This review provides an overview about what is known about breast cancer incidence and mortality in LMICs, with a focus on sub-Saharan Africa. It discusses the implications of these trends for breast cancer early detection and treatment strategies and identifies what is currently known about delivery of such care in LMICs. It focuses on the limitations of the existing data and areas in which high-quality research is most needed.
Keywords: Breast cancer, Developing countries, Low- and middle-income countries, Sub-Saharan Africa
Abstract
The objective of this review is to describe existing data on breast cancer incidence and mortality in low- and middle-income countries (LMICs), in particular in sub-Saharan Africa; identify the limitations of these data; and review what is known about breast cancer control strategies in sub-Saharan African countries and other LMICs. Available estimates demonstrate that breast cancer incidence and mortality are rising in LMICs, including in Africa, although high-quality data from LMICs (and particularly from sub-Saharan Africa) are largely lacking. Case fatality rates from breast cancer appear to be substantially higher in LMICs than in high-income countries. Significant challenges exist to developing breast cancer control programs in LMICs, perhaps particularly in sub-Saharan Africa, and the most effective strategies for treatment and early detection in the context of limited resources are uncertain. High-quality research on breast cancer incidence and mortality and implementation research to guide effective breast cancer control strategies in LMICs are urgently needed. Enhanced investment in breast cancer research and treatment in LMICs should be a global public health priority.
Implications for Practice:
The numbers of new cases of breast cancer, and breast cancer deaths per year, in low- and middle-income countries are rising. Engagement by the international breast cancer community is critical to reduce global disparities in breast cancer outcomes. Cancer specialists and institutions in high-income countries can serve as key partners in training initiatives, clinical care, protocol and program development, and research. This article provides an overview of what is known about breast cancer incidence, mortality, and effective strategies for breast cancer control in sub-Saharan Africa and identifies key gaps in the literature. This information can help guide priorities for engagement by the global cancer community.
Introduction
The global burden of cancer is growing as the world’s population undergoes significant demographic and epidemiologic transitions, with a decreased burden of infectious diseases, longer life expectancies, and shifts in cancer risk factors [1–3]. These transitions have intensified global interest in and concern about cancer in low- and middle-income countries (LMICs), including in sub-Saharan Africa, where resources and infrastructure for cancer care and control are particularly nascent and cancer outcomes are dismal. As the most common cancer among women worldwide [1], breast cancer is an area of particular global concern. In this review, we provide an overview about what is known about breast cancer incidence and mortality in LMICs, with an emphasis on sub-Saharan Africa. We then review the implications of these trends for breast cancer early detection and treatment strategies and identify what is currently known about delivery of breast cancer care in LMICs. We focus on the limitations of the existing data and areas in which high-quality research is most needed.
Trends in Incidence of Breast Cancer in LMICs
Data on cancer incidence in the developing world are extremely limited. Although the GLOBOCAN project, run by the International Agency for Research on Cancer (http://www.iarc.fr), is an important and widely used resource for estimates of global cancer incidence and mortality, the quantity and quality of data from countries designated as low- or middle-income by the World Bank [4] are generally low. The dearth of high-quality data is particularly apparent for sub-Saharan Africa.
Ideally, cancer incidence in a given country is calculated according to data from population-based cancer registries (PBCRs); however only 2% of Africa’s population is covered by high-quality cancer incidence data from PBCRs [1]. Of the 48 countries or territories with the two highest-quality categories of data, 8 are designated as middle-income by the World Bank [4]. None are low-income, and none are in Africa. For countries in which national or regional registries are not available or are of insufficient quality to provide national incidence rates, GLOBOCAN estimates are derived in a variety of ways: (a) They are estimated from national mortality rates (when available) and modeled survival from breast cancer in that country; (b) they are estimated from weighted averages of subnational registries, or from a single subnational registry, when available; or (c) they are derived from average incidence from neighboring countries when no adequate-quality in-country data are available [1].
