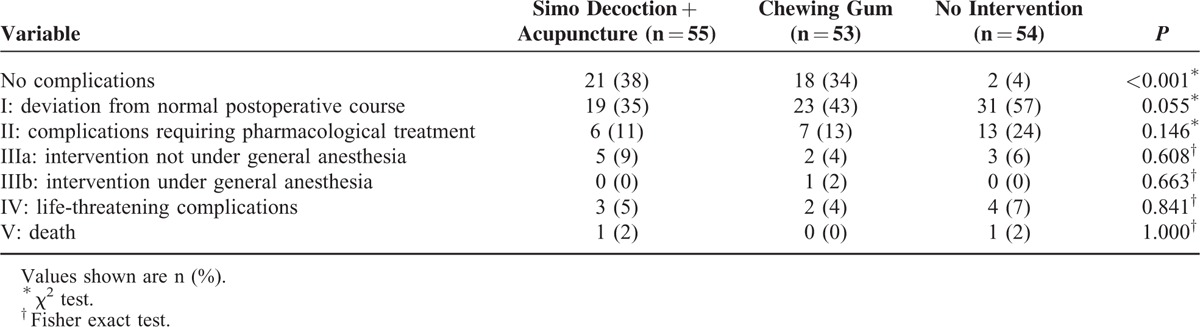
The frequency of complications was significantly higher in the no-intervention group than in the groups receiving SMD with acupuncture or receiving chewing gum (P < 0.001). Most complications were grade I or II and included wound pain, abdominal distension, fever, and hydrothorax. One patient in the chewing gum group required second surgery because of liver bleeding. One patient in the SMD with acupuncture group and 1 patient in the no-intervention group died within 30 d after hepatectomy because of liver failure (Table 3).
TABLE 3.
Clavien–Dindo Classification of Postresection Complications in Patients With Hepatocellular Carcinoma Treated With Simo Decoction + Acupuncture, Chewing Gum, or No Intervention
DISCUSSION
Although most hepatectomies do not involve gastrointestinal surgery, transient impairment of gastrointestinal motility known as postoperative ileus occurs in a substantial proportion of patients. This increases healthcare costs and resource utilization.19 Various strategies have been developed to reduce the incidence of postoperative ileus, including fast-track care, minimally invasive surgery, and epidural anesthesia, but none of these methods is entirely satisfactory.20 Our results suggest that the combination of SMD and acupuncture may reduce incidence of postoperative ileus and shorten hospital stay in HCC patients after hepatectomy. Chewing gum may also reduce incidence of ileus but does not appear to significantly affect hospital stay.
Our findings in this randomized controlled trial are consistent with our previous small retrospective study, in which SMD with acupuncture reduced incidence of postoperative ileus in HCC patients after hepatectomy.17 Our observation that chewing gum reduced the incidence of postoperative ileus is supported by findings in other randomized trials11–13 and meta-analyses,4,21 as well as a small prospective case–control study from South Korea in which HCC patients who chewed gum after hepatectomy recovered bowel function faster than those who did not.22 Thus the available evidence suggests that SMD combined with acupuncture may be the most promising strategy for reducing the incidence of postoperative ileus and shortening the length of hospital stay for HCC patients after hepatectomy. Incidence of grade I and II postoperative complications was significantly lower in the group receiving SMD with acupuncture than in the no-intervention group. We did not observe any adverse events related to SMD, acupuncture, or chewing gum in the present study, similar to the lack of adverse events in previous trials.10,17,21,23
Postoperative ileus may have multiple causes, though surgically induced intestinal inflammation appears to be the most frequent one.24,25 Inflammatory infiltration into the intestinal muscularis can lead to hypomotility along the entire gastrointestinal tract.26 Consistent with this, early inhibition of inflammation reduces the incidence of postoperative ileus,27,28 usually by vagus nerve-mediated activation of the autonomic nervous system.29,30 This may help explain why we observed that gum chewing promoted recovery of gastrointestinal function: chewing gum not only activates the cephalic-vagal reflex as a form of sham feeding,31 but it also reduces systemic inflammation.11
Whether SMD, long used in traditional Chinese medicine to boost gastrointestinal hypomotility, works by a similar mechanism is unclear. Evidence from animal models suggests that SMD can reduce serum levels of proinflammatory cytokines and white blood cells.32,33 That it may also directly promote gastrointestinal motility is suggested by the observation that it promotes contraction of antral circular strips by activating muscarinic M3 receptors.34 Acupuncture may help regulate the gastrointestinal tract via the autonomic nervous system,35,36 and acupuncture at the tsusanli acupoint, located on the stomach meridian, is thought to regulate the intestines. Administering vitamin B1 at acupoints is thought to intensify and prolong acupoint stimulation synergistically. This may help explain why we found that SMD with tsusanli acupoint injection with vitamin B1 promoted gastrointestinal hypomotility to a greater extent than chewing gum. The ability of tsusanli acupoint injection to reduce incidence of postoperative ileus has been demonstrated in numerous studies.10,23,36 We extend these findings to the combination of SMD with tsusanli acupoint injection.
