Abstract
The relationship between spinal sagittal alignment and pelvic parameters is well known in adolescent idiopathic scoliosis. However, few studies have reported the sagittal spinopelvic relationship after selective posterior fusion of thoracolumbar/lumbar (TL/L) curves.
We evaluated the relationship between spinal sagittal alignment and the pelvis, and analyzed how the pelvic sagittal state is adjusted in Lenke type 5C patients.
We conducted a retrospective study of 36 patients with Lenke type 5C curves who received selective posterior TL/L curve fusion. Coronal and spinopelvic sagittal parameters were pre and postoperatively compared. Pearson coefficients were used to analyze the correlation between all spinopelvic sagittal parameters before and after surgery. We also evaluated 3 pelvic morphologies (anteverted, normal, and retroverted) before and after surgery.
Preoperatively, the mean pelvic incidence was 46.0°, with a pelvic tilt and sacral slope (SS) of 8.2° and 37.8°, respectively, and 25% (9/36) of patients had an anteverted pelvis, whereas the other 75% had a normal pelvis. Postoperatively, 42% (15/36) of patients had a retroverted pelvis, 53% (19/36) had a normal pelvis, and 2 patients had an anteverted pelvis. Logistic regression analyses yielded 2 factors that were significantly associated with the risk for a postoperative unrecovered anteverted pelvis, including increased lumbar lordosis (LL) (odds ratio [OR] 4.8, P = 0.029) and increased SS (OR 5.6, P = 0.018). Four factors were significantly associated with the risk of a postoperative newly anteverted pelvis, including LL at the final follow-up (OR 6.9, P = 0.009), increased LL (OR 8.9, P = 0.003), LL below fusion (OR 9.4, P = 0.002), and increased SS (OR 11.5, P = 0.001).
The pelvic state may be adjusted after selective posterior TL/L curve fusion in Lenke 5C adolescent idiopathic scoliosis patients. It is difficult to improve an anteverted pelvis in patients who have an LL that is increased by more than 11.6° or an SS that is increased by more than 4.7° after surgery. The anteverted pelvic state will generally occur with posterior correction surgery for patients with an LL that is greater than 63.7°, or an LL or SS that is respectively increased by more than 17.6° or 9.0° postoperatively.
INTRODUCTION
Adolescent idiopathic scoliosis (AIS) is a complex 3-dimensional deformity that involves the coronal, sagittal, and axial planes. Satisfactory treatment for AIS includes maximum correction in the coronal plane, in addition to adequate restoration of the sagittal spinal alignment and vertebral rotation. Recent research has recognized the importance of sagittal balance and spinopelvic alignment in normal and disease states.1–3 Mac-Thiong et al4 evaluated the spinopelvic sagittal alignment in AIS and found that lumbar lordosis (LL) was strongly related to pelvic configuration, whereas the scoliotic curve type was not associated with a specific pattern of sagittal pelvic morphology or balance. Upasani et al also found that the sagittal contour of the lumbar spine was a strong association with the pelvic geometry. Roussouly et al6 proposed 3 pelvic sagittal states (anteverted, normal, and retroverted), and showed that corrective surgery with modern instrumentation can alter the pelvic alignment and create a slight pelvic retroversion, as manifested by an increase in pelvic tilt (PT) and a slight decrease in sacral slope (SS). Yang et al7 found that almost half of Lenke 5 patients who had AIS had an anteverted pelvis, which could not be corrected by posterior correction surgery when patients had a small PI or distal lower end vertebra.
Lenke type 5C AIS is characterized by a structural thoracolumbar/lumbar (TL/L) curve and a compensatory thoracic curve. The lumbar spine is closest to the pelvis, and similarly, LL is closely related to the pelvic orientation and is expressed by the SS, which is strongly influenced by pelvic incidence (PI).8 However, few studies have reported the influence of spinopelvic sagittal alignment in patients with Lenke 5C AIS after a single posterior lumbar curve correction. Li et al9 suggested that patients who have a preoperative thoracic curve <30° and a preoperative thoracic curve that bends <20° may benefit from selective posterior fusion. Similarly, we found that a large proportion of Lenke 5C patients had a significantly increased LL after surgery that may be associated with alteration of the spinopelvic sagittal alignment. The purpose of this study was to investigate the relationships among the spinopelvic sagittal parameters in Lenke 5C AIS patients who received selective posterior TL/L fusions.
METHODS AND MATERIALS
Setting and Patient Population
Between June 2011 and January 2013, 36 consecutive Lenke 5C AIS patients were treated with a 1-stage posterior TL/L spinal instrumentation and fusion. Study inclusion criteria included a >40° TL/L curve Cobb angle and no previous additional flexibility-modifying surgeries. Patients were aged between 12 and 19 years, and had a minimum of 2 years follow-up. On the basis of the Lenke et al10 classification scheme, 5 patients had “−” sagittal thoracic modifiers and no patients had “+” modifiers. All 36 cases used the Expedium (DepuySynthes) instrumentation system. All surgical procedures were performed by 1 senior surgeon. The study was approved by the hospital institutional review board.
