Abstract
An acute perilunate wrist injury that is unreduced for more than 6 weeks results in severe disability, and even open reduction with stabilization through wide dorsal and volar approaches is technically challenging. This report describes an arthroscopic technique for reduction and percutaneous wire stabilization of a chronic perilunate wrist dislocations. The technique involves initial radiocarpal and midcarpal access through the 6R and 3-4 portals, and these portals are used for synovectomy and debridement of capsular flap tears. The midcarpal joint is accessed initially through the radiocarpal joint, and additional midcarpal portals are used for sequential perilunate adhesiolysis before carpal mobilization and reduction. A percutaneous wire drilled into the lunate is used as a joystick to manipulate the lunate into its anatomic alignment along the carpal bones, and percutaneous transcarpal wire fixation is performed to stabilize the carpus. Arthroscopic and fluoroscopic guidance is used to optimize anatomic reduction and to confirm stability. The wrist is immobilized for 6 weeks; the percutaneous wires are removed thereafter, and the wrist is mobilized. Overall, the arthroscopic technique provides a safe and reproducible method for treatment of this complex chronic injury.
Perilunate dislocation of the wrist is a severe and disabling injury that involves complete separation of the midcarpal articulation and loss of contact between the lunate and capitate.1 Perilunate injuries necessitate urgent emergency reduction and stabilization to prevent late complications such as avascular necrosis, chronic instability, and arthritis.2 Acute perilunate injuries may be misdiagnosed and treated conservatively in 25% of cases; an acute injury that is unreduced for more than 6 weeks results in a unique situation of a chronic perilunate dislocation.3, 4 Chronic perilunate injuries are extremely difficult to treat and are associated with a less favorable prognosis; closed reduction after 6 weeks is impossible, and even open reduction with stabilization through wide dorsal and volar approaches is technically challenging.5, 6
The role of arthroscopy in the treatment of acute perilunate wrist injuries has been evaluated; however, arthroscopic management of chronic injuries has not been described previously.7, 8, 9 This report describes an arthroscopic technique for reduction and percutaneous stabilization of a chronic perilunate wrist dislocation. The arthroscopic pathoanatomy and sequential steps of perilunate adhesiolysis are demonstrated, and reduction maneuvers prior to percutaneous wire transfixation are described.
Technique
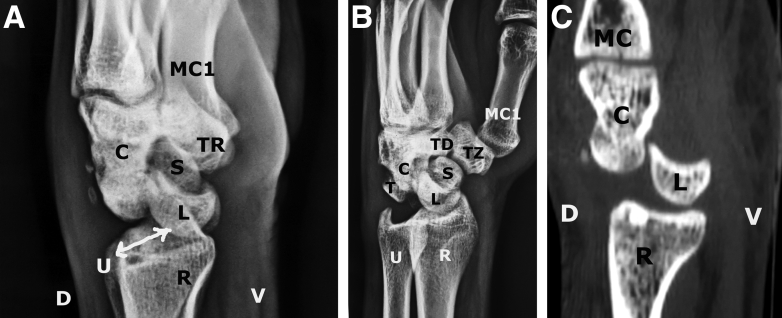
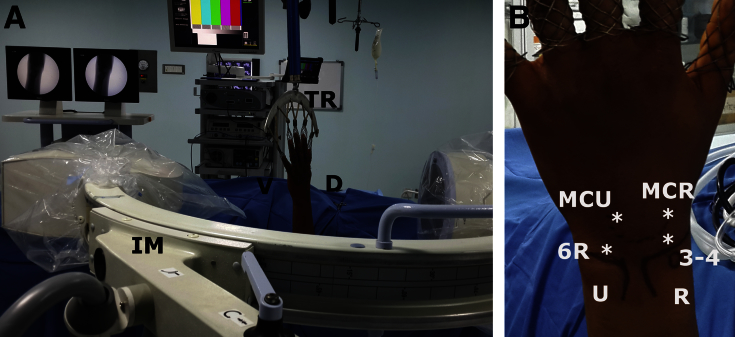
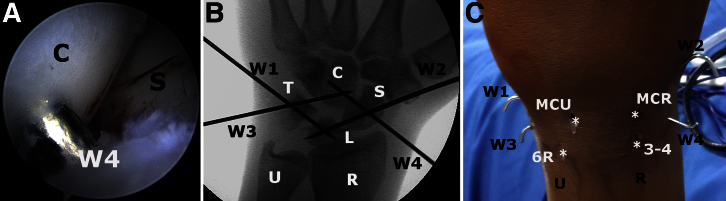
Preoperative imaging is studied, and the perilunate injury is assessed; the position of the lunate is noted, and any associated fractures are identified (Fig 1).1 The procedure is performed with the patient in the supine position; the shoulder is abducted to 90° and the elbow flexed 90°. The upper limb is suspended with Chinese finger traps (5 digits), and a countertraction force of 2 to 4 kg is used to distract the joint. Four dorsal wrist arthroscopy portals are marked (3-4 and 6R radiocarpal portals and midcarpal radial [MCR] and midcarpal ulnar [MCU] portals), and 30° arthroscopes (1.9 mm × 65 mm and 2.4 mm × 75 mm; Arthrex, Naples, FL) are used for radiocarpal and midcarpal arthroscopy (Fig 2). The key steps and surgical pearls of the technique are summarized in Table 1, Table 2, and the steps are demonstrated in Video 1.
