Abstract
Purpose
Programs that address stroke family caregiver needs and skill-building are recommended based on the literature and patient care guidelines for stroke rehabilitation. The purpose of this study was to explore patterns of perceived needs and skill-building during a stroke caregiver intervention program.
Method
Descriptive statistics were used to analyze data from 123 stroke caregivers enrolled in the intervention group of a randomized controlled clinical trial. Caregivers received 8 weekly telephone sessions, with a booster session a month later. At each session, the Caregiver Needs and Concerns Checklist (CNCC) was used to identify and prioritize current needs that were then addressed through skill-building strategies.
Results
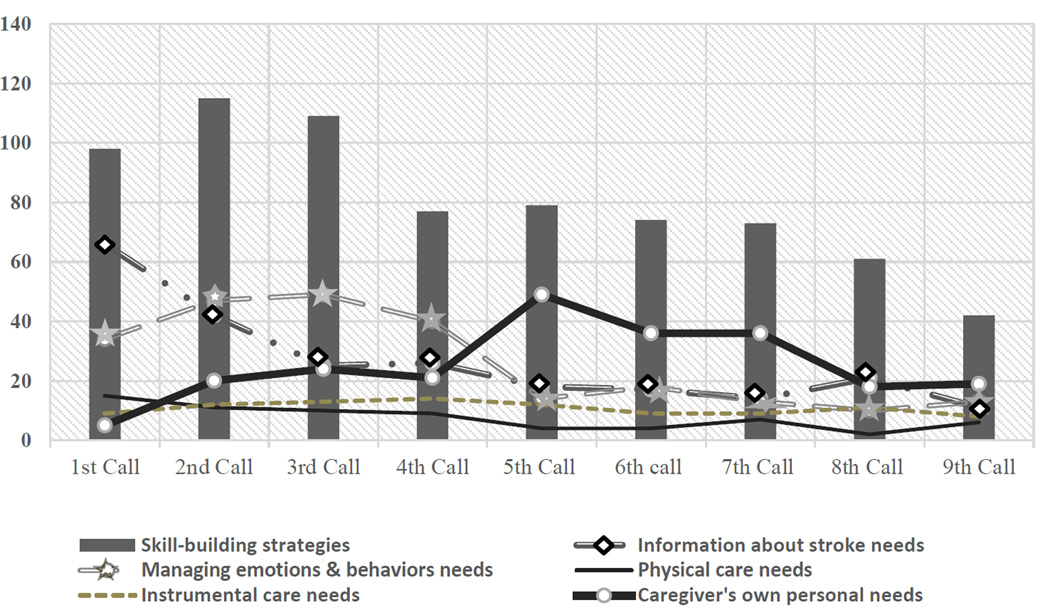
Perceived needs changed over time. Information about stroke was the highest priority need during Session 1. Managing survivor emotions and behaviors was the highest priority for Sessions 2 through 4. Caregivers generally waited until Sessions 5 through 9 to address their own emotional and physical health needs. Physical and instrumental care needs were relatively low but stable across all 9 sessions. Skill-building was consistently high, though it peaked during Sessions 2 and 3.
Conclusions
Tracking patterns of needs and skill-building suggest appropriate timing for targeting different types of family caregiver support during stroke rehabilitation.
Keywords: stroke, family, caregiver, stress, behavior, clinical trials
Stroke is a significant healthcare problem that impacts the whole family. Approximately 795,000 people experience a new or recurrent stroke in the United States each year [1]. World-wide, 25% to 74% of an estimated 50 million persons with stroke are partly or fully dependent on caregivers for activities of daily living [2]. The sudden crisis of stroke and lack of available stroke information and caregiving training [3–5], as well as lack of attention to caregivers from healthcare providers [6], result in caregivers experiencing a myriad of unmet needs [3, 7, 8]. These needs often center on caregivers’ limited understanding of stroke and a lack of education, training, and support in dealing with the patient’s physical and emotional needs [9, 10]. Other unmet caregiver needs, similar across countries and health care systems [11], are related to caregiver preparation, promoting the survivor’s function, sustaining the self and family, and adapting to a changed role [8, 10].
Although some studies have cited positive caregiver attitudes [12] and reduced caregiver stress [13] following stroke rehabilitation, other studies have highlighted problems. For example, Ski & O’Connell [14] found that rehabilitation was delayed by poor hospital follow-up procedures and that caregivers felt “let down” by the hospital discharge process because they were not given adequate information about community support services. Caregivers reported waiting up to 3 weeks after discharge before hospital staff contacted them about receiving occupational and physiotherapy in the home. Another study [5] found caregivers’ had unmet needs related to finding services addressing survivors’ emotional responses and difficult behaviors, as well as to finding resources for managing their own emotions, their reluctance to use resources for themselves, and their general lack of knowledge about which resources would help.
During the stroke recovery process, caregiver needs and corresponding skill-building interest evolve over time. For example, King & Semik [8] reported that the most difficult times for family caregivers were during the hospitalization period and the first months at home. During this period, not only are caregivers faced with sudden life changes due to their loved one’s stroke, but they must quickly learn the caregiver role and gain new skills [8, 11]. In the findings from Cobley et al., [9], O’Shea & Goode, [15], and Perry and Middleton [11], caregivers reported they were either not given any or enough information information about stroke, and communication mismatches were common. Caregivers described feeling isolated, neglected, and excluded from the discharge decision and planning process [9], and they wanted a more collaborative interaction with health care providers [16]. Wilz and Barskova [17] emphasized the importance of studying the long-term effects of caregiving, noting that their multi-component intervention for spousal stroke caregivers did not produce significant changes in caregiver depressive symptoms until six months after the intervention. These findings suggest that caregiver needs may change over the long term.
Cameron and colleagues [18] also demonstrated that caregiver needs evolve over time. In a qualitative study using the “Timing It Right” (TIR) framework, they found caregivers had different informational and instrumental support needs during each phase of the TIR framework. Needs were highest when preparing to bring the patient home and during the first few months at home [18]. Their study also reported a lack of agreement between the health care providers and caregivers regarding who should be the primary focus of care across all phases of the TIR framework. Health care providers consistently considered the patient as the primary focus of care. However, caregivers also wanted to receive support, beginning from the discharge (preparation) to the post-discharge (adaptation) phases [18], a finding consistent with other studies [8, 9, 15, 16].