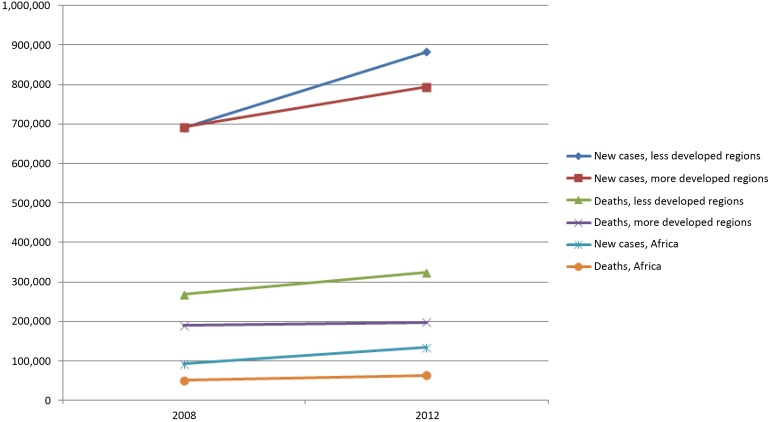
Despite their currently unavoidable reliance on estimates and models for many countries, GLOBOCAN data are widely regarded as the best estimates available. GLOBOCAN estimates suggest that breast cancer is the second most common cancer in the world (after lung cancer) and the most common cancer among women. In Africa overall, breast cancer is the most common cancer among women, although in East Africa the estimated incidence of cervical cancer appears higher than that of breast cancer [1]. Although age-standardized breast cancer incidence rates are lower in lower-income compared with higher-income countries [5], in 2012 the number of new breast cancer cases in less developed countries (883,000) was higher than the number of new cases in more developed countries (794,000) (Fig. 1). In contrast, incidence estimated by GLOBOCAN were almost equal in developed and developing regions in 2008 (691,000 cases in developing countries and 692,000 in developed countries) (Fig. 1) [6]. In Africa overall, the estimated number of new cases was 92,600 in 2008 and 133,900 in 2012 [1, 6].
Figure 1.
GLOBOCAN estimates of breast cancer incidence and mortality worldwide and in Africa in 2008 and 2012. Data obtained from [1, 6].
GLOBOCAN authors note that caution should be exercised in drawing conclusions about trends from these numbers, given changes in data sources and methods over time and the inherent limitations of the data [1]. However, comparison of 2008 and 2012, and a more detailed analysis of GLOBOCAN breast cancer rates among 39 countries with PBCR data [7], demonstrate that both the number of incident cases and age-specific incident rates in LMICs are rising. This finding is consistent with findings from a modeling-based study of cervical and breast cancer incidence and mortality worldwide [8] and with findings from the Global Burden of Disease project [9]. Overall increasing incidence reflects population growth and aging as well as increasing age-specific incidence rates [9]. Rising incidence rates may reflect shifts in other risk factors known to increase breast cancer risk in developed countries, including lower fertility rates, as well as body mass index and a “Western” diet [10–12]. Despite the plausibility of these shifts in distributions of risk factors, more data are needed to confirm these associations in LMICs, including in sub-Saharan African countries. Furthermore, the role of increasing awareness about breast cancer or greater access to diagnostic services, leading to more breast cancer diagnoses in LMICs, is unclear.
Breast Cancer Mortality in LMICs
Cancer mortality statistics are as limited as incidence data in LMICs, especially in Africa and Asia, where comprehensive death registration systems are often lacking [1]. In GLOBOCAN 2012, of the 71 countries or territories with data sources in the top-two quality categories, 24 are middle-income, none are low-income, and none are in Africa [1, 4]. In the cases (83 of 184 countries) in which national mortality data were not available for GLOBOCAN 2012, mortality was modeled by using cancer-specific 5-year survival rates adjusted by a country’s level of human development, as measured by the Human Development Index; in 3 countries, mortality rates from neighboring countries were used instead [1]. GLOBOCAN mortality estimates suggest that although breast cancer is the the leading cause of cancer deaths among women in less developed countries overall (324,000 deaths in 2012), in eastern, middle, and southern Africa it is the second leading cause of cancer deaths among women (27,000 deaths), after cervical cancer.
Overall, case fatality rates for breast cancer (which can be approximated by mortality/incidence ratios) appear to be significantly higher in LMICs than in high-income countries. In a recent analysis of 2012 GLOBOCAN data, mortality/incidence ratios ranged from 0.55 in Central Africa to 0.16 in the U.S. [7]. Mortality rates appear to be rising in some LMICs, whereas they decline in most high-income countries [7]; the increasing rates probably reflect rising incidence rates as well as late-stage diagnoses and limited access to treatment in LMICs. A range of facility-based studies from LMICs convey the extent to which women present with late stage disease in low-resource settings. For example, in retrospective cohort studies, women with stage III and IV disease made up 77% of patients with breast cancer at Mulago Hospital in Uganda [13]; 77% of patients at Butaro Cancer Center of Excellence in Rwanda [14]; and 78% of breast cancer patients at the Angolan Institute of Cancer Control [15].
