Abstract
Background
Knee reinjury after anterior cruciate ligament (ACL) reconstruction is common and increases the risk of osteoarthritis. There is sparse evidence to guide return to sport (RTS) decisions in this population.
Objectives
To assess the relationship between knee reinjury after ACL reconstruction and 1) return to level I sports, 2) timing of return to sports, and 3) knee function prior to return.
Methods
106 patients who participated in pivoting sports participated in this prospective two year cohort study. Sports participation and knee reinjury were recorded monthly. Knee function was assessed with the Knee Outcome Survey–Activities of Daily Living Scale, global rating scale of function, and quadriceps strength and hop test symmetry. Pass RTS criteria was defined as scores >90 on all tests, failure as failing any.
Results
Patients who returned to level I sports had 4.32 (p=0.048) higher reinjury rate than those who did not. The reinjury rate was significantly reduced by 51 % for each month RTS was delayed until 9 months after surgery, after which no further risk reduction was observed. 38.2 % of those who failed RTS criteria suffered reinjuries versus 5.6 % of those who passed (HR: 0.16, p=0.075). More symmetrical quadriceps strength prior to return significantly reduced the knee reinjury rate.
Conclusion
Returning to level I sports after ACL reconstruction leads to a more than 4-fold increase in reinjury rates over 2 years. Return to sport 9 months or later after surgery and more symmetrical quadriceps strength prior to return substantially reduces the reinjury rate.
Keywords: anterior cruciate ligament, anterior cruciate ligament reconstruction, return to sport, knee function, knee injury
INTRODUCTION
250,000 anterior cruciate ligament (ACL) injuries are estimated to occur annually in the United States.1 The short and long term consequences include muscle weakness, functional deficits, lower sports participation, increased risk of knee reinjury, and knee osteoarthritis (OA).2–5 Up to 30 % of young active patients who undergo reconstruction suffer a second ACL rupture in the first few years after surgery,3,6 leading to poorer health-related quality of life.7 The most devastating outcome, however, is the significantly increased rate of knee OA in those ACL injured individuals who also sustain a meniscus injury. Within five years, 50 % of patients may undergo meniscus surgery,8 increasing their prognosis of posttraumatic knee OA from 0–13 % to 21–48 %.4 We can reduce this high rate of knee OA through prevention of secondary meniscus injuries. In the US alone, halving the OA rate after ACL injury could lead to $1.1 billion in cost savings annually.9
Intent to return to level I (jumping, pivoting and hard cutting) sports 10–12 is the main reason why a patient with an ACL rupture undergoes ACL reconstruction.5 Younger age and participation in pivoting sports are also unfortunately consistent predictors of another ACL rupture after ACL reconstruction.13–17 Activity restrictions based on postsurgical time (a surrogate for biological healing) and functional status (assessed with test batteries) have been advocated to enable the safest possible return to sport.18,19 There is currently no clear evidence to guide whether participation in level I sports should be delayed or what level of function the patient should achieve prior to returning to level I sports.20
The aims of this study were therefore to assess if the two year risk of a knee reinjury after ACL reconstruction was associated with 1) return to level I sports, 2) timing of return to level I sports, and 3) knee function prior to return to level I sport.
MATERIAL AND METHODS
Subjects
This cohort consists of the ACL injured patients in the Norwegian arm (n=150) of the Delaware-Oslo ACL Cohort Study (n=300) who underwent ACL reconstruction (n=106).5 Patients were consecutively screened for inclusion at the Norwegian Sports Medicine Clinic between 2007 and 2011. We included patients who had sustained a unilateral ACL rupture within 3 months of enrolment (verified by magnetic resonance imaging [MRI] and ≥ 3 mm side-to-side difference in anterior laxity measured by KT-100021). Other inclusion criteria were age between 13 and 60 years and preinjury participation in level I or II sports10 at least twice weekly. Patients were excluded if they had current or previous injury to the contralateral knee, previous knee injury on the index knee, or concomitant grade III knee ligament injury, fracture, or full-thickness cartilage defects. Patients with meniscus injuries were excluded only if they had pain or effusion during plyometric activities that had not resolved three months from injury. Approval from the Regional Committee for Medical Research Ethics was obtained, and written informed consent was acquired, prior to inclusion.