Because the caregiver is primarily perceived as a resource for and providing assistance to the person with stroke, rather than someone who also needs support, caregiver needs are often overlooked [19]. Not only do caregivers experience unmet needs regarding the care of the person with stroke, but they also experience personal problems as they adapt to the many changes in their lives as a result of providing care [3, 10, 20, 21]. These include loss of employment, changes in their social life and emotional health, as well as additional responsibilities previously assumed by the person with stroke [3, 7, 9, 20]. In a meta-synthesis of qualitative research, Quinn and colleagues [10] identified themes such as searching for one’s own space and well-being, suffering in silence, putting one’s own needs aside, and adapting to a changed role. Barskova and Wilz [22] found that caregivers’ acceptance of a post-stroke life situation influenced stroke survivors’ cognitive and emotional recovery. Their findings further support the need to focus on caregiver life changes and how their personal responses to caregiving may impact the survivors’ recovery.
Caregiver needs and concerns expressed in a prior qualitative study were used to develop the Caregiver Needs and Concerns Checklist (CNCC) [3]. The checklist assesses needs in five main categories: 1) information about stroke; 2) managing survivor’s emotions and behaviors; 3) providing physical care; 4) providing instrumental care; and 5) addressing personal responses to caregiving. Other studies in this context [15, 19, 23–26] have identified similar unmet caregiver needs regarding stroke education and knowledge, managing survivor emotions and behaviors, providing physical care, and dealing with the impact of caregiving on their own lives.
Current recommendations for stroke caregiver interventions include incorporation of psycho-educational strategies addressing needs along with skill-building (e.g., problem solving, stress management, goal setting) for optimum effect [2, 18, 27–28]. The literature makes clear that no “one size fits all” intervention can be designed to address all needs of individual caregivers [2, 20, 27]. Perceived needs vary, and they evolve over time, consistent with Cameron’s “Timing it Right” framework [18]. This provides further rationale for individualized interventions teaching skill-building strategies such as problem solving and stress management [2, 27].
One example of the use of individualized interventions that incorporate information about skill-building strategies for stroke caregivers is the Telephone Assessment and Skill-building Kit (TASK) [29, 30]. TASK was developed based on a conceptual model derived from the CNCC [3, 29]. The protocol involved nurses who trained caregivers how to self-assess their needs using the CNCC during the early period after hospital discharge. Caregivers were trained how to use corresponding tip sheets within the TASK Resource Guide to address these perceived needs as they evolved over time. Caregivers used tip sheets that were primarily aimed at increasing stroke-related knowledge, but also tip sheets based on the principle skill-building processes in Lazarus’ Theory of Stress and Coping and Mishel’s Uncertainty in Illness Theory [29]. The skill-building tip sheets, which were tailored to the context of stroke caregiving, summarized strategies to strengthen existing skills, screen for caregiver depressive symptoms, maintain realistic expectations, engage in problem solving, communicate with health professionals, and manage stress [29]. Based on results from the TASK pilot [29, 30], the intervention was revised for the TASK II intervention, with tip sheets added about finding a nursing home and end-of-life care, as well as an additional assessment beginning with the 5th session involving caregiver life changes using the Bakas Caregiving Outcomes Scale (BCOS).
The purpose of this study was to explore patterns of perceived needs and concerns as they evolved over time in stroke caregivers randomized to the revised TASK II intervention, as well as to identify the most frequently used tip sheets, both those on stroke-related information and skill-building strategies, overs the intervention period.
Methods
Design
The parent study employed a randomized controlled clinical trial design to test efficacy of the revised Telephone Assessment and Skill-building Kit (TASK II) compared with an Information, Support, and Referral (ISR) intervention (NIH R01NR010388; ClinicalTrials.gov Identifier: NCT01275495). Within 8 weeks after the survivor was discharged home, the TASK II intervention group (n=123) received by mail the Telephone Assessment and Skill-Building Kit (TASK II) consisting of a TASK II Caregiver Resource Guide that included tip sheets addressing each perceived need or concern item on the CNCC, as well as tip sheets focused on skill-building strategies. The ISR intervention group (n=131) received by mail a brochure about stroke and caregiving from the American Stroke Association. Both groups received 8 weekly telephone calls to their homes from a nurse, with a booster session provided a month later (i.e., the 9th call). The TASK II calls focused on helping caregivers self-assess and prioritize their needs and concerns and address them using the tip sheets in the TASK II Caregiver Resource Guide. The ISR calls focused more on active listening and helping caregivers find information and referral in the brochure from the American Stroke Association. Analysis for the parent study is ongoing, with the primary outcomes being caregiver depressive symptoms, caregiving-related negative life changes, and unhealthy days. Secondary outcomes include caregiver task difficulty, optimism, and threat appraisal. The study was approved by the university institutional review board, and informed consent was provided by all participants.
This sub-study provides a descriptive analysis of the perceived priority needs and the skill-building tip sheets used by caregivers who were randomly assigned to the TASK II intervention. The aim was to identify patterns of expressed needs and interest in skill-building strategies and how these changed over the course of the TASK II intervention.
Sample
Stroke caregivers (n=123) who were randomized to the TASK II group within 8 weeks after discharge comprised the sample for this sub-study. Table 1 displays sample characteristics. Most participants were female (78.1%) and Caucasian (70.7%), and about half were spouses (48.0%). Non-spouses (52.0%) included adult children, adult children-in-law, other relatives, and significant others. About half of the persons with stroke were male (49.6%), and the survivors were rated by their caregivers using the Stroke Specific Quality of Life Scale Proxy as on average having moderate functioning in terms of mobility (Mean = 3.4) and thinking (Mean = 2.7), with possible scores ranging from 1 to 5 and higher scores indicating higher functioning [30].
Table 1.
Sample characteristics of TASK II intervention group (n=123).
