Abstract
Background
A scoring system allows risk stratification of morbidity might be helpful for selecting risk-adapted interventions to improve surgical safety. Few studies have been designed to develop scoring systems to predict SSIs after laparoscopic gastrectomy for gastric cancer.
Methods
We analyzed the records of 2364 patients who underwent laparoscopic gastrectomy for gastric cancer. A logistic regression model was used to identify the determinant variables and develop a predictive score.
Results
There were 2364 patients, of whom 131 (5.5 %) developed overall SSIs, 33 (1.4 %) developed incisional SSIs, and 98 (4.1 %) developed organ/space SSIs. No significant risk factor was associated with incisional SSIs. A multivariate analysis showed the following adverse risk factors for organ/space SSIs: BMI ≥ 25 kg/m2, intraoperative blood loss ≥75 ml, operation time ≥240 min, and perioperative transfusion. Each of these factors contributed 1 point to the risk score. The organ/space SSIs rates were 1.8, 3.9, 9.9, and 39.0 % for the low-, intermediate-, high-, and extremely high-risk categories, respectively (p < 0.001). The area under the receiver operating characteristic curve for the score of organ/space SSIs was 0.734. There were no statistically significant differences between the observed and predicted incidence rates for organ/space SSIs in the validation set.
Conclusions
This validated and simple scoring system could accurately predict the risk of organ/space SSIs after laparoscopic gastrectomy for gastric cancer. The score might be helpful in the selection of risk-adapted interventions to decrease the incidence rates of organ/space SSIs.
Keywords: Stomach cancer, Laparoscopy, Gastrectomy, SSI, Scoring system
Surgical site infections (SSIs) are one of the most common nosocomial infections, accounting for 14–16 % of nosocomial infections overall and 38 % of nosocomial infections among surgical patients [1]. SSIs can lead to prolonged hospitalization, increased morbidity and mortality, increased surgery-related costs, and decreased quality of life [1, 2]. The incidence rates of overall SSIs after open gastrectomy are 7.0–20.8 % [3–6]. With an increase in the number of laparoscopic surgeries performed in gastric cancer patients, SSIs after laparoscopic gastrectomy have decreased compared with open procedures [7], but they are still one of the most serious concerns for surgeons and surgical patients. Therefore, the identification of patients who are at a high risk of SSIs might allow for the selection of a risk-adapted laparoscopic procedure and intervening perioperative measures to reduce SSIs, improve surgical safety and patient quality of life, and achieve the goal of being minimally invasive. The objective of the present study was to identify the risk factors for SSIs after a laparoscopic radical gastrectomy for gastric cancer in 2364 patients treated in our center. We aimed to use these risk factors to develop a scoring system for predicting SSIs.
Materials and methods
Materials
This study was a retrospective analysis of a prospectively collected database of 2364 primary gastric cancer patients treated with a laparoscopic radical gastrectomy in the Department of Gastric Surgery of Fujian Medical University Union Hospital, Fuzhou, China, between May 2007 and Jun 2014. The inclusion criteria were as follows: a histologically confirmed adenocarcinoma of the stomach; no evidence of tumors invading the adjacent organs (pancreas, spleen, liver, and transverse colon), para-aortic lymph node enlargement, or distant metastasis demonstrated by abdominal computed tomography (CT) and/or abdominal ultrasound and posteroanterior chest radiographs; and a D1/D1 + α/D1 + β/D2 lymphadenectomy with curative R0 according to the pathological diagnosis after the operation. The exclusion criteria were as follows: intraoperative evidence of peritoneal dissemination, invasion into the adjacent organs, or a distant metastasis; conversion to an open laparotomy; and incomplete pathological data. All procedures were performed after obtaining written informed consent following explanation of the surgical and oncological risks. The patient demographics, underlying diseases, clinicopathology, surgery data, and data on the preoperative and postoperative monitoring were recorded in a clinical data system for gastric cancer surgery [8]. The staging was performed according to the 7th edition of the UICC TNM classification [9]. The type of surgical resection (i.e., a distal subtotal gastrectomy, proximal subtotal gastrectomy, or total gastrectomy) and extent of lymph node dissection were selected according to the Japanese gastric cancer treatment guidelines [10]. Data were randomly assigned into two subsets using the SPSS version 18.0 (SPSS, Chicago, IL, USA), which were split 70/30: one for model development and the other for validation testing.
Variables and definitions
We defined SSIs according to the surgical patient component of the 1999 Centers for Disease Control and Prevention (CDC) National Nosocomial Infection Surveillance (NNIS) System manual; [1] this definition includes incisional (superficial, deep) and organ/space SSIs. Briefly, superficial incisional SSIs were diagnosed within 30 days of the operation, confined to the skin and subcutaneous tissue, and associated with at least one of the following: pus, microorganisms isolated from culture of fluid or tissue, or signs or symptoms of infection. Either the surgeon or an attending physician made the diagnosis of a superficial SSI. A deep incisional SSI was diagnosed when the wound infection had spread to the fascia and muscular layers, but not the peritoneal cavity or pelvis (the organ/space), and one of the following criteria was also present: pus originating from the deep part of the incision, spontaneous wound dehiscence, or a wound opened by the surgeon. The surgeon made the diagnosis of a deep infection. Organ/space infections involved any organ or space other than an incised layer of the abdominal wall, such as the peritoneal cavity or pelvis.
