Abstract
Policies to “rebalance” funding away from nursing homes and toward home and community-based services (HCBS) have encouraged national trends of nursing home closure and an expansion of the HCBS industry. These changes are unfolding without a clear understanding of what services are available at the local level. The purpose of this study was: (1) to describe the current distribution of community-based services (CBS) in areas where nursing homes have closed and (2) to examine differences in availability of CBS using local market and population characteristics as regressors in a multinomial logistic model. We collected data on and geocoded CBS facilities and then used ArcGIS to define a 5-mile radius around all nursing homes that closed between 2006 and 2010 and compared these local market areas. In rural areas, availability of CBS does not appear to compensate for nursing home closures. Policies encouraging HCBS may be outpacing availability of CBS, especially in rural areas.
Keywords: community-based services, long-term care, nursing homes, rural access
Introduction
Local long-term care market structures throughout the United States are undergoing profound transformation. Federal policies to “rebalance” funding away from nursing homes and toward support of home and community-based services (HCBS) have encouraged national trends of nursing home closure and the expansion of the HCBS industry. However, these changes are unfolding without a clear understanding of what services are available at the local level as nursing homes have closed. The purpose of this study was twofold: (1) to describe the current distribution of community-based providers, focusing on assisted living facilities (ALFs) and adult day services centers (ADSCs; i.e., community-based rather than home-based providers), in areas where nursing homes have closed and (2) to examine differences in availability of these community-based providers using local market characteristics, population characteristics, and state policy differences as regressors in a multinomial logistic model.
Literature Review
Consumer preference for receiving care in one’s home or community and budget concerns at both the state and federal levels have resulted in efforts to rebalance funding for long-term care away from nursing homes and toward HCBS (Konetzka, 2014). The term “rebalancing” is used to describe changes in state and federal policies aimed at rectifying Medicaid policy that favored the provision of long-term care in institutional settings. For example, the Omnibus Reconciliation Act of 1981 encouraged use of HCBS through section 1915(c) of the Social Security Act. 1915(c) waivers allow states to waive certain Medicaid requirements, so that community-based alternatives to institutional care can be provided (Leblanc, Tonner, & Harrington, 2000). Through the use of these waivers, and other policy changes, HCBS was intended to replace most institutional long-term care (Grabowski et al., 2010) and has indeed contributed to a spate of nursing home closures over the past two decades. Castle, Engberg, Lave, and Fisher (2009) warn that as states work to rebalance long-term care, they should be conscious of the effect their policy decisions have on nursing homes (and indirectly, on families seeking appropriate care for their elderly family members), and how these decisions may accelerate the closure of other nursing homes.
Feng and colleagues examined nursing home closures between 1999 and 2008 and found that 11% of stand-alone nursing homes (N = 1776) and almost half of all hospital-based nursing homes (N = 1126) closed during that decade (Feng et al., 2011). This represented a loss of 16% of all Medicare/Medicaid-certified nursing homes and a total cumulative 10% decrease in existing nursing home beds. Their analyses also found that nursing home closures do not occur randomly across locations. Rather, closure rates were nearly twice as high in zip codes that are disproportionately low income and have populations with greater proportions of either Blacks or Hispanics. The cumulative loss of nursing homes and a lack of attention to the availability of community-based providers in areas where nursing homes have closed (arguably the areas with the greatest need) suggest that these types of disparities in availability could increase (Katz, 2011).
HCBS takes various forms which, as the term implies, are available in one’s home or community. Community-based services (CBS) include ALFs and ADSCs. ALFs are residential settings providing housing, meals, and some personal and supportive care 24 hours a day. ADSCs are nonresidential and provide meals, programs of activities, and general supervision for several hours each day. Although ALFs generally meet less skilled needs than nursing homes, they are able to provide levels of supportive care that are comparable to that of nursing homes (Golant, 2004). ADSCs also provide comprehensive, skilled health care in a community-based group setting. ADSCs are increasingly serving as an appropriate setting for chronic disease management, and as a result are viewed as an alternative to nursing home care (Metlife, 2010).