Diagnostic delays appear to be an important cause of late-stage diagnoses in LMICs. A growing number of small studies have examined the diagnostic and treatment delays and barriers to care experienced by breast cancer patients in LMICs, including in sub-Saharan Africa [16–21]; these demonstrate that patients experience long delays between initial symptoms and presentation at a health facility (patient delay) and then between first presentation and definitive diagnosis or treatment (provider delay). At two facilities in Rwanda, delay between initial development of symptoms and ultimate receipt of a diagnosis was 15 months; patient and provider delays were equally long, and both appeared to contribute to late-stage disease [21]. Reasons for patient delays cited in studies from sub-Saharan Africa include patients’ lack of awareness of breast cancer symptoms and their seriousness [20–23], fear of a cancer diagnosis [21, 23], use of traditional healers [21–23], and financial concerns about treatment [20, 21]. Provider delays have been less extensively investigated in LMICs, including in sub-Saharan Africa, but lack of breast cancer experience and knowledge among primary care clinicians and limited access to tertiary centers are some of the probable contributors.
Treatment of Breast Cancer in LMICs
Because in high-resource countries early breast cancer is a largely curable disease, advanced-stage presentations and high mortality rates in LMICs have led to intense interest in promoting breast cancer screening and early detection in these settings. However, before development of any early-detection strategies, adequate referral, diagnosis, and treatment programs must be in place to ensure that high-risk women identified through screening and early detection have access to high-quality diagnostic services (imaging and pathology) and effective treatment [24]. The Disease Control Priorities Project, a global initiative funded by the Bill & Melinda Gates Foundation and coordinated by the University of Washington, has identified treatment of early breast cancer as part of a set of essential cancer interventions for LMICs that could be “effective, cost-effective, affordable, and feasible,” along with tobacco control, human papillomavirus and hepatitis B virus vaccinations, cervical cancer screening, surgery to treat bowel obstruction from colorectal cancer, and treatment of select pediatric cancers [25]. Groups such as the Breast Health Global Initiative [26] have worked to identify key steps in developing breast cancer treatment programs tailored to existing resources, and breast cancer treatment is available at centers in many LMICs, including countries in sub-Saharan Africa. However, detailed guidance on steps to actually implement such programs in low-resource settings is scant, and there are few studies from LMICs, particularly sub-Saharan Africa, that evaluate long-term outcomes from treatment protocols used in these settings [13, 27].
One crucial challenge in breast cancer treatment in sub-Saharan Africa is the scarcity of health professionals with training in cancer diagnosis and care. Pathologists (and high-quality and reliable pathology laboratories) and medical oncologists are rare, especially in the poorest countries [28, 29]. Recent studies indicate that partnerships with pathologists based remotely may help ease the shortage of pathologists and build pathology capacity in rural areas [30, 31]. Skilled surgical oncology services are of vital importance in treatment of early breast cancer [25], but human resource capacity, associated services such as imaging, and financing for these services are highly limited in many sub-Saharan African countries. It has been estimated that of the 15 million cancer cases estimated to occur by the end of 2015, about 80% will require surgical oncologic care, and 75% of these (mostly in LMICs) will not receive safe, affordable, and timely surgical services [32]. Surgical capacity-building is increasingly recognized as an essential part of the post-2015 global health agenda [33], and this must be an critical and early component of building health systems that are prepared to address breast cancer control. Chemotherapy and endocrine therapy can be essential for reducing the risk for recurrence and improving survival. Task-shifting models that use nurses, clinical officers, and general practitioners in close partnership with remotely or locally based oncologists show early promise in facilitating cancer care in remote areas and are being used and examined in settings such as Rwanda and Kenya [34–36].
It has been estimated that of the 15 million cancer cases estimated to occur by the end of 2015, about 80% will require surgical oncologic care, and 75% of these (mostly in LMICs) will not receive safe, affordable, and timely surgical services.
In addition to limited human resources, limited financial resources for breast cancer treatment, follow-up, and palliation (at the level of governments, health systems and facilities, and patients) are another central issue. The World Health Organization has identified several chemotherapeutic and palliative agents used in early and metastatic breast cancer on its Essential Medicines List, updated in 2015 [37], but these remain unavailable or unaffordable for patients in many sub-Saharan African countries. Although endocrine therapies, such as tamoxifen, are often available at low prices, targeted therapies such as trastuzumab remain prohibitively expensive in most low-resource settings. The cost of chemotherapy highlights the need for strategic procurement of affordable chemotherapy and development of context-specific treatment protocols that optimize safety and effectiveness while minimizing costs [34].
Radiotherapy is a particularly limited resource in LMICs, especially in Africa. A recent systematic review found that 29 countries in Africa lack any radiotherapy capacity [38]. Because postmastectomy radiation plays a particularly important role in the treatment of locally advanced breast cancer, and locally advanced disease is currently very common in LMICs, the dearth of radiotherapy capacity for breast cancer is of particular concern, and its absence will certainly add to avoidable mortality. Financial support for patients must also be a key element of cancer treatment services in sub-Saharan Africa and other low-income countries. Even when cancer services can be subsidized by insurance plans, governments, or organizations, patients may face significant out-of-pocket expenses for cancer care [39, 40]. Loss to follow-up is a major issue that threatens the efficacy of treatment protocols even when treatment is available [41]. Particular attention needs to be paid to understanding and addressing the social and financial barriers that threaten treatment adherence and completion and additional resources that need to be dedicated to patient support.