In our population, SMD with acupuncture reduced hospital stay duration by 2.5 d, which was significant, while chewing gum reduced it by 1.8 d, which was not significant. It is possible that the effects of chewing gum would become significant with a larger sample. These results have several possible explanations. One is that either chewing gum or the combination of SMD with acupuncture stimulates gastrointestinal motility, leading to shorter time to first peristalsis, flatus, and defecation. Such patients will more quickly achieve euphagia without vomiting and start to ambulate. Another possible explanation is that the lower incidence of grade I and II postoperative complications in the 2 intervention groups translated to shorter hospital stay.
The results of the present study should be interpreted with caution given several limitations. One is that length of stay within each group was calculated over patients undergoing minor and major hepatectomies, which may have confounded the analysis. Nevertheless the frequencies of hepatectomy type were similar among the groups. A second limitation is lack of blinding, which was not feasible because of the nature of the interventions. A third limitation is that patients within each group differed in whether they received opioid analgesia, which may have confounded our analysis. Nevertheless, the frequencies of these treatments were similar among the groups.
In conclusion, the present study suggests that acupuncture, SMD, and chewing gum can be safely administered in a postoperative setting to HCC patients after hepatectomy. This is consistent with previous studies.10,17,21,23,36 Our data also suggest that gum chewing or the combination of SMD with acupuncture can prevent postoperative ileus in these patients, and that at least SMD with acupuncture significantly shortens hospital stay. Future studies should examine whether chewing gum or SMD with acupuncture can treat postoperative ileus after it has already developed.
ACKNOWLEDGMENT
The authors thank A. Chapin Rodríguez, PhD, for his language editing, which substantially improved the quality of the article.
Footnotes
Abbreviations: HCC = hepatocellular carcinoma, SMD = simo decoction.
Xue-Mei You, Xin-Shao Mo, and Liang Ma contributed equally to this work.