Due primarily to a lack of available data, few studies have examined the availability of these CBS. Stevenson and Grabowski (2010) examined the availability of ALFs and found that while there were over 11,000 facilities in the United States in 2007, availability of these varied widely by state and facilities were more likely to be located in wealthier counties. With regard to ADSCs, the MetLife study of adult day services found 4,600 ADSCs in 2010, which was a 35% increase over the number of ADSCs operating in 2002. This industry now serves over 260,000 participants (Anderson, Dabelko-Schoeny, & Johnson, 2013).
Despite the growth in HCBS, there is still concern about the availability of these types of CBS. In a survey of long-term care experts, about a third of respondents reported that the supply of providers is among the top three challenges facing long-term care (Grabowski et al., 2010). Previous research has also shown that access to services by long-term care consumers varies widely by state and that access to these services is restricted by state policies (Ng, Stone, & Harrington, 2015).
This study is the first, to our knowledge, to examine the availability of CBS in areas where nursing homes have closed. We do this by (1) describing the current distribution of community-based providers in areas where nursing homes have closed, and (2) by examining differences in availability of these community-based providers in a model including local market characteristics, population characteristics, and state policies.
We did not include home-based services, such as home health care and personal assistant services, in this study for a number of reasons. Home-based service providers are not as amenable to geocoding as are CBS. The location of a home care or home health agency (based on mailing address) does not provide enough information about the market where services are provided. In most cases, staff travel to clients’ homes from their own homes, not from the agency office. Therefore, the market served by a home care or health agency is defined differently than the market served by a nursing home, ALF or ADSC, and the size of the market served also likely varies by agency depending on the number of staff employed and the home addresses of those staff. Given these differences between community-based and home-based services (CBS require a location and full organizational base to provide services to clients; markets are defined differently), it makes better sense to examine CBS and home-based services separately. For these reasons, our study focused on the availability of community-based providers in areas where nursing homes have closed.
Research Design
In order to describe the availability of CBS, ALFs and ADSCs, in areas where nursing homes had closed, we gathered data for these services in the 48 contiguous states and merged these data with our existing nursing home closure data. Because there are no standardized data available on CBS, we built a database using Internet searches and by calling state departments of health to gather lists of existing ALFs and ADSCs in 2008/2009 and 2010, respectively. Data collection included information on service capacity (bed or slot size), founding date, licensure information, and complete addresses. Although we gathered data on all ALFs, we limited our analysis to ALFs with 25 or more beds as has been done in previous research (Stevenson & Grabowski, 2010). We then used addresses to geocode these providers using ArcGIS (ESRI, 2011). We then merged these data with an existing data file of all nursing homes in the United States that had been created for another project (Feng et al., 2011). This file included all existing and closed nursing homes in the United States through 2008; we updated this file using our geo-coded CBS file and with the addition of data on all nursing homes that had opened or closed in 2009 and 2010, as identified in the Online Survey Certification and Reporting (OSCAR) data available for nearly all U.S. nursing homes, both freestanding and hospital based. We chose to include both types of nursing home closures and additions because recent research has shown that freestanding and hospital-based facilities are providing more similar care than in the past; patient acuity and therapy provision have increased in free-standing facilities, while these services have decreased in hospital-based facilities (Tyler et al., 2013). Finally, we used ArcGIS to create 5-mile radii around each U.S. nursing home that had closed between 2006 and 2010. These radii are how we defined the local market area around closed nursing homes.
The literature focusing on health care catchment areas is extremely limited, with significant gaps in accounts of the methodologies used to develop health care catchment definitions (Schuurman, Fiedler, Grzybowski, & Grund, 2006). Previous research has used zip codes, counties, and specified mileages or travel times to define health care markets (Basu & Cooper, 2000; Gresenz, Rogowski, & Escarce, 2004; Grzybowski, Stoll, & Kornelsen, 2011; Hall, Kaufman, & Ricketts, 2006; Lowe et al., 2009; Rudavsky & Mehrotra, 2010; Schuurman et al., 2006; Virnig, Ma, Hartman, Moscovice, & Carlin, 2006). We chose a market radius of 5 miles for both rural and urban areas because unlike using zip codes or counties with substantial variation in size of the catchment area, a 5-mile radius allows for true market comparison. We utilized the same 5-mile radius in urban and rural areas because we could find no previous research where different sized markets were used in urban versus rural areas.