Early Detection and Screening
The prevalence of late-stage breast cancer in many LMICs often leads policymakers to the conclusion that development of early detection policies and programs, including screening of asymptomatic women, should be an early step in breast cancer control in such settings. However, systematic efforts to promote earlier detection of disease should be undertaken only once effective, high-quality treatment can be assured for all patients diagnosed with early-stage breast cancer. Even without systematic early detection efforts, the availability of affordable treatment can lead to earlier detection of breast cancer in a population. As access to affordable treatment grows, awareness of breast cancer and its treatability should increase, leading women to present with breast symptoms earlier, and primary health care providers to refer them more expeditiously. A report from Soweto, South Africa, for example, suggested that even without systematic screening or early detection campaigns, the development of a specialized breast clinic and more accessible treatment at a public hospital led to a shift in the stage distribution of disease over time [42].
Once cancer diagnostic and treatment infrastructure is in place, systematic efforts to promote earlier detection of symptomatic disease are of vital importance and in the lowest-resource settings should probably occur before any widespread screening. Given that diagnostic delays occur between the development of symptoms and first presentation at a health facility, and between first presentation and diagnosis or treatment, barriers at both the community and health system levels must be addressed [16, 18, 21]. Interventions to reduce these delays would ideally increase the proportion of patients with breast cancer that is potentially curable and ultimately reduce breast cancer mortality while minimizing expense, inefficiency, and potential harms (for example, false-positive results and unnecessary biopsies). The Breast Health Global Initiative recommends phased approaches to early detection based on the resources available in a given country where resources for diagnosis and treatment are available [43]. In settings with the most limited resources, the approach might focus on enhanced awareness and building capacity for breast evaluation, followed by a focus on downsizing of symptomatic disease, with the highest-resource settings pursuing screening of asymptomatic women [43]. However, few LMIC studies exist to document and evaluate these approaches, and none examine the outcome of breast cancer mortality resulting from early detection interventions.
Most existing studies of early detection in LMICs have been investigations of screening through clinical breast examination (CBE). In settings where most women present with palpable breast lesions, CBE is likely to have far more effect on outcomes than it is in settings where mammography is widely available [44]. Mammography is the only screening modality shown (through studies conducted in North America and Europe) to reduce breast cancer mortality, although the reduction is modest [45]. But in most low-income countries, including throughout sub-Saharan Africa, population-based screening mammography is not yet available. Furthermore, mammography has much lower absolute benefit among younger women [45] and in lower-incidence settings, so that even with wide availability of this technology, it is not clear that mammography would have benefits in sub-Saharan Africa comparable to even its modest breast cancer mortality reduction in the West [5].
Several large studies are examining the use of screening CBE in low-income settings, including Africa. Preliminary results from cluster randomized controlled trials of screening CBE in India [46, 47] suggest that screening CBE can lead to substantial rates of downstaging. A pilot intervention in Sudan has suggested that community-based CBE screening by trained lay volunteers can lead to an increased breast cancer detection rate and potential downstaging [48]. In China, after 1.5 million women were screened for breast cancer by using CBE, 70% of the 631 women diagnosed with cancer had early-stage disease [49]. In a small study in Tanzania in which health workers traveled to a randomly selected intervention village, visited homes, and performed comprehensive screening histories and physical examinations (including breast examinations), there were more breast cancers and a higher proportion of early-stage disease diagnosed after the intervention compared with findings in a similarly sized control village (although the study appears to have major limitations, and the comparability of the villages in terms of sex and age distributions and other risk factors has s not been reported) [50]. However, no study has yet demonstrated reductions in breast cancer mortality from screening CBE, a critical outcome to demonstrate because of the historically limited access to effective treatment in the countries in which these studies are being conducted.
In addition, increases in early-stage diagnoses through screening of asymptomatic women do not always clearly translate to improved cancer outcomes in high-income countries [51, 52]. However, in settings where late-stage disease is prevalent and the focus is on early treatment of already symptomatic disease, downstaging (for example, from stage III to stage I or II disease) might be expected to have more consistent associations with mortality decreases.