Treatment algorithm
All patients underwent our previously published preoperative rehabilitation programme.22 Further treatment (surgery or continued rehabilitation) was decided after this five week programme. The ACL reconstruction was performed in one of seven different hospitals, using bone-patellar-tendon-bone (BPTB) or hamstrings autograft. The postoperative rehabilitation was individually tailored based on concomitant surgery, graft choice and function. Rehab consisted of three phases: The acute phase where the aims were to eliminate effusion, range of motion (ROM) deficits and minimise muscle atrophy. The rehabilitation phase where the aims were to regain neuromuscular control of terminal knee extension in weight bearing positions and to regain ≥ 80 % muscle strength and hop performance. The last phase, the return to sport phase, aimed at regaining ≥ 90 % muscle strength and hop performance, while transitioning to sport through sport-specific drills and gradual participation. Patients were advised against full participation in level I sports if they had not regained more than 90 % quadriceps and hamstring strength and hopping performance compared to the uninjured leg.
Data collection
Starting the first month after ACL reconstruction, sports participation data were collected monthly using an online activity survey.11 Patients reported which sports they participated in by ticking a box for the respective sport. Each month, one reminder was automatically sent out to patients who had not responded after one week. The online activity survey has excellent test-retest reliability (κ=0.92 for level I sports participation).11 Knee reinjuries with an acute onset were recorded through the online survey and at clinical follow-ups at six months, one year and two years after reconstruction. The injuries were diagnosed according to the standard practice at our clinic. Of 24 reinjured patients, two were diagnosed after clinical examination, ten after clinical examination and MRI, five after clinical examination and arthroscopic surgery, and seven after clinical examination, MRI and arthroscopic surgery.
The comprehensive RTS test battery19,23,24 investigated in this study consisted of isokinetic quadriceps strength testing, four single-legged hop tests, and two self-report outcomes.23,24 These data were collected at baseline (mean 2.1 ± 0.6 months after injury) and six and 12 months after surgery. Isokinetic concentric quadriceps strength was measured at 60°/sec with an electromechanical dynamometer (Biodex 6000, Biodex Medical Systems, Shirley, New York). Four submaximal practice trials were followed by one minute rest before five maximum effort repetitions were recorded. After strength testing, four hop tests were performed in the following order: Single hop for distance, crossover hop for distance, triple hop for distance and 6-m timed hop.25,26 All patients performed one practice trial hop and then two hops were recorded. The uninvolved leg was always tested first. After the hop testing, patients completed the Knee Outcome Survey – Activities of Daily Living Scale (KOS-ADLS)27 and a global rating scale (GRS) of perceived function.23 The KOS-ADLS is a 14-item self-reported assessment of symptoms and function in activities of daily living, scored from 0 (worst) to 100 (best). The GRS asks the patient to rate current knee function on a scale from 0 (not able to perform any activity) to 100 (level of function prior to the knee injury).
Data management and statistical analysis
Return to level I sport was defined as any reported participation in handball, football, basketball or floorball, regardless of training/match participation or level of competition. The first recorded participation in level I sports was reported in months after surgery.
We extracted data on knee function from the 6 month follow-up for those who returned to level I sports 5–11 months after surgery (n=49) and from the 12 month follow-up for those who returned 12–23 months after surgery (n=20). The limb symmetry indexes (LSI) of the peak quadriceps torque (highest achieved value) and hop test distance/time were calculated by involved/uninvolved × 100, except for the 6m timed hop test which was calculated by uninvolved/involved × 100. Patients were classified as having passed RTS criteria if they scored > 90 on all seven variables. Patients who returned to level I sport less than five months after surgery (n=4) were a priori classified as not having passed RTS criteria.23,24
A Cox proportional hazards regression model with months after surgery as the time variable was used to assess the reinjury rate in patients who participated in level I sports after surgery versus those who did not. Cox regression models were also used to assess the association between knee reinjury and time of return, and knee function prior to return to level I sports. Time 0 was defined as the first month of level I sports participation to limit bias from more sports exposure in patients who returned early to level I sports. The independent variables were months from surgery to return to sport, passing/failing RTS criteria and continuous LSIs of the individual RTS variables. Separate results were reported for those who returned before and after nine months after surgery, as the assumption of proportionality was violated in the analysis of time of return. All analyses were adjusted for age. Two-sided p-values less than or equal to 0.05 were considered statistically significant.
