Abstract
Objective
To use meta-analytic techniques to assess average effect sizes in studies of: (1) the correlation between patient health literacy and both medication and non-medication adherence, and (2) the efficacy of health literacy interventions on improving health literacy and treatment adherence.
Methods
PsychINFO and PubMed databases were searched (1948–2012). A total of 220 published articles met the criteria for inclusion; effect sizes were extracted and articles were coded for moderators.
Results
Health literacy was positively associated with adherence (r= .14), and this association was significantly higher among non-medication regimens and in samples with cardiovascular disease. Health literacy interventions increased both health literacy (r = .22) and adherence outcomes (r= .16). Moderator analyses revealed greater intervention efficacy when health literacy and adherence were assessed using subjective measures compared to objective measures. Health literacy interventions had a greater effect on adherence in samples of lower income and of racial-ethnic minority patients than in non-minority and higher income samples.
Conclusion
This is the first study to synthesize both correlational and intervention studies examining the relationship between health literacy and adherence to both medication and non-medication regimens.
Implications
These findings demonstrate the importance of health literacy and the efficacy of health literacy interventions especially among more vulnerable patient groups.
Keywords: health literacy, patient adherence, compliance, health literacy interventions, and meta-analysis
1. Introduction
Patient adherence (also called compliance) is defined as the degree to which patients follow treatment recommendations prescribed by their clinician or health care provider [1]. Adherence has been found to have positive and significant effects on treatment outcomes [2, 3]. Rates of adherence, however, vary widely across different patient populations, treatment regimens, and disease types. On average 25%, of patients are nonadherent to prevention and disease management activities including medication taking, appointment keeping, screening, exercise, and dietary changes [4]. For chronic disease management, nearly 50% of patients fail to adhere to their medical directives [5]. Adherence is driven by many factors including: patients’ lack of understanding of their disease and associated treatment, patients’ beliefs about the benefits and efficacy of prescribed regimens, real or perceived barriers (e.g., side effects, financial constraints), treatment regimen demands, depression, and patients’ lack of social support [3, 6, 7]. In order to improve adherence, patients need to clearly and appropriately understand health information related to their specific illness or disease. This understanding may be essential to helping patients generate the motivation, beliefs, and appropriate health behaviors needed to improve overall adherence behaviors [3, 8].
1.1 Health literacy and Adherence Relationship
Current research suggests that improving patients’ health literacy can be used as an effective education and prevention tool to improve disease management behaviors, including treatment adherence [9, 10, 11]. Health literacy is defined as patients’ ability to obtain, process, communicate and understand basic health information and services needed to make appropriate health decisions [9, 10]. Thus, when patients are adequately informed and understand clearly what they are asked to do, they are better able to share in the decisions that affect their health, and are thus more adherent to regimens that they had a part in choosing [3, 12]. In the United States over 90 million people lack the health literacy skills needed to properly understand and act on health information given by their providers [13]. Low patient health literacy has been associated with poor health outcomes, including: suboptimal use of preventive services, delays in diagnoses, higher rates of hospitalization, and increased risk of mortality among adults [14, 15]. Individuals with poor health literacy often incur higher medical costs and have been found in many studies to receive lower quality health services [16, 17, 18].
Several empirical studies suggest that health literacy is essential to improving medication adherence because aspects of information exchange and patient’s understanding of their medication information are often overlooked by health professionals [19]. Health literacy also predicts the acquisition of knowledge about self-management in the care of asthma; several empirical intervention studies show a strong association between asthma medication refill adherence and health literacy [19, 20, 21]. Some studies have found no health literacy-adherence relationship, however. For example, in one longitudinal study, health literacy was unrelated to antiretroviral adherence because once in a therapeutic state, even patients with low health literacy effectively utilized disease management skills and maintain their adherence over time [20]. Inconsistent findings suggest the need to better understand the corpus of empirical research on the health literacy-adherence relationship; this understanding is fundamental to the design of initiatives aimed at improving health care delivery.
1.2 Present Meta-Analysis Goals
The current research addresses the following questions using quantitative meta-analytic techniques. First, is there a relationship between patient health literacy and treatment adherence, and how large is this association on average? Second, are health literacy interventions effective at improving a patient’s level of health literacy? Third, are health literacy interventions effective at improving patients’ adherence to medical treatment? Finally, to what extent do variations in patient characteristics, diseases, regimens, treatment setting characteristics, and measurement strategies moderate these effects? The techniques of meta-analysis allow empirical assessment of these questions [22].