Radiographic and Clinical Assessment
The radiographic assessment included preoperative and final follow-ups with postoperative standing posterior–anterior (PA) and lateral radiographs. Coronal radiographs were used for measuring the major TL/L curve Cobb angle, minor thoracic curve, coronal balance (CB), and radiographic shoulder height (RSH). CB was measured in millimeters by the C7 coronal plumb line lateral displacement from the central sacral vertical line. RSH is the perpendicular distance in the soft tissue shadow that is directly superior to the acromioclavicular joint. CB values were rated as coronal decompensation (CB >20 mm), satisfactory (CB ≤20 mm), and excellent (CB ≤10 mm). RSH was graded as significant imbalance (>30 mm), moderate imbalance (20–30 mm), minimal imbalance (10–20 mm), or balanced (<10 mm).
The spinopelvic sagittal radiographic parameters included measurements of thoracic kyphosis (TK), thoracolumbar junction (TLJ), LL, lumbar lordosis within fusion (LLWF), lumbar lordosis below fusion (LLBF), PI, SS, pelvic tilt (PT), and the sagittal vertical axis (SVA).
Thoracic kyphosis, TLJ, and LL are defined as the angle between lines from the T5 superior end plate and the T12 inferior end plate, the angle between lines drawn from the T10 superior end plate and the L2 inferior end plate, and the angle between lines from the T12 superior end plate and the S1 inferior end plate, respectively. LLWF is defined as the angle between the upper end plate of T12 and the lower end plate of the lowest instrumented vertebra. LLBF is defined as the angle between the lower end plate of the lowest instrumented vertebra and the upper end plate of S1. SVA is the distance between the posterosuperior point of the sacral plate and the plumb line from C7. A negative value indicated that the C7 plumb line was posterior to the sacrum posterior corner.
Pelvic incidence, SS, and PT are defined as the angles that are subtended by a line that is in the middle of the femoral head to the midpoint of the sacral endplate and a line that is perpendicular to the middle of the sacral endplate, the angle between a horizontal line and the sacrum's superior endplate, and the angle between the vertical line and the line joining the middle of the sacral endplate and the hip axis, respectively.
According to the pelvic positioning classification by Roussouly et al,6 the pelvis is anteverted when the PT is less than 20% of the PI/2, normal when the PT is between 20% and 80% of the PI/2, and retroverted when the PT is greater than 80% of the PI/2.
All radiographic parameters were manually measured by 2 investigators, who calculated the parameters’ average values. An experienced spine surgeon reviewed all patients’ medical records and plain radiographs.
Statistical Analyses
All parameters were analyzed using the SPSS statistical software v. 17.0 (Chicago, IL). Pre and postoperative radiographic parameters were compared using paired t tests. Pearson correlation coefficient was used for bivariate analyses. Correlation values were defined as follows: high, 0.80 to 1.00; marked, 0.60 to 0.79; moderate, 0.40 to 0.59; and low to none, <0.40.11 Logistic regression models were used for multivariate analyses of risk factors for a postoperative unrecovered anteverted pelvis and a newly anteverted pelvis. Statistical significance was defined as P < 0.05.
RESULTS
The study included 34 females (94.4%) and 2 males (5.6%). The mean age at the time of surgery was 15.7 ± 2.0 years. The mean follow-up time period was 2.3 ± 0.5 years. The Upper instrumented vertebra was located at T8 in 1 patient, T9 in 11 patients, T10 in 16 patients, and T11 in 8 patients. The Lowest instrumented vertebra (LIV) was located at L3 in 7 patients, L4 in 24 patients, and L5 in 5 patients.
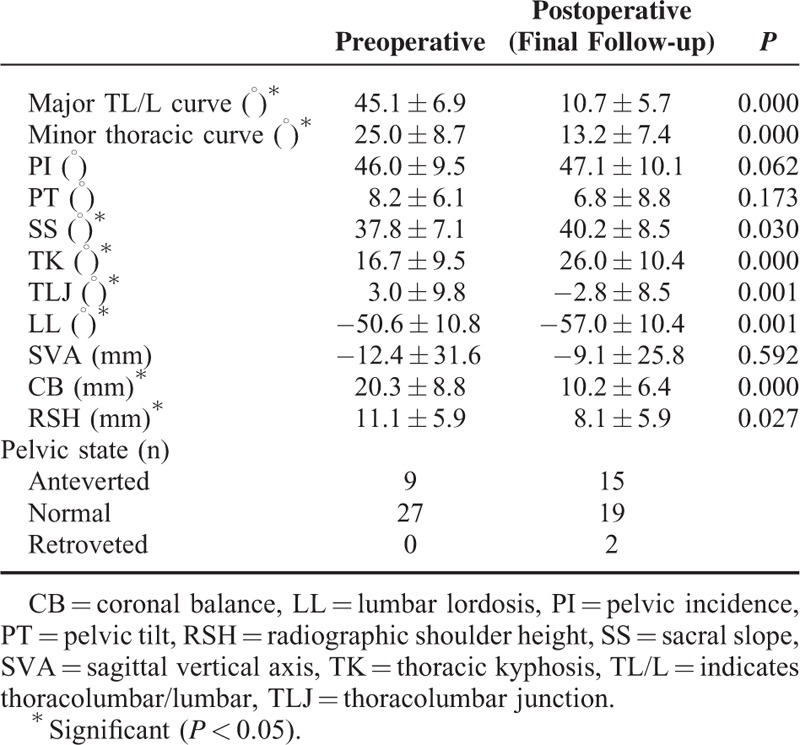
Preoperatively, the mean PI, PT, and SS were 46.0° ± 9.5°, 8.2° ± 6.1°, and 37.8° ± 7.1°, respectively. According to the pelvic positioning classification by Roussouly et al,6 25% (9/36) of the patients had an anteverted pelvis, whereas the remaining 75% had a normal pelvis. Postoperatively, the mean PI, PT, and SS were 47.1° ± 10.1°, 6.8° ± 8.8°, and 40.2° ± 8.5°, respectively. However, 42% (15/36) of the patients had a retroverted pelvis, 53% (19/36) of patients had a normal pelvis, and 2 patients had an anteverted pelvis. With respect to pre and postoperative differences in all radiographic parameters, there were no significant differences for PI, PT, and SVA, whereas significant differences were observed for SS, TK, TLJ, LL, CB, and RSH. The coronal balance and radiographic shoulder height of the coronal parameters showed marked improvement after surgery. Sagittal balance was stable after surgery (Table 1).