RESULTS
From the original 106 patients who underwent ACL reconstruction, one hundred (94.3 %) had data on sports participation and knee reinjuries (one withdrew from study, five did not respond to the online activity survey). The monthly data on sports participation and reinjuries were 92.9 % complete for the 100 patients (2230 reports in total). Descriptive characteristics of the cohort can be seen in Table 1.
Table 1.
Characteristics of the ACL reconstructed patients (n=100)
| Sex, men/women (% men) | 46/54 (46.0) |
| Age, mean ± SD | 24.3 ± 7.3 |
| Preinjury participation in level I sports, n (%) | 83 (83.0) |
| Handball* | 30 (30.0) |
| Football* | 53 (53.0) |
| Basketball* | 6 (6.0) |
| Floorball* | 11 (11.0) |
| Months from injury to surgery, median (min–max) | 4.8 (1.6–25.4) |
| ACL graft, n (%) | |
| BPTB | 33 (33.0) |
| Hamstring | 67 (67.0) |
| Baseline concomitant injuries, n (%) | |
| Medial meniscus injury | 26 (26.0) |
| Lateral meniscus injury | 20 (20.0) |
| Medial cartilage injury | 3 (3.0) |
| Lateral cartilage injury | 9 (9.0) |
| MCL injury grade I–II | 30 (30.0) |
| LCL injury grade I–II | 1 (1.0) |
| Popliteus injury | 2 (2.0) |
| Baseline knee function, mean ± SD | |
| Quadriceps strength, LSI | 89.2 ± 10.2 |
| Single hop for distance, LSI | 91.2 ± 10.4 |
| Triple crossover hop, LSI | 92.9 ± 9.3 |
| Triple hop, LSI | 91.3 ± 8.3 |
| 6 meter timed hop, LSI | 94.6 ± 8.3 |
| KOS-ADLS | 82.4 ± 9.6 |
| Global rating scale | 79.3 ± 12.8 |
Baseline: At enrolment in the study and prior to ACL reconstruction, mean 2.1 (SD: 0.6) months from injury
BPTB: Bone-patellar tendon-bone
LSI: limb symmetry index
Concomitant injuries were diagnosed by MRI
Some participated in multiple level I sports
74/83 patients who previously participated in level I sports returned to level I sports within two years of ACL reconstruction. None of the 17 who did not participate in level I sport before injury participated in level I sports after surgery. The mean number of months participating in level I sports was 8.1 ± 5.7 over the two postoperative years. The time of return to level I sports varied from 3 to 23 months after surgery, with a median of 8 months after surgery.
69/74 (93.2 %) patients who participated in level I sports underwent functional testing prior to return to sport. One patient did not attend any of the follow-ups. Four patients returned to sport fewer than five months after surgery. All four of these patients suffered a knee reinjury within two months of return. The mean time from functional testing to return to level I sport was 2.3 ± 2.4 months. Of the 49 patients who returned to level I sports 5–11 months after surgery, 7 (14.3 %) had passed the RTS criteria at the 6 month follow-up test. Eleven of the 20 patients (55.0 %) who returned to level I sport 12–23 months after surgery had passed the RTS criteria at the 12 month follow-up. In total, 18 of the 74 patients (24.3 %) were classified as having passed the functional RTS criteria prior to return to sport.