Next, we used a multinomial logistic regression model to examine differences in availability of community-based providers. We ran separate models examining availability of ALFs in local market areas where nursing homes had closed, availability of ADSCs in these areas, and availability of both. The reference category for these models was local market areas with neither ALFs nor ADSCs. We included in these models local market characteristics, including urban location, the year the nursing home in the area closed, the number of nursing home closures in the area, and the number of operating nursing homes in the area as well as whether the closed nursing home was hospital based. Urban location, year of closure, and whether the closed nursing home was hospital-based were obtained from the OSCAR file. The number of closed and open nursing homes in the area was determined using our ArcGIS data file.
We also included population characteristics for the local market area by merging zip code level census data into our data set. For each local market area, population data for the zip code of the closed nursing home were used. In some cases, small portions of other zip code areas were included in the 5-mile radius around the closed nursing home. However, for consistency and because this was accurate for most local market areas, we used only the population data for the one primary zip code. This included data on the proportion of the population that was non-White, the proportion living below poverty, and the proportion age 65 or older. We included data on those over age 65 because 85% of people in nursing homes are aged 65 or older (Centers for Medicare and Medicaid Services, 2013). Finally, we controlled for state policy differences, specifically the proportion of state Medicaid funds spent on HCBS in 2010. These data were available from ltcfocus.org, a product of the Shaping Long Term Care in America project at Brown University.
Results
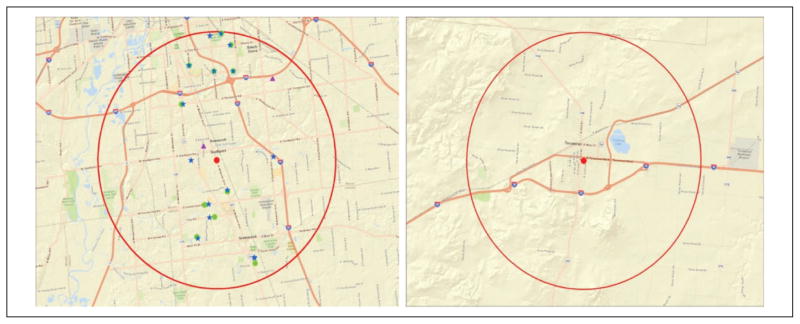
Our data collection efforts identified over 11,000 ALFs with 25 or more beds in 2008/2009 and approximately 4,000 ADSCs in 2010. Our examination of the local market areas around closed nursing homes revealed that about one quarter of these areas had no ALFs and over 50% had no ADSCs. There was also a strong association between urban/rural location and the availability of CBS in areas where nursing homes had closed. We found that about 80% of rural local market areas around closed nursing homes had no ADSCs, over 50% of rural local market areas had no ALFs, and 30% of rural local market areas around closed nursing homes had no ADSCs, ALFs, or other operating nursing homes. As an illustration, Figure 1 shows the CBS available in one urban local market area compared to the lack of services available in one rural local market area.
Figure 1.
Community-based services available in urban versus rural local market areas.
Note. Dot in the center of the circle represents the closed nursing home, the circle represents the local market area (i.e. the 5 mile radius around the closed nursing home), other dots in the circle are open nursing homes, stars are ALFs and triangles are ADSCs.
Table 1 includes descriptive statistics for the closed nursing homes and local market areas included in our analyses. Between 2006 and 2010, 714 nursing homes in the United States closed. Just over 40% of these were hospital-based facilities. Approximately two thirds of these closures occurred in urban areas and one third in rural areas.
Table 1.
Descriptive Statistics for Closed Nursing Homes & Local Area Markets.
| Variables | N or Mean | Data source |
|---|---|---|
| Total nursing home closures 2006–2010 | 714 | OSCAR |
| Closures in 2006 | 176 | OSCAR |
| Closures in 2007 | 168 | OSCAR |
| Closures in 2008 | 149 | OSCAR |
| Closures in 2009 | 117 | OSCAR |
| Closures in 2010 | 104 | OSCAR |
| Hospital-based closures | 308 | OSCAR |
| Urban location | 467 | OSCAR |
| % Non-White | 28.3 | Zip-code level census |
| % Below poverty | 14.3 | Zip-code level census |
| % Over age 65 | 14.6 | Zip-code level census |
| % Medicaid dollars on HCBS | 33.9 | Zip-code level census |
| Number of other NH closures | 0.5 | Derived by authors |
| Number of operating NHs | 6.5 | Derived by authors |
Note. OSCAR = online survey certification and reporting; HCBS = home and community-based services; NH = nursing home.