TABLE 1.
Mean Preoperative and Postoperative Radiographical Assessment of the Coronal and Sagittal Plane in all Lenke 5C Patients with AIS (n = 36)
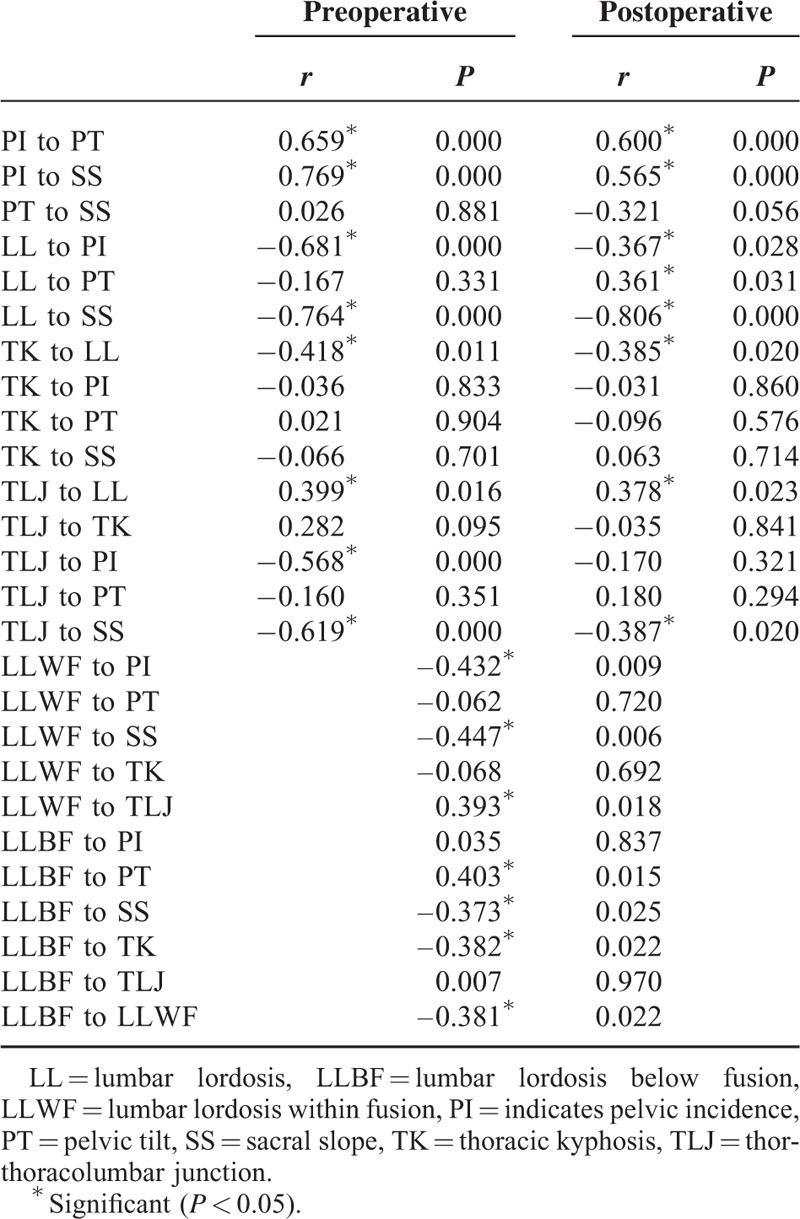
Pearson correlation analyses were also performed for all patients’ spinopelvic sagittal parameters. PI was related to PT and SS pre and postoperatively. However, there was no significant correlation between PT and SS. PI and SS were correlated with LL pre and postoperatively. LL was not related to PT preoperatively, but was slightly related to PT postoperatively. LLBF was related to PI, PT, and SS postoperatively. LLWF was related to PI and SS postoperatively. However, the correlation between LLWF and PT was not significant. There were no significant correlations between TK and the pelvic parameters pre or postoperatively. TK was significantly influenced by LL and LLBF. There was a negative correlation between LLWF and LLBF postoperatively. TLJ was associated with PI and SS preoperatively, but only with SS postoperatively. TLJ was significantly associated with LL pre and postoperatively. However, the correlation between TLJ and TK was not significant. TLJ was correlated with LLWF but not LLBF postoperatively (Table 2).