| Characteristic | Mean (SD) (range) | f (%) |
|---|---|---|
| Caregiver Age in Years | 54 (12.5) (26–83) | |
| Caregiver Race | ||
| African-American | 30 (24.4%) | |
| White | 87 (70.7%) | |
| Asian | 2 (1.6%) | |
| American Indian/Alaskan Native | 1 (0.8%) | |
| More than 1 Race | 3 (2.4%) | |
| Caregiver Gender | ||
| Male | 27 (21.9%) | |
| Female | 96 (78.1%) | |
| Caregiver Relationship | ||
| Spouse | 59 (48.0%) | |
| Non-Spouse | 64 (52.0%) | |
| Survivor Age | 62.6 (14.4) (23–91) | |
| Survivor Race | ||
| African-American | 32 (26.0%) | |
| White | 87 (70.7%) | |
| Asian | 1 (0.8%) | |
| Hawaiian/Pacific Islander | 1 (0.8%) | |
| Other or Unknown | 1 (0.8%) | |
| Frequency Missing | 1 (0.8%) | |
| Survivor Gender | ||
| Male | 60 (49.6%) | |
| Female | 61 (50.4%) | |
| Survivor Mobility (SSQOL) | 3.4 (1.0) (1–5) | |
| Survivor Thinking (SSQOL) | 2.7 (1.0) (1–5) |
Procedures
Within 8 weeks of the survivor’s discharge home, telephone sessions took place every week for 8 weeks, with a booster session a month later. At each session, the CNCC was used by caregivers to identify and prioritize new concerns. The CNCC used in the TASK II program consisted of 35 perceived needs or concerns related to five main areas: a) information about stroke (8 items), b) managing survivor emotions and behaviors (8 items), c) providing physical care (5 items), d) providing instrumental care (5 items + 2 newly added), and e) caregivers’ personal responses to caregiving (7 items) [3, 29]. Information about stroke included content about warning signs of another stroke, lifestyle changes, and where to find resources. Managing survivor emotions and behaviors addressed the survivors’ feelings, personality changes, cognition, communication, and social activities. Providing physical care addressed medications, diet, exercise, mobility, and activities of daily living. Providing instrumental care focused on finances, legal healthcare issues, transportation, and respite care. The caregiver’s personal responses addressed topics relating to the caregiver’s emotions, social activities, and health. Balancing other responsibilities and asking for help were also included in this domain. Because the CNCC is a checklist with response options of yes or no for each need, psychometric data have not been provided for this instrument; however, the items were provided by actual caregivers and are consistent with the literature [8, 10, 18, 20]. The original TASK Resource Guide [29] consisted of tip sheets that were developed from each of the CNCC items. The TASK II Resource Guide added two new tip sheets in the instrumental care section about finding a nursing home and end-of-life care, respectively. Each CNCC item in the TASK II program had a corresponding content tip sheet in the TASK II Resource Guide for caregivers to use to address their priority needs.
Skill-building tip sheets were also used during the calls that addressed a) strengthening existing skills, b) screening for caregiver depressive symptoms, c), maintaining realistic schedules and expectations, d) problem-solving strategies, e) communication with health professionals, and e) a stress management workbook for caregivers and persons with stroke [29]. Nurses trained caregivers to choose skill-building tip sheets in the TASK II Resource Guide to further individualize their efforts in addressing their needs through skill-building strategies. Aside from the newly developed informational tip sheets regarding nursing home placement and end-of-life care, all of the content and skill-building tip sheets in the TASK II Resource Guide underwent extensive content validity testing with a total of 10 research, clinician, and lay caregiver experts [29]. The two newly included tip sheets were added based on caregiver feedback from our pilot work [29, 30], then were reviewed by three researchers with expertise in family caregiving, institutionalization, and end-of-life care.
Beginning with the 5th week, the BCOS [32, 33] was added as an additional assessment tool to enable caregivers to focus more on their personal needs and concerns [29, 30]. The BCOS consists of 15 different types of life changes experienced by family caregivers of persons with stroke. The items address changes in social functioning, well-being, and health specifically as a result of providing care. Psychometric properties have been reported for the BCOS providing evidence of internal consistency reliability (Cronbach alpha .90), test-retest reliability, and content, construct, and criterion-related validity [32, 33]. The BCOS items were tied to the CNCC items addressing the caregiver’s personal needs so that caregivers experiencing life changes could select the appropriate TASK II tip sheets to address these needs. For example, the BCOS item, “My physical health” was tied to the CNCC item and tip sheet entitled, “Taking care of my own health.” The BCOS item, “My emotional well-being” was tied to the CNCC item and tip sheet entitled, “Dealing with my emotions while providing care.” All 15 BCOS items were tied to one or more CNCC items and corresponding tip sheets.
The nurses taught caregivers how to self-identify their own needs using the CNCC and the BCOS, and then helped them learn how to select a priority need to focus on during each call. These priority needs were the focus of the analyses in the current study, with the aim of determining how the perceived needs changed over time. After informational tip sheets corresponding to the CNCC and the BCOS assessments were reviewed with the caregivers, nurses taught caregivers how to use the skill-building tip sheets (i.e., strengthening existing skills, screening for depressive symptoms, maintaining realistic schedules and expectations, problem solving, communication with healthcare professionals, stress management) to individualize their strategies for dealing with their needs and concerns. The skill-building tip sheets were regarded as the “process” tip sheets to enable caregivers to build their skills. During each call, the nurse recorded the specific needs and skill-building tip sheets selected by the caregiver as the priority for that call.
Data Analysis
Descriptive analyses (frequencies) were used to describe the types of needs and the use of skill-building tip sheets for those receiving the TASK II intervention over 8 weekly calls by a nurse and a booster session at 12 weeks (9th call). Changes in perceived needs and use of skill-building tip sheets over the 9 calls are depicted in Figure 1. Because caregivers’ personal needs were particularly of interest, those frequencies were converted to percentages and highlighted in the analyses (Table 2). That is, the frequency of the caregivers’ personal needs was divided by the total frequency of identified needs for that particular session, and then multiplied by 100 to create percentages. For example, in Session 1, 129 needs were expressed by the 123 caregivers randomized to the TASK II intervention. Out of those 129 needs, 5, or 3.9%, were related to the caregiver’s personal needs. For Session 2, 122 needs were expressed, and 20, or 15.1%, addressed the caregiver’s personal needs. We also compared the percentages of caregivers’ personal needs from the TASK II study with our original TASK pilot data to assess whether use of the BCOS to assist caregivers to focus on their own needs was effective (Table 2). The TASK pilot sample (n=21) [30] was not significantly different from the TASK II sample (n=123) in terms of age, race, type of relationship, or average survivor mobility and thinking scores. However, a larger proportion of caregivers in the TASK pilot were males compared with the TASK II study (38% and 22%, respectively).
Figure 1.
Patterns of priority needs and skill-building strategies over the 9 calls based on frequencies (N=123)
Table 2.
Frequencies and percentages of caregiver’s personal needs (emotional and physical health) out of the total needs identified during each session over the 9 calls.
| 1st f % |
2nd f % |
3rd f % |
4th f % |
5th f % |
6th f % |
7th f % |
8th f % |
9th f % |
Total f % |
|
|---|---|---|---|---|---|---|---|---|---|---|
| TASK | 3 | 4 | 2 | 1 | 5 | 4 | 5 | 2 | NA | 26 |
| (n=21) | 13.0 | 21.1 | 10.0 | 4.0 | 26.3 | 22.2 | 26.3 | 14.3 | NA | 16.6 |
| TASK II | 5 | 20 | 24 | 21 | 49 | 36 | 36 | 18 | 19 | 228 |
| (n=123) | 3.9 | 15.1 | 19.8 | 19.1 | 50.5 | 42.9 | 45.6 | 29.0 | 33.3 | 25.4 |
The number of minutes spent on the calls with the nurse was timed by the nurses during intervention delivery and is summarized in Table 3. The number of minutes caregivers had spent reading the TASK II Resource Guide since the previous session was collected from caregivers. These data were also summarized in Table 3.