Furthermore, important challenges exist to CBE screening programs in LMICs, limitations that could be of particular concern in sub-Saharan Africa. First, quality control and ongoing training of practitioners in CBE must be an essential part of a CBE screening or early detection program. Although a study of CBE screening in the Philippines also demonstrated a shift toward earlier-stage presentations among screened women, CBE as performed in the study had low sensitivity (39.8%), and the rate of positive CBEs was low (2.5%), suggesting that practitioners may have lacked skill [53]. Second, follow-up of abnormal results is also a key challenge. The Philippines study found low rates of follow-up of positive CBE findings: Only 35% of screen-positive women pursued further diagnostic evaluation despite provision of financial support and home visits. These issues led to early termination of the study [53]. A study of CBE and mammography in Indonesia similarly demonstrated low rates of follow-up among women actually diagnosed with cancer, with only 42.8% of those returning for treatment [54]. A report of a breast cancer awareness and screening campaign in the Democratic Republic of Congo (DRC) reported that 73% of women found to have a palpable mass never followed up for further evaluation; although not emphasized in the article, it seems that women had to pay for most of their subsequent evaluation, which presumably presented a significant barrier to follow-up as well as treatment of cancers detected [55]. The DRC findings mirror outcomes from a World Health Organization demonstration project of cervical cancer screening in six sub-Saharan African countries, in which only 30% of women with cervical lesions suspicious for cancer were investigated [56]. Together, these experiences highlight that screening or early detection campaigns must investigate and address barriers to care, establish accessible treatment services, and provide robust patient tracking systems as well as economic and social support to facilitate patient follow-up.
Finally, widespread screening CBE (and even programs to promote high-quality evaluation and CBE of symptomatic women) may entail substantial numbers of patients with false-positive results presenting to referral facilities [47, 49, 57]. Thus, there is a strong need to identify efficient screening protocols and for clinical algorithms to evaluate symptomatic women that can be used at various levels of a low-resource health care system.
Given the limitations of existing screening methods, the epidemiology of breast cancer in sub-Saharan Africa, the challenges of implementing any screening program, and the realities of breast cancer presentations in most LMICs, the most beneficial starting point is likely to be initial strategies to encourage women to present earlier with symptomatic disease and to promote efficient referrals of women with suspicious findings to facilities where cancer diagnosis and treatment are available. Long-term follow up will be essential to identify whether strategies to promote earlier detection of symptomatic disease in LMICs can reduce mortality from breast cancer, and what referral and treatment resources and systems need to be in place to ensure that women can benefit. Studies to identify feasible, cost-effective service delivery strategies are of vital importance in settings where primary care infrastructure and resources are highly limited [24]. However, given what is known about diagnostic delays, late-stage presentation, and the epidemiology of breast cancer in sub-Saharan Africa, it is clear that breast cancer control policies must focus first and foremost on establishing accessible treatment for early-stage disease.
Long-term follow up will be essential to identify whether strategies to promote earlier detection of symptomatic disease in LMICs can reduce mortality from breast cancer, and what referral and treatment resources and systems need to be in place to ensure that women can benefit.
Conclusion
Data on breast cancer incidence and mortality in LMICs, particularly in sub-Saharan Africa, are highly limited. However, the burden of cancer in LMICs is clearly growing, and existing estimates suggest that age-specific incidence and mortality rates are also rising in some LMICs, including those in sub-Saharan Africa. There are profound disparities in breast cancer outcomes between resource-rich and resource-constrained settings. There are few rigorous examinations of effective diagnostic and treatment strategies for breast cancer in LMICs that address the unique and diverse challenges that LMICs face. Ongoing research may illuminate the most effective and feasible screening and early detection techniques for LMICs, but these must be tested in a range of geographic, cultural, and resource contexts to identify the most feasible ways to ensure that such strategies benefit women in LMICs. High-quality population-based cancer registries are needed to guide resource allocation and development of national and regional cancer control strategies and to monitor the effect of interventions. Our review of the literature underscores both the dire need for better understanding of breast cancer in LMICs and the urgency of facilitating effective treatment that is accessible and affordable for all women. Dedicated resources to promote high-quality breast cancer diagnostic services and treatment should be a global public health priority. The gap between mortality/incidence ratios in high- and low-income countries underscores the number of patients who die of breast cancer in resource-limited settings, who would have survived if they had access to standard treatments readily available in resource-rich settings.
This article is available for continuing medical education credit at CME.TheOncologist.com.
Acknowledgments
This work was supported by the Breast Cancer Research Foundation and the Mary Ann Tynan Fellowship in Women’s Health, Brigham and Women’s Hospital, Boston, MA.
Author Contributions
Conception/Design: Lydia E. Pace, Lawrence N. Shulman
Data analysis and interpretation: Lydia E. Pace
Manuscript writing: Lydia E. Pace, Lawrence N. Shulman
Final approval of manuscript: Lawrence N. Shulman
Disclosures
The authors indicated no financial relationships.