TABLE 2.
Spinopelvic Sagittal Parameters of the Pearson Correlation Analysis
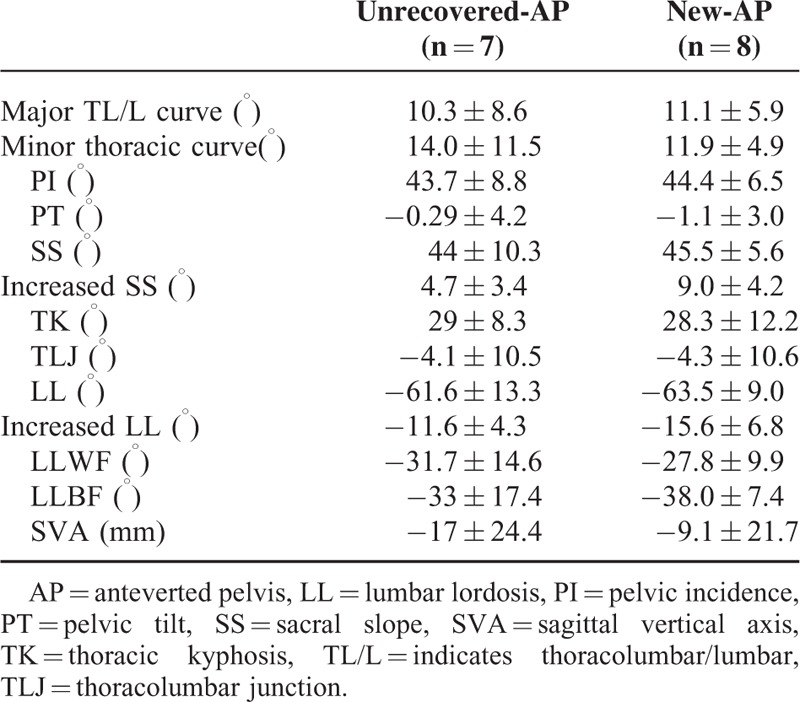
According to the pelvic state after surgery classification by Yang et al,7 2 patients had a recovered anteverted pelvis and 7 patients had a nonrecovered anteverted pelvis (unrecovered-AP). Eight patients had a new anteverted pelvis (new-AP) (Table 3). Logistic regression analyses yielded 2 factors that were significantly associated with the risk for a postoperative unrecovered anteverted pelvis: increased LL (odds ratio [OR] 4.8, 95%, P = 0.029) and increased SS (OR 5.6, 95%, P = 0.018). Four factors were significantly associated with the risk for postoperative new-AP, including postoperative LL (OR 6.9, 95%, P = 0.009), increased LL (OR 8.9, 95%, P = 0.003), LLBF (OR 9.4, 95%, P = 0.002), and increased SS (OR 11.5, 95%, P = 0.001) (Table 3).
TABLE 3.
Comparisons of Spinopelvic Parameters Between Patients With Unrecovered Anteverted Pelvis and With Newly Formed Anteverted Pelvis
DISCUSSION
An upright balanced posture is determined by spinal alignment and the pelvic state.12 The spine and pelvis interact with each other to minimize energy expenditure.13 Several studies have reported relatively wide variations in sagittal alignment and pelvic orientation with respect to age, sex, race, and coronal curve type morphology.4,14–16 However, few studies have addressed the influence of the spine's sagittal balance on pelvic morphology after surgery in AIS patients. Our study focused on the spinopelvic sagittal alignment that was affected by the selection of posterior fusion in Lenke 5C AIS.
Pelvic incidence is an important anatomical parameter that is unique for each individual and does not depend on position or spatial orientation, whereas SS and PT are directly related to pelvic position.8 Mac-Thiong et al4 reported pelvic measurements of 57.3° ± 13.8° for PI, 47.8° ± 9.3° for SS, and 9.5° ± 8.7°for PT in 160 patients who had AIS, and 58.6° ± 14.3° for PI, 48.2° ± 10.3° for SS, and 10.3° ± 9.1° for PT in the lumbar curve type. They showed that the pelvic parameters (PI, SS, and PT) did not significantly differ between the thoracic and lumbar curve types.4 Upasani et al5 also reported that the parameters (PI, SS, and PT) did not significantly differ between the thoracic and thoracolumbar curve patterns. Tanguay et al17 were the first to investigate the influence of pelvic geometry on LL in patients with AIS who were treated by posterior spinal instrumentation and fusion. However, they did not determine the pelvic parameter (PI, SS, and PT) values or the pelvic parameter variations after surgery.18 Roussouly et al6 found no significant difference for PI (53.0° ± 12.4° vs 53.5° ± 12.7°), but reported a significant difference for SS (42.0° ± 8.7° vs 41.1° ± 9.0°) and PT (11.1°± 8.1° vs 12.7° ± 8.5°) pre and postoperatively. Yang et al7 also compared pre and postoperative pelvic parameters in Lenke 5C patients who had AIS and found no significant difference for PI (44.3° ± 9.5° vs 44.2° ± 9.8°), but significant differences for SS (40.2° ± 6.3° vs 33.8° ± 5.5°) and PT (4.1°± 7.8° vs 10.4° ± 7.3°). In our study, there was a significant difference for SS (37.8° ± 7.1° vs 40.2° ± 8.5°), and no significant pre or postoperative differences for PI (46.0° ± 9.5° vs 47.1°± 10.1°) or PT (8.2° ± 6.1° vs 6.8° ± 8.8°). We also found that PI was a stable value that was not affected by surgery. Additionally, our study found that the PT value did not change significantly after surgery, which was not consistent with the research reviewed above.6,7 We believe that this difference may have been caused by the newly anteverted pelvis. PI is an individual anatomical parameter and a higher value is associated with greater capacity for pelvic compensation.8 Our PI value (46°) was not large enough; thus, it may be easier to achieve pelvic decompensation because the compensation ability is limited. Yang et al.7 also indicated that an abnormal pelvic sagittal state would not generally be corrected when patients have a small PI (less than 39°).