Table 2 includes the results from our multinomial logistic regression models. We ran separate models for local market areas with just ADSCs, those with just ALFs, and those with both of these services. Local market areas around closed nursing homes with none of these services were the reference group. Focusing on the availability of both ADSCs and ALFs in local market areas where nursing homes have closed, urban location has a very strong significant association with the availability of these CBS. The existence of other nursing homes operating in the local market area was also significantly related to greater log odds of an area having both of these CBS. The proportion of the population, that is non-White, has a very small positive association with the availability of both ADSCs and ALFs in an area, and the proportion of the population in poverty has a small negative association with the availability of these services.
Table 2.
Association Between Market and Population, Characteristics and Availability of ADSC, ALF, or Both in Market Around Closed NH.
| Variables | Has only ADSC
|
Has only ALF
|
Has both
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| 95% confidence interval for B
|
95% confidence interval for B
|
95% confidence interval for B
|
|||||||
| B | Lower bound | Upper bound | B | Lower bound | Upper bound | B | Lower bound | Upper bound | |
| Intercept | −1.997 | −4.634 | 0.640 | −0.660 | −2.211 | 0.890 | −0.886 | −2.587 | 0.814 |
| Closed in 2007 | −0.114 | −1.284 | 1.057 | −0.001 | −0.793 | 0.790 | 0.229 | −0.619 | 1.078 |
| Closed in 2008 | −0.505 | −1.776 | 0.766 | 0.078 | −0.683 | 0.838 | −0.130 | −0.974 | 0.715 |
| Closed in 2009 | −0.691 | −1.998 | 0.616 | −0.304 | −1.119 | 0.511 | −0.307 | −1.205 | 0.591 |
| Closed in 2010 | −1.412 | −3.103 | 0.279 | −0.190 | −1.024 | 0.644 | −0.248 | −1.167 | 0.671 |
| Hospital-based closure | 1.423** | 0.530 | 2.315 | 1.088*** | 0.534 | 1.642 | 1.281*** | 0.675 | 1.887 |
| Number of other closures | −0.084 | −0.992 | 0.824 | 0.311 | −0.393 | 1.015 | 0.177 | −0.535 | 0.888 |
| Number of operating NHs | 0.705*** | 0.491 | 0.920 | 0.750*** | 0.553 | 0.946 | 0.819*** | 0.622 | 1.016 |
| Urban location | −0.294 | −1.354 | 0.766 | 0.510 | −0.109 | 1.129 | 1.141** | 0.430 | 1.852 |
| % Non-White | 0.043** | 0.016 | 0.070 | 0.013 | −0.007 | 0.032 | 0.032** | 0.011 | 0.053 |
| % Below poverty | −0.108** | −0.190 | −0.026 | −0.072* | −0.128 | −0.016 | −0.145*** | −0.205 | −0.085 |
| % Over age 65 | −0.084 | −0.201 | 0.033 | −0.027 | −0.093 | 0.039 | −0.067 | −0.139 | 0.005 |
| % Medicaid on HCBS | 0.018 | −0.016 | 0.051 | −0.001 | −0.022 | 0.019 | 0.003 | −0.019 | 0.026 |
| n | 30 | 250 | 254 | ||||||
Note. Reference category = local market areas with no community-based services (N = 171). NH = nursing home; ALF = assisted living facility; ADSC = adult day services center; HCBS = home and community-based services.
p ≤ .05.
p ≤ .01.
p ≤ .001.
The results related to our other two models examining the availability of only ADSCs or only ALFs were fairly consistent. The number of operating nursing homes remains strongly positively associated with the availability of only an ADSC or only an ALF. However, urban location is not significantly associated with the availability of only an ADSC or only an ALF. In fact, urban location is negatively associated with the availability of only ADSCs or ALFs. This suggests that urban local market areas are more likely to have more services.