Table 3.
Average number of minutes on the calls with the nurse and caregiver-reported time spent reading the TASK II Resource Guide between each session over the 9 calls.
| 1st M (SD) Range |
2nd M (SD) Range |
3rd M (SD) Range |
4th M (SD) Range |
5th M (SD) Range |
6th M (SD) Range |
7th M (SD) Range |
8th M (SD) Range |
9th M (SD) Range |
Total M (SD) Range |
|
|---|---|---|---|---|---|---|---|---|---|---|
|
Minutes on calls |
35.6 (13.7) 0–67 |
27.3 (16.7) 0–65 |
26.5 (16.7) 0–61 |
22.1 (16.4) 0–61 |
23.5 (17.4) 0–60 |
22.1 (17.2) 0–59 |
21.1 (16.8) 0–62 |
18.1 (15.6) 0–58 |
18.7 (15.6) 0–60 |
27.7 (15.1) 0–67 |
|
Minutes reading |
30.3 (64.4) 0–600 |
28.9 (51) 0–300 |
21.8 (42.2) 0–270 |
23.2 (40.1) 0–240 |
19.6 (52.6) 0–450 |
21.3 (46.2) 0–360 |
11.9 (22.3) 0–120 |
14.6 (27.7) 0–210 |
36.9 (115.1) 0–840 |
33.1 (66.5) 0–840 |
Results
Figure 1 displays frequencies of caregiver priority needs and use of skill-building tip sheets over 8 weekly calls by a nurse and a booster session at 12 weeks (9th call). Of the total 896 needs and concerns tip sheets used by the 123 caregivers over the 9 calls, 240 (26.8%) related to finding information about stroke, 238 (26.6%) to managing emotions and behaviors of the survivor, 68 (7.6%) to providing physical care, and 97 (10.8%) to providing instrumental care for the survivor. Caregivers generally waited until the 5th session to begin focusing on their own emotional and physical health needs, with 228 of the total of 896 (25.4%) focused in this area.
Information about stroke
From Figure 1, finding information about stroke and the related tip sheets were the highest priority, particularly during the first call. For example, there were 129 concerns identified by the 123 caregivers during the first call, 66 of which were in the area of finding information about stroke. Of these 66, 29 of the concerns were related to our first tip sheet"Warning Signs of Stroke.” This trend tapered off over the calls, but seemed to increase slightly around the 8th call, perhaps as a “refresher.” Other popular tip sheets in this area related to where to find resources, how to manage specific problems or complications of the person with stroke, recommended lifestyle changes, risk factors for stroke, and common medications.
Managing emotions and behaviors
Managing emotions and behaviors of the person with stroke was the second most common area of concern for caregivers over the 9 calls. This area was particularly relevant during the 3rd call, when 49 out of the total of 122 needs (40.2%) were in this area. In this category, the most widely used tip sheets focused on emotions of the person with stroke (e.g., depression, sadness, anger, or frustration), feelings about himself or herself (e.g., dependency or helplessness, worthlessness), behaviors exhibited by the person with stroke (e.g., losing temper, foul language, poor judgment, apathy, sudden crying or laughing outbursts), and problems with thinking (e.g., forgetfulness, memory loss, distraction, poor decision-making, or confusion). Other topics within this area included communication needs, affection and sexuality issues, as well as promoting social activities.
Physical and instrumental care needs
Surprisingly, there were relatively fewer needs related to providing physical and instrumental care expressed over the course of the 9 calls, although their frequencies remained fairly stable. Most of the physical care needs related to promoting exercise, ensuring a proper diet, medication management, getting to the bathroom, and avoiding falls. Instrumental care needs focused on finances, transportation, legal issues, and finding care while away. Few expressed concerns about end of life and finding a nursing home, and these concerns were addressed within the category of instrumental care.
Caregiver’s personal needs
Caregivers generally waited until Sessions 5 through 9 to begin to focus on taking care of themselves as a caregiver. For example, the caregiver’s personal needs were highest at the 5th call, representing 49 of the total 97 needs (50.5%) expressed by the 123 caregivers (Figure 1). This trend was similar to findings from our TASK pilot study (See Table 2). The trend was increased in the TASK II study because of a concerted effort to enhance this focus by using the BCOS to further assess life changes linked to needs in this area (Table 2). In the original TASK pilot, expressed needs in this area jumped from 4.0% for the 4th call to 26.3% for the 5th call. In our TASK II study, needs in this area increased from 19.1% in the 4th call to 50.5% in the 5th call after adding the BCOS addressing caregiver life changes as an additional assessment of needs. However, this increased focus on the caregiver’s own responses to the caregiving situation in the TASK II sample compared with the TASK pilot should be interpreted with caution since there were relatively fewer male caregivers in the TASK II study (22%). The most common tip sheet used in addressing the caregivers’ personal needs was dealing with one’s own emotions, which represented 29.8% of the needs in this area. Other tip sheets used in this area related to the caregiver’s energy level (14.9%), social activities (14.9%), balancing other responsibilities (11.4%), asking family and friends for help (11.0%), and taking care of his or her own health (11.0%).
Skill-building strategies
Use of the skill-building tip sheets was consistently high (See the bars in Figure 1). Most of the skill-building focus occurred during the 2nd and 3rd calls since much of the first call was spent orienting the caregiver to the TASK II Resource Guide. The use of the skill-building tip sheets during the calls tapered off in the later calls, probably because caregivers had already been exposed to most of these tip sheets and only needed brief reviews. Of the total 728 skill-building tip sheets used by the 123 caregivers over the 9 calls, 147 (20.2%) focused on strengthening existing skills, 136 (18.7%) on problem solving, 135 (18.5%) on stress management, 121 (16.6%) on screening for caregiver depressive symptoms, 113 (15.5%) on realistic schedules and expectations, and 76 (10.4%) on communication with health professionals.