The potential variables for SSIs were extracted from the database, including antibiotic prophylaxis (1 g of cefazolin was given 30 < 30 min before the incision, and an additional dose was given every 3 h during surgery), gender, age, body mass index (BMI, BMI ≥ 25 is considered as overweight, according to the World Health Organization classification [11]), previous abdominal surgery, Charlson co-morbidity score, perioperative transfusion (transfusion threshold Hb < 8.0 g/dl; maintenance range 8.0–9.5 g/dl), tumor location, tumor diameter, T stage, N stage, TNM stage, operation time (recorded from the skin incision to skin closure), intraoperative blood loss (estimated according to the volume of blood absorbed by the gauze and suction pumped after subtracting the volume of the fluids used for irrigation), type of surgical resection, type of reconstruction, D1/D1 +/D2 lymphadenectomy, and numbers of resected LNs.
Statistical analysis
The continuous data were reported as the mean ± SD, and the differences between the groups were analyzed using t tests. The categorical data are presented as the proportion percentage and were analyzed with the Chi-square test or Fisher’s exact test. The variables with p < 0.05 in the univariate analysis were subsequently included in a multivariate binary logistic regression model. The variables that remained significant in the multivariate analysis were used to construct a scoring system to classify the patients into groups according to their risk of SSIs. A goodness-of-fit test was conducted to assess how well the model could discriminate between patients with and without SSIs. Model calibration, the degree to which the observed outcomes were similar to the outcomes predicted by the model across patients, was examined by comparing the observed averages with the predicted averages within each of the subgroups arranged in increasing order of patient risk. p < 0.05 was considered to be statistically significant. The statistical analyses were performed with SPSS version 18.0 (SPSS, Chicago, IL, USA).
Results
Clinicopathological characteristics of the patients
The clinicopathological characteristics of the 2364 patients are listed in Table 1. There were 1775 males and 589 females with a mean age of 60.93 ± 10.84 years. The average body mass index (BMI) of the patients was 22.20 ± 3.08 kg/m2. A total gastrectomy was performed in 1264 patients (53.5 %), distal gastrectomy in 1045 patients (44.2 %), and proximal gastrectomy in 55 patients (2.3 %); a D1 lymphadenectomy or D1 + lymphadenectomy was performed in 450 patients (19.0 %) and 1 914 patients for D2 lymphadenectomy (81.0 %); combined resection of other organs was performed in 17 patients (nine splenectomy: six for parenchymal injuries, one for splenic hilar vascular injury, one for splenic infarction, one for hypersplenism; three combined cholecystectomy for gallstone; three combined partial transverse colectomy for injuries; and two combined partial jejunectomy for injuries). The average surgery time was 180.86 ± 51.49 min, blood loss was 73.50 ± 104.04 ml, and the number of dissected lymph nodes per patient was 33.38 ± 12.96. According to the UICC TNM Classification of Malignant Tumors, 7th Edition, 477 patients (20.2 %) were in stage Ia, 216 (9.1 %) were in stage Ib, 242 (10.2 %) were in stage IIa, 264 (11.2 %) were in stage IIb, 239 (10.1 %) were in stage IIIa, 374 (15.8 %) were in stage IIIb, and 552 (23.3 %) were in stage IIIc.
Table 1.
Univariable analyses of possible risk factors for the development of SSIs
| Variables | No. patients | Incisional SSIs | Organ/space SSIs | Overall SSIs | |||
|---|---|---|---|---|---|---|---|
| (n = 2364) | (n = 33) | p | (n = 98) | p | (n = 131) | p | |
| Age (year) | 0.810 | 0.344 | 0.481 | ||||
| <65 | 1529 | 22 | 59 | 81 | |||
| ≥65 | 835 | 11 | 39 | 50 | |||
| Gender | 0.753 | 0.077 | 0.168 | ||||
| Male | 1775 | 24 | 81 | 105 | |||
| Female | 589 | 9 | 17 | 26 | |||
| ASA | 0.255 | 0.461 | 0.953 | ||||
| ≤2 | 2276 | 33 | 93 | 126 | |||
| >2 | 88 | 0 | 5 | 5 | |||
| BMI (kg/m2) | 0.390 | 0.000 | 0.000 | ||||
| <25 | 2026 | 30 | 62 | 92 | |||
| ≥25 | 338 | 3 | 36 | 39 | |||
| Previous abdominal surgery | 0.809 | 0.858 | 0.954 | ||||