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Bray F, Jemal A, Grey N, et al. Global cancer transitions according to the Human Development Index (2008-2030): A population-based study. Lancet Oncol. 2012;13:790–801. doi: 10.1016/S1470-2045(12)70211-5. [DOI] [PubMed] [Google Scholar]
- 3.Soerjomataram I, Lortet-Tieulent J, Parkin DM, et al. Global burden of cancer in 2008: A systematic analysis of disability-adjusted life-years in 12 world regions. Lancet. 2012;380:1840–1850. doi: 10.1016/S0140-6736(12)60919-2. [DOI] [PubMed] [Google Scholar]
- 4.The World Bank. Country and lending groups. 2015. Available at http://data.worldbank.org/about/country-and-lending-groups. Accessed October 14, 2015.
- 5.Harford JB. Breast-cancer early detection in low-income and middle-income countries: do what you can versus one size fits all. Lancet Oncol. 2011;12:306–312. doi: 10.1016/S1470-2045(10)70273-4. [DOI] [PubMed] [Google Scholar]
- 6.Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 7.DeSantis CE, Bray F, Ferlay J, et al. International variation in female breast cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2015;24:1495–1506. doi: 10.1158/1055-9965.EPI-15-0535. [DOI] [PubMed] [Google Scholar]
- 8.Forouzanfar MH, Foreman KJ, Delossantos AM, et al. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet. 2011;378:1461–1484. doi: 10.1016/S0140-6736(11)61351-2. [DOI] [PubMed] [Google Scholar]
- 9.Fitzmaurice C, Dicker D, Pain A, et al. The global burden of cancer 2013. JAMA Oncol. 2015;1:505–527. doi: 10.1001/jamaoncol.2015.0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Linos E, Spanos D, Rosner BA, et al. Effects of reproductive and demographic changes on breast cancer incidence in China: A modeling analysis. J Natl Cancer Inst. 2008;100:1352–1360. doi: 10.1093/jnci/djn305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park S, Kim Y, Shin HR, et al. Population-attributable causes of cancer in Korea: Obesity and physical inactivity. PLoS One. 2014;9:e90871. doi: 10.1371/journal.pone.0090871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Porter P. “Westernizing” women’s risks? Breast cancer in lower-income countries. N Engl J Med. 2008;358:213–216. doi: 10.1056/NEJMp0708307. [DOI] [PubMed] [Google Scholar]
- 13.Gakwaya A, Kigula-Mugambe JB, Kavuma A, et al. Cancer of the breast: 5-year survival in a tertiary hospital in Uganda. Br J Cancer. 2008;99:63–67. doi: 10.1038/sj.bjc.6604435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pace LE, Dusengimana JM, Hategekimana V, et al. Benign and malignant breast disease at Rwanda’s first public cancer referral center. The Oncologist. 2016;5:000–000. doi: 10.1634/theoncologist.2015-0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lopes LV, Miguel F, Freitas H, et al. Stage at presentation of breast cancer in Luanda, Angola - a retrospective study. BMC Health Serv Res. 2015;15:471. doi: 10.1186/s12913-015-1092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Unger-Saldaña K. Challenges to the early diagnosis and treatment of breast cancer in developing countries. World J Clin Oncol. 2014;5:465–477. doi: 10.5306/wjco.v5.i3.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma K, Costas A, Shulman LN, et al. A systematic review of barriers to breast cancer care in developing countries resulting in delayed patient presentation. J Oncol. 2012;2012:121873. doi: 10.1155/2012/121873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Otieno ES, Micheni JN, Kimende SK, et al. Provider delay in the diagnosis and initiation of definitive treatment for breast cancer patients. East Afr Med J. 2010;87:143–146. doi: 10.4314/eamj.v87i4.62201. [DOI] [PubMed] [Google Scholar]
- 19.Clegg-Lamptey J, Dakubo J, Attobra YN. Why do breast cancer patients report late or abscond during treatment in ghana? A pilot study. Ghana Med J. 2009;43:127–131. [PMC free article] [PubMed] [Google Scholar]