2. Methods
Each article was coded for how adherence was measured, including subjective or objective measures. Subjective measures included self-reports or questionnaires, self-report diaries, and other reports (e.g., parent, family member, spouse, or researcher); objective measures included pill counts, electronic pill monitors (e.g., Medication Event Monitoring System), pharmacy or medical records, and physiological markers or tests. Articles were also coded for the type of adherence measure (e.g., dichotomous or continuous), type of regimen (e.g., medication, appointment and screening appointment- keeping, diet or exercise), and study and sample characteristics (average income of patients in the study and location of the research). In addition, due to the variability in the current literature regarding the definition or conceptualization of health literacy each article was coded for how health literacy was conceptualized and measured. For example, some conceptualized health literacy as the personal, cognitive, and social ability of individuals to access, understand, and use health-related information to promote and maintain good health [23]. Other conceptualizations included educational level or health numeracy (which involves the understanding and processing of numerical, quantitative, and graphical health information) [24, 25]. These conceptualizations are based on constructs reviewed and conceptually underpinned in the literature and include the following definitions used by researchers: “patient health literacy”, “patients’ health knowledge”, “functional literacy”, “patient educational level”, “health numeracy”, and “access to health messages or information.” Examples of how health literacy was measured and coded for each study in this meta-analysis include: patient interviews, surveys, questionnaires and assessments (e.g., Test of Functional Health Literacy in Adults (TOFHLA) and Rapid Estimate of Adult Literacy in Medicine (REALM)). Refer to Table 1 for detail.
Table 1.
Moderator Variables Coded in 48 Correlational, 71 Health Literacy Interventions to Improve Patient Health Literacy, and 101 Health Literacy Interventions to Improve Patient Adherence Studies
| Moderator variables coded in studies | Distribution of codes analyzed; number of samples in coded categories |
|---|---|
| Study characteristics | |
| Source of articlea | 32 from bottom-up search; 174 from top-down search; 14 from reference searches |
| Location of study | 101 studies located in the U.S.; 117 located outside the U.S.; 4 with unspecified locations; 2 located in multiple categories |
| Context of care | 3 studies set in HMOs; 4 in Veterans Affairs hospitals; 41 in university medical centers; 6 in private practices; 39 in clinics; 49 in hospitals; 6 in patient homes; 99 in other settings; 24 in multiple categories |
| Conceptualizations of health literacy | 6 studies used health literacy; 31 used health knowledge, education and understanding (no intervention); 74 used health knowledge and understanding (due to intervention); 10 used functional literacy; 32 used education level; 5 used access to health messages or information; 2 used technologies assistance with regimen; 55 used combined categories |
| Health Literacy | |
| Health literacy assessment | 10 studies used surveys; 20 used patient interviews; 94 used questionnaires and assessments (e.g., TOFHLA or REALM); 17 used other forms of assessment; 19 used combined categories |
| Who rated patient health literacy | 78 studies included patients rating health literacy; 11 included doctors; 10 included parents; 12 included other raters; 13 included unspecified raters; 4 included multiple categories |
| Adherence | |
| Adherence assessment | Subjective measures included: 88 self-reports or questionnaire studies; 10 patient diary studies; 25 “other” reported studies. Objective measures included: 21 pill count studies; 30 physical examination studies; 16 electronic assessment studies; 8 used MEMS; 9 pharmacy refill studies; 2 appointment-keeping studies; 3 medical record studies; 49 combined category studies |
| Who rated patient adherence | 84 studies included patients rating health literacy; 32 included doctors; 9 included parents; 53 included other raters; 12 included unspecified raters; 38 included multiple categories |
| Patient & treatment characteristics | |
| Illness type | 18 studies included patients with HIV/AIDS; 13 with cancer; 25 with cardiovascular disease; 5 with end stage renal disease; 17 with pulmonary disease; 6 with gastrointestinal disorders; 2 with blood disorders; 27 with diabetes; 32 with asthma; 3 with OB-GYN related illnesses; 9 with arthritis; 3 with transplants; 1 with infections; 5 with osteoporosis; 76 with other illnesses; 18 with multiple categories |
| Treatment regimen | 144 studies included patients with medication regimens; 27 with diet regimens; 8 with exercise regimens; 10 with screening regimens; 39 with behavior regimens; 21 with appointment regimens; 1 with vaccination regimens; 27 with other regimens; 38 with combined categories |
| Ethnicity | 22 studies included patients of Asian ethnicity; 72 of African ethnicity; 70 of Caucasian ethnicity; 35 of Latino ethnicity; 1 of Pacific Islander ethnicity; 41 of other ethnicity; 126 of unspecified ethnicity; 63 of combined categories |