| Yes | 347 | 4 | 15 | 19 | |||
| None | 2017 | 29 | 83 | 112 | |||
| Charlson score | 0.756 | 0.002 | 0.023 | ||||
| 0 | 1652 | 22 | 59 | 84 | |||
| 1 | 492 | 5 | 34 | 39 | |||
| ≥2 | 220 | 3 | 5 | 8 | |||
| Perioperative transfusion | 0.191 | 0.000 | 0.000 | ||||
| Yes | 319 | 7 | 34 | 41 | |||
| None | 2045 | 26 | 64 | 90 | |||
| Tumor diameter (mm) | 0.406 | 0.698 | 0.930 | ||||
| <50 | 1634 | 25 | 66 | 91 | |||
| ≥50 | 730 | 8 | 32 | 40 | |||
| Tumor location | 0.998 | 0.644 | 0.761 | ||||
| Upper | 614 | 8 | 26 | 34 | |||
| Middle | 424 | 7 | 16 | 23 | |||
| Lower | 1034 | 14 | 40 | 54 | |||
| ≥2 areas | 292 | 4 | 16 | 20 | |||
| T stage | 0.603 | 0.877 | 0.939 | ||||
| T1 | 572 | 10 | 21 | 31 | |||
| T2 | 286 | 3 | 11 | 14 | |||
| T3 | 687 | 9 | 29 | 38 | |||
| T4a | 819 | 11 | 37 | 48 | |||
| N stage | 0.133 | 0.227 | 0.674 | ||||
| N0 | 888 | 15 | 29 | 44 | |||
| N1 | 341 | 8 | 14 | 22 | |||
| N2 | 382 | 2 | 22 | 24 | |||
| N3 | 753 | 8 | 33 | 41 | |||
| TNM stage | 0.559 | 0.787 | 0.766 | ||||
| IA | 477 | 6 | 17 | 23 | |||
| IB | 216 | 5 | 6 | 11 | |||
| IIA | 242 | 2 | 8 | 10 | |||
| IIB | 264 | 6 | 13 | 19 | |||
| IIIA | 239 | 4 | 11 | 15 | |||
| IIIB | 374 | 4 | 16 | 20 | |||
| IIIC | 552 | 6 | 27 | 33 | |||
| Operative time (mins) | 0.261 | 0.000 | 0.000 | ||||
| <180 | 1625 | 27 | 46 | 73 | |||
| 180–240 | 519 | 4 | 22 | 26 | |||
| ≥240 | 220 | 2 | 30 | 32 | |||
| IBL (ml) | 0.914 | 0.000 | 0.000 | ||||
| <75 | 1917 | 27 | 55 | 82 | |||
| ≥75 | 447 | 6 | 43 | 49 | |||
| Surgical resection | 0.546 | 0.061 | 0.186 | ||||
| Total | 1264 | 16 | 60 | 76 | |||
| Distal | 1045 | 16 | 38 | 54 | |||
| Proximate | 55 | 1 | 0 | 1 | |||
| Reconstruction | 0.499 | 0.063 | 0.203 | ||||
| Roux-en-Y | 1264 | 16 | 60 | 76 | |||
| B-I | 879 | 13 | 32 | 45 | |||
| B-II | 166 | 3 | 6 | 9 | |||
| Esophagogastric | 55 | 1 | 0 | 1 | |||
| Lymphadenectomy | 0.567 | 0.485 | 0.367 | ||||
| D1/D1+ | 450 | 5 | 16 | 21 | |||
| D2 | 1914 | 28 | 82 | 110 | |||
| No. of resected LNs | 0.861 | 0.292 | 0.407 | ||||
| <33 | 1325 | 18 | 60 | 79 | |||
| ≥33 | 1039 | 15 | 38 | 53 | |||
BMI body mass index, IBL intraoperative blood loss
Incidence and characteristics of SSIs
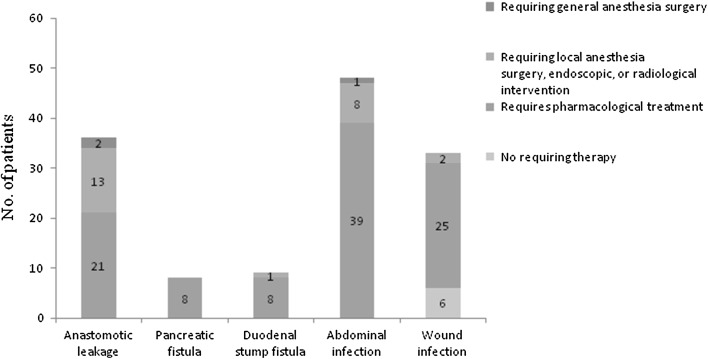
Of 2364 patients, intraoperative complications were observed in 25 patients (1.1 %). Postoperative complications were observed in 330 patients (14.0 %) (Table 2), among which SSIs (all incisional and organ/space SSIs were grouped together) were present in 131 patients. A total of 33 (1.4 %) patients had incisional SSIs, including 29 superficial incisional SSIs and four deep incisional SSIs. A total of 98 (4.1 %) patients had organ/space SSIs. Thirty-three of the 98 organ/space SSIs were intra-abdominal abscesses due to anastomotic leakage; nine resulted from duodenal stump fistula, five resulted from pancreatic fistula, three were abscesses resulting from both pancreatic fistula and anastomotic leakage, and the cause of organ/space SSIs was unknown in 48 patients. Seventy-one of the 98 organ/space SSIs required anti-infection treatment, 24 required endoscopic or radiological intervention, and three required general anesthesia during surgery (two anastomotic leakages and one intra-abdominal abscess). Six of the 33 incisional SSIs only required dressing changes, 25 required anti-infection treatment, and two required resuturing (Fig. 1). The mean lengths of the postoperative hospital stay of patients with non-SSI were 12.30 ± 5.18 days, and of patients with overall SSIs, superficial incisional SSIs, and organ/space SSIs were 27.69 ± 16.56, 18.27 ± 8.80, and 30.87 ± 17.37 days, respectively. Four patients (0.2 %) died by the 30th postoperative day. The following causes of death were noted: intra-abdominal abscesses due to anastomotic leakage (two patients); pancreatic fistula and anastomotic leakage (one patient); and organ/space SSIs with unknown cause (one patient). And by the 90th postoperative day, the deaths added up to eight patients (0.3 %). Complications associated with SSIs were anastomotic bleeding, abdominal bleeding, chylous leak, sepsis, pneumonia, and transient liver enzyme abnormalities (Table 2).
Table 2.
Intraoperative and postoperative morbidity associated with surgical site infections
| No. Patients N (%) |
With SSIs N (%) |
OR | p | |
|---|---|---|---|---|
| Intraoperative morbidity | 25 (1.1) | 3 (0.1) | 2.355 (0.696–7.973) | 0.168 |
| Vascular injury | 13 (0.6) | 2 (0.1) | 3.132 (0.687–14.277) | 0.140 |
| Spleen injury | 7 (0.3) | 1 (0.0) | 2.855 (0.341–23.891) | 0.333 |
| Transverse colon injury | 3 (0.1) | 0 | 0 | 0.999 |
| Jejunum injury | 2 (0.1) | 0 | 0 | 0.999 |
| Postoperative morbidity | 330 (14.0) | / | / | / |
| Incisional SSIs | 31 (1.3) | / | / | / |
| Organ/space SSIs | 98 (4.1) | / | / | / |
| Anastomotic bleeding | 11 (0.5) | 3 (0.1) | 6.519 (1.709–24.865) | 0.006 |
| Abdominal bleeding | 18 (0.8) | 7 (0.3)) | 11.403 (4.346–29.923) | 0.000 |
| Ileus | 24 (1.0) | 2 (0.1) | 1.558 (0.362–6.698) | 0.551 |
| Anastomotic stricture | 3 (0.1) | 0 | 0 | 0.999 |
| Remnant gastric stasis | 25 (1.1) | 0 | 0 | 0.998 |
| Chylous leak | 21 (0.9) | 7 (0.3) | 8.948 (3.548–22.568) | 0.000 |
| Sepsis | 5 (0.2) | 4 (0.2) | 70.299 (7.800–633.557) | 0.000 |
| Adhesive intestinal obstruction | 1 (0.0) | 0 | 0 | 0.999 |
| Infarct of spleen | 1 (0.0) | 0 | 0 | 0.999 |
| Pneumonia | 137 (5.8) | 35 (1.5) | 7.617 (4.930–11.768) | 0.000 |
| Arrhythmia | 6 (0.3) | 0 | 0 | 0.999 |
| Cardiac failure | 3 (0.1) | 0 | 0 | 0.999 |
| Transient liver enzyme abnormalities | 8 (0.3) | 2 (0.1) | 5.755 (1.150–28.792) | 0.033 |
| Urinary tract infection | 11 (0.5) | 2 (0.1) | 3.447 (0.747–15.893) | 0.113 |
| Catheter-related infection | 4 (0.2) | 0 | 0 | 0.999 |
| DIC | 4 (0.2) | 0 | 0 | 0.999 |
| Cerebral infarction | 1 (0.0) | 0 | 0 | 0.999 |
SSIs surgical site infections; DIC disseminated intravascular coagulation
Fig. 1.
Rates of the SSIs and the treatments for the SSIs
Univariate and multivariate analyses associated with the SSIs
Tables 1 and 3 show the results of the univariate and multivariate analyses of the possible risk factors for the development of SSIs. No statistically significant factors were associated with incisional SSIs in the univariate analyses. In addition, five factors were associated with an increased risk of organ/space SSIs, including the BMI (p < 0.001), Charlson co-morbidity score (p = 0.002), perioperative transfusion (p < 0.001), operation time ≥240 min (p < 0.001), and intraoperative blood loss (p < 0.001). We evaluated the risk factors for organ/space SSIs by multivariate analysis. The multivariate analysis revealed that the following were adverse risk factors for organ/space SSIs: BMI ≥ 25 kg/m2 (OR = 3.638, p < 0.001), intraoperative blood loss ≥ 75 ml (OR = 2.071, p = 0.010), operation time ≥ 240 min (OR = 3.865, p < 0.001), and perioperative transfusion (OR = 3.131, p < 0.001).
Table 3.
Multivariate analysis associated with organ/space SSIs
| Variables | β | OR | 95 % CI | p |
|---|---|---|---|---|
| BMI ≥ 25 kg/m2 | 1.291 | 3.638 | 2.135–6.199 | <0.001 |
| Operative time ≥ 240 min | 1.352 | 3.865 | 2.137–6.990 | <0.001 |
| IBL ≥ 75 ml | 0.728 | 2.071 | 1.192–3.597 | 0.010 |
| Perioperative transfusion | 1.141 | 3.131 | 1.798–5.450 | <0.001 |
β regression coefficients, BMI body mass index, IBL intraoperative blood loss
The scoring system for organ/space SSIs
Despite the differences in the regression coefficients, which ranged from 0.728 to 1.352 for organ/space SSIs, respectively, 1 point was assigned for each of the risk factors for simplicity. The resulting BBOT (BMI, blood loss, operation time, and transfusion) scores were built for organ/space SSIs. Because only five of the patients had 4 points, the following four risk groups were established: low risk (0 points, i.e., no risk factors), intermediate risk (1 point, i.e., one risk factor), high risk (2 points, i.e., two risk factors), and extremely high risk (3 or 4 points, i.e., three or four risk factors). The distribution of the patients according to the scoring system was as follows: low risk, 59.0 %, intermediate risk, 28.2 %, high risk, 10.3 %, and extremely high risk, 2.5 %. The incidence rates of organ/space SSIs among the patients in the low-, intermediate-, high-, and extremely high-risk categories were 1.8, 3.9, 9.9, and 39.0 %, respectively (p < 0.001).The relative risks of organ/space SSIs in the intermediate-, high-, and extremely high-risk groups compared with the low-risk group were 2.136 (95 %CI, 1.101–4.145, p = 0.025), 5.869 (95 % CI, 2.960–11.635, p < 0.001), and 34.027 (95 % CI, 15.570–74.360, p < 0.001), respectively (Table 4).
Table 4.
BBOT scoring system for organ/space SSIs
| Risk group | BBOT score | No. patients (n = 1653 %) | No. patients (n %) | OR | 95 % CI | p |
|---|---|---|---|---|---|---|
| Low | 0 | 975 (59.0) | 18 (1.8) | 1 | / | / |
| Intermediate | 1 | 466 (28.2) | 18 (3.9) | 2.136 | 1.101–4.145 | 0.025 |
| High | 2 | 171 (10.3) | 17 (9.9) | 5.869 | 2.960–11.635 | <0.001 |
| Extremely high | ≥3 | 41 (2.5) | 16 (39.0) | 34.027 | 15.570–74.360 | <0.001 |
BBOT, BMI, blood loss, operation time, and transfusion
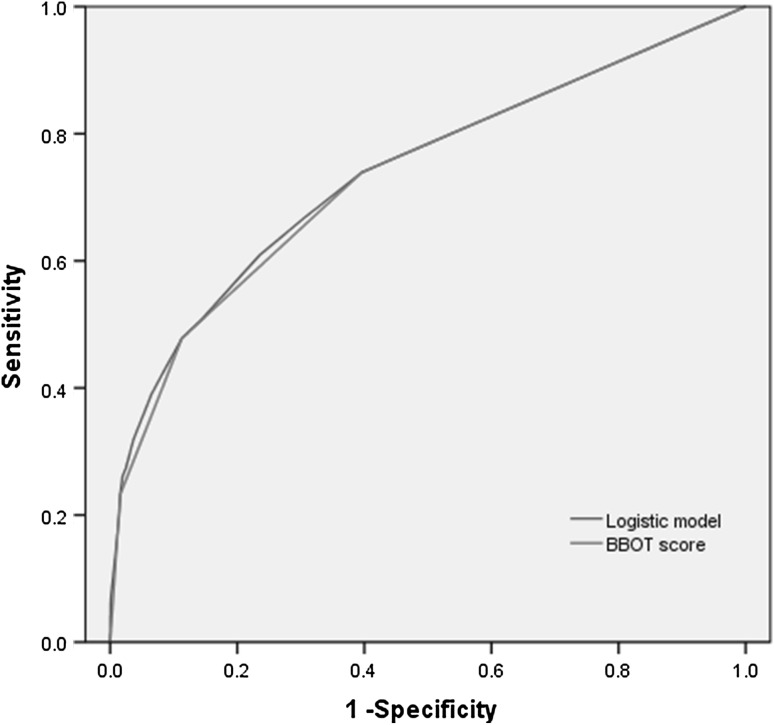
Discrimination
The final models discriminated the development sets with the areas under the receiver operating characteristic (ROC) curve. The area under the ROC curve was 0.739 (0.669–0.808) for the logistic regression model and 0.734 (0.665–0.803) for the simplified BBOT score for organ/space SSIs (Fig. 2). To evaluate the models’ performance, the observed versus predicted incidence rates in the validation set were compared. The predicted incidence rates for the low-, intermediate-, high-, and extremely high-risk categories in the validation set were 1.9, 3.9, 10.0, and 39.0 %, respectively. There were no statistically significant differences found between the observed and BBOT predicted incidence rates for organ/space SSIs in the validation set (p > 0.05) (Table 5).
Fig. 2.
Receiver operating characteristic curves for prediction of organ/space SSIs after laparoscopic gastrectomy in the development sets
Table 5.
Observed and BBOT predicted incidence rates for organ/space SSIs in the validation set
| Risk group | Observed organ/space SSIs (%) | BBOT predicted organ/space SSIs (%) | p |
|---|---|---|---|
| Low | 2.3 | 1.9 | 0.590 |
| Intermediate | 3.0 | 3.9 | 0.587 |
| High | 8.8 | 10.0 | 0.772 |
| Extremely high | 38.9 | 39.0 | >0.999 |
Discussion
SSIs are one of the most common nosocomial infections, and they are a fundamentally important clinical outcome indicator in elective surgery [12–15]. Effectively decreasing the incidence of SSIs is a global challenge. In 2002, the Surgical Infection Prevention project (SIP) was initiated under the direction of the CMS and CDC [16]. The aim of SIP was to reduce the nationwide incidence of SSI through systems level protocol implementation. The SIP evolved into the Surgical Care Improvement Project (SCIP), which was a joint effort between the CMS and Joint Commission to further improve the nationwide compliance with standards of care in surgical practice. Some sites have demonstrated decreased incidence of SSIs associated with improved compliance in SCIP measures [17, 18]. However, the incidence of SSIs has failed to decrease substantially over time on a national scale [19, 20]. Therefore, it is particularly important to identify and prevent the risk factors for SSIs. The incidence rates of overall SSIs, incisional SSIs, and organ/space SSIs after tradition open gastrectomy are 7.0–20.8, 1.7–8.6, and 5.1–13.3 %, respectively [3–6]. To the best of my knowledge, no reports have been designed to identify the risk factors for SSIs after a laparoscopic radical gastrectomy for gastric cancer. In the present study, laparoscopic gastrectomy was initially performed in patients diagnosed with cT1N0M0–cT2N0M0 gastric cancer. With the experience accumulation and expanded use of laparoscopic gastrectomy, the indications were then gradually extended to more advanced stages of disease. And the incidence rates of overall SSIs, incisional SSIs, and organ/space SSIs after traditional open gastrectomy were 5.5, 1.4, and 4.1 %, respectively. Moreover, 4.1 % (4/98) of patients with organ/space SSIs died by the 30th postoperative day. As a result, investigating the risk factors for organ/space SSIs and selecting risk-adapted interventions may help reduce the incidence rates of organ/space SSIs.
Previous studies have reported several risk factors for SSIs after open gastrectomy, such as advanced age, a BMI of 25 or higher, diabetes mellitus, a longer operation duration, blood loss, total gastrectomy, and combined resection procedures [4, 6, 21]. However, laparoscopic gastrectomy has its own characteristics, and the aforementioned risk factors have provided limited reference value for this procedure. And we found that the perioperative transfusion, operation time ≥240 min, intraoperative blood loss ≥75 ml, and BMI ≥ 25 kg/m2 were the risk factors associated with the incidence of organ/space SSIs after laparoscopic gastrectomy. Intraoperative blood loss requires additional hemostasis by ligation and compression, and a massive hemorrhage might lead to hypovolemia; these conditions appear to be associated with poor wound healing and increased infection rates from hypoxia [22–24]. Furthermore, the cases of preoperative anemia, intraoperative or postoperative blood loss that require allogeneic blood transfusion typically induce immunosuppression and predispose patients to postoperative infection. Allogeneic leukocytes may play a critical role in the induction of transfusion-induced immunosuppression [25–28]. The operation time depends on various parameters, such as the surgeon’s experience and technical or intraoperative problems (e.g., accidental puncture of an intra-abdominal organ, intraoperative hematoma, or organ lesions). Increasing the length of the procedure theoretically increases the susceptibility of the wound by increasing bacterial exposure and the extent of tissue trauma (more extensive surgical procedure) and decreasing the tissue level of the antibiotic [29, 30]. In addition, there is more surrounding tissue to separate and dissect in patients who have a high BMI. These patients typically have significantly higher rates of SSIs as well as conversion to open surgery and postoperative complications [6].
Few studies have been designed to create a scoring system for predicting the risk of SSIs after an open procedure. Among these systems, the National Nosocomial Infections Surveillance (NNIS) basic risk index is one of the most widely used systems to predict the risk of SSIs. The NNIS basic SSI risk index consists of the following three criteria: American Society of Anesthesiologists score of 3, 4, or 5; wound class; and duration of surgery. Moreover, it has proven to be useful for risk adjustment for many open procedures. However, Gaynes [7] also noted that the use of a laparoscope is accompanied by significantly lower rates of SSIs after gastric surgery, and the NNIS basic SSI risk index might be not suitable for laparoscopic gastrectomy. Our BBOT scoring system was based on the final logistic regression model. With respect to the risk stratification for organ/space SSIs, the BBOT scoring system classified the patients after laparoscopic gastrectomy into four groups and identified the extremely high-risk group, which had a 23.8-fold higher risk of organ/space SSIs than that of the lowest risk group. The BBOT scoring system discriminated the development sets with an area under the ROC curve of 0.734, which is similar to the logistic regression model. There were no statistically significant differences between the observed and BBOT scoring system predicted incidence rates in the validation set, indicating that this system performed well. Patient and disease characteristic data are routinely available, which might have implications for selecting risk-adapted interventions to improve surgical safety. Since only the BMI can be identified preoperatively, overweight patients (BMI ≥ 25 kg/m2) might be referred to operators with more experience to cut operation time and reduce blood loss. Also, if one or more of their other risk factors occurs intraoperatively or postoperatively, such as perioperative transfusion, operation time ≥240 min, intraoperative blood loss ≥75 ml, it is necessary to be aware of the sign and symptom closely and must be examined by laboratory tests and imageological examinations postoperatively, in order to early detection and treatment of SSI.
Our study has some limitations. Firstly, as with other retrospective studies, inherent selective bias is inevitable, although we use a prospectively collected database. Second, there are only 14.3 % patients with BMI ≥ 25 kg/m2 in our study, whereas one-third of the US population had a BMI of 27 kg/m2 or greater [31]. So it would seem that this scoring system should be validated by Western centers before applying it in Westerners.
In conclusion, our BBOT scoring system allows for easy and validated risk stratification of the organ/space SSIs in the clinical setting. This stratification might be helpful for selecting risk-adapted interventions that reduce the rates of organ/space SSIs and improve the surgical safety. A prospective multiple-center study with a large series would help validate this scoring system.
Acknowledgments
The authors are thankful to Fujian Medical University Union Hospital for the management of our gastric cancer patient database.
Funding
This study was funded by the National Key Clinical Specialty Discipline Construction program of China (No. [2012]649) and the Key Projects of Science and Technology Plan of Fujian Province (No. 2014Y0025).
Compliance with ethical standards
Disclosures
Drs. Ru-Hong Tu, Chang-Ming Huang, Jian-Xian Lin, Qi-Yue Chen, Chao-Hui Zheng, Ping Li, Jian-Wei Xie, Jia-Bin Wang, Jun Lu, Long-Long Cao, and Mi Lin have no conflicts of interest or financial ties to disclose.
References
- 1.Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250–278. doi: 10.1086/501620. [DOI] [PubMed] [Google Scholar]
- 2.Smith RL, Bohl JK, McElearney ST, Friel CM, Barclay MM, Sawyer RG, Foley EF. Wound infection after elective colorectal resection. Ann Surg. 2004;239:599–605. doi: 10.1097/01.sla.0000124292.21605.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gervaz P, Bandiera-Clerc C, Buchs NC, Eisenring MC, Troillet N, Perneger T, Harbarth S. Scoring system to predict the risk of surgical-site infection after colorectal resection. Br J Surg. 2012;99:589–595. doi: 10.1002/bjs.8656. [DOI] [PubMed] [Google Scholar]
- 4.Migita K, Takayama T, Matsumoto S, Wakatsuki K, Enomoto K, Tanaka T, Ito M, Nakajima Y. Risk factors for surgical site infections after elective gastrectomy. J Gastrointest Surg. 2012;16:1107–1115. doi: 10.1007/s11605-012-1838-1. [DOI] [PubMed] [Google Scholar]
- 5.Ozalp N, Zulfikaroglu B, Gocmen E, Acar A, Ekiz I, Koc M, Tez M. Risk factors for surgical site infection after gastrectomy with D2 lymphadenectomy. Surg Today. 2009;39:1013–1015. doi: 10.1007/s00595-008-3984-3. [DOI] [PubMed] [Google Scholar]
- 6.Hirao M, Tsujinaka T, Imamura H, Kurokawa Y, Inoue K, Kimura Y, Shimokawa T, Furukawa H, Osaka Gastrointestinal Cancer Chemotherapy Study Group (OGSG) Overweight is a risk factor for surgical site infection following distal gastrectomy for gastric cancer. Gastric Cancer. 2013;16:239–244. doi: 10.1007/s10120-012-0174-1. [DOI] [PubMed] [Google Scholar]
- 7.Gaynes RP, Culver DH, Horan TC, Edwards JR, Richards C, Tolson JS. Surgical site infection (SSI) rates in the United States, 1992–1998: the National Nosocomial Infections Surveillance System basic SSI risk index. Clin Infect Dis. 2001;33(Suppl 2):S69–S77. doi: 10.1086/321860. [DOI] [PubMed] [Google Scholar]
- 8.Hu YF, Yu J, Zhang C, Wang YN, Cheng X, Huang F, Li GX. Development and implementation of a clinical data mining system for gastric cancer surgery. Zhonghua Wei Chang Wai Ke Za Zhi. 2010;13:510–515. [PubMed] [Google Scholar]
- 9.Sobin LH, Gospodarowicz MK, Wittekind C. International Union Against Cancer(UICC) TNM classification of malignanttumours. 7. New York: Wiley-Liss; 2010. [Google Scholar]
- 10.Japanese Gastric Cancer Association Japanese gastric cancer treatment guidelines 2010 (ver. 3) Gastric Cancer. 2011;14:113–123. doi: 10.1007/s10120-011-0042-4. [DOI] [PubMed] [Google Scholar]
- 11.Seidell JC, Flegal KM. Assessing obesity: classification and epidemiology. Br Med Bull. 1997;53:238–252. doi: 10.1093/oxfordjournals.bmb.a011611. [DOI] [PubMed] [Google Scholar]
- 12.Stone HH, Hooper CA, Kolb LD, Geheber CE, Dawkins EJ. Antibiotic prophylaxis in gastric, biliary and colonic surgery. Ann Surg. 1976;184:443–452. doi: 10.1097/00000658-197610000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cruse PJ, Foord R, The epidemiology of wound infection A 10-year prospective study of 62,939 wounds. Surg Clin North Am. 1980;60:27–40. doi: 10.1016/s0039-6109(16)42031-1. [DOI] [PubMed] [Google Scholar]
- 14.Haley RW, Culver DH, White JW, Morgan WM, Emori TG. The nationwide nosocomial infection rate. A new need for vital statistics. Am J Epidemiol. 1985;121:159–167. doi: 10.1093/oxfordjournals.aje.a113988. [DOI] [PubMed] [Google Scholar]
- 15.Vegas AA, Jodra VM, Garcia ML. Nosocomial infection in surgery wards: a controlled study of increased duration of hospital stays and directs cost of hospitalization. Eur J Epidemiol. 1993;9:504–510. [PubMed] [Google Scholar]
- 16.Dellinger EP, Hausmann SM, Bratzler DW, Johnson RM, Daniel DM, Bunt KM, Baumgardner GA, Sugarman JR. Hospitals collaborate to decrease surgical site infections. Am J Surg. 2005;190:9–15. doi: 10.1016/j.amjsurg.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Hedrick TL, Turrentine FE, Smith RL, McElearney ST, Evans HL, Pruett TL, Sawyer RG. Single-institutional experience with the surgical infection prevention project in intra-abdominal surgery. Surg Infect (Larchmt) 2007;8:425–435. doi: 10.1089/sur.2006.043. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen N, Yegiyants S, Kaloostian C, Abbas MA, Difronzo LA. The Surgical Care Improvement project (SCIP) initiative to reduce infection in elective colorectal surgery: which performance measures affect outcome? Am Surg. 2008;74:1012–1016. doi: 10.1177/000313480807401028. [DOI] [PubMed] [Google Scholar]
- 19.Hawn MT, Vick CC, Richman J, Holman W, Deierhoi RJ, Graham LA, Henderson WG, Itani KM. Surgical site infection prevention: time to move beyond the surgical care improvement program. Ann Surg. 2011;254:494–499. doi: 10.1097/SLA.0b013e31822c6929. [DOI] [PubMed] [Google Scholar]
- 20.Stulberg JJ, Delaney CP, Neuhauser DV, Aron DC, Fu P, Koroukian SM. Adherence to surgical care improvement project measures and the association with postoperative infections. JAMA. 2010;303:2479–2485. doi: 10.1001/jama.2010.841. [DOI] [PubMed] [Google Scholar]
- 21.Watanabe A, Kohnoe S, Shimabukuro R, Yamanaka T, Iso Y, Baba H, Higashi H, Orita H, Emi Y, Takahashi I, Korenaga D, Maehara Y. Risk factors associated with surgical site infection in upper and lower gastrointestinal surgery. Surg Today. 2008;38:404–412. doi: 10.1007/s00595-007-3637-y. [DOI] [PubMed] [Google Scholar]
- 22.Hartmann M, Jonsson K, Zederfeldt B. Effect of tissue perfusion and oxygenation on accumulation of collagen in healing wounds. Randomized study in patients after major abdominal operations. Eur J Surg. 1992;158:521–526. [PubMed] [Google Scholar]
- 23.Esrig BC, Frazee L, Stephenson SF, Polk HC, Fulton RL, Jones CE. The predisposition to infection following hemorrhagic shock. Surg Gynecol Obstet. 1977;144:915–917. [PubMed] [Google Scholar]
- 24.Hunt TK, Zederfeldt BH, Goldstick TK, Conolly WB. Tissue oxygen tensions during controlled hemorrhage. Surg Forum. 1967;18:3–4. [PubMed] [Google Scholar]
- 25.Heiss MM, Mempel W, Jauch KW, Delanoff C, Mayer G, Mempel M, Eissner HJ, Schildberg FW. Beneficial effect of autologous blood transfusion on infectious complications after colorectal cancer surgery. Lancet. 1993;342:1328–1333. doi: 10.1016/0140-6736(93)92247-Q. [DOI] [PubMed] [Google Scholar]
- 26.Jensen LS, Andersen AJ, Christiansen PM, Hokland P, Juhl CO, Madsen G, Mortensen J, Møller-Nielsen C, Hanberg-Sørensen F, Hokland M. Postoperative infection and natural killer cell function following blood transfusion in patients undergoing elective colorectal surgery. Br J Surg. 1992;79:513–516. doi: 10.1002/bjs.1800790613. [DOI] [PubMed] [Google Scholar]
- 27.Tartter PI. Blood transfusion and infectious complications following colorectal cancer surgery. Br J Surg. 1988;75:789–792. doi: 10.1002/bjs.1800750822. [DOI] [PubMed] [Google Scholar]
- 28.Rohde JM, Dimcheff DE, Blumberg N, Saint S, Langa KM, Kuhn L, Hickner A, Rogers MA. Health care-associated infection after red blood cell transfusion: a systematic review and meta-analysis. JAMA. 2014;311:1317–1326. doi: 10.1001/jama.2014.2726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hooton TM, Haley RW, Culver DH, White JW, Morgan WM, Carroll RJ. The joint associations of multiple risk factors with the occurrence of nosocomial infection. Am J Med. 1981;70:960–970. doi: 10.1016/0002-9343(81)90562-3. [DOI] [PubMed] [Google Scholar]
- 30.Tang RP, Chen HH, Wang YL, Changchien CR, Chen JS, Hsu KC, Chiang JM, Wang JY. Risk factors for surgical site infection after elective resection of the colon and rectum: a single-center prospective study of 2809 consecutive patients. Ann Surg. 2001;234:181–189. doi: 10.1097/00000658-200108000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL. Increasing prevalence of overweight among US adults. The National Health and Nutrition Examination Surveys, 1960–1991. JAMA. 1994;20(272):205–211. doi: 10.1001/jama.1994.03520030047027. [DOI] [PubMed] [Google Scholar]