- 20.Ibrahim NA, Oludara MA. Socio-demographic factors and reasons associated with delay in breast cancer presentation: A study in Nigerian women. Breast. 2012;21:416–418. doi: 10.1016/j.breast.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 21.Pace LE, Mpunga T, Hategekimana V, et al. Delays in breast cancer presentation and diagnosis at two rural cancer referral centers in Rwanda. The Oncologist. 2015;20:780–788. doi: 10.1634/theoncologist.2014-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ukwenya AY, Yusufu LM, Nmadu PT, et al. Delayed treatment of symptomatic breast cancer: The experience from Kaduna, Nigeria. S Afr J Surg. 2008;46:106–110. [PubMed] [Google Scholar]
- 23.Otieno ES, Micheni JN, Kimende SK, et al. Delayed presentation of breast cancer patients. East Afr Med J. 2010;87:147–150. doi: 10.4314/eamj.v87i4.62410. [DOI] [PubMed] [Google Scholar]
- 24.Pace LE, Katz IT. Breast and cervical cancer screening: Investing in health care systems. Harvard Public Health Rev. 2015;2015:5. [Google Scholar]
- 25.Gelband H, Sankaranarayanan R, Gauvreau CL, et al. Costs, affordability, and feasibility of an essential package of cancer control interventions in low-income and middle-income countries: Key messages from disease control priorities, 3rd edition. Lancet. 2015 doi: 10.1016/S0140-6736(15)00755-2. [DOI] [PubMed] [Google Scholar]
- 26.Anderson BO, Cazap E, El Saghir NS, et al. Optimisation of breast cancer management in low-resource and middle-resource countries: executive summary of the Breast Health Global Initiative consensus, 2010. Lancet Oncol. 2011;12:387–398. doi: 10.1016/S1470-2045(11)70031-6. [DOI] [PubMed] [Google Scholar]
- 27.Kantelhardt EJ, Zerche P, Mathewos A, et al. Breast cancer survival in Ethiopia: A cohort study of 1,070 women. Int J Cancer. 2014;135:702–709. doi: 10.1002/ijc.28691. [DOI] [PubMed] [Google Scholar]
- 28.Adesina A, Chumba D, Nelson AM, et al. Improvement of pathology in sub-Saharan Africa. Lancet Oncol. 2013;14:e152–e157. doi: 10.1016/S1470-2045(12)70598-3. [DOI] [PubMed] [Google Scholar]
- 29.African Strategies for Advancing Pathology Group Members Quality pathology and laboratory diagnostic services are key to improving global health outcomes: Improving global health outcomes is not possible without accurate disease diagnosis. Am J Clin Pathol. 2015;143:325–328. doi: 10.1309/AJCP6K0DZCNVCSCI. [DOI] [PubMed] [Google Scholar]
- 30.Mpunga T, Tapela N, Hedt-Gauthier BL, et al. Diagnosis of cancer in rural Rwanda: Early outcomes of a phased approach to implement anatomic pathology services in resource-limited settings. Am J Clin Pathol. 2014;142:541–545. doi: 10.1309/AJCPYPDES6Z8ELEY. [DOI] [PubMed] [Google Scholar]
- 31.Gopal S, Krysiak R, Liomba NG, et al. Early experience after developing a pathology laboratory in Malawi, with emphasis on cancer diagnoses. PLoS One. 2013;8:e70361. doi: 10.1371/journal.pone.0070361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sullivan R, Alatise OI, Anderson BO, et al. Global cancer surgery: Delivering safe, affordable, and timely cancer surgery. Lancet Oncol. 2015;16:1193–1224. doi: 10.1016/S1470-2045(15)00223-5. [DOI] [PubMed] [Google Scholar]
- 33.Meara JG, Hagander L, Leather AJ. Surgery and global health: A Lancet Commission. Lancet. 2014;383:12–13. doi: 10.1016/S0140-6736(13)62345-4. [DOI] [PubMed] [Google Scholar]
- 34.Stulac S, Binagwaho A, Tapela NM, et al. Capacity building for oncology programmes in sub-Saharan Africa: The Rwanda experience. Lancet Oncol. 2015;16:e405–e413. doi: 10.1016/S1470-2045(15)00161-8. [DOI] [PubMed] [Google Scholar]
- 35.Shulman LN, Mpunga T, Tapela N, et al. Bringing cancer care to the poor: Experiences from Rwanda. Nat Rev Cancer. 2014;14:815–821. doi: 10.1038/nrc3848. [DOI] [PubMed] [Google Scholar]
- 36.Strother RM, Asirwa FC, Busakhala NB, et al. AMPATH-Oncology: A model for comprehensive cancer care in Sub-Saharan Africa. J Cancer Policy. 2003;1:e42–e48. [Google Scholar]
- 37.World Health Organization. WHO Model List of Essential Medicines, 19th List. 2015. Available at http://www.who.int/selection_medicines/committees/expert/20/EML_2015_FINAL_amended_AUG2015.pdf?ua=1. Accessed October 14, 2015.