| Income | 24 studies included patient with incomes less than $8,375; 33 between $8,375 and $34,000; 12 between $34,000 and $82,400; 11 between $82,400 and $171,850; 11 between $171,850 and $373,650; 11 greater than $373,650; 193 with unspecified income; 28 with multiple categories |
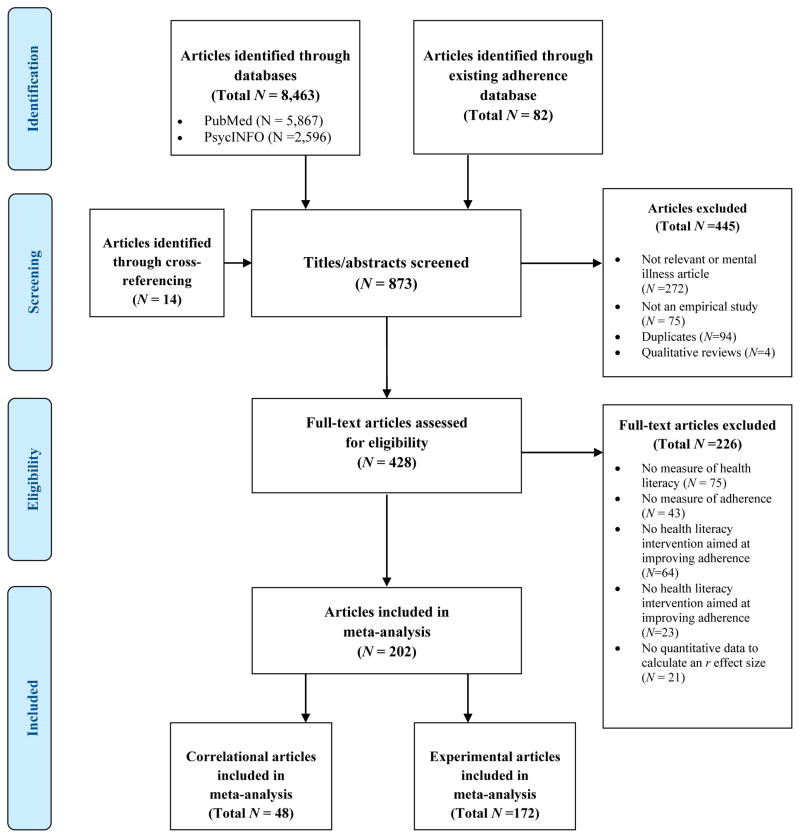
See the PRISMA flow diagram that shows the samples of studies searched (from the year 1948–2011) and the inclusion and exclusions results to get to the final sample of 220 total empirical articles used in this meta-analysis.
2.1 Inclusion/exclusion criteria
Empirical studies were included if they: (1) were published in a peer-reviewed, English language journal, (2) defined and explained a method of measuring patient adherence (or compliance), (3) defined a method of measuring health literacy (using any conceptualization listed above), and (4) provided a measure of or means to calculate the correlation between patient health literacy and adherence and/or the effect size measuring the effect of a health literacy intervention on patient health literacy and/or patient adherence. Meta-analytic techniques were used to extract (or calculate) and average “r” effect sizes and assess their significance. There were 48 studies correlating health literacy and adherence, 71 studies examining the effects of health literacy interventions on improving health literacy, and 101 studies examining the effects of health literacy interventions on improving adherence. Studies that focused on adherence to regimens for mental health, psychiatric disorders, or substance abuse were not included in the present meta-analysis. In these conditions, the reasons for nonadherence (e.g., cognitive, emotional, social dysfunction) and variability in types of therapy or treatment (e.g., medication, counseling) can make comparison with non-psychiatric chronic or acute disease difficult [26]. Meta-analytic work focusing on adherence in mental health care is receiving attention, and variability in cultural values, disease severity, and comorbidities are being systematically examined [26].
2.2 Search strategy
Several methods were used to achieve a complete census of the relevant research studies from the databases searched. The first strategy was a “top down” search using PubMed and PsychInfo from the year 1948 through 2012, using combinations of the following keywords: health literacy, patient literacy patient knowledge, health numeracy, functional literacy, education level with patient adherence, patient compliance, persistence and also randomized control trial and intervention. Second, a “bottom-up” search of an existing literature database on patient adherence (compliance) that is housed in the author’s laboratory was conducted. This database included empirical journal articles on patient adherence; further information can be found in previous meta-analyses [5–7, 27]. Lastly, the reference sections of included articles and literature reviews were examined (cross-reference method). A total of 220 studies met the inclusion criteria for inclusion in this meta-analysis (see Figure 1).
Figure 1.
PRISMA flow diagram
2.3 Statistical analyses
The effect size “r” was the statistical basis for this meta-analysis because “r” illustrates both the strength and direction of the relationship between variables [5, 22]. For the correlational studies, a positive r indicates that patients with higher health literacy are more adherent; a negative r indicates that those with higher health literacy are less adherent. For the intervention studies, a positive r indicates that an intervention aimed at improving patient health literacy is effective, and/or improves the adherence of patients who received the health literacy intervention. A negative r indicates that the intervention reduced patient’s level of health literacy and/or adherence to treatment.
The random effects model was used to compute and combine the effect size statistics, using the unweighted mean r based on k (the total number of studies included). The random effects model allows the generalization of findings beyond those included in this meta-analysis [22, 28]. The fixed effects model was also used to carry out weighted mean analyses and tests of heterogeneity, based on N (the total number of participants across all studies). Fixed effects tests are informative because they consider all participants in the studies, although the results are not as easy to generalize as random effects tests [22]. In order to address the file drawer problem, the fail-safe N was calculated. The fail-safe N indicates the number of null findings in studies, new, unpublished or not retrieved that would need to exist in order for significant results to be declared non-significant at p<.05 [29]. The standardized odds ratio and standardized relative risk (including confidence intervals) were also calculated from the unweighted mean r using the binomial effect size display (BESD). The BESD is an effect size estimator that can be used to display changes in success rates (i.e., survival or improvement rates) that are attributable to specific treatment procedure [29]. Preliminary statistical analyses (i.e., calculation of means, medians, standard deviations, correlations and t-tests) were conducted using SPSS 12.0; a TI-84 Plus graphing calculator and Excel 2008 v.12.2.3 were used for essential calculation verification. Moderator analyses were conducted using the random effects model t-tests to explore variability in effect sizes as a function of substantive and methodological differences between studies.