Poverty rates have a small negative association with the availability of only ADSCs and only ALFs in local market areas. The proportion of the population, that is non-White, was not consistently significantly associated with availability of ALFs or ADSCs. Nor was the proportion of the population aged 65 or older. Finally, the proportion of state Medicaid funds spent on HCBS was not consistently associated with the availability of CBS in local market areas where nursing homes had closed.
As a sensitivity test, we repeated our analyses using 10-mile radii to define the local market area around closed nursing homes. Results were very similar.
Discussion
The Affordable Care Act (ACA) includes initiatives designed to improve access to and delivery of long-term services and supports. Among these, initiative is the Balancing Incentive Program, which provides states with financial incentives to improve access to community-based long-term care as an alternative to institutional care. Through this program, the ACA makes up to US$3 billion available in federal matching funds. Many states have taken advantage of these federal funds. The ACA also brought about expansion of the 1915 (i) HCBS state plan option, which gives states the ability to provide HCBS as an optional Medicaid benefit. This change expands both financial eligibility for services and the scope of services provided. Several states have implemented the HCBS option since the ACA was enacted. A related new Medicaid option, the community first choice option, allows states to provide HCBS attendant supports and services and provides additional federal funding to support services to assist people with ADL and IADL difficulties (Kaiser Commission on Medicaid and the Uninsured, 2013).
These new programs are part of over two decades of effort to rebalance long-term care away from care in institutional settings to services provided in one’s home or community. Despite these continued efforts to rebalance long-term care, little research has examined how this has played out at the local community level. Our study is the first to examine the availability of CBS at the local community level and, specifically, to examine the availability of CBS in areas where nursing homes have closed. While much research has demonstrated, consumer preference for care in one’s home or community (Kane & Kane, 2001) and policy makers have attempted to balance state budgets by shifting funds to lower cost HCBS, there has been little focus on ensuring that CBS become available in locations where institutional services have been lost.
Our results show that market characteristics are more strongly associated with the availability of CBS in local market areas where nursing homes have closed than population characteristics. Urban location and the existence of other operating nursing homes in an area were significantly related to the availability of ALFs and ADSCs, while the proportion of the population aged 65 or older was not. Our results suggest that efforts to rebalance long-term care may only be increasing options in urban areas and that CBS may not be available in rural locations where nursing homes have closed. This, combined with previously identified obstacles to HCBS, such as the lack of availability of case management and the need for single access points (Kassner, 2008), may further hinder rebalancing efforts.
Our results also show that having greater proportions of the local population living below poverty was related to lower odds of having any type of CBS available where nursing homes had closed. This finding is consistent with those of Stevenson and Grabowski (2010) who found that ALFs were disproportionately located in areas with higher educational attainment, income, and housing wealth. Lower availability of CBS in rural areas and in poorer areas suggests that disparities in availability of these more desirable services are occurring. Policies to rebalance long-term care, including those in the ACA, may be contributing to these disparities. Others have suggested that consumer access to these services is restricted by state policies and that availability could be improved by standardizing and liberalizing state HCBS policies (Ng, Stone, & Harrington, 2015). More research is needed to examine these possible disparities in the availability of CBS and find ways to improve availability by distributing these services more uniformly across communities and states. In addition, considering the increased focus on HCBS found in some provisions of the ACA, it may be important for states to conduct strategic planning regarding where service providers are most needed. This may be especially important in rural states and in areas of concentrated poverty.
Our findings are limited by the fact that there are no standardized data available on CBS and, therefore, we had to collect these data ourselves through websites and calls to state departments of health. The validity of the lists of existing ALFs and ADSCs we obtained may have varied by state. We also chose to include only ALFs with 25 or more beds in our analyses as had been done in previous research (Stevenson & Grabowski, 2010). Part of the logic for this exclusion has been the extreme heterogeneity in service profiles among the smallest ALFs. However, our findings may have been different had we included smaller ALFs because it is possible that ALF size is related to location and that smaller ALFs may be located disproportionately in rural locations. We also did not include home-based services in our analyses primarily because the market served by these organizations is more difficult to establish using a street address. Future research should attempt to examine the availability of home-based services, such as home health and personal assistance services, in areas where nursing homes have closed. This research will need to include data collection beyond just providers’ addresses and should include data on the size of the agency’s catchment area, the number of individuals served, and the type of payment accepted, including private pay, Medicare and/or Medicaid.