Fig 1.
Radiologic imaging of a chronic (8 weeks) perilunate dislocation. (A) Lateral radiograph of left wrist. The capitate (C) and the rest of the carpus are dislocated dorsal to the lunate (L). The lunate is in palmar flexion toward the volar aspect of the radiocarpal articulation, and most of the lunate fossa is empty (arrow). (D, dorsal; MC1, first metacarpal; R, radius; S, scaphoid; TR, trapezium; U, ulna; V, volar.) (B) Oblique radiograph of left wrist. The scapho-trapezio-trapezoid joint (S-TZ-TD) can be evaluated. The lunate (L) is not displaced beyond the volar lip of the radius (R), and the scaphoid and capitate can be evaluated for any associated fractures. (C, capitate; MC1, first metacarpal; T, triquetrum; TR, trapezium; U, ulna.) (C) Computed tomography scan of the left wrist confirms the palmar angulation and displacement of the lunate (L) up to the volar lip of the distal radius (R); however, there is no lunate dislocation. The capitate (C) is seen dislocated dorsal (D) to the lunate. The radiocarpal space between the radius and the carpus (C, L) is empty and eventually fills up with scar tissue and fibrosis. (MC, metacarpal; V, volar.)
Fig 2.
(A) The patient is positioned supine; the upper limb is suspended with Chinese finger traps (TR) on all 5 digits, and a countertraction force of 2 to 4 kg is used. This uniform traction assists in reduction of the carpal bones after adhesiolysis. Fluoroscopy (IM) is used during the procedure to confirm reduction and for percutaneous wire passage. (D, dorsal; V, volar.) (B) Wrist arthroscopy portals (asterisks) used in technique (left wrist). The 6R portal is the radiocarpal viewing portal, and the 3-4 portal is the radiocarpal working portal. Standard midcarpal radial (MCR) and midcarpal ulnar (MCU) portals are placed by an outside-in technique and are used for midcarpal viewing (MCR) and adhesiolysis (MCU). An additional scapho-trapezio-trapezoid portal may be necessary for adhesiolysis within the scapho-trapezio-trapezoid joint. (R, radius; U, ulna.)
Table 1.
Key Steps of Procedure
| Correct upper limb positioning is important; the wrist is suspended with finger traps on all digits for uniform distribution of countertraction force across the wrist. |
| Diagnostic arthroscopy performed through the 3-4 viewing portal is difficult because of malrotation of the scaphoid; a 6R portal is useful for end-on visualization of the scaphoid, and the entire radiocarpal space is evaluated. Preliminary evaluation of the midcarpal space is also performed using the 6R viewing portal. |
| Radiocarpal adhesiolysis is performed through the 6R viewing and 3-4 working portals. |
| Midcarpal evaluation and adhesiolysis are performed through the midcarpal radial viewing portal and the midcarpal ulnar working portal. A scapho-trapezio-trapezoid portal may be used for adhesiolysis within the scapho-trapezio-trapezoid joint. |
| Perilunate adhesiolysis is performed sequentially before lunate reduction. Lunate fossa fibrosis is cleared, and the scapholunate and lunotriquetral surfaces are debrided. |
| A wire is drilled into the lunate and is used as a joystick to manipulate it into dorsiflexion. Capitate coverage is obtained by repositioning the lunate into its anatomic position. |
| Percutaneous transfixation wires are passed, under fluoroscopic guidance, to stabilize the unstable reduction. |
| A brace is worn for 6 wk in the postoperative period; alternately, a volar plaster slab may be applied. The wires are removed under local anesthesia after 6 wk, and mobilization is permitted. |
Table 2.