2.4 Article coding and effect size calculation
For the purpose of moderator analysis, each article was coded for specific variables (see Table 1). One coding team consisting of two trained coders (and the author) assigned categories for each study included. Any disagreements were discussed and negotiated between the two coders and the author before assigning a code. Thus, the percentage agreement among coders for each article was 100%. Prior to assigning codes for each journal article, each coder was trained to understand completely the meaning and conceptualization of each moderator variable included in this study. As part of the training, the author provided examples and coded several example journal articles to ensure that each coder understood the specific moderator inclusion criteria for this study. The effect size r of each study was extracted or computed from group means and standard deviations, or from Cohen’s d, t, Z, the exact p-value, chi-square, or the F-test (with 1 degree of freedom in the numerator); if a study reported and described the direction of a significant result but did not report an exact p-value, then the one-tailed p-value was assumed to be .025. If a study reported results that were non-significant and no exact p-value was provided then it was conservatively assigned p=.5 one-tailed, and r=0 [22]. An effect size of r=0 indicated that there is no relationship between health literacy and patient adherence or that health literacy interventions did not have an effect on health literacy or on adherence. For studies with multiple measures of adherence, the r for each measure was converted to a Fisher’s Zr and averaged for an overall effect size. All calculations involving r were performed by first transforming r to Fisher’s z transformation of r and then returning the results back to r [29]. Full references for all the empirical journal articles used in this meta-analysis including coding details can be found in Appendices A–C.
3. Results
3.1 Correlation of patient health literacy and treatment adherence
Across 48 studies, using both fixed (weighted mean) and random effect models, the average correlation between health literacy and patient adherence is positive and highly significant (p<. 001). Patients with higher levels of health literacy are more adherent to treatment. Based on the binomial effect size display (BESD), using the random effects unweighted mean r, there is a 14% higher risk of nonadherence [r= .14, 95% CI=. 08, .19] among patients who have lower health literacy than among patients with higher health literacy. The fail-safe N is well above the “tolerance level” of 250; over 3,191 unretrieved studies with an average of null effects would need to exist in order to render this finding nonsignificant. Nonadherence is more than 1.33 times higher (standardized relative risk) among individuals who have lower health literacy. The odds of patients adhering are 1.76 times better (standardized odds ratio) if they have higher health literacy. Table 2 details all meta-analysis results.
Table 2.
Summary of Meta-Analysis Results
| Effect of Health literacy | ka | Total Nb | Unweighted Median r (range)c | mean r [95% Confidence Interval] | mean r [95% Confidence Interval] | Fail safe Nd | Odds Ratio [95% Confidence Interval]e | Relative Risk [95% Confidence Interval]e |
|---|---|---|---|---|---|---|---|---|
| Health literacy and adherence correlationf | 48 | 19072 | 0.10 (−0.60, 0.80) | 0.12 [0.10, 0.13] ** | 0.14 [0.08, 0.19] ** | 3191 (tolerance level 250) | 1.76 [1.38, 2.16] | 1.33 [1.17, 1.47] |
| Health literacy interventions aimed at improving health literacyg | 71 | 12691 | 0.20 (0.06, 0.56) | 0.14 [0.12, 0.16] ** | 0.22 [0.18, 0.25] ** | 7922 (tolerance level 365) | 2.45 [2.07, 2.78] | 1.56 [1.44, 1.67] |
| Health literacy interventions aimed at improving patient adherenceh | 101 | 20545 | 0.15 (−0.08, 0.49) | 0.10 [0.09, 0.12] ** | 0.16 [0.14, 0.19] ** | 10431 (tolerance level 515) | 1.91 [1.76, 2.16] | 1.38 [1.32, 1.47] |
Note.
p <.001
Number of samples;
total N across all samples;
for each sample, a positive r indicates that patients who are more health literate are more likely to be adherent or health literacy interventions were effective in improving a patient’s level of health literacy or adherence to treatment. A negative r indicates that patients who are more health literate are less likely to be adherent or health literacy interventions were not effective in improving a patient’s level of health literacy or adherence to treatment;
since the fail N exceeds the “level of tolerance for future null results” it is unlikely that the “file drawer problem” is a bias;
the binomial effects size display from the unweighted mean effects in the random effects model was used to obtain the standardized odds ratio and relative risk;
the heterogeneity test (k=48) for health literacy and adherence correlational studies is significant (X2= 591.36, p<.001);
the heterogeneity test (k=78) for health literacy interventions aimed at improving health literacy is significant (X2=235.10, p<.001);
the heterogeneity test (k=101) health literacy interventions aimed at improving patient adherence is significant (X2= 249.87, p<.001)
Table 3 shows significant moderators at the random effects level. The correlation between health literacy and patient adherence was significantly higher when the treatment regimen was a non-medication regimen and when the disease type was cardiovascular disease. No other potential moderators approached even borderline significance, including the variable categorizing the conceptualization of health literacy.