Several studies have demonstrated that PI is strongly related to PT and SS; however, there was no correlation between PT and SS in AIS patients.7,9,19 Our study had similar results. In addition, we found that PI maintained a strong correlation with PT and SS at the final follow-up. Nevertheless, there was no significant correlation between PT and SS after surgery. The relationships between PI and other sagittal parameters have been detailed in previous studies.2,4,5,15,18 Mac-Thiong et al4 and Yong et al20 reported that PI was strongly related to LL; however, there was no correlation between PI and KT. Upasani et al5 also reported that PI was related to LL; however, there was no correlation between PI and TK or TLJ. Our study indicated that PI was related to LL and TLJ and there was no correlation between PI and TK before surgery; however, a significant correlation was still observed between PI and LL and no correlation was observed between PI and TK or TLJ after surgery. Our study found that TK was not related to pelvic parameters (PI, SS, and PT) pre or postoperatively. The lumbar spine connects the pelvic and thoracic spine; thus, LL may be the compensatory mechanism for TK, which was not associated with pelvic parameters. Several studies have found that TK is related to LL in adolescents with and without idiopathic scoliosis.11,21,22 However, some studies have reported that TK was not correlated with LL in AIS patients.23 Legaye et al12 and Mac-Thiong et al4 found that TK was correlated with LL. However, few studies have reported the relationship between TK and LL after posterior instrumentation and fusion. Blondel et al24 found that TK was associated with LL at the final follow-up. Tanguary et al18 reported that TK had a significant influence on the preoperative, but not postoperative, LL. Our study showed that TK was preoperatively and postoperatively correlated with LL. We divided LL into LLBF and LLWF. Tanguary et al18 reported that no pelvic parameters influenced LLWF; however, PI and SS were correlated with the LLBF. We found that LLWF was correlated with the pelvic parameters PI and SS, whereas LLBF was related to the pelvic parameters PT and SS; in contrast, LLWF was negatively associated with LLBF. These results further indicate that pelvic morphology can be influenced by posterior instrumentation and fusion. We only selected patients who had a diagnosis of Lenke 5C AIS, which was corrected by a selective posterior fusion of the TL/L curves. Therefore, we consider that the pelvic state could be significantly influenced by the lumbar sagittal geometry after surgical correction.
The posterior surgery significantly adjusted the pelvic morphology. Preoperatively, 25% (9/36) of the patients had an anteverted pelvis, and postoperatively, 7 of 9 patients had an unrecovered anteverted pelvis (Fig. 1), whereas 2 recovered to normal (Fig. 2). Furthermore, 8 patients who had a preoperative normal pelvis had a newly anteverted pelvis (Fig. 3). The remaining 42% (15/36) of the patients had a postoperative anteverted pelvis, and 2 patients who had a preoperative normal pelvis had a retroverted pelvis after surgery (Fig. 4). Yang et al7 found that almost half of the patients evaluated had a preoperative anteverted pelvis, whereas 9 patients had a postoperatively nonrecovered anteverted pelvis. They also found that PI and LIV were strongly associated with the risk for a nonrecovered anteverted pelvis.7 Pelvic anteversion usually occurs in patients who have a smaller PI because a small PI is difficult to correct by surgery.7 Our study found that increased LL and SS were significantly associated with the risk for postoperative nonrecovered pelvic anteversion. LL was strongly related to SS pre and postoperatively.18 Thus, excessive LL corrections make it challenging to improve an anteverted pelvis. In the nonrecovered AP group, the increase in LL was 11.6° ± 4.3°, with an increase in SS of 4.7° ± 3.4° at follow-up. We also found that 4 factors—LL at follow-up, increased LL, LLBF, and increased SS—were significantly associated with the risk for postoperative new AP. LL at follow-up was strongly related to increased LL, LLBF, and increased SS. In the new-AP group, LL was 63.5° ± 9.0°, with an increase in LL of 15.6° ± 6.8° and an increase in SS of 9.0° ± 4.2° at follow-up. We consider that TL/L curve correction surgery using a pedicle screw can create new anteversion of the pelvis because of a decrease in PT and an increase in SS. Decreased PT compensated for correction of a larger LL, which maintained the sagittal alignment. In our study, 2 patients who had a preoperatively normal pelvis had a retroverted pelvis after surgery. According to these 2 patients’ data, there was a large Cobb angle of LL (72°), a small Cobb angle of LL after surgery (56.5°), and a large PI (65.5°). We believe that corrective surgery can create a retroverted pelvis, with an increase in PT coupled with a decrease in SS. The increased PT compensated for correction of a smaller LL for maintaining sagittal balance.