Technical Pearls for Key Steps of Procedure
| Steps | Pearls |
|---|---|
| Portals and visualization | The 6R portal is the main viewing portal for radiocarpal arthroscopy, and the MCR portal is the viewing portal for the midcarpal space. The midcarpal space is difficult to access directly. The midcarpal joint should be visualized first through the 6R portal, and the correct position of the MCR portal is determined by an outside-in technique. Gross derangement of internal anatomic relations permits midcarpal viewing through the 6R portal. A 2.4-mm 30° arthroscope is used for radiocarpal and midcarpal evaluation and provides good visualization. A 1.9-mm arthroscope is useful prior to adhesiolysis within the midcarpal space. A countertraction force of 2 to 4 kg provides an adequate working space for initial clearance. Once access is obtained, the countertraction weight is reduced. |
| Adhesiolysis | Radiocarpal adhesiolysis and preliminary midcarpal adhesiolysis are necessary for lunate identification. Perilunate adhesiolysis is performed in 5 zones (midcarpal, scapholunate, dorsal midcarpal, lunate fossa, and radiocarpal) before lunate reduction. The lunate cannot be reduced anatomically without this release. |
| Perilunate reduction | Correct alignment of the carpal bones is determined by assessing (1) lunotriquetral and scapholunate reduction, (2) capitate coverage by the lunate, and (3) lunate dorsiflexion. These 3 parameters are assessed arthroscopically and confirmed under fluoroscopic guidance. The maneuvers for perilunate reduction include (1) lunate joystick wire for dorsiflexion, (2) lunate dorsal translation, and (3) traction on the volar ligaments. |
| Percutaneous transfixation wire fixation | Lunotriquetral and scapholunate transfixation is performed first. Correct alignment is confirmed on arthroscopy and fluoroscopy. Scapho-capitate and triquetro-capitate transfixation is necessary in chronic perilunate injuries to stabilize the midcarpal articulation. The wires are passed in a diamond-shaped configuration, as shown in Figure 10. The wires are pulled out after 6 to 7 wk. Intermittent radiographs are obtained to confirm alignment of the wrist. |
MCR, midcarpal radial.
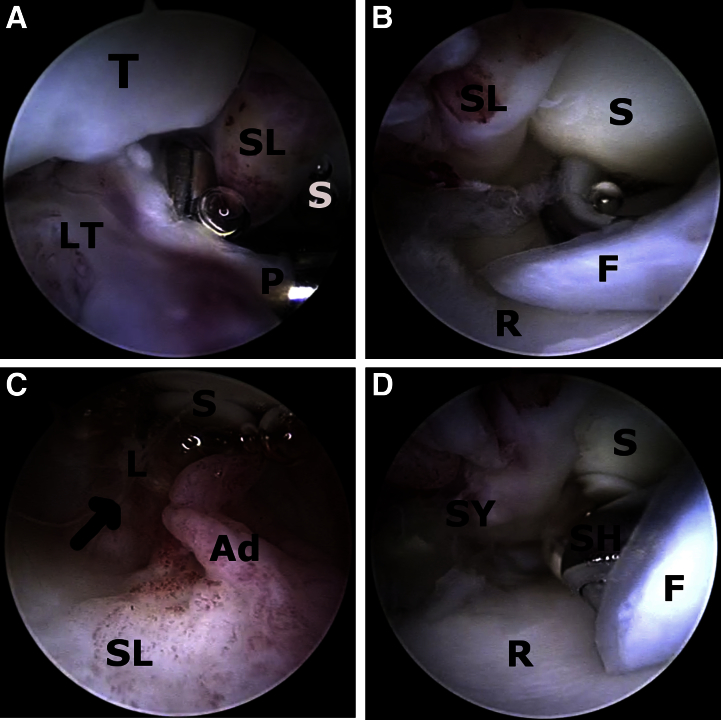
Step 1: Diagnostic Radiocarpal Arthroscopy
The 6R and 3-4 radiocarpal portals are placed; diagnostic arthroscopy is performed using the 6R portal as the viewing portal (Fig 2B). The triquetrum and scaphoid are identified, and the torn scapholunate and lunotriquetral ligaments are seen; the lunate is displaced volarly and is ensheathed in the fibrous scar tissue that occupies the lunate fossa. The position of the lunate is confirmed by palpating with a probe in the interval between the scaphoid and the triquetrum. Dorsal capsular flap tears and synovitis prevent adequate visualization through the 3-4 portal (Figs 3 A-C).