Table 3.
Significant Moderators in Correlational and Experimental Studies
| Moderating variable | Categories | No. of studies in each group | Group means (SD) | t significance test (random effects model: t (df), p, r effect size) |
|---|---|---|---|---|
| Correlational studies | ||||
| Treatment regimen | Medication | 33 | 0.09 (.11) | t(46) = −2.443, p = .018, r = .34 |
| Not | 15 | 0.20 (.20) | ||
| Patient illness | Cardiovascular disease | 6 | 0.27 (.30) | t(46) = 2.564, p = .014, r = .35 |
| Not | 42 | 0.11 (.11) | ||
| Health literacy interventions to improve patient health literacy | ||||
| Health literacy assessed by | Subjective measure | 43 | 0.26 (.13) | t(69) = 3.992, p < .001, r = .43 |
| Not | 28 | 0.14 (.13) | ||
| Health literacy rated by | Patient | 49 | 0.24 (.14) | t(69) = 2.251, p = .028, r =.26 |
| Not | 22 | 0.16 (.14) | ||
| Location of study | US | 29 | .17 (.14) | t(69) = −1.971, p = .053, r = .23 |
| Not | 42 | .24 (.14) | ||
| Context of care | University Medical Center | 14 | .14 (.13) | t(69) = −2.170, p = .033, r = .25 |
| Not | 57 | .23 (.14) | ||
| Patient income | Less than $8,375 | 7 | .09 (.11) | t(69) = −2.345, p = .022, r = .27 |
| Not | 64 | .22 (.14) | ||
| Health literacy interventions to improve patient adherence | ||||
| Adherence assessed | Subjective measure | 10 | .32 (.10) | t(99) = 4.578, p < .001, r = .42 |
| Not | 91 | .14 (.12) | ||
| Patient ethnicity | Caucasian | 30 | .12 (.12) | t(99) = −2.060, p = .042, r = .20 |
| Not | 71 | .18 (.12) | ||
3.2 Effect of health literacy interventions on improving health literacy
Table 2 summarizes the result of 71 studies examining the effect of health literacy interventions on improving patients’ level of health literacy. Of these effect sizes, 65 were positive (indicating that interventions improved, rather than reduced, health literacy); 6 were reported as zero. The average of these 71 effects was significantly higher than zero (using fixed and random effects models); thus, health literacy interventions were found, on average, to significantly improve patients’ health literacy (p<. 001). Based on the random effects unweighted mean, there is a 22% difference in risk of low health literacy [r=. 22, 95% CI= .18, .25] (BESD based) among patients who do participate in a health literacy intervention compared to those who do not. The fail-safe N exceeds the tolerance level (365) and indicates that over 7,922 unpublished, unretrieved studies averaging effect sizes of .00, would need to exist in order to render this finding nonsignificant. The risk of low health literacy is more than 1.56 times higher among patients who do not receive interventions, and the odds of having higher health literacy are 2.45 times higher if a patient participates in a health literacy intervention.
Analysis using random effects model t-tests produced 5 significant moderators. Health literacy interventions aimed at improving a patient’s level of health literacy were more effective if health literacy was assessed using subjective measurements, and if patients rated their own level of health literacy as opposed to having another rate it (e.g., spouse or health care provider). Health literacy intervention studies were more effective outside the US compared with inside the U.S, and in settings other than University Medical Centers, where the efficacy of health literacy intervention was lower. Health literacy interventions were more effective in studies with low-income patients (Table 3).
3.3 Effect of Health Literacy Interventions on Patient Adherence
Across 101 studies, the effect of health literacy interventions on adherence was positive and significant (p<. 001). Based on the random effects unweighted mean, there is a 16% higher risk of nonadherence [r=. 16, 95% CI= .14, .19] (BESD based) among patients who do not participate in a health literacy intervention than among patients that do (see Table 2). The fail-safe N is higher than the tolerance level of 520; over 10,845 unpublished, unretrieved studies, averaging effect sizes of .00, would be needed to render this finding nonsignificant. The risk of nonadherence is more than 1.38 times higher among patients who did not participate in interventions, and the odds of a patient adhering are 1.91 times better if the patient participates in an intervention. Moderators were tested using the random-effects model approach and produced 2 significant moderators. Interventions were more effective in improving patient adherence when adherence was assessed using subjective measures, and when the study involved a sample of patients of non-Caucasian ethnicity. All t-tests and accompanying means and standard deviations are presented in Table 3.