Time spent on calls and reading materials
As expected, the number of minutes spent on the calls with the nurse each week declined over the 9 calls (Table 3). Importantly, however, caregivers still spent an average of 18 minutes and 19 minutes, respectively, on the 8th and 9th calls with the nurse, and they reported an average of 37 minutes reading the tip sheets in the TASK II Resource Guide prior to the 9th call. These findings indicate continued use of the TASK II program for most of the caregivers. The mean number of minutes that caregivers spent reading the TASK II Resource Guide varied over the course of the nurse calls. Most of the reading time occurred across the first 4 sessions. However, there was a large increase in reading time between the 8th and 9th calls because four weeks had transpired between these two sessions (Table 3).
Discussion
Information about stroke
The finding that information about stroke is a priority need right after hospital discharge is not surprising given the suddenness of stroke and the immediate learning needs of caregivers upon discharge [3–5, 10, 11, 20, 29]. Other studies have similarly shown caregivers expressing the need for information about stroke, including stroke risk factors, the likelihood of future strokes, which drugs are effective to prevent the recurrence of and aid the recovery from stroke, as well as the time to recuperate from stroke [24, 25, 34].
In Cobley and colleagues’ [9] qualitative study, caregivers voiced concerns about their limited understanding of the causes, prevention, and lifestyle changes of stroke. Caregivers indicated that the information had been delivered after a lengthy wait and in an inappropriate format. Similarly, O’Shea & Goode [15] found that stroke caregivers were dissatisfied with the information they had received regarding the role of caregiver. The caregivers reported they were not given enough information regarding the complications of stroke, personality changes, and the risk for stroke recurrence. In addition to needing information about stroke, caregivers desired more information about where to find and contact community resources and support [3, 5, 8, 11, 21]. Karahan and colleagues [35] emphasized that the rehabilitation team should be aware that lack of information and resources, along with inability to cope with stress, were key contributors to perceived caregiver burden. Other caregiver needs Le Dorze & Signori [21] identified were recognition of the difficulties caregivers faced in caring for their aphasic spouse, as well as lack of respite from caregiving.
One factor to consider when providing information is the timing of its delivery. King & Semik [8] found that the most difficult times for most caregivers were during hospitalization and the first few months post-discharge. This finding underscores the need for early caregiver assessment followed by individualized caregiver interventions during these critical time periods following stroke [19, 27, 28]. Results in Creasy et al.’s [16] study showed it was important to caregivers that information about stroke was presented in a timely fashion and was applicable to the person with stroke, and also that health care providers emphasized the importance of this information to the caregivers. Cameron et al.’s 2013 [18] and 2014 [36] studies using the “Timing it Right” framework illustrated how stroke caregivers’ needs for information and support change over time. For example, less information was needed during the event’s diagnosis and stabilization phases, and more was needed during the preparation and implementation phases of hospital discharge [18]. Results from these studies are consistent with our findings of more needs for information about stroke during the first two nurse calls, which rapidly tapered off during the remaining calls. This emphasizes the need to deliver information about stroke early so that caregivers can attend to other concerns.
Managing emotions and behavior
Managing survivor emotions and behaviors continues to be a priority need, consistent with other studies that have highlighted these issues as being most difficult for family caregivers [2, 3, 4, 8, 37–44]. Caregivers often ranked managing the survivor’s emotional turmoil and depressive symptoms as the most stressful problem [8, 9, 25, 26, 45–47], and they often found it difficult not to take the emotional stress of the person with stroke personally [40]. In Gonzalez and Bakas’ [43] study, male stroke survivors exhibited significantly more bothersome behaviors than females. Controlling for gender, these behaviors were significantly associated with a variety of negative caregiver outcomes related to task difficulty, threat appraisal, depressive symptoms, and life changes [43]. Although Alexander and Wilz [48] found that caregiving wives generally reported more anxiety and depressive symptoms than caregiving husbands, this trend was reversed at 15 months after stroke onset when husband caregivers whose wives exhibited cognitive and mental impairments experienced more anxiety and depressive symptoms. These findings underscore the importance of individualizing interventions based on perceived needs of the caregiver, since gender, as well as other demographics, may play a role.
Another behavior caregivers found difficult was managing communication with the person with stroke [3, 4, 21, 49]. A caregiver in Grawburg and colleagues’ [49] study described it as “…the constant pressure of communication, being that communication facilitator of a person with aphasia.” Findings from Grawburg and colleagues’ [49] study showed that the stroke survivors’ aphasia affected the health, “third- party functioning and disability” of family caregivers.
Additional survivor behaviors caregivers found difficult were keeping the survivor socially active and balancing the survivor’s needs for independence vs. dependence [3, 8, 25, 26, 38]. Although few studies have addressed survivor emotions in particular, it is imperative that caregivers receive much-needed support in their role of managing these difficult emotions and behaviors [13, 20]
Physical and instrumental care needs
Physical and instrumental care requirements were as high a priority in this study as in others, possibly due to existing training and support prior to discharge in our research sites. It is also possible that caregivers had mastered these issues over time and that relatively more training was needed regarding the emotions and behaviors of the survivor. Similarly, Haley and colleagues’ [45] findings showed caregiver concerns about managing survivor emotions of sadness and anxiety, and the survivors’ repeated questioning of events and cognitive impairment, were reported more frequently than concerns regarding the provision of physical care. In another study of 116 stroke caregivers, after providing emotional support and managing behaviors, the most difficult instrumental care tasks were taking care of household tasks and managing finances, with approximately 17 to 18% finding these activities very or extremely difficult [4]. Providing transportation (14.2%), finding respite care while away (15.3%), and finding resources (9.1%) were also rated as very or extremely difficult [37] by some.
Caregiver’s personal needs
Our findings showed caregivers often delayed focusing on their own health and emotional needs until the 5th session. In fact, we had noted this in our TASK pilot, and strengthened the intervention further by adding the BCOS at the 5th session to encourage caregivers to identify and address more of their personal needs as a result of providing care. Family caregivers of persons with stroke have reported finding ways of dealing with their emotional responses of feeling undervalued, lacking freedom, and role relationship changes [24] in addition to managing the survivors’ emotions and behaviors [9, 18, 25, 45]. In addition, the patient’s aphasia has also been reported to impact the caregivers’ self-care, domestic, social, community, and major life areas [49]. Other consequences of caregiving are the impact on the caregivers’ social functioning, emotional well-being, physical health, autonomy, and independence [3, 4, 8–10, 37, 38, 50], with female caregivers tending to have more depressive symptoms and anxiety [48; 51]. Though caregivers speak highly of the positive aspects of rehabilitation, many have continued concerns about the daily tasks and routines that jeopardize their own lifestyles [12]. Caregivers often share their concerns about their family member before they express their own concerns [10, 20]. Caregivers experiencing many unmet needs may be at risk for physical and mental health problems, which can negatively impact the survivor’s care and recovery [22, 52]. Identifying at-risk caregivers in time to effectively intervene not only promotes positive caregiver outcomes, but may also decrease societal costs related to premature institutionalization of the person with stroke [27, 53, 54].