Fig 3.
(A) Diagnostic radiocarpal arthroscopy of left wrist. The arthroscope is placed in the 6R portal and is positioned in the lunate fossa. The triquetrum (T) is visualized and probed (P) at the ulnar aspect of the joint, and the scaphoid (S) is toward the radial side. The lunate is not visualized at its usual position, and the scarred scapholunate (SL) and lunotriquetral (LT) ligaments are seen occupying the lunate fossa. (B) Diagnostic radiocarpal arthroscopy of left wrist. The arthroscope is placed in the 6R portal and is positioned in the lunate fossa. The scaphoid (S) along with the torn scapholunate ligament (SL) is visualized. Large flap tears (F) of the dorsal capsule are seen overlying the radius articular surface (R). (C) Diagnostic radiocarpal arthroscopy of left wrist. The arthroscope is placed in the 6R portal and is positioned in the volar aspect of the lunate fossa between the scaphoid (S) and triquetrum (not shown here). The scarred scapholunate ligament (SL) and lunate fossa adhesions (Ad) prevent visualization of the lunate (L, arrow). (D) Radiocarpal arthroscopy of left wrist. The arthroscope is placed in the 6R portal and is positioned in the lunate fossa. A 3-mm shaver (SH) is placed in the 3-4 portal and is used to debride the flap tears (F) and the synovitis (SY) until the radius articular surface is clearly visualized (R). (S, scaphoid.)
Step 2: Radiocarpal Adhesiolysis
A 3-mm shaver (Sabre; Arthrex) is introduced into the radiocarpal joint through the 3-4 portal. Radiocarpal adhesions are excised, and a thorough synovectomy is performed. Dorsal capsular flap tears are seen interposed within the joint and are debrided. The triangular fibrocartilage complex is evaluated; any triangular fibrocartilage complex tears are debrided at this stage, and a synovectomy is performed (Fig 3D).
Step 3: Midcarpal Access
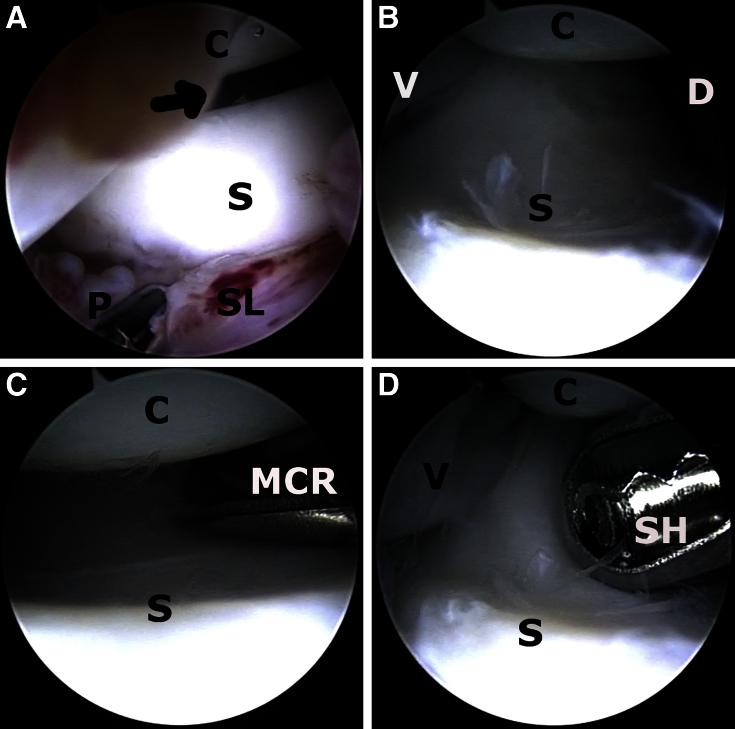
The midcarpal joint is initially visualized through the 6R portal; this permits an ulnar-to-radial end-on view of the midcarpal joint and is possible because the lunate is not in its anatomic position. The MCR portal is now placed with an outside-in technique. A 3-mm shaver (Sabre) is passed through this portal, and preliminary midcarpal clearance is performed (Fig 4).