- 38.Grover S, Xu MJ, Yeager A, et al. A systematic review of radiotherapy capacity in low- and middle-income countries. Front Oncol. 2014;4:380. doi: 10.3389/fonc.2014.00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O’Neill KM, Mandigo M, Pyda J, et al. Out-of-pocket expenses incurred by patients obtaining free breast cancer care in Haiti. Lancet. 2015;385(suppl 2):S48. doi: 10.1016/S0140-6736(15)60843-1. [DOI] [PubMed] [Google Scholar]
- 40.Okoronkwo IL, Ejike-Okoye P, Chinweuba AU, et al. Financial barriers to utilization of screening and treatment services for breast cancer: An equity analysis in Nigeria. Niger J Clin Pract. 2015;18:287–291. doi: 10.4103/1119-3077.151070. [DOI] [PubMed] [Google Scholar]
- 41.Galukande M, Wabinga H, Mirembe F. Breast cancer survival experiences at a tertiary hospital in sub-Saharan Africa: A cohort study. World J Surg Oncol. 2015;13:220. doi: 10.1186/s12957-015-0632-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murugan N, Dickens C, McCormack V, et al. Down-staging of breast cancer in the pre-screening era: Experiences from Chris Hani Baragwanath Academic Hospital, Soweto, South Africa. S Afr Med J. 2014;104:380. doi: 10.7196/samj.8243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yip CH, Smith RA, Anderson BO, et al. Guideline implementation for breast healthcare in low- and middle-income countries: Early detection resource allocation. Cancer. 2008;113(suppl):2244–2256. doi: 10.1002/cncr.23842. [DOI] [PubMed] [Google Scholar]
- 44.Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314:1599–1614. doi: 10.1001/jama.2015.12783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pace LE, Keating NL. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA. 2014;311:1327–1335. doi: 10.1001/jama.2014.1398. [DOI] [PubMed] [Google Scholar]
- 46.Mittra I, Mishra GA, Singh S, et al. A cluster randomized, controlled trial of breast and cervix cancer screening in Mumbai, India: methodology and interim results after three rounds of screening. Int J Cancer. 2010;126:976–984. doi: 10.1002/ijc.24840. [DOI] [PubMed] [Google Scholar]
- 47.Sankaranarayanan R, Ramadas K, Thara S, et al. Clinical breast examination: Preliminary results from a cluster randomized controlled trial in India. J Natl Cancer Inst. 2011;103:1476–1480. doi: 10.1093/jnci/djr304. [DOI] [PubMed] [Google Scholar]
- 48.Abuidris DO, Elsheikh A, Ali M, et al. Breast-cancer screening with trained volunteers in a rural area of Sudan: A pilot study. Lancet Oncol. 2013;14:363–370. doi: 10.1016/S1470-2045(12)70583-1. [DOI] [PubMed] [Google Scholar]
- 49.Song QK, Wang XL, Zhou XN, et al. Breast cancer challenges and screening in China: Lessons from current registry data and population screening studies. The Oncologist. 2015;20:773–779. doi: 10.1634/theoncologist.2014-0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ngoma T, Mandeli J, Holland JF. Downstaging cancer in rural Africa. Int J Cancer. 2015;136:2875–2879. doi: 10.1002/ijc.29348. [DOI] [PubMed] [Google Scholar]
- 51.Harding C, Pompei F, Burmistrov D, et al. Breast cancer screening, incidence, and mortality across US counties. JAMA Intern Med. 2015;175:1483–1489. doi: 10.1001/jamainternmed.2015.3043. [DOI] [PubMed] [Google Scholar]
- 52.Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367:1998–2005. doi: 10.1056/NEJMoa1206809. [DOI] [PubMed] [Google Scholar]
- 53.Pisani P, Parkin DM, Ngelangel C, et al. Outcome of screening by clinical examination of the breast in a trial in the Philippines. Int J Cancer. 2006;118:149–154. doi: 10.1002/ijc.21343. [DOI] [PubMed] [Google Scholar]
- 54.Kardinah D, Anderson BO, Duggan C, et al. Short report: Limited effectiveness of screening mammography in addition to clinical breast examination by trained nurse midwives in rural Jakarta, Indonesia. Int J Cancer. 2014;134:1250–1255. doi: 10.1002/ijc.28442. [DOI] [PubMed] [Google Scholar]
- 55.Luyeye Mvila G, Postema S, Marchal G, et al. From the set-up of a screening program of breast cancer patients to the identification of the first BRCA mutation in the DR Congo. BMC Public Health. 2014;14:759. doi: 10.1186/1471-2458-14-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Denny L. Control of cancer of the cervix in low- and middle-income countries. Ann Surg Oncol. 2015;22:728–733. doi: 10.1245/s10434-014-4344-8. [DOI] [PubMed] [Google Scholar]
- 57.Denewer A, Hussein O, Farouk O, et al. Cost-effectiveness of clinical breast assessment-based screening in rural Egypt. World J Surg. 2010;34:2204–2210. doi: 10.1007/s00268-010-0620-3. [DOI] [PubMed] [Google Scholar]