FIGURE 1.
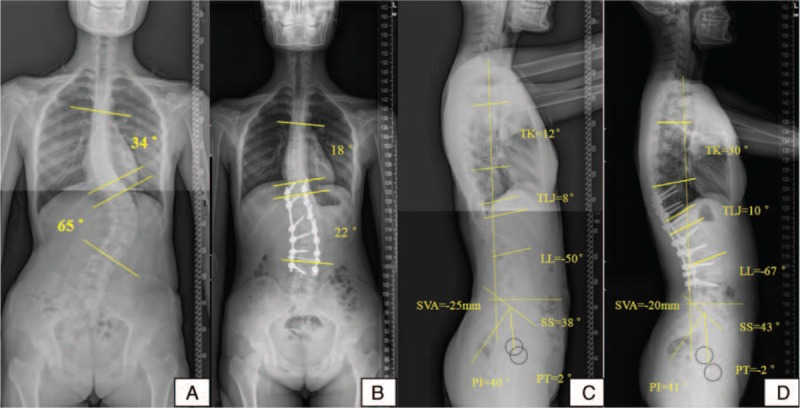
Preoperative and 2-year postoperative standing coronal and sagittal radiographs for a 17-year-old female with Lenke 5C AIS with an anteverted pelvis (not recovered by surgery). A, Preoperative coronal Cobb angle of the major TL/L curve of 65° from T11 to L3 and a 34° compensatory minor thoracic curve from T5 to T11. B, A 2-year postoperative standing coronal radiograph obtained after selective posterior instrumentation and fusion with pedicle screws from T10 to L4, showing a 23° major TL/L curve and a 22° noninstrumentation compensatory curve with a satisfactory coronal and shoulder balance. C, The preoperative sagittal alignment showed an anteverted pelvis with PT = 2°, which is smaller than 4.0° (20% PI/2). The preoperative LL was 50°. D, The 2-year postoperative pelvis showed nonrecovery of anteversion (PT = −2°). The LL was 67°. AIS = adolescent idiopathic scoliosis, PI = pelvic incidence, PT = pelvic tilt, SS = sacral slope, TL/L = thoracolumbar/lumbar.
FIGURE 2.
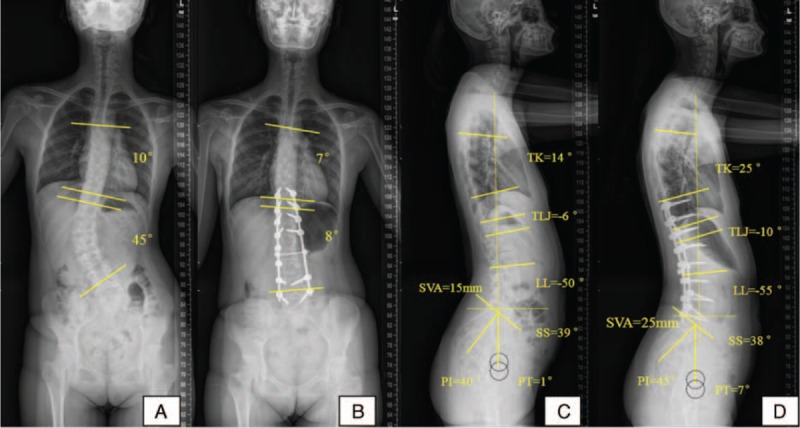
Preoperative and 2-year postoperative standing coronal and sagittal radiographs for a 16-year-old female with Lenke 5C AIS and an anteverted pelvis (recovered by surgery). A, Preoperative coronal Cobb angle of the major TL/L curve of 45° from T11 to L4 and a 10° compensatory minor thoracic curve from T5 to T11. B, A 2-year postoperative standing coronal radiograph obtained after selective posterior instrumentation and fusion with pedicle screws from T10 to L5, showing a 7° major TL/L curve and an 8° noninstrumentation compensatory curve with satisfactory coronal and shoulder balance. C, The preoperative sagittal alignment showed an anteverted pelvis with PT = 1°, which is smaller than 4.0° (20% PI/2). The preoperative LL was 50°. D, The 2-year postoperative pelvis showed recovery of anteversion (PT = 7°). The LL was 55°. AIS = adolescent idiopathic scoliosis, PI = pelvic incidence, PT = pelvic tilt, SS = sacral slope, TL/L = thoracolumbar/lumbar.
FIGURE 3.