This work was supported by the National Science and Technology Major Special Project of the Ministry of Science and Technology of China (2012ZX10002010001009), the National Natural Science Foundation of China (81260331, 81160262, 81560460), the Guangxi University of Science and Technology Research Projects (KY2015LX056), the Self-Raised Scientific Research Fund of the Ministry of Health of Guangxi Province (GZPT1240, GZZC15-34, Z2015621, Z2014241), the Innovation Project of Guangxi Graduate Education (YCBZ2015030), and the Guangxi Science and Technology Development Projects (14124003-4).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Zhong JH, Ke Y, Wang YY, et al. Liver resection for patients with hepatocellular carcinoma and macrovascular invasion, multiple tumours, or portal hypertension. Gut 2015; 64:520–521. [DOI] [PubMed] [Google Scholar]
- 2.Zhong JH, Rodriguez AC, Ke Y, et al. Hepatic resection as a safe and effective treatment for hepatocellular carcinoma involving a single large tumor, multiple tumors, or macrovascular invasion. Medicine (Baltimore) 2015; 94:e396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhong JH, Ke Y, Gong WF, et al. Hepatic resection associated with good survival for selected patients with intermediate and advanced-stage hepatocellular carcinoma. Ann Surg 2014; 260:329–340. [DOI] [PubMed] [Google Scholar]
- 4.Noble EJ, Harris R, Hosie KB, et al. Gum chewing reduces postoperative ileus? A systematic review and meta-analysis. Int J Surg 2009; 7:100–105. [DOI] [PubMed] [Google Scholar]
- 5.Ho YM, Smith SR, Pockney P, et al. A meta-analysis on the effect of sham feeding following colectomy: should gum chewing be included in enhanced recovery after surgery protocols? Dis Colon Rectum 2014; 57:115–126. [DOI] [PubMed] [Google Scholar]
- 6.Marwah S, Singla S, Tinna P. Role of gum chewing on the duration of postoperative ileus following ileostomy closure done for typhoid ileal perforation: a prospective randomized trial. Saudi J Gastroenterol 2012; 18:111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gan TJ, Robinson SB, Oderda GM, et al. Impact of postsurgical opioid use and ileus on economic outcomes in gastrointestinal surgeries. Curr Med Res Opin 2015; 31:677–686. [DOI] [PubMed] [Google Scholar]
- 8.Koo KC, Yoon YE, Chung BH, et al. Analgesic opioid dose is an important indicator of postoperative ileus following radical cystectomy with ileal conduit: experience in the robotic surgery era. Yonsei Med J 2014; 55:1359–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chong T, Jin HB, Zhang JD, et al. [Clinical effects of the treatment of gastrointestinal dysfunction after stable thoracolumbar fractures with Simo decoction oral liquid]. Zhongguo Gu Shang 2010; 23:595–597. [PubMed] [Google Scholar]
- 10.Wang M, Gao YH, Xu J, et al. Zusanli (ST36) acupoint injection for preventing postoperative ileus: a systematic review and meta-analysis of randomized clinical trials. Complement Ther Med 2015; 23:469–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van den Heijkant TC, Costes LM, van der Lee DG, et al. Randomized clinical trial of the effect of gum chewing on postoperative ileus and inflammation in colorectal surgery. Br J Surg 2015; 102:202–211. [DOI] [PubMed] [Google Scholar]
- 12.Ertas IE, Gungorduk K, Ozdemir A, et al. Influence of gum chewing on postoperative bowel activity after complete staging surgery for gynecological malignancies: a randomized controlled trial. Gynecol Oncol 2013; 131:118–122. [DOI] [PubMed] [Google Scholar]
- 13.Jakkaew B, Charoenkwan K. Effects of gum chewing on recovery of bowel function following cesarean section: a randomized controlled trial. Arch Gynecol Obstet 2013; 288:255–260. [DOI] [PubMed] [Google Scholar]
- 14.Zhong JH, You XM, Lu SD, et al. Historical comparison of overall survival after hepatic resection for patients with large and/or multinodular hepatocellular carcinoma. Medicine (Baltimore) 2015; 94:e1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhong JH, Xiang BD, Gong WF, et al. Comparison of long-term survival of patients with BCLC stage B hepatocellular carcinoma after liver resection or transarterial chemoembolization. PLoS ONE 2013; 8:e68193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pang YH, Ma L, Mao CL, et al. Influence of acupoint therapy with simo decoction on postoperative gastrointestinal function recovery of primary liver cancer patients. J Nurs (China) 2013; 20 (3A):53–55. [Google Scholar]