Another consideration is the lack of knowledge regarding long-term personal needs of the caregiver [17, 48]. Although these needs tapered off toward the 8th and 9th sessions in this study, these results should be interpreted with caution since one study highlighted improvements in depressive symptoms up to six months after a multi-component intervention [48]. Another study reported that, though female caregivers had more anxiety and depressive symptoms early on, male caregivers later demonstrated more anxiety and depressive symptoms when caring for a wife with cognitive and mental impairments [48]. Though one could assume that the tapering of personal needs during the 8th and 9th sessions in this study was because caregiver needs were satisfied, ongoing interventions may be needed over the long term for continued emotional support and communication about issues such as grief, guilt, and anxiety [17, 48].
Limitations
This study has a number of limitations with implications for future research. First, data were obtained only in the Mid-west. Furthermore, subgroup analyses to explore patterns of needs based on gender, different age groups, and types of relationship would have provided more information about patterns of needs among these important subgroups [48; 51]. Another limitation is the lack of long-term follow-up data about patterns of needs that extend 6 months or more beyond the intervention process. Several studies, including this one, have highlighted unmet stroke caregiver needs during the early discharge period [3, 8, 9, 11, 15, 18, 23–26], but little is known about ongoing and long-term needs in this population [17, 18, 48]. Despite these limitations, this study has provided detailed information about the emerging patterns of needs over the course of an intervention. In the context of our intervention, specifically, the 5th session was the point when caregivers seemed ready to address their personal needs.
Implications and Conclusion
Family caregivers of persons with stroke play an essential role in the rehabilitation process of the stroke survivor. Identifying and addressing the priority needs and concerns of these caregivers during the early discharge period enable them to provide sustained support for the survivors. Information about stroke and how to manage emotions and behaviors of the survivor are priority areas for caregiver interventions during early stroke rehabilitation. A need for help with physical and instrumental care continues over time. The TASK II program identified the 5th call as a point at which many caregivers seemed ready to begin focusing on their own emotional and physical health needs. Caregiver readiness for particular types of information is an important factor to consider in the timing of interventions. Skill-building information and discussion were important in individualizing interventions and providing additional strategies to sustain caregivers in addressing their needs and concerns. Tracking patterns of needs and interest in skill-building can reveal important areas for improvement of existing stroke caregiver intervention programs, as well as for addressing individual caregiver concerns that evolve over time. Addressing these evolving needs as caregivers and survivors transition to home settings is an area to consider in improving stroke rehabilitation services. Miller and colleagues’ [2] rehabilitation guidelines recommended detailed assessment of self-reported caregiver needs in inpatient and outpatient settings with follow-up contacts and referrals. Additional recommendations include providing caregivers with information about stroke (warning signs, risk factors, post-stroke complications, medication management, lifestyle changes, and related care), skill-building strategies such as problem solving and counseling to help manage emotions and behaviors, and techniques to help communicate with the person with stroke. They also recommended that family caregivers be included as integral members of interdisciplinary teams and be involved in the decision-making process for the patient’s care.
Further recommendations included encouraging health professionals to attend to the caregivers’ emotional and physical health and motivating caregivers to seek regular health checkups [2, 20]. Incorporating these stroke rehabilitation recommendations into caregiver interventions may help improve caregiver outcomes, which may ultimately contribute to sustained patient care and expedite recovery [11, 35]. Rehabilitation professionals are in a key position to identify and address priority needs and concerns of family caregivers of persons with stroke as they evolve over time during stroke recovery and rehabilitation.
Acknowledgments
The authors would like to acknowledge the assistance of Phyllis Dexter, PhD, RN, Indiana University School of Nursing, for her helpful review of this manuscript.
Funding for this study was provided by the National Institutes of Health, National Institute of Nursing Research, R01NR010388 (Tamilyn Bakas, PI) and K01NR008712 (Tamilyn Bakas, PI).
Footnotes
Declaration of Interest
The authors report no other conflicts of interest.
References
- 1.Go AS, Mozaffarian D, Roger VI, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, III, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turna TN, Virani SS, Wong ND, Woo D, Turner MB on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–3292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller EL, Murray L, Lorie R, Zorowitz RD, Bakas T, Clark P, Billinger SA. Comprehensive overview of nursing and interdisciplinary rehabilitation care of the stroke patient: a scientific statement from the American Heart Association. Stroke. 2010;41:2402–2448. doi: 10.1161/STR.0b013e3181e7512b. [DOI] [PubMed] [Google Scholar]
- 3.Bakas T, Austin JK, Okonkwo KF, Lewis R, Chadwick L. Needs, concerns, strategies, and advice of stroke caregivers the first six months after discharge. Journal of Neuroscience Nursing. 2002;34:242–251. doi: 10.1097/01376517-200210000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Bakas T, Kroenke K, Plue LD, Perkins SM, Williams LS. Outcomes among family caregivers of aphasic versus non-aphasic stroke survivors. Rehabilitation Nursing. 2002;31:33–42. doi: 10.1002/j.2048-7940.2006.tb00008.x. [DOI] [PubMed] [Google Scholar]
- 5.King RB, Hartke RJ, Lee J, Raad J. The stroke caregiver unmet resource needs scale: development and psychometric testing. Journal of Neuroscience Nursing. 2013;45(6):320–328. doi: 10.1097/JNN.0b013e3182a3ce40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Low JTS, Payne S, Roderick P. The impact of stroke on informal caregivers: A literature review. Social Science & Medicine. 1999;49:711–725. doi: 10.1016/s0277-9536(99)00194-x. [DOI] [PubMed] [Google Scholar]