4. Discussion
4.1 Discussion
Patients with higher levels of health literacy have rates of adherence that are, on average, 14% higher than patients that have low health literacy skills, according to the BESD. In addition, health literacy interventions are effective in improving patients’ levels of health literacy (22%) and adherence to treatment (16%). Two important disease and treatment regimen factors moderate the relationship between health literacy and patient adherence. The average correlation between health literacy and patient adherence is higher in studies of patients with cardiovascular disease compared with studies of patients with other disease conditions. Perhaps because the consequences of both medication and lifestyle nonadherence in cardiovascular disease can be severe (e.g., lack of blood pressure control, inhibition of lipoprotein cholesterol reduction, and increased mortality), patients may be more motivated to adhere when properly educated and given the opportunity to understand their treatment regimens [30]. It is also possible that despite extensive examination of possible moderating variables, the studies differed in ways not accounted for by coded moderators.
Moderator analyses also showed that the average relationship between health literacy and adherence is higher in non-medication regimens (e.g., lifestyle, exercise, diet) compared with medication regimens. Health behavior change and complex treatment management behaviors (such as glucose testing) may demand greater patient health literacy than does medication adherence. This difference may be illustrated in the relay of instructions, which can be more complex than simply taking medication and can be quite confusing to patients; elderly patients with low to marginal health literacy in one study were more likely to be nonadherent because they misunderstood their hospital discharge instructions given by their clinicians [31]. Frequent clinician contact with patients may be necessary to address inconsistencies and questions that arise, particularly with patients of low health literacy, whom may not be equipped to gather necessary information on their own [32, 33]. Studies assessing various health-related materials, such as informed consent forms and medication package inserts, have also found drastic inconsistencies in the reading levels of the material and the reading skills of the intended audience [34]. Research suggests that health care professionals must ensure that their patients understand their treatment recommendations by using literacy-dependent teaching methods (e.g., the “teach-back” method) and reinforcing education about their patients’ conditions over time [33].
Contrary to what was expected, moderator analyses revealed no statistical differences in the conceptualizations of health literacy (e.g., “patients’ health knowledge,” “functional literacy,” “patient educational level,” “health numeracy,” and “access to health messages or information”) on improving health literacy or adherence. Perhaps these findings are a result of the variability in the term “health literacy.”
Several methodological and measurement moderators increased the effect of health literacy interventions on patients’ level of health literacy. These included: health literacy assessment (effect size higher for subjective measures versus objective measures), health literacy rating (effect size higher when assessed by the patient versus by clinician or other members of the medical team, differences in reliability and validity of measurements might account for these differences in average effects), location of study (effect size lower in U.S vs. non-U.S.), and context of care (effects size lower in University medical center versus other, such as HMO, community medical practice, and Veteran Affairs Hospital). Health literacy interventions were also more effective in improving patients’ health literacy in studies of lower income patients than in studies of patients with higher income. This finding is of particular interest considering past research showing that low income and traditionally underserved populations are specifically at risk of low health literacy [21, 35, 36].
Additionally, patients who received interventions to improve their health literacy had a 16% higher rate of treatment adherence than did those who did not participate in the intervention. According the binomial effect size display there is a 16% risk difference in adherence between individuals who receive, and those who do not receive health literacy interventions. Applying this 16% risk difference in adherence to the Institute of Medicine’s estimate of 90 million low health literacy adults in the US yields an estimate that 14.4 million patients might be more adherent if they are offered interventions to improve their health literacy.
Moderator analyses show that in studies in which the outcome of patient adherence was assessed by subjective measures, health literacy training yielded a stronger effect on patient adherence than when adherence was assessed using other more objective methods. Additionally, health literacy training did not improve adherence as much in studies with mostly Caucasian patients as it did in studies with patients of other (usually minority) ethnicities. This suggests the even greater benefit of health literacy interventions in vulnerable populations and the need for health literacy training as part of comprehensive care. Since methodological and measurement design moderators do influence the relationship between health literacy and adherence, such variation should continue to be studied in future research.
Note of potential limitations of this study is in order. Although several literature search strategies were utilized here, it is possible that some studies were missed unintentionally. Studies with statistically significant findings may have had greater likelihood of publication. The large fail-safe N’s makes it unlikely that any missed or unpublished studies would dramatically change the current results, however, and the “file drawer bias” is unlikely to be a major problem. It is possible that although many conceptualizations of health literacy were identified in this meta-analysis, other conceptual approaches to health literacy, not used here, would yield additional studies.
4.2 Conclusion
The present study offers an extensive review of the empirical literature and a quantitative assessment of the health literacy-adherence relationship and its moderators, as well as an assessment of the effect of interventions to improve health literacy and treatment adherence. The present work extends to several disease management regimens beyond medication adherence and includes appointment keeping, screening (e.g., breast cancer and HIV screening), and exercise and dietary changes, among other health behaviors. The first part of this meta-analysis involves the correlation between health literacy and adherence, limiting causal inference; however, studies of health literacy interventions and their effect on adherence are also examined, and suggest a strong positive effect. The incorporation and quantitative examination of experimental studies of health literacy interventions aimed at improving health literacy and adherence does support some causal interpretation, thus this is the first study to support directionality of the health literacy-adherence relationship.