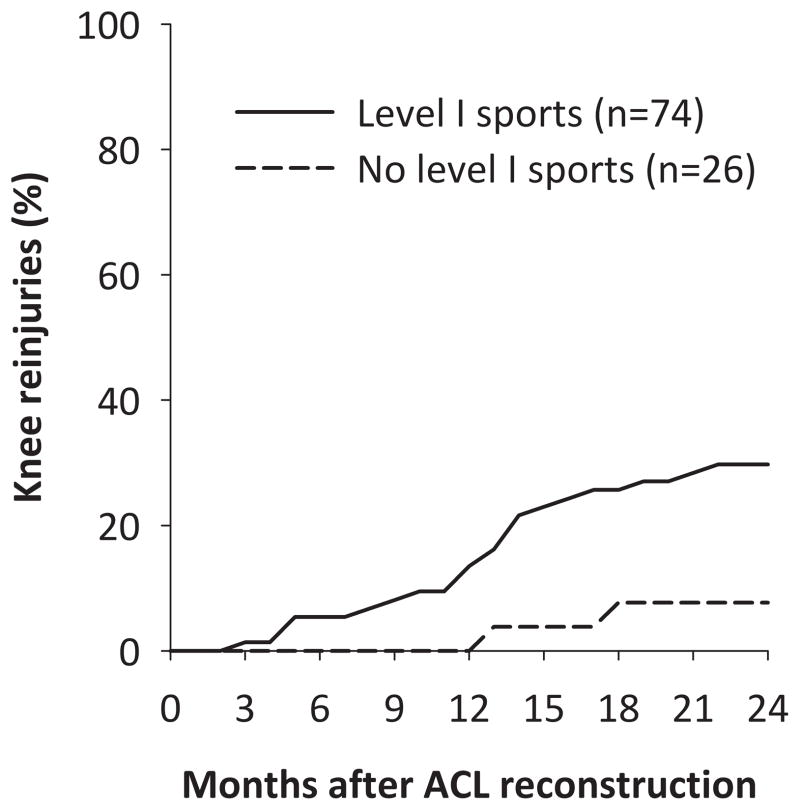
24 (24.0 %) patients sustained 28 knee reinjuries, including eight ACL graft ruptures and eight medial meniscus injuries (Table 2). The reinjuries occurred from the 3rd to the 22nd postoperative month, with a median of 13 months after surgery. The time between returning to level I sports and sustaining a knee reinjury varied from less than one month to 16 months, with 45.5 % of the reinjuries sustained within two months of return to sport. In the 26 patients who did not return to level I sports, two reported a knee reinjury (7.7 %). The two year reinjury risk in patients who returned to level I sports after surgery was 29.7 % (22 of 74). After adjusting for age, patients who participated in level I sports after ACL reconstruction had 4.32 (95 % CI: 1.01–18.40, p=0.048) times higher reinjury rate than those who participated in lower level sports (Fig. 1).
Table 2.
Knee reinjuries over two years in ACL reconstructed patients
| Index knee | |
|---|---|
| ACL graft rupture | 8 (8.0) |
| Medial meniscus injury | 8 (8.0) |
| Lateral meniscus injury | 2 (2.0) |
| Medial cartilage injury | 1 (1.0) |
| Lateral cartilage injury | 1 (1.0) |
| Patellofemoral cartilage injury | 2 (2.0) |
| Medial collateral ligament injury | 1 (1.0) |
| Patella subluxation | 1 (1.0) |
| Contralateral knee | |
| ACL rupture | 2 (2.0) |
| Lateral meniscus injury | 1 (1.0) |
| Medial collateral ligament injury n (%) | 1 (1.0) |
Four patients had two reinjuries (same trauma).
Figure 1.
Knee reinjuries after ACL reconstruction in those who participated in level I sports and those who did not
During the first nine months after surgery, a later return to sport was significantly associated with a lower reinjury rate. For every one month delay in return to sport, the reinjury rate was reduced by 51 % (Table 3). In patients who returned between 9 and 23 months after surgery, time to return was not significantly associated with knee reinjury. Patients who participated in level I sports earlier than nine months after surgery sustained 39.5 % reinjuries (15 of 38), compared to 19.4 % knee reinjuries (7 of 36) in those who returned to level I sports later than nine months after surgery.
Table 3.