- 7.Anderson CS, Linto J, Stewart-Wynne EG. A population-based assessment of the impact and burden of caregiving for long-term stroke survivors. Stroke. 1995;26:843–849. doi: 10.1161/01.str.26.5.843. [DOI] [PubMed] [Google Scholar]
- 8.King RB, Semik PE. Stroke caregiving: difficult times, resource use and needs during the first 2 years. Journal of Gerontological Nursing. 2006;32(4):37–44. doi: 10.3928/00989134-20060401-07. [DOI] [PubMed] [Google Scholar]
- 9.Cobley CS, Fisher RJ, Chouliara N, Kerr M, Walker MF. A qualitative study exploring patients' and carers' experiences of early supported discharge services after stroke. Clinical Rehabilitation. 2013;27:750–757. doi: 10.1177/0269215512474030. [DOI] [PubMed] [Google Scholar]
- 10.Quinn K, Murray C, Malone C. Spousal experiences of coping with and adapting to caregiving for a partner who has a stroke: a meta-synthesis of qualitative research. Disability & Rehabilitation. 2014;36(3):185–198. doi: 10.3109/09638288.2013.783630. [DOI] [PubMed] [Google Scholar]
- 11.Perry L, Middleton S. An investigation of family carers’ needs following stroke survivors’ discharge from acute hospital in Australia. Disability & Rehabilitation. 2011;33(19–20):1890–1900. doi: 10.3109/09638288.2011.553702. [DOI] [PubMed] [Google Scholar]
- 12.Gustafsson L, Bootle K. Client and carer experience of transition home from inpatient stroke rehabilitation. Disability & Rehabilitation. 2013;35(16):1380–1386. doi: 10.3109/09638288.2012.740134. [DOI] [PubMed] [Google Scholar]
- 13.Jones AL, Charlesworth JF, Hendra TJ. Patient mood and carer strain during stroke rehabilitation in the community following early hospital discharge. Disability & Rehabilitation. 2000;22(11):490–494. doi: 10.1080/096382800413970. [DOI] [PubMed] [Google Scholar]
- 14.Ski C, O’Connell B. Stroke: The increasing complexity of carer needs. Journal of Neuroscience Nursing. 2007;39(3):172–179. [PubMed] [Google Scholar]
- 15.O'Shea R, Goode D. Effects of stroke on informal carers. Nursing Standard. 2013;28(15):43–7. doi: 10.7748/ns2013.12.28.15.43.e8095. [DOI] [PubMed] [Google Scholar]
- 16.Creasy KR, Lutz BJ, Young ME, Ford A, Martz C. The impact of interactions with providers on stroke caregivers’ needs. Rehabilitation Nursing. 2013;38(2):88–98. doi: 10.1002/rnj.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilz G, Barskova T. Evaluation of a cognitive behavioral group intervention program fro spouses of stroke patients. Behaviour Research and Therapy. 2007;45:2508–2517. doi: 10.1016/j.brat.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 18.Cameron JI, Naglie G, Silver FL, Gignac MAM. Stroke family caregivers’ support needs change across the care continuum: a qualitative study using the timing it right framework. Disability & Rehabilitation. 2013;34(4):315–324. doi: 10.3109/09638288.2012.691937. [DOI] [PubMed] [Google Scholar]
- 19.Young ME, Lutz BJ, Creasy KR, Cox KJ, Martz C. A comprehensive assessment of family caregivers of stroke survivors during inpatient rehabilitation. Disability & Rehabilitation. 2014;36(22):1892–1902. doi: 10.3109/09638288.2014.881565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bakas T, Scarton L. Chapter 46: Stroke and the Family. In: Stein J, Harvey RL, Winstein CJ, Zorowitz RD, Wittenberg GE, editors. Stroke Recovery and Rehabilitation. 2nd. New York: Demos Medical Publishing; 2015. [Google Scholar]
- 21.Le Dorze G, Signori FH. Needs, barriers and facilitators experienced by spouses of people with aphasia. Disability & Rehabilitation. 2010;32(13):1073–1087. doi: 10.3109/09638280903374121. [DOI] [PubMed] [Google Scholar]
- 22.Barskova T, Wilz G. Interdependence of stroke survivors’ recovery and their relatives’ attitudes and health: A contribution to investigating the causal effects. Disability and Rehabilitation. 2007;29(19):1481–1491. doi: 10.1080/09638280601029399. [DOI] [PubMed] [Google Scholar]
- 23.El Masry Y, Mullan B, Hackett M. Psychosocial experiences and needs of Australian caregivers of people with stroke: prognosis messages, caregiver resilience, and relationships. Topics in Stroke Rehabilitation. 2013;20(4):356–368. doi: 10.1310/tsr2004-356. [DOI] [PubMed] [Google Scholar]
- 24.Greenwood N, Mackenzie A, Cloud GC, Wilson N. Informal primary carers of stroke survivors living at home - challenges, satisfactions and coping: a systematic review of qualitative studies. Disability & Rehabilitation. 2009;3(5):337–351. doi: 10.1080/09638280802051721. [DOI] [PubMed] [Google Scholar]
- 25.Hayashi Y, Hai HH, Tai NA. Assessment of the needs of caregivers of stroke patients at state-owned acute-care hospitals in southern Vietnam, 2011. Preventing Chronic Disease. 2013;10:E139.130023. doi: 10.5888/pcd10.130023. doi: http://dx.doi.org/10.5888/pcd10.130023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones L, Morris R. Experiences of adult stroke survivors and their parent carers: a qualitative study. Clinical Rehabilitation. 2013;27(3):272–280. doi: 10.1177/0269215512455532. [DOI] [PubMed] [Google Scholar]
- 27.Bakas T, Clark PC, Kelly-Hayes M, King RB, Lutz BJ, Miller E. on behalf of the American Heart Association Council on Cardiovascular and Stroke Nursing and the Stroke Council. Evidence for stroke family caregiver and dyad interventions: A statement for healthcare professionals from the American Heart Association. Stroke. 2014;45(9):2836–2852. doi: 10.1161/STR.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 28.Brereton L. Interventions for adult family carers of people who have had a stroke: a systematic review. Clinical Rehabilitation. 2007;21:867–884. doi: 10.1177/0269215507078313. [DOI] [PubMed] [Google Scholar]
- 29.Bakas T, Farran CJ, Austin JK, Given BA, Johnson EA. Content validity and satisfaction with a stroke caregiver intervention program. Journal of Nursing Scholarship. 2009;41(4):368–375. doi: 10.1111/j.1547-5069.2009.01282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bakas T, Farran CJ, Austin JK, Given BA, Johnson EA, Williams LS. Stroke caregiver outcomes from the Telephone Assessment and Skill-Building Kit (TASK) Topics in Stroke Rehabilitation. 2009;16(2):105–121. doi: 10.1310/tsr1602-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williams LS, Bakas T, Brizendine E, Plue L, Tu W, Hendrie H, Kroenke K. How valid are family proxy assessments of stroke patients’ health-related quality of life? Stroke. 2006;37:2081–2085. doi: 10.1161/01.STR.0000230583.10311.9f. [DOI] [PubMed] [Google Scholar]