- 18.Trotti A, Colevas AD, Setser A, et al. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol 2003; 13:176–181. [DOI] [PubMed] [Google Scholar]
- 19.Barletta JF, Senagore AJ. Reducing the burden of postoperative ileus: evaluating and implementing an evidence-based strategy. World J Surg 2014; 38:1966–1977. [DOI] [PubMed] [Google Scholar]
- 20.van Bree SH, Nemethova A, Cailotto C, et al. New therapeutic strategies for postoperative ileus. Nat Rev Gastroenterol Hepatol 2012; 9:675–683. [DOI] [PubMed] [Google Scholar]
- 21.Li S, Liu Y, Peng Q, et al. Chewing gum reduces postoperative ileus following abdominal surgery: a meta-analysis of 17 randomized controlled trials. J Gastroenterol Hepatol 2013; 28:1122–1132. [DOI] [PubMed] [Google Scholar]
- 22.Jang SY, Ju EY, Kim DE, et al. First flatus time and xerostomia associated with gum-chewing after liver resection. J Clin Nurs 2012; 21:2188–2192. [DOI] [PubMed] [Google Scholar]
- 23.Meng ZQ, Garcia MK, Chiang JS, et al. Electro-acupuncture to prevent prolonged postoperative ileus: a randomized clinical trial. World J Gastroenterol 2010; 16:104–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stoffels B, Hupa KJ, Snoek SA, et al. Postoperative ileus involves interleukin-1 receptor signaling in enteric glia. Gastroenterology 2014; 146:176.e1–187.e1. [DOI] [PubMed] [Google Scholar]
- 25.The FO, Bennink RJ, Ankum WM, et al. Intestinal handling-induced mast cell activation and inflammation in human postoperative ileus. Gut 2008; 57:33–40. [DOI] [PubMed] [Google Scholar]
- 26.Engel DR, Koscielny A, Wehner S, et al. T helper type 1 memory cells disseminate postoperative ileus over the entire intestinal tract. Nat Med 2010; 16:1407–1413. [DOI] [PubMed] [Google Scholar]
- 27.van Bree SH, Gomez-Pinilla PJ, van de Bovenkamp FS, et al. Inhibition of spleen tyrosine kinase as treatment of postoperative ileus. Gut 2013; 62:1581–1590. [DOI] [PubMed] [Google Scholar]
- 28.Lubbers T, Luyer MD, de Haan JJ, et al. Lipid-rich enteral nutrition reduces postoperative ileus in rats via activation of cholecystokinin-receptors. Ann Surg 2009; 249:481–487. [DOI] [PubMed] [Google Scholar]
- 29.The F, Cailotto C, van der Vliet J, et al. Central activation of the cholinergic anti-inflammatory pathway reduces surgical inflammation in experimental post-operative ileus. Br J Pharmacol 2011; 163:1007–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luyer MD, Greve JW, Hadfoune M, et al. Nutritional stimulation of cholecystokinin receptors inhibits inflammation via the vagus nerve. J Exp Med 2005; 202:1023–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stern RM, Crawford HE, Stewart WR, et al. Sham feeding. Cephalic-vagal influences on gastric myoelectric activity. Dig Dis Sci 1989; 34:521–527. [DOI] [PubMed] [Google Scholar]
- 32.Wang CX, Hou LB, Liu ST. Effect of Changtong oral liquid on serum cytokine concentrations in rats with postoperative intestinal adhesion. Di Yi Jun Yi Da Xue Xue Bao 2005; 25:601–604. [PubMed] [Google Scholar]
- 33.Wang CX, Hou LB, Ma Y. [Changtong oral liquid for prevention of postoperative intestinal adhesion: an experimental study]. Di Yi Jun Yi Da Xue Xue Bao 2005; 25:187–189.200. [PubMed] [Google Scholar]
- 34.Dai C, Liu N, Chen W, et al. Simo decoction promotes contraction of antral circular smooth muscle mainly via muscarinic M3 receptor. J Ethnopharmacol 2012; 144:270–276. [DOI] [PubMed] [Google Scholar]
- 35.Li Y, Tougas G, Chiverton SG, et al. The effect of acupuncture on gastrointestinal function and disorders. Am J Gastroenterol 1992; 87:1372–1381. [PubMed] [Google Scholar]
- 36.Ng SS, Leung WW, Mak TW, et al. Electroacupuncture reduces duration of postoperative ileus after laparoscopic surgery for colorectal cancer. Gastroenterology 2013; 144:307.e1–313.e1. [DOI] [PubMed] [Google Scholar]