This study also emphasizes the importance of attention to methodological choices made and suggests that the type and quality of measurement assessments can greatly affect the health literacy-adherence relationship. Scale type, number of measures, and use of self-reports can moderate the adherence-outcome relationships [7]. Multiple and continuous adherence assessments may offer greater reliability and validity, and variations in measurement assessments should continue to be examined [7].
The findings of the present study also contribute further to understanding the components of health literacy interventions that can increase both health literacy and treatment adherence. Components of effective health literacy interventions in this study that produced the largest average effect sizes between the efficacy of health literacy interventions on improving health literacy and treatment adherence incorporated aspects of patient education through information handouts or pamphlets, audiovisual offerings, online resources, educational software programs, and web-based educational applications regarding particular disease conditions, disease management, and social support resources. In addition, some interventions emphasized and incorporated effective communication between patients’ and health care providers to better address patients’ questions and concerns. Future research should continue to focus closely on identifying specific aspects of health literacy interventions that are most effective in improving patients’ level of health literacy and adherence. Additionally, researchers should utilize longitudinal studies that examine the health literacy-adherence relationship over time in order to gain a better understanding of the factors that affect health outcomes in vulnerable patient populations.
4.3 Practice Implications
Research on the health literacy-adherence relationship suggests some important clinical recommendations. First, medical teams should incorporate literacy-dependent teaching methods to educate their patients about their condition in effort to increase adherence behaviors [37]. For example, clinicians should focus on utilizing face-to face communication in combination with supplemental methods of transmitting appropriate health information using language and medical terminology that is completely understood by patients [38, 39]. Additionally, through shared decision-making, patients and their providers can effectively collaborate towards treatment plans that are conducive to healthy patients’ lifestyles and for which there is realistic assessment of patients’ health knowledge and understanding of their regimen. Taking the proper steps towards these goals can help patients to adopt more effective disease management skills.
Highlights.
Examined correlational and intervention studies of health literacy-adherence relationship.
Health literacy positively associated with adherence to non-medication regimens.
Health literacy positively associated with adherence in cardiovascular disease patients.
Health literacy interventions increased patients’ health literacy and treatment adherence.
First meta-analysis to suggest directionality of health literacy-adherence relationship.
Acknowledgments
This research was conducted in the Health Communication Lab at UC Riverside and was supported by a Robert Wood Johnson Investigator Award in Health Policy, and by NIH grant 5R03AG27552-02 to M. Robin DiMatteo, the author’s dissertation advisor. Thanks are due to Dr. M. Robin DiMatteo for her continued guidance and expertise in meta-analysis. Thank you to Dr. Robert Rosenthal for his advice and feedback on this meta-analysis. Thank you also to Allen Roughton for diligently helping to organize, code, analyze moderators and manage data tables for this meta-analysis, and to research assistants Pablo Ruiz, Samantha Ratnayake, Ashlee Randolph, Natalie Gonzales, Vanessa Gutierrez, Shriraj Shah, and Punam Patel for their assistance with literature searching and code checking.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Vermeire E, Hearnshaw H, Van Royen P, et al. Patient adherence to treatment: Three decades of research: A comprehensive review. J Clin Pharm Ther. 2001;26:331–342. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 2.Modi AC, Quittner AL. Barriers to treatment adherence for children with cystic fibrosis and asthma: What gets in the way? J Pediatr Psychol. 2006;31:846–858. doi: 10.1093/jpepsy/jsj096. [DOI] [PubMed] [Google Scholar]
- 3.DiMatteo MR, Haskard-Zolnierek KB, Martin LR. Improving patient adherence: A three-factor model to guide practice. Health Psychol Rev. 2012;6:74–91. [Google Scholar]
- 4.DiMatteo MR. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychol. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 5.Haskard-Zolnierek KB, DiMatteo MR. Physician communication and patient adherence to treatment: A meta-analysis. Med Care. 2009;47:826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DiMatteo MR, Giordani PJ, Lepper HS, et al. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 7.DiMatteo MR. Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Med Care. 2004b;42:200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 8.Martin LR, Haskard-Zolnierek KB, DiMatteo MR. Health behavior change and treatment adherence. New York: Oxford University Press, Inc; 2010. [Google Scholar]
- 9.Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21:878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolf MS, Davis TC, Osborn CY, et al. Literacy, self-efficacy, and HIV medication adherence. Patient Educ Couns. 2007;65:253–260. doi: 10.1016/j.pec.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Zhang NJ, Terry A, McHorney CA. Impact of health literacy on medication adherence: a systematic review and meta-analysis. Ann Phamacother. 2014;48:741–751. doi: 10.1177/1060028014526562. [DOI] [PubMed] [Google Scholar]