Fig 4.
Preliminary midcarpal access shown in a left wrist. (A) The arthroscope is placed in the 6R portal, and the scaphoid (S) is dorsiflexed by pulling down on the scaphoid attachment of the scapholunate ligament (SL) using a probe (P). This maneuver opens up the scapho-capitate joint (arrow). (C, capitate.) (B) The 6R portal provides an end-on view of the scaphoid (S) midcarpal surface. The displaced lunate and the dorsiflexed scaphoid permit this access. (C, capitate; D, dorsal aspect; V, volar aspect.) (C) The midcarpal radial (MCR) portal is created using a needle passed with an outside-in technique. The needle is parallel to the scaphoid surface and should permit access to the radial and ulnar aspects of the scapho-capitate joint (S-C). (D) Preliminary clearance of the scapho-capitate joint is performed using a 3-mm shaver (SH) in the MCR portal. This permits excision of any adhesions before midcarpal arthroscopy through the MCR portal. (C, capitate; S, scaphoid; V, volar aspect.)
Step 4: Midcarpal Arthroscopy and Adhesiolysis
The arthroscope is placed in the MCR portal, and the midcarpal joint is evaluated. The scapho-trapezio-trapezoid joint is evaluated for congruity and adhesions. The scapho-capitate joint is followed to the lunate fossa and triquetrum. The volar aspect of the lunate fossa shows the palmar flexed lunate and the torn volar ligaments. Cartilage defects over the lunate and capitate are identified and documented (Fig 5). A standard ulnar midcarpal portal (MCU) is now placed using an outside-in technique, and a 3-mm shaver (Sabre) is used to sequentially debride the perilunate adhesions and lunate fossa fibrosis. The debridement starts with clearance of the lunate midcarpal surface and proceeds to the scapholunate and dorsal midcarpal adhesions. Thereafter the lunate fossa is cleared, and the radiocarpal surface of the lunate can be accessed and debrided (Fig 6). Complete perilunate release is necessary to reduce the lunate back to its anatomic position.
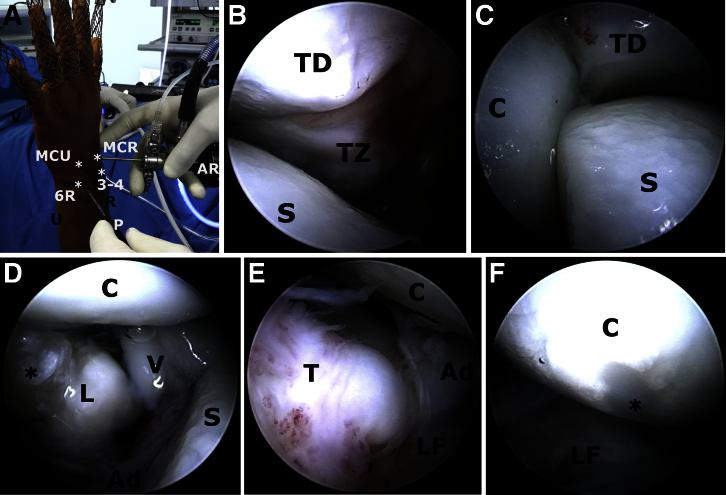
Fig 5.
Midcarpal arthroscopy through the midcarpal radial (MCR) viewing portal in a left wrist. (A) The MCR portal is used as a viewing portal for the remainder of the procedure. The midcarpal ulnar (MCU) portal and the 6R portal are used as working portals. Asterisks indicate portal placement. (AR, arthroscope; D, dorsal aspect; P, probe; R, radius; U, ulna; V, volar aspect.) (B, C) The scapho-trapezio-trapezoid joint is evaluated for adhesions, and any scarring in this region is excised through an additional portal (not shown). (C, capitate; S, scaphoid; TD, trapezoid; TZ, trapezium.) (D) The scapho-capitate joint is followed down to the lunate fossa. The lunate (L) is seen displaced volarly through a tear in the volar ligaments (V) and is in palmar flexion. The cartilage defect (asterisk) on the dorsal aspect of the lunate results from avulsion of the attached ligaments on this surface. Adhesions (Ad) in the lunate fossa prevent reduction of the lunate at this stage. (C, capitate; S, scaphoid.) (E) The ulnar aspect of the lunate fossa shows an unstable triquetrum (T). Adhesions (Ad) and remnants of torn ligaments are seen scarred in the lunate fossa (LF). (C, capitate.) (F) The proximal capitate (C) is evaluated for cartilage defects (asterisk) that may have occurred during the capito-lunate dissociation. (LF, lunate fossa.)