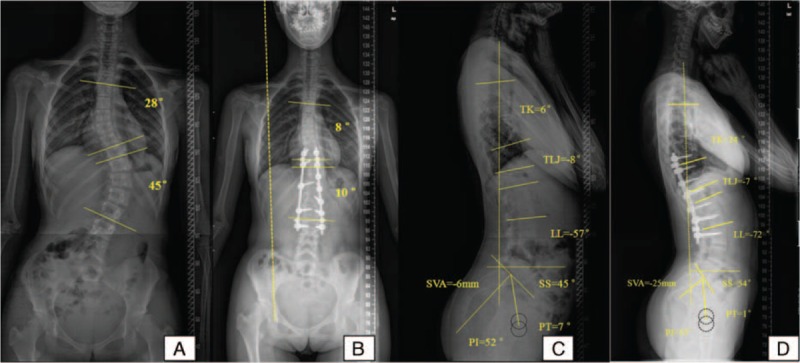
Preoperative and 2.3-year postoperative standing coronal and sagittal radiographs for a 15-year-old female with Lenke 5C AIS with a normal pelvis (anteverted pelvis by surgery). A, Preoperative coronal Cobb angle of the major TL/L curve of 45° from T10 to L2 and a 28° compensatory minor thoracic curve from T5 to T10. B, A 2.3-year postoperative standing coronal radiograph obtained after selective posterior instrumentation and fusion with pedicle screws from T9 to L3, showing a 10° major TL/L curve and an 8.0° noninstrumentation compensatory curve with satisfactory coronal and shoulder balance. C, The preoperative sagittal alignment showed a normal pelvic with PT = 7°, which is larger than 5.2° (20% PI/2). The preoperative LL was 57°. D, The 2.3-year postoperative pelvis showed anteversion (PT = 1°). The LL was 72°. AIS = adolescent idiopathic scoliosis, PI = pelvic incidence, PT = pelvic tilt, SS = sacral slope, TL/L, thoracolumbar/lumbar.
FIGURE 4.
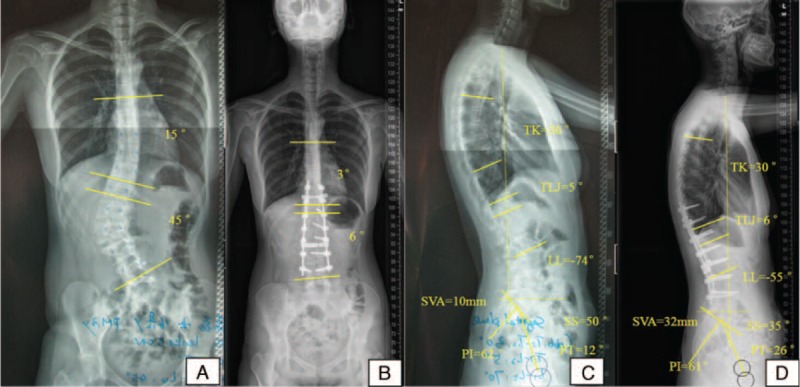
Preoperative and 3-year postoperative standing coronal and sagittal radiographs for a 16-year-old female with Lenke 5C AIS with a normal pelvis (retroverted by surgery). A, Preoperative coronal Cobb angle of the major TL/L curve of 45° from T12 to L4 and 15° compensatory minor thoracic curve from T7 to T12. B, A 3-year postoperative standing coronal radiograph obtained after selective posterior instrumentation and fusion with pedicle screws from T10 to L4, showing a 6° major TL/L curve and a 3° noninstrumentation compensatory curve with satisfactory coronal and shoulder balance. C, The preoperative sagittal alignment showed a normal pelvis with PT = 12, which is smaller than 6.2° (20% PI/2). The preoperative LL was 74°. D, A 3-year postoperative normal pelvis PT = 26, which is larger than 24.4°(20%PI/2). The LL was 55°. AIS = adolescent idiopathic scoliosis, PI = pelvic incidence, PT = pelvic tilt, SS = sacral slope, TL/L = thoracolumbar/lumbar.
There are several limitations in the current study. First, the number of patients who have Lenke 5C AIS with TL/L curves is relatively small. Second, this study was retrospective and had a relatively short follow-up period. However, the major strength of this study is the detailed description of the relationship between the sagittal balance and pelvic alignment before and after surgery. Moreover, pedicle screws were the only instrumentation method in every case, and all surgical procedures were performed by 1 senior surgeon. Nonetheless, a larger, longer follow-up study is necessary to further validate our findings.
In conclusion, the pelvic state may be altered after selective posterior fusion of TL/L (Lenke 5C) curves in idiopathic scoliosis. LL is pre and postoperatively correlated with pelvic parameters. Thus, it is important to evaluate LL and pelvic morphology before surgery to maintain or recover spinopelvic sagittal balance. However, we find that it is difficult to improve an anteverted pelvis in patients who have an increased of LL >11.6° or an increase of SS >4.7° after surgery. Anteversion of the pelvis will be created by posterior correction surgery when patients have an LL >63.5°, an increase of LL >15.6°, or an increase of SS >9.0°. Pelvic retroversion should be avoided when a large LL is corrected to be smaller than it was preoperatively by posterior selective TL/L curve instrumentation and fusion.
Footnotes
Abbreviations: AIS = adolescent idiopathic scoliosis, CB = coronal balance, LL = lumbar lordosis, LLBF = lumbar lordosis below fusion, LLWF = lumbar lordosis within fusion, PA = posterior–anterior, PI = pelvic incidence, PT = pelvic tilt, RSH = radiographic shoulder height, SS = sacral slope, SVA = sagittal vertical axis, TK = thoracic kyphosis, UIV = upper instrumented vertebra, LIV = lowest instrumented vertebra, TL/L = thoracolumbar/lumbar, TLJ = thoracolumbar junction.