- 12.Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60:301–312. doi: 10.1016/j.pec.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine. Health literacy: A prescription to end confusion. Washington DC: National Academy Press; 2004. [Google Scholar]
- 14.Gazmararian JA, Williams MV, Peel J, et al. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 15.Gazmararian JA, Baker DW, Wolf MS, et al. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167:1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 16.Weiss BD, Palmer R. Relationship between health care costs and very low literacy skills in a medically needy and indigent Medicaid population. J Am Board Fam Pract. 2004;17:44–47. doi: 10.3122/jabfm.17.1.44. [DOI] [PubMed] [Google Scholar]
- 17.Gazmararian J, Howard DH, Parker RM. The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am J Med. 2005;118:371–377. doi: 10.1016/j.amjmed.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 18.Fry-Bowers EK, Maliski S, Lewis MA, et al. Health literacy and interpersonal interactions as predictors of maternal perception of ambulatory care for low-income, Latino children. Patient Education and Counseling. 2013;91(2):213–220. doi: 10.1016/j.pec.2012.12.019. [DOI] [PubMed] [Google Scholar]
- 19.Wagner CV, Steptoe A, Wolf MS, et al. Health literacy and health actions: A review and a framework from health psychology. Health Educ Behav. 2009;36:860–877. doi: 10.1177/1090198108322819. [DOI] [PubMed] [Google Scholar]
- 20.Mancuso CA, Rincon M. Impact of health literacy on longitudinal asthma outcomes. J Gen Intern Med. 2006;21:813–817. doi: 10.1111/j.1525-1497.2006.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paasche-Orlow MK, Cheng DM, Palepu A, et al. Health literacy, antiretroviral adherence, and HIV-RNA suppression: A longitudinal perspective. J Gen Intern Med. 2006;21:835–840. doi: 10.1111/j.1525-1497.2006.00527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenthal R, DiMatteo MR. Meta-analysis: Recent developments in quantitative methods for literature reviews. Annu Rev Psychol. 2001;52:59–82. doi: 10.1146/annurev.psych.52.1.59. [DOI] [PubMed] [Google Scholar]
- 23.Berkman ND, Davis TC, McCormack L. Health literacy: What is it? J Health Commun. 2010;15:9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- 24.Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67:2072–2078. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 25.Goldbeck AL, Ahlers-Schmidt CR, Paschal, et al. A definition and operational framework of health numeracy: A definition and operational framework of health numeracy. Am J Prev Med. 2005;29:375–376. doi: 10.1016/j.amepre.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 26.Sin NL, DiMatteo MR. Depression treatment enhances adherence to antiretroviral therapy: A meta-analysis. Ann Behav Med. 2013;47:259–269. doi: 10.1007/s12160-013-9559-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DiMatteo MR, Haskard KB, Williams SL. Health beliefs, disease severity, and patient adherence: A meta-analysis. Med Care. 2007;45:521–528. doi: 10.1097/MLR.0b013e318032937e. [DOI] [PubMed] [Google Scholar]
- 28.Frattaroli J. Experimental Disclosure and its Moderators: A Meta-Analysis. Psycholo Bull. 2006;132:823–865. doi: 10.1037/0033-2909.132.6.823. [DOI] [PubMed] [Google Scholar]
- 29.Rosenthal R, Rosnow RL. Essentials of behavioral research. New York, NY: The McGraw-Hill Companies; 2008. [Google Scholar]
- 30.Gazmararian JA, Kripalani S, Miller MJ, et al. Factors associated with medication refill adherence in cardiovascular-related diseases: A focus on health literacy. J Gen Intern Med. 2006;21:1215–1221. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paasche-Orlow MK, Wolf MS. The casual pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31:819–826. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 32.Kalichman SC, Cherry J, Cain D. Nurse-delivered antiretroviral treatment adherence intervention for people with low health literacy skills and living with HIV. J Assoc Nurses AIDS Care. 2005;16:3–15. doi: 10.1016/j.jana.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 33.Lindquist LA, Go L, Fleisher J, et al. Relationship of health literacy to intentional and unintentional non-adherence of hospital discharge medication. J Gen Intern Med. 2011;27:173–178. doi: 10.1007/s11606-011-1886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rudd R. Health literacy skills of US adults. Am J Health Behav. 2007;31:S8–S18. doi: 10.5555/ajhb.2007.31.supp.S8. [DOI] [PubMed] [Google Scholar]
- 35.Sudore RL, Landefeld CS, Williams BA, et al. Use of a modified informed consent process among vulnerable patients: A descriptive study. J Gen Intern Med. 2006;21:867–873. doi: 10.1111/j.1525-1497.2006.00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gazmararian JA, Baker DW, Williams MV, et al. Health literacy among medicare enrollees in a managed care organization. JAMA. 1999;1:545–551. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 37.Cooper LA, Roter DL, Johnson RL, et al. Patient-centered communication, rating of care, and concordance of patient and physician race. ACP J Club. 2003;139:907–9115. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 38.Schillinger D, Bindman A, Wang F, et al. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Educ Couns. 2004;52:315–323. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 39.Shaw A, Ibrahim S, Reid F, et al. Patients’ perspective of the doctor-patient relationship and information giving across a range of literacy levels. Patient Educ Couns. 2009;75:14–120. doi: 10.1016/j.pec.2008.09.026. [DOI] [PubMed] [Google Scholar]