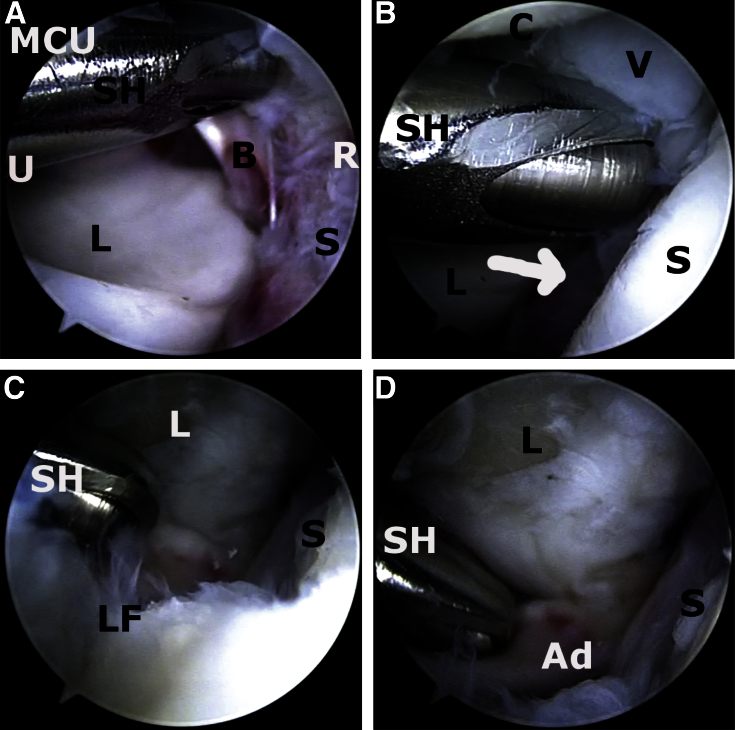
Fig 6.
Sequential midcarpal adhesiolysis in a left wrist (midcarpal radial viewing portal). (A) The 3-mm shaver (SH) is used through the midcarpal ulnar (MCU) portal to excise adhesions along the midcarpal articular surface (L) and the volar surface of the lunate. Scapholunate adhesions (S) are visualized along the radial (R) aspect of the field. Small bony avulsions (B) are seen adherent to the volar ligaments and are excised before reduction. (U, ulnar.) (B) Scapholunate adhesions are excised next, and a 3-mm shaver (SH) is inserted in the interval (arrow) between the scaphoid (S) and lunate (L). (C, capitate; V, volar ligaments.) (C) The dorsal midcarpal adhesions and the lunate fossa adhesions (LF) are excised to clear the lunate fossa before lunate reduction and dorsiflexion. (L, lunate; S, scaphoid; SH, shaver.) (D) Inferior radiocarpal surface adhesions (Ad) are excised last. One should note that the scaphoid (S) and lunate (L) are now clearly visualized, and the lunate fossa is visible. (SH, shaver.)
Step 5: Lunate Reduction and Stabilization
A 1.5-mm guidewire is drilled percutaneously or through the MCU portal into the lunate and is confirmed with fluoroscopy. The lunate wire is used as a joystick to control lunate flexion, and the lunate is gently dorsiflexed. Dorsal traction is used to pull the lunate into the lunate fossa, and capitate coverage is achieved. A percutaneous wire is now drilled, under fluoroscopic guidance, from the ulnar aspect, and transfixation of the lunotriquetral joint is achieved (Fig 7). Next, the lunate is reduced to the scaphoid; a grasper is used to grasp the volar ligaments through the MCU portal, and dorsal traction approximates the scapholunate joint. A percutaneous wire is now drilled, under fluoroscopic guidance, from the radial aspect, and transfixation of the scapholunate joint is achieved (Fig 8). Further stabilization is achieved by passing scapho-capitate and triquetro-capitate wires using arthroscopic and fluoroscopic guidance. All 4 percutaneous wires are bent and cut short outