Abstract
Subtle syndesmotic instability not evident on radiography can result in chronic ankle pain. The diagnosis is uncommon, and arthroscopic evaluation remains the gold standard for diagnosis. Definitive surgical management can be performed at the time of diagnosis. Patients with 2 to 4 mm of diastasis of the syndesmosis or translation can be treated with debridement alone, and patients with 4 mm or more of diastasis or translation can be treated with arthroscopic debridement and reduction followed by percutaneous stabilization. Percutaneous stabilization is accomplished by a TightRope technique, which involves passing 1 or 2 suture buttons through all 4 cortices of the distal tibia and fibula. This technique is used in lieu of the traditional syndesmotic screw, which requires a subsequent operation for removal.
Subtle syndesmotic injuries that fail to respond to conservative therapy can result in chronic pain and potential instability. It is also possible that chronic laxity of the talus within the mortise may contribute to arthrosis.1, 2 Treatment can be tailored to the degree of instability determined arthroscopically. Previous case series have reported success with arthroscopic debridement alone when the syndesmosis is measured to be 2 mm. Other studies have indicated that it may be useful to stabilize the syndesmosis after debridement.3, 4, 5, 6 It is important to differentiate subtle syndesmotic instability from frank or radiographically apparent syndesmotic widening because frank instability or widening does not necessarily require arthroscopic evaluation.1, 7, 8 We describe a treatment technique that allows for surgical debridement, reduction, and stabilization of subtle syndesmotic injuries at the time of arthroscopic diagnosis.
Surgical Technique
The patient is placed supine on the operating room table with a bump under the ipsilateral hip, and a thigh tourniquet is placed to minimize blood loss and maximize visualization when the surgeon is performing ankle arthroscopy. An Arthrex distal extremity leg holder is used to keep the operative foot level with an Arthrex noninvasive ankle distractor. This system again allows for better visualization within the ankle joint. Care is taken to ensure that the ankle is at the end of the radiolucent table to allow for potential radiographic evaluation. Landmarks are palpated after the ankle is in traction. The skin is marked just medial to the anterior tibial tendon at the level of the ankle in preparation for the anteromedial portal. An 18-gauge needle is used to insufflate the ankle with saline solution through the planned anteromedial portal. Insufflation allows the surgeon to verify the portal location and to protect the articular cartilage at the time of trocar placement. Once the location is verified, a small incision is made in the skin and a blunt trocar is used to enter the capsule. Return of saline solution through the trocar verifies the position of the trocar. A Stryker CrossFlow arthroscopy pump is used for continuous insufflation of the joint during arthroscopy. A Stryker arthroscopy camera is used for arthroscopic visualization of the ankle joint. A lateral portal can then be made under direct visualization with transillumination. The surgeon should ensure that the lateral portal is placed just anterior to the syndesmosis to allow access to the syndesmosis with a graduated probe and shaver.
A diagnostic arthroscopy is then performed in the usual fashion. The syndesmosis can be visualized through the medial portal. A congruent syndesmosis will have cartilaginous articulation of the fibula (Fig 1). If there is significant synovitis blocking visualization (Video 1), this can be debrided with a small shaver (Fig 2). We use the Stryker Aggressive Plus 3.5-mm shaver. The anterior-inferior tibiofibular ligament (Fig 3) and posterior-inferior tibiofibular ligament (Fig 4) are easily seen during most routine ankle arthroscopies.
Fig 1.
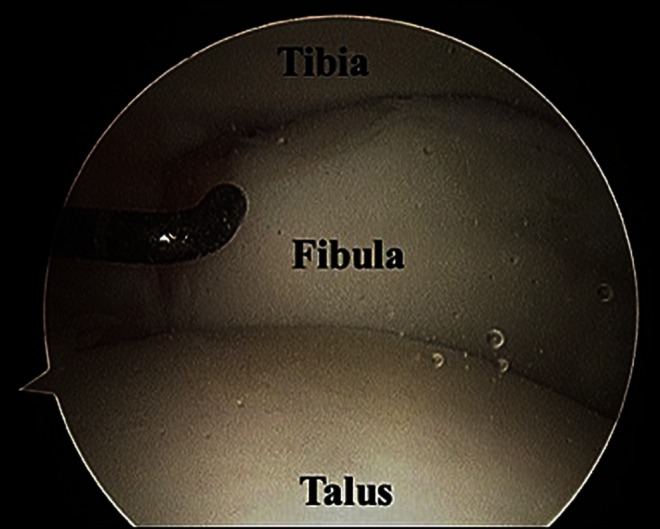
The syndesmosis of the ankle can be visualized through an anteromedial portal, which is made at the level of the ankle joint just medial to the anterior tibial tendon. The probe points to the articulation of the fibula and tibia. The matching curvature of the 2 articular surfaces should be noted.
Fig 2.
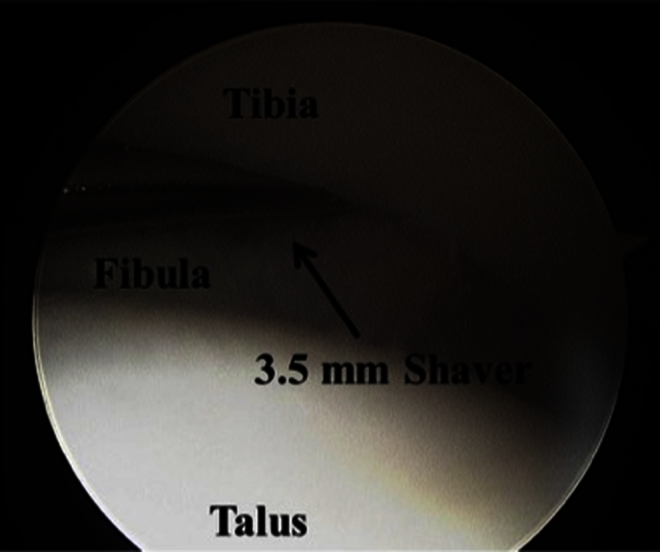
Synovitis within the syndesmosis of the ankle can make it difficult to visualize the degree of diastasis and to obtain adequate reduction. This can be accomplished by performing an external rotation stress test to open the joint and then using a 3.5-mm shaver, inserted through a lateral portal, to debride the synovitis.
Fig 3.
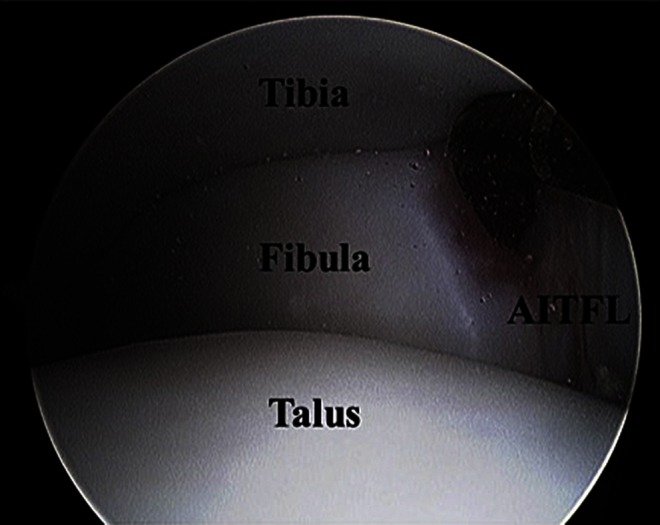
The anterior-inferior tibiofibular ligament (AITFL) in this left ankle is well visualized through the anteromedial portal. This normal-appearing ligament can be probed with a calibrated probe. Intact ligaments, in addition to a reduced and congruent syndesmosis, are signs of a stable ankle.
Fig 4.
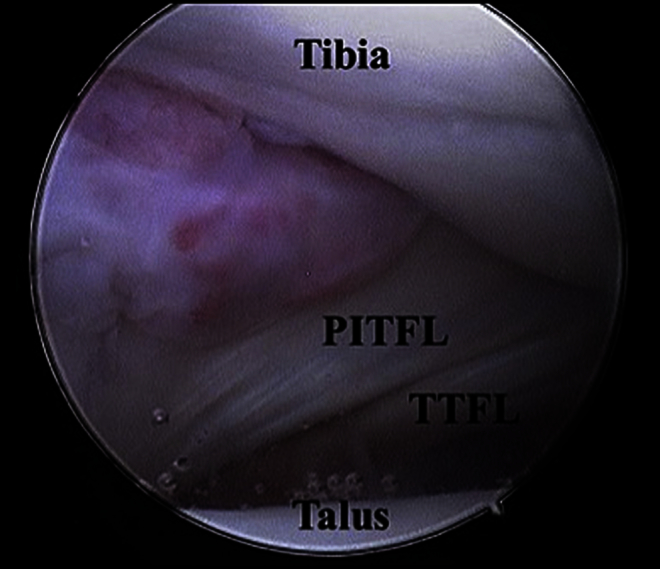
The posterior-inferior tibiofibular ligament (PITFL) provides most of the strength of the syndesmosis. This normal-appearing PITFL and the transverse tibiofibular ligament (TTFL) in the posterior aspect of the syndesmosis are seen during diagnostic arthroscopy. The synovium seen in the recess between the posterior aspect of the fibula and the PITFL is a normal finding.
Evaluation of the syndesmosis can then be performed. A probe can be used to measure any initial diastasis. An external rotation stress test can be performed under arthroscopic visualization with the ankle in the distractor by rotating the dorsiflexed forefoot laterally (Video 1). Any diastasis under stress should be measured using the graduated probe (Fig 5). If there is diastasis but synovitis prevents measurement, an additional debridement within the syndesmosis can be performed with the ankle stressed. After the external stress test, a fibular shuck test is performed. In patients with an average body habitus, the fibula can be grasped with the surgeon's hand and translated anteriorly and posteriorly. This translation can also be measured.
Fig 5.
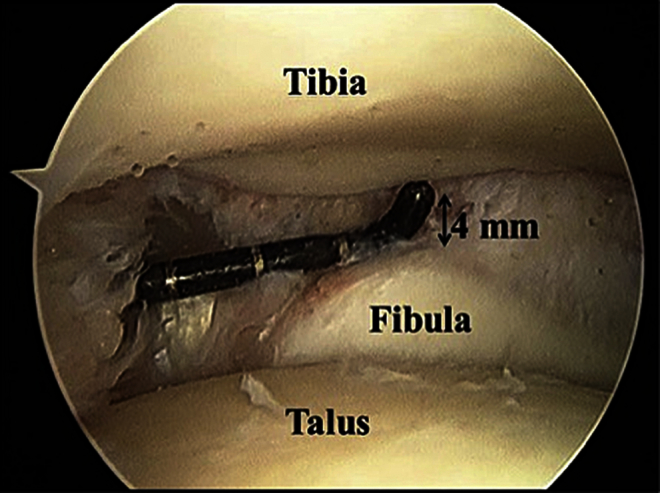
Direct visualization of the syndesmosis during arthroscopy can demonstrate syndesmotic injury not seen on radiographs. Using the calibrated probe, the degree of diastasis can be measured, which can guide the decision for fixation.
Once the diagnosis is made, treatment is tailored to the degree of instability. Patients in whom the syndesmosis sits reduced and has less than 4 mm of diastasis or translation when measured with the graduated probe are treated with debridement alone. Patients with at least 4 mm of translation or diastasis are treated with reduction and stabilization. Typically, the reduction can be performed with manual translation of the fibula while the ankle is held in internal rotation. In some cases, a medial translation has to be performed because of diastasis. An incision is made over the distal fibula for direct visualization of the start point for the Kirschner wires and drill. The reduction is then held with a K-wire. Care should be taken to place the wire in the correct orientation but not in a location where planned syndesmotic fixation will occur (Fig 6). If residual diastasis is seen, a clamp can be used to reduce the syndesmosis in line with the reduction wire (Fig 7). Reduction can be re-evaluated arthroscopically by directly visualizing the syndesmosis through the anteromedial port and again performing an external rotation stress test or fibular shuck test (Video 1).
Fig 6.

K-wires are placed to hold the reduction of the syndesmosis before definitive fixation. It is important that the 2 K-wires be placed slightly divergent in the sagittal plane to provide rotational control. The K-wires should also be placed parallel to the joint, as shown.
Fig 7.
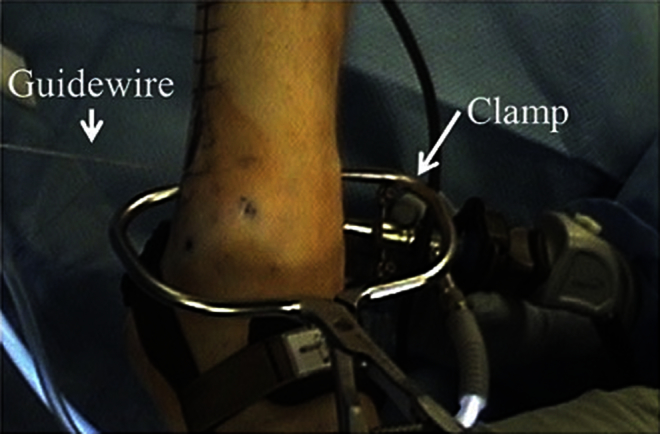
If reduction of an unstable syndesmosis cannot be achieved with a K-wire and manual pressure alone, a reduction clamp can be applied to achieve and maintain reduction while definitive fixation is placed. It is important that the clamp be collinear with the planned suture buttons, as shown.
Once an anatomic reduction is obtained, stabilization can proceed. A suture button can be passed in line with the joint. This is performed by first using a 3.5-mm drill bit to drill through all 4 cortices in the transmalleolar plane 1.5 cm above the ankle joint. We prefer to use a solid drill because it better allows for tactile feedback regarding 4-cortical penetration (Fig 8). The Arthrex TightRope Syndesmosis fixation is then passed through the predrilled hole using a leading needle attached to the suture button with FiberWire (Arthrex) (Video 1, Fig 9). When passing the suture button, we recommend that a single C-arm image be taken to ensure that the suture button has passed through the medial cortex because we have had the leading edge become entrapped within cancellous bone if the button is turned prior to complete passage. In addition, if the medial button is not sitting flush on bone, we recommend a small medial incision to ensure that the saphenous nerve is not constrained by the button (Fig 10). Once the medial side is set, the lateral side can be tensioned by pulling on the 2 sutures emerging from the lateral button (Video 1). The construct is secured by placing 3 half-hitches and cutting the suture. Knotless TightRopes are also available and are self-securing. If the guidewires or K-wires have been placed outside of the planned second button, they can be left in place, but in some cases we will remove one guidewire to facilitate proper fixation placement. The second fixation device is placed 1 cm above the first and slightly divergent in the sagittal plane but should be relatively parallel in the coronal plane (Fig 11). At this point, the second fixation is tensioned and the K-wires can be removed. The joint is re-evaluated arthroscopically to ensure a stable reduction (Video 1). If a rare, third fixation device is required, we have found that bringing this device closer to the joint aids in stability. Although we have observed a syndesmosis overconstrained with screws placed too proximal to the syndesmosis (this results in a valgus ankle), we have not observed the same occurrence with the suture button devices close to the joint. The skin can then be closed and dressed and the ankle placed in a temporary plaster slab splint. Indications, pearls, pitfalls, and key points are listed in Table 1.
Fig 8.

After reduction has been maintained, definitive fixation is accomplished with the Arthrex TightRope construct. Holes are predrilled using a 3.5-mm drill bit, ensuring four-cortical penetration. Ideally, the K-wires should be placed in a location that would not interfere with drilling.
Fig 9.

The Arthrex TightRope Syndesmosis fixation is passed through the predrilled holes in the bone with the guide needle passing through the skin. A small incision can be made on the medial side to directly visualize the medial button and ensure that the saphenous nerve is not entrapped.
Fig 10.

When the surgeon is passing the suture button for definitive fixation, it is important to use C-arm imaging. By doing so, he or she can ensure that the button has passed completely through the bone because it can become caught in cancellous bone, as well as ensure that the button is sitting flush against the bone.
Fig 11.

When suture buttons are used for definitive fixation, it is important that they be parallel to the joint line in the coronal plane. As shown on this postoperative radiograph, the TightRopes are slightly divergent in the sagittal plane, providing additional support.
Table 1.
Indications, Pearls, Pitfalls, and Key Points
| Indications |
| Syndesmotic injury (without fracture) with chronic complaint of instability, not readily visible on radiographs |
| Syndesmotic injury refractory to conservative management |
| Syndesmotic injury (with fracture) that remains unstable after fixation of fracture |
| Pearl |
| If a 3.5-mm shaver fits within the syndesmosis for debridement, the diastasis is likely significant enough to warrant fixation. |
| Pitfall |
| C-arm imaging should always be used to ensure that the suture button passes through the medial cortex and rests flush against the bone. |
| Key point |
| The TightRope technique does not require a second operation for removal as compared with the traditional syndesmotic screw. |
Discussion
Studies related to treatment of latent syndesmotic instability are fairly scarce. When fixation has been used in the literature, techniques typically have included temporary screws as a means of stabilization or autograft tendons for reconstruction. Two of the larger studies on subtle syndesmotic injuries favored arthroscopic debridement alone without stabilization. Ogilvie-Harris and Reed5 retrospectively evaluated 19 patients with chronic syndesmotic instability who were found to have greater than 2 mm of diastasis on arthroscopy. These patients were treated solely with debridement of the involved ligaments (interosseous ligament and posterior-inferior tibiofibular ligament) and chondral lesions. Subjective improvements in pain and function were noted in all patients. Similarly, Han et al.3 showed success using debridement alone when they compared arthroscopic debridement versus debridement combined with screw fixation. Because no significant difference was found between the 2 treatment methods, they recommended debridement alone.
Other authors have found that debridement alone is not universally successful. Morris et al.4 looked at 6 patients with chronic instability that had previously been diagnosed and treated arthroscopically with debridement alone. Because of continued symptoms, these patients underwent reconstruction of the interosseous ligament and anterior tibiofibular ligament with a semitendinosus autograft. The authors found improvements in pain as well as American Orthopaedic Foot & Ankle Society, Short Form 36, and Maryland foot scores, showing that reduction and repair in some circumstances are superior to arthroscopic debridement alone.
We agree that there are circumstances in which debridement alone is sufficient. Generally, if the syndesmosis sits reduced arthroscopically and translates less than 4 mm with external rotation or shuck testing, we will simply debride the reactive synovitis. Without screw fixation of the syndesmosis, we believe that it is difficult to make 2 mm of diastasis better while allowing for anatomic motion. With that said, we believe that there is a role for stabilization in those cases in which the macromotion of the syndesmosis may cause recurrent impingement or symptoms of instability (Fig 12). The technique described in this report allows the surgeon an option for the treatment of subtle syndesmotic injuries that may require stabilization after debridement. The use of the TightRope construct in stabilization has the advantage of not routinely needing to be removed, in contrast to the traditional syndesmotic screw. It also eliminates other complications of screw fixation such as broken hardware. The risks of this procedure are few, but most notably, care should be taken not to entrap the saphenous nerve with the medial button. Overall, we have found the TightRope construct to be easy to apply with good results in reduction of pain and increased stability. In summary, arthroscopic debridement and percutaneous stabilization of chronic subtle syndesmotic injuries have allowed us to treat moderate degrees of instability in a minimally invasive fashion.
Fig 12.
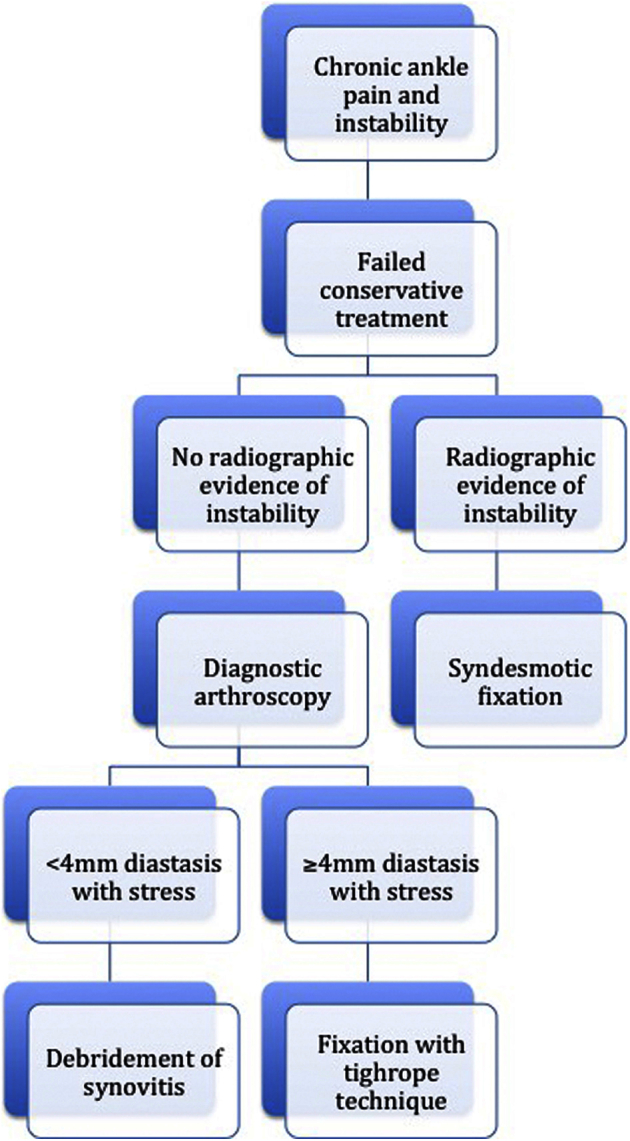
The treatment algorithm for our technique is similar to that for a high ankle sprain. Diagnostic arthroscopy is indicated when radiographic evidence of syndesmotic injury is not apparent and conservative management has failed.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
A subtle syndesmotic injury not visualized on radiographs can be evaluated using diagnostic arthroscopy to directly visualize the syndesmosis under stress. When arthroscopic evaluation shows an unstable syndesmosis with significant diastasis, reduction can be accomplished through debridement and application of an external clamp. Definitive fixation through the use of a TightRope–suture button construct has proved effective.
References
- 1.Grass R., Rammelt S., Biewener A., Zwipp H. Peroneus longus ligamentoplasty for chronic instability of the distal tibiofibular syndesmosis. Foot Ankle Int. 2003;24:392–397. doi: 10.1177/107110070302400503. [DOI] [PubMed] [Google Scholar]
- 2.Ramsey P.L., Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am. 1976;58:356–357. [PubMed] [Google Scholar]
- 3.Han S.H., Lee J.W., Kim S., Suh J.S., Choi Y.R. Chronic tibiofibular syndesmosis injury: The diagnostic efficiency of magnetic resonance imaging and comparative analysis of operative treatment. Foot Ankle Int. 2007;28:336–342. doi: 10.3113/FAI.2007.0336. [DOI] [PubMed] [Google Scholar]
- 4.Morris M.W., Rice P., Schneider T.E. Distal tibiofibular syndesmosis reconstruction using a free hamstring autograft. Foot Ankle Int. 2009;30:506–511. doi: 10.3113/FAI.2009.0506. [DOI] [PubMed] [Google Scholar]
- 5.Ogilvie-Harris D.J., Reed S.C. Disruption of the ankle syndesmosis: Diagnosis and treatment by arthroscopic surgery. Arthroscopy. 1994;10:561–568. doi: 10.1016/s0749-8063(05)80015-5. [DOI] [PubMed] [Google Scholar]
- 6.Zamzami M.M., Zamzam M.M. Chronic isolated distal tibiofibular syndesmotic disruption: Diagnosis and management. Foot Ankle Surg. 2009;15:14–19. doi: 10.1016/j.fas.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Olson K.M., Dairyko G.H., Toolan B.C. Salvage of chronic instability of the syndesmosis with distal tibiofibular arthrodesis. J Bone Joint Surg Am. 2011;93:66–72. doi: 10.2106/JBJS.J.00030. [DOI] [PubMed] [Google Scholar]
- 8.Rammelt S., Zwipp H., Grass R. Injuries to the distal tibiofibular syndesmosis: An evidence-based approach to acute and chronic lesions. Foot Ankle Clin. 2008;13:611–633. doi: 10.1016/j.fcl.2008.08.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A subtle syndesmotic injury not visualized on radiographs can be evaluated using diagnostic arthroscopy to directly visualize the syndesmosis under stress. When arthroscopic evaluation shows an unstable syndesmosis with significant diastasis, reduction can be accomplished through debridement and application of an external clamp. Definitive fixation through the use of a TightRope–suture button construct has proved effective.