- 32.Bakas T, Champion V. Development and psychometric testing of the Bakas Caregiving Outcomes Scale. Nursing Research. 1999;48(5):250–259. doi: 10.1097/00006199-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Bakas T, Champion V, Perkins SM, Farran CJ, Williams LS. Psychometric testing of the Revised 15-item Bakas Caregiving Outcomes Scale. Nursing Research. 2006;55(5):346–355. doi: 10.1097/00006199-200609000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Mackenzie A, Perry L, Lockhart E, Cottee M, Cloud G, Mann H. Family carers of stroke survivors: needs knowledge, satisfaction and competence in caring. Disability & Rehabilitation. 2007;29(2):111–121. doi: 10.1080/09638280600731599. [DOI] [PubMed] [Google Scholar]
- 35.Karahan AY, Kucuksen S, Yilmaz H, Salli A, Gungor T, Sahin M. Effects of rehabilitation services on anxiety, depression, care-giving burden and perceived social support of stroke caregivers. Acta Medica. 2014;57(2):68–72. doi: 10.14712/18059694.2014.42. http://dx.doi.org/10.14712/18059694.2014.42. [DOI] [PubMed] [Google Scholar]
- 36.Cameron JI, Naglie G, Gignac MAM, Bayley M, Warner G, Green T, Czerwonka A, Huijbregts M, Silver FL, Philipps SJ, Cheung AM. Randomized clinical trial of the timing it right stroke family support program: research protocol. Biomed Central Health Services Research. 2014;14(18):1–9. doi: 10.1186/1472-6963-14-18. http://www.biomedcentral.com/1472-6963/14/18 Trial registration: ClinicalTrials.gov: NCT00958607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bakas T, Austin JK, Jessup SL, Williams LS, Oberst MT. Time and difficulty of tasks provided by family caregivers of stroke survivors. Journal of Neuroscience Nursing. 2004;36(2):95–106. doi: 10.1097/01376517-200404000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Greenwood N, Mackenzie A, Cloud G, Wilson N. Loss of autonomy, control and independence when caring: A qualitative study of informal carers of stroke survivors in the first three months after discharge. Disability & Rehabilitation. 2010;32(2):125–133. doi: 10.3109/09638280903050069. [DOI] [PubMed] [Google Scholar]
- 39.Cameron JI, Cheung AM, Streiner DL, Coyte PC, Stewart DE. Stroke survivors’ behavioral and psychological symptoms are associated with informal caregivers’ experiences of depression. Archives of Physical Medicine and Rehabilitation. 2006;87(2):177–183. doi: 10.1016/j.apmr.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 40.Clark PC, Dunbar SB, Shields CG, Viswanathan B, Aycock DM, Wolf SL. Influence of stroke survivor characteristics and family conflict surrounding recovery on caregivers’ mental and physical health. Nursing Research. 2004;53(6):406–413. doi: 10.1097/00006199-200411000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Davis LL, Grant JS. Constructing the reality of recovery: Family home care management strategies. Advances in Nursing Science. 1994;17(2):66–76. doi: 10.1097/00012272-199412000-00009. [DOI] [PubMed] [Google Scholar]
- 42.Stewart MJ, Doble S, Hart G, Langille L, MacPherson K. Peer visitor support for family caregivers of seniors with stroke. Canadian Journal of Nursing Research. 1998;30(2):87–17. [PubMed] [Google Scholar]
- 43.Gonzalez C, Bakas T. Factors associated with stroke survivor behaviors as identified by family caregivers. Rehabilitation Nursing. 2013;38(4):202–11. doi: 10.1002/rnj.85. Epub 2013 May 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bulley C, Shiels J, Wilkie K, Salisbury L. Carer experiences of life after stroke - a qualitative analysis. Disability & Rehabilitation. 2010;32(17):1406–1413. doi: 10.3109/09638280903531238. [DOI] [PubMed] [Google Scholar]
- 45.Haley WE, Allen JY, Grant JS, Clay OJ, Perkins M, Roth DL. Problems and benefits reported by stroke family caregivers: Results from a prospective epidemiological study. Stroke. 2009;40(6):2129–2133. doi: 10.1161/STROKEAHA.108.545269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lurbe-Puerto K, Leandro ME, Baumann M. Experiences of caregiving, satisfaction of life, and social repercussions among family caregivers, two years post-stroke. Social Work in Health Care. 2012;51:725–742. doi: 10.1080/00981389.2012.692351. [DOI] [PubMed] [Google Scholar]
- 47.Cameron JI, Cheung AM, Streiner DL, Coyte PC, Stewart Stroke survivor depressive symptoms are associated with family caregiver depression during the first 2 years poststroke. Stroke. 2011;42:302–306. doi: 10.1161/STROKEAHA.110.597963. [DOI] [PubMed] [Google Scholar]
- 48.Alexander T, Wilz G. Gender differences in adjustment to stroke survivors’ mental changes. Rehabilitation Psychology. 2010;55(2):159–169. doi: 10.1037/a0019253. [DOI] [PubMed] [Google Scholar]
- 49.Grawburg M, Howe T, Worrall L, Scarinci N. Describing the impact of aphasia on close family members using the ICF framework. Disability & Rehabilitation. 2014;36(14):1184–1195. doi: 10.3109/09638288.2013.834984. [DOI] [PubMed] [Google Scholar]
- 50.Klinedinst NJ, Gebhardt MC, Aycock DM, Nichols-Larsen DS, Uswatte G, Wolf SL, Clark PC. Caregiver characteristics predict stroke survivor quality of life at 4 months and 1 year. Research in Nursing & Health. 2009;32:592–605. doi: 10.1002/nur.20348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jessup NM, Bakas T, Mclennon SM, Weaver MT. Are there gender, racial or relationship differences in caregiver task difficulty, depressive symptoms and life changes among stroke family caregivers? Brain Injury. 2015;29(1):17–24. doi: 10.3109/02699052.2014.947631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McLennon SM, Bakas T, Jessup NM, Habermann B, Weaver MT. Task difficulty and life changes among stroke family caregivers: Relationship to depressive symptoms. Archives of Physical Medicine and Rehabilitation. 2014;95(12):2484–2490. doi: 10.1016/j.apmr.2014.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Family Caregiver Alliance. Report from a National Consensus Development Conference. I. San Francisco: Author; 2006. Caregiver Assessment: Principles, Guidelines, and Strategies for Change. [Google Scholar]
- 54.Lindsay P, Bayley M, Hellings C, Hill M, Woodbury E, Phillips S. on behalf of the Canadian Stroke Strategy, a joint initiative of the Canadian Stroke Network and the Heart and Stroke Foundation of Canada. Canadian Best Practice Recommendations for Stroke Care: Summary. Canadian Medical Association Journal. 2008;179:S1–S25. doi: 10.1503/cmaj.081536. [DOI] [PMC free article] [PubMed] [Google Scholar]