X-MX, FW, X-YZ and Z-XL contributed equally to this work.
The authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
The authors report no conflicts of interest.
REFERENCES
- 1.Marty C, Boisaubert B, Descamps H, et al. The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J 2002; 11:119–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li W, Sun Z, Guo Z, et al. Analysis of spinopelvic sagittal alignment in patients with thoracic and thoracolumbar angular kyphosis. Spine (Phila Pa 1976) 2013; 38:E813–E818. [DOI] [PubMed] [Google Scholar]
- 3.Mac-Thiong JM, Labelle H, Berthonnaud E, et al. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J 2007; 16:227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mac-Thiong JM, Labelle H, Charlebois M, et al. Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine (Phila Pa 1976) 2003; 28:1404–1409. [DOI] [PubMed] [Google Scholar]
- 5.Upasani VV, Tis J, Bastrom T, et al. Analysis of sagittal alignment in thoracic and thoracolumbar curves in adolescent idiopathic scoliosis: how do these two curve types differ? Spine (Phila Pa 1976) 2007; 32:1355–1359. [DOI] [PubMed] [Google Scholar]
- 6.Roussouly P, Labelle H, Rouissi J, et al. Pre- and post-operative sagittal balance in idiopathic scoliosis: a comparison over the ages of two cohorts of 132 adolescents and 52 adults. Eur Spine J 2013; 22 suppl 2:S203–S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang X, Liu L, Song Y, et al. Pre- and postoperative spinopelvic sagittal balance in adolescent patients with Lenke type 5 idiopathic scoliosis. Spine (Phila Pa 1976) 2015; 40:102–108. [DOI] [PubMed] [Google Scholar]
- 8.La Maida GA, Zottarelli L, Mineo GV, et al. Sagittal balance in adolescent idiopathic scoliosis: radiographic study of spino-pelvic compensation after surgery. Eur Spine J 2013; 22 suppl 6:S859–S867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li M, Fang X, Sun Y, et al. Thoracic curve correction after posterior fusion and instrumentation of structural lumbar curves in patients with adolescent idiopathic scoliosis. Arch Orthop Trauma Surg 2011; 131:1375–1381. [DOI] [PubMed] [Google Scholar]
- 10.Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001; 83-A:1169–1181. [PubMed] [Google Scholar]
- 11.Franzblau A. A Primer of Statistics for Non-Statisticians. Edited. New York:Harcourt, Brace & World; 1958. [Google Scholar]
- 12.Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 1998; 7:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duval-Beaupère G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 1992; 20:451–462. [DOI] [PubMed] [Google Scholar]
- 14.Lonner BS, Auerbach JD, Sponseller P, et al. Variations in pelvic and other sagittal spinal parameters as a function of race in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010; 35:E374–E377. [DOI] [PubMed] [Google Scholar]
- 15.Berjano P, Langella F, Ismael MF, et al. Successful correction of sagittal imbalance can be calculated on the basis of pelvic incidence and age. Eur Spine J 2014; 23 Suppl 6:587–596. [DOI] [PubMed] [Google Scholar]
- 16.Schlösser TP, Vincken KL, Rogers K, et al. Natural sagittal spino-pelvic alignment in boys and girls before, at and after the adolescent growth spurt. Eur Spine J 2014. [DOI] [PubMed] [Google Scholar]
- 17.Tanguay F, Mac-Thiong JM, de Guise JA, et al. Relation between the sagittal pelvic and lumbar spine geometries following surgical correction of adolescent idiopathic scoliosis: a preliminary study. Stud Health Technol Inform 2006; 123:299–302. [PubMed] [Google Scholar]
- 18.Tanguay F, Mac-Thiong JM, de Guise JA, et al. Relation between the sagittal pelvic and lumbar spine geometries following surgical correction of adolescent idiopathic scoliosis. Eur Spine J 2007; 16:531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tanguay F, Mac-Thiong JM, de Guise JA, et al. Relation between the sagittal pelvic and lumbar spine geometries following surgical correction of adolescent idiopathic scoliosis. Eur Spine J 2007; 16:531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yong Q, Zhen L, Zezhang Z, et al. Comparison of sagittal spinopelvic alignment in Chinese adolescents with and without idiopathic thoracic scoliosis. Spine (Phila Pa 1976) 2012; 37:E714–E720. [DOI] [PubMed] [Google Scholar]
- 21.Mac-Thiong JM, Berthonnaud E, Dimar JR2nd, et al. Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976) 2004; 29:1642–1647. [DOI] [PubMed] [Google Scholar]
- 22.Jackson RP, Peterson MD, McManus AC, et al. Compensatory spinopelvic balance over the hip axis and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine (Phila Pa 1976) 1998; 23:1750–1767. [DOI] [PubMed] [Google Scholar]
- 23.Vedantam R, Lenke LG, Keeney JA, et al. Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine (Phila Pa 1976) 1998; 23:211–215. [DOI] [PubMed] [Google Scholar]
- 24.Blondel B, Lafage V, Schwab F, et al. Reciprocal sagittal alignment changes after posterior fusion in the setting of adolescent idiopathic scoliosis. Eur Spine J 2012; 21:1964–1971. [DOI] [PMC free article] [PubMed] [Google Scholar]