Despite these limitations, our findings suggest that efforts to rebalance long-term care away from institutional settings may be resulting in disparities in availability of CBS. This seems especially true in rural areas and may also be true in areas with greater proportions of the population living in poverty. It would be unfortunate if efforts to decrease institutionalization among those needing long-term services and supports had similar results to the closure of psychiatric hospitals in decades past whereby policy decisions to close facilities without first determining whether community-based mental health service providers were in fact available. The resulting deinstitutionalization of the mentally ill was immediately accompanied by high rates of homelessness of the chronically mentally ill (Smith, 2001; Smith, Feng, Fennell, Zinn, & Mor, 2008). The closure of nursing homes may not be a bad thing when nursing homes are poorly managed and deliver low quality care, but to close off institutional sources of care in areas where home and community-based substitutes are not available seems ill-advised.
Conclusion
In rural areas, availability of CBS does not appear to compensate for nursing home closures. Greater attention needs to be paid to the availability of community-based providers in local market areas where nursing homes have closed. For example, we found that 30% of rural local market areas where nursing homes have closed, include no other nursing homes, ALFs or ADSCs. Federal and state policy changes seeking to rebalance long-term care and favoring HCBS, including several provisions of the ACA, may be outpacing availability of these services, especially in rural areas. Future research should examine possible disparities in the availability of CBS, the availability of homes-based services, and the potential role of federal and state policies in addressing any disparities identified.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research made possible in part by the Shaping Long Term Care in America project funded by the National Institute on Aging (P01AG027296).
Biographies
Denise A. Tyler, PhD, is an assistant professor (research) in the department of Health Services, Policy and Practice and the Center for Gerontology and Healthcare Research at the Brown University School of Public Health. Her research focuses on long-term care, especially nursing homes and their employees.
Dr. Mary Fennell is a professor of sociology, and a senior investigator with the Center for Gerontology and Healthcare Research, Brown University. Her current work examines patterns of change and innovation in health care organizations, particularly long-term care providers and cancer care delivery systems.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Anderson KA, Dabelko-Schoeny H, Johnson TD. The state of adult day services: Findings and implications from the MetLife national study of adult day services. Journal of Applied Gerontology. 2013;32:729–748. doi: 10.1177/0733464812447284. [DOI] [PubMed] [Google Scholar]
- Basu J, Cooper J. Out of area travel for rural and urban counties: A story of ambulatory care sensitive hospitalizations for New York state residents. The Journal of Rural Health. 2000;16:129–138. doi: 10.1111/j.1748-0361.2000.tb00446.x. [DOI] [PubMed] [Google Scholar]
- Castle NG, Engberg J, Lave J, Fisher A. Factors associated with increasing nursing home closures. Health Services Research. 2009;44:1088–1109. doi: 10.1111/j.1475-6773.2009.00954.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Nursing home data compendium 2013. 2013 Retrieved from https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/downloads/nursinghomedatacompendium_508.pdf.
- ESRI. ArcGIS Desktop: Release 10. Redlands, CA: Environmental Systems Research Institute; 2011. [Google Scholar]
- Feng Z, Lepore M, Clark MA, Tyler D, Smith DB, Mor V, Fennell ML. Geographic concentration and correlates of nursing home closures: 1999–2008. Archives of Internal Medicine. 2011;171:806–813. doi: 10.1001/archinternmed.2010.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, Cadigan RO, Miller EA, Stevenson DG, Clark M, Mor V. Supporting home-and community-based care: Views of long-term care specialists. Medical Care Research and Review. 2010;67:82S–101S. doi: 10.1177/1077558710366863. [DOI] [PubMed] [Google Scholar]
- Golant SM. Do impaired older persons with health care needs occupy US assisted living facilities? An analysis of six national studies. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2004;59:S68–S79. doi: 10.1093/geronb/59.2.s68. [DOI] [PubMed] [Google Scholar]
- Gresenz CR, Rogowski J, Escarce JJ. Updated variable radius measures of hospital competition. Health Services Research. 2004;39:417–430. doi: 10.1111/j.1475-6773.2004.00235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grzybowski S, Stoll K, Kornelsen J. Distance matters: A population based study examining access to maternity services for rural women. BMC Health Services Research. 2011;11:147–154. doi: 10.1186/1472-6963-11-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. epidemiologic studies. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2006;83 doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. How is the Affordable Care Act leading to changes in Medicaid long-term services and supports (LTSS) today? State adoption of six LTSS options. 2013 Retrieved from https://kaiserfamilyfoundation.files.wordpress.com/2013/04/8079-02.pdf.
- Kane RL, Kane RA. What older people want from long-term care, and how they can get it. Health Affairs. 2001;20:114–127. doi: 10.1377/hlthaff.20.6.114. [DOI] [PubMed] [Google Scholar]
- Kassner E. A balancing act: State long-term care reform. Washington, DC: AARP, Public Policy Institute; 2008. [Google Scholar]
- Katz MH. There’s no place like home. Archives of Internal Medicine. 2011;171:804–805. doi: 10.1001/archinternmed.2010.493a. [DOI] [PubMed] [Google Scholar]
- Konetzka RT. The hidden costs of rebalancing long-term care. Health Services Research. 2014;49:771–777. doi: 10.1111/1475-6773.12190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBlanc AJ, Tonner MC, Harrington C. Medicaid 1915 (c) home and community-based services waivers across the states. Health Care Financing Review. 2000;22:159–174. [PMC free article] [PubMed] [Google Scholar]
- Lowe RA, Fu R, Ong ET, McGinnis PB, Fagnan LJ, Vuckovic N, Gallia C. Community characteristics affecting emergency department use by Medicaid enrollees. Medical Care. 2009;47:15–22. doi: 10.1097/MLR.0b013e3181844e1c. [DOI] [PubMed] [Google Scholar]
- Metlife. The MetLife National Study of adult day services providing support to individuals and their family caregivers. 2010 Retrieved from https://www.metlife.com/assets/cao/mmi/publications/studies/2010/mmi-adult-day-services.pdf.
- Ng T, Stone J, Harrington C. Medicaid home and community-based services: How consumer access is restricted by state policies. Journal of Aging & Social Policy. 2015;27:21–46. doi: 10.1080/08959420.2015.969078. [DOI] [PubMed] [Google Scholar]
- Rudavsky R, Mehrotra A. Sociodemographic characteristics of communities served by retail clinics. The Journal of the American Board of Family Medicine. 2010;23:42–48. doi: 10.3122/jabfm.2010.01.090033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuurman N, Fiedler RS, Grzybowski SCW, Grund D. Defining rational hospital catchments for non-urban areas based on travel-time. International Journal of Health Geographics. 2006;5:43–53. doi: 10.1186/1476-072X-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DB. Long term care in transition: The regulation of nursing homes. Washington, DC: Beard Books; 2001. [Google Scholar]
- Smith DB, Feng Z, Fennell ML, Zinn J, Mor V. Racial disparities in access to long-term care: The illusive pursuit of equity. Journal of Health Politics, Policy and Law. 2008;33:861–881. doi: 10.1215/03616878-2008-022. [DOI] [PubMed] [Google Scholar]
- Stevenson DG, Grabowski DC. Sizing up the market for assisted living. Health Affairs. 2010;29:35–43. doi: 10.1377/hlthaff.2009.0527. [DOI] [PubMed] [Google Scholar]
- Tyler DA, Feng Z, Leland NE, Gozalo PL, Intrator I, Mor V. Trends in post-acute care and staffing in US nursing homes, 2001–2010. Journal of the American Medical Directors Association. 2013;14:817–820. doi: 10.1016/j.jamda.2013.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virnig BA, Ma H, Hartman LK, Moscovice I, Carlin B. Access to home-based hospice care for rural populations: Identification of areas lacking service. Journal of Palliative Medicine. 2006;9:1292–1299. doi: 10.1089/jpm.2006.9.1292. [DOI] [PubMed] [Google Scholar]