Factors associated with knee reinjury in patients who returned to level I sport after ACL reconstruction (n=74)
| n | No reinjury | n | Reinjury | Adjusted HR (95 % CI), p-value | |
|---|---|---|---|---|---|
| All patients | |||||
| Return to level I sports, months from surgery | 52 | 10.7 ± 4.3 | 22 | 7.2 ± 2.7 | |
| Passed RTS criteria, n (%) | 51 | 17 (33.3) | 22 | 1 (4.5) | 0.16 (0.02–1.20), 0.08 |
| Quadriceps strength, LSI | 51 | 84.4 ± 15.2 | 18 | 75.0 ± 16.7 | 0.97 (0.94–0.99), 0.03 |
| Single hop for distance, LSI | 48 | 89.4 ± 13.0 | 17 | 91.0 ± 11.7 | 1.01 (0.96–1.05), 0.77 |
| Triple crossover hop, LSI | 47 | 90.7 ± 11.8 | 16 | 93.8 ± 8.5 | 1.04 (0.98–1.10), 0.22 |
| Triple hop, LSI | 47 | 91.2 ± 10.0 | 15 | 93.5 ± 10.8 | 1.03 (0.96–1.10), 0.44 |
| 6 meter timed hop, LSI | 47 | 96.1 ± 9.9 | 16 | 92.4 ± 6.2 | 0.97 (0.93–1.02), 0.20 |
| KOS-ADLS | 51 | 89.2 ± 9.6 | 18 | 86.9 ± 10.7 | 0.98 (0.94–1.03), 0.43 |
| Global rating scale | 51 | 86.4 ± 13.9 | 18 | 77.7 ± 16.1 | 0.98 (0.95–1.01), 0.12 |
| Patients who returned before 9 months | |||||
| Return to level I sports, months from surgery | 23 | 7.3 ± 0.9 | 15 | 5.7 ± 1.7 | 0.49 (0.34–0.70), <0.001 |
| Patients who returned 9 months or later | |||||
| Return to level I sports, months from surgery | 29 | 13.4 ± 4.0 | 7 | 10.4 ± 1.0 | 0.75 (0.49–1.14), 0.18 |
Values are mean ± SD unless otherwise indicated. All analyses are adjusted for age. LSI: Limb symmetry index (%). HR (hazard ratio) below 1 indicates lower injury rate with higher values of the respective variable. All HR reflect the relative change in reinjury rate for a one unit increase in the respective variable. Passed RTS criteria was coded 1=yes, 0=no.
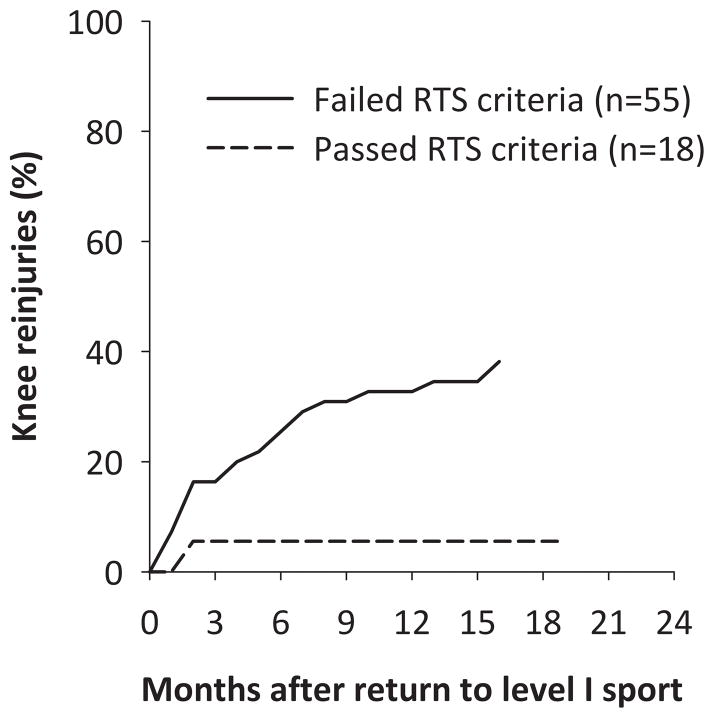
Of the 55 patients who failed RTS criteria, 21 (38.2 %) suffered knee reinjuries (fig. 2). Only one of the 18 patients (5.6 %) who passed RTS criteria suffered a knee reinjury. Patients who passed the RTS criteria showed a not statistically significant 84 % lower reinjury rate (HR: 0.16 [95 % CI: 0.02–1.20, p=0.075]). Of the individual components in the RTS test battery, quadriceps strength deficit prior to return to level I sport was a significant predictor of a knee reinjury, with 3 % reduced reinjury rate for every one percentage point increase in strength symmetry (Table 3). Fifteen of the 45 patients (33.3 %) who returned to level I sport with quadriceps LSI < 90 % suffered reinjuries, versus three (12.5 %) reinjuries in the 24 patients who had quadriceps LSI > 90 % prior to return.
Figure 2.
Knee reinjuries after return to level I sports in those who failed and those who passed return to sport (RTS) criteria prior to return
DISCUSSION
This 2-year prospective study showed that the knee reinjury rate was over four times higher in ACL reconstructed patients who returned to level I sports after surgery. Furthermore, returning to sport earlier after surgery and having asymmetrical quadriceps strength prior to return increased the risk of knee reinjury.
Our study is the first to evaluate the risk of all acute knee reinjuries in those who return to high level pivoting sports. Meniscus injury was the most frequent knee reinjury, a significant factor for development of OA.28 Reducing the risk of secondary injuries is therefore of uttermost importance. The age and sex distribution of our patient sample is similar to patients in the Scandinavian ACL registries,29 and the ACL reinjury rate seems to be generally consistent with previous studies in young, active adults,30,31 yet lower than that of high-school athletes.3
Previous studies on time to sports return and the risk of contralateral ACL rupture or ACL graft rupture have shown conflicting evidence.3,16,31 Different sports place different demands on the knee, and our finding of an increased risk with earlier sports return may be specific to athletes who return to level I sports. The increased risk could be due to insufficient biologic healing (e.g. graft incorporation and remodelling), incomplete rehabilitation, or both. Our results suggest that time to return is associated with reinjury, and the effect is larger in the early months after surgery. Of note, all patients who returned to sport before 5 months suffered a knee reinjury. Beyond 9 months after surgery, we did not find a statistically significant decreased risk by month later return. Still, 19.4 % of these patients also suffered knee reinjuries. Time alone is therefore not sufficient for determining readiness for level I sports participation.
Our findings support the use of both time-based and functional RTS criteria. There was an estimated 84 % lower knee reinjury rate in patients who passed RTS criteria, a magnitude of high clinical relevance. This finding was not statistically significant (p=0.075), likely due to low statistical power as only one of the 18 patients who passed the criteria and returned to sport suffered a knee reinjury. The low proportion of patients who passed RTS criteria is not surprising as the investigated RTS battery was not used to determine when patients were cleared to RTS in our study. Further, patients were tested 2.3 ± 2.4 months prior to return, and a higher number of patients might have passed had they undergone testing immediately prior to RTS. We have previously reported similar rates of passing RTS criteria at six months for the entire Delaware-Oslo ACL Cohort.23 The rate of passing RTS criteria was 52.5 % at one year after surgery,23 and only 66 % had quadriceps strength symmetry ≥ 90 % two years after surgery.5 These outcomes exist in a cohort that has shown superior patient-reported outcomes compared to the general ACL reconstructed population,32 suggesting that even larger functional deficits might persist after usual care.
While we still do not know the optimal content of a RTS test battery,19 our results show that quadriceps strength testing should be included. Asymmetrical quadriceps strength at the time of return to sport is associated with asymmetrical knee biomechanics during hopping,33 which in turn has been found to predict a second ACL injury.34 Quadriceps weakness is also a risk factor for knee OA,35 further highlighting the importance of thorough rehabilitation and quadriceps strength assessment. Postural control deficits and altered neuromuscular control of the hip and knee have also been found to predispose an athlete to a second ACL injury.34 So far, modifiable risk factors for reinjury after ACL reconstruction have only been identified using sophisticated testing equipment (isokinetic dynamometry and 3-dimensional motion analysis), and a future focus should be to validate more clinically accessible tests.
The main strength of this study is the frequent follow-up and high follow-up rate of ACL reconstructed patients who were consecutively screened for inclusion at one sports medicine clinic. A main limitation is the lack of exact athlete exposure time. Return to sport was defined as their first participation in a level I sport, and not necessarily full participation including match play. We were unable to control for the exact time spent in sports, full or limited participation, and training/match exposure.
CONCLUSION
Athletes who undergo ACL reconstruction should be informed that postoperative participation in level I sports increases the two year knee reinjury rate more than four times. A later return to level I sports and more symmetrical quadriceps strength prior to return decreases this rate significantly. A combination of strict time-based and functional RTS criteria therefore have great potential to improve long term function, substantially decrease the prevalence of posttraumatic knee osteoarthritis in these patients, and reduce downstream healthcare costs.
What are the new findings?
In the first 2 years after ACL reconstruction, 30 % of people who returned to level I sports sustained a reinjury compared to 8 % of those who participated in lower level sports.
For every month that return to sport was delayed, until 9 months after ACL reconstruction, the rate of knee reinjury was reduced by 51%.
More symmetrical quadriceps strength prior to return to sport significantly reduced the knee reinjury rate.
How might it impact on clinical practice in the near future?
Clinicians should inform patients of the increased risk of knee reinjury if they decide to return to level I sport
Strict time-based and functional return to sport criteria should be implemented
Return to level I sport should be delayed until at least 9 months have passed from surgery and the patient has regained quadriceps strength comparable to the uninjured side
Acknowledgments
The Delaware-Oslo Cohort Study is financed by the National Institutes of Health, grant R37 HD37985
We thank Ingrid Eitzen, Annika Storevold, Ida Svege, Espen Selboskar, Karin Rydevik, and Marte Lund with their assistance in data collection for this study. We acknowledge the Norwegian Sports Medicine Clinic, NIMI (www.nimi.no), for supporting the Norwegian Research Center for Active Rehabilitation (NAR; www.active-rehab.no) with rehabilitation facilities and research staff.
References
- 1.Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, DeMaio M, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34(9):1512–32. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 2.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116–21. doi: 10.1097/JSM.0b013e318246ef9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of Second ACL Injuries 2 Years After Primary ACL Reconstruction and Return to Sport. Am J Sports Med. 2014;42(7):1567–73. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–43. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 5.Grindem H, Eitzen I, Engebretsen L, Snyder-Mackler L, Risberg MA. Nonsurgical or Surgical Treatment of ACL Injuries: Knee Function, Sports Participation, and Knee Reinjury: The Delaware-Oslo ACL Cohort Study. J Bone Joint Surg Am. 2014;96(15):1233–41. doi: 10.2106/JBJS.M.01054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):641–7. doi: 10.1177/0363546513517540. [DOI] [PubMed] [Google Scholar]
- 7.Filbay SR, Ackerman IN, Russell TG, Macri EM, Crossley KM. Health-related quality of life after anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2014;42(5):1247–55. doi: 10.1177/0363546513512774. [DOI] [PubMed] [Google Scholar]
- 8.Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ. 2013;346:f232. doi: 10.1136/bmj.f232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mather RC, III, Koenig L, Kocher MS, Dall TM, Gallo P, Scott DJ, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95(19):1751–9. doi: 10.2106/JBJS.L.01705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):226–34. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 11.Grindem H, Eitzen I, Snyder-Mackler L, Risberg MA. Online registration of monthly sports participation after anterior cruciate ligament injury: a reliability and validity study. Br J Sports Med. 2014;48(9):748–53. doi: 10.1136/bjsports-2012-092075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moksnes H, Snyder-Mackler L, Risberg MA. Individuals with an anterior cruciate ligament-deficient knee classified as noncopers may be candidates for nonsurgical rehabilitation. J Orthop Sports Phys Ther. 2008;38(10):586–95. doi: 10.2519/jospt.2008.2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP. Risk Factors and Predictors of Subsequent ACL Injury in Either Knee After ACL Reconstruction: Prospective Analysis of 2488 Primary ACL Reconstructions From the MOON Cohort. Am J Sports Med. 2015;43(7):1583–90. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myklebust G, Holm I, Maehlum S, Engebretsen L, Bahr R. Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury: a follow-up study. Am J Sports Med. 2003;31(6):981–9. doi: 10.1177/03635465030310063901. [DOI] [PubMed] [Google Scholar]
- 15.Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–57. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 16.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–51. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 17.Sward P, Kostogiannis I, Roos H. Risk factors for a contralateral anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):277–91. doi: 10.1007/s00167-009-1026-3. [DOI] [PubMed] [Google Scholar]
- 18.Thomee R, Kaplan Y, Kvist J, Myklebust G, Risberg MA, Theisen D, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1798–805. doi: 10.1007/s00167-011-1669-8. [DOI] [PubMed] [Google Scholar]
- 19.Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697–705. doi: 10.1016/j.arthro.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Spindler KP, Wright RW. Clinical practice. Anterior cruciate ligament tear. N Engl J Med. 2008;359(20):2135–42. doi: 10.1056/NEJMcp0804745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daniel DM, Stone ML, Sachs R, Malcom L. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med. 1985;13(6):401–7. doi: 10.1177/036354658501300607. [DOI] [PubMed] [Google Scholar]
- 22.Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A Progressive 5-Week Exercise Therapy Program Leads to Significant Improvement in Knee Function Early After Anterior Cruciate Ligament Injury. J Orthop Sports Phys Ther. 2010;40(11):705–21. doi: 10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Logerstedt D, Di Stasi S, Grindem H, Lynch A, Eitzen I, Engebretsen L, et al. Self-reported knee function can identify athletes who fail return-to-activity criteria up to 1 year after anterior cruciate ligament reconstruction: a delaware-oslo ACL cohort study. J Orthop Sports Phys Ther. 2014;44(12):914–23. doi: 10.2519/jospt.2014.4852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hartigan EH, Axe MJ, Snyder-Mackler L. Time Line for Noncopers to Pass Return-to-Sports Criteria After Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther. 2010;40(3):141–54. doi: 10.2519/jospt.2010.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Logerstedt D, Grindem H, Lynch A, Eitzen I, Engebretsen L, Risberg MA, et al. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40(10):2348–56. doi: 10.1177/0363546512457551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grindem H, Logerstedt D, Eitzen I, Moksnes H, Axe MJ, Snyder-Mackler L, et al. Single-legged hop tests as predictors of self-reported knee function in nonoperatively treated individuals with anterior cruciate ligament injury. Am J Sports Med. 2011;39(11):2347–54. doi: 10.1177/0363546511417085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80(8):1132–45. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 28.van Meer BL, Meuffels DE, van Eijsden WA, Verhaar JA, Bierma-Zeinstra SM, Reijman M. Which determinants predict tibiofemoral and patellofemoral osteoarthritis after anterior cruciate ligament injury? A systematic review. Br J Sports Med. 2015;49(15):975–83. doi: 10.1136/bjsports-2013-093258. [DOI] [PubMed] [Google Scholar]
- 29.Granan LP, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004–2007: baseline epidemiology. Acta Orthop. 2009;80(5):563–7. doi: 10.3109/17453670903350107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–42. doi: 10.1056/NEJMoa0907797. [DOI] [PubMed] [Google Scholar]
- 31.Laboute E, Savalli L, Puig P, Trouve P, Sabot G, Monnier G, et al. Analysis of return to competition and repeat rupture for 298 anterior cruciate ligament reconstructions with patellar or hamstring tendon autograft in sportspeople. Ann Phys Rehabil Med. 2010;53(10):598–614. doi: 10.1016/j.rehab.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 32.Grindem H, Granan LP, Risberg MA, Engebretsen L, Snyder-Mackler L, Eitzen I. How does a combined preoperative and postoperative rehabilitation programme influence the outcome of ACL reconstruction 2 years after surgery? A comparison between patients in the Delaware-Oslo ACL Cohort and the Norwegian National Knee Ligament Registry. Br J Sports Med. 2015;49(6):385–9. doi: 10.1136/bjsports-2014-093891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Palmieri-Smith RM, Lepley LK. Quadriceps Strength Asymmetry After Anterior Cruciate Ligament Reconstruction Alters Knee Joint Biomechanics and Functional Performance at Time of Return to Activity. Am J Sports Med. 2015;43(7):1662–9. doi: 10.1177/0363546515578252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–78. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Øiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23(2):171–7. doi: 10.1016/j.joca.2014.10.008. [DOI] [PubMed] [Google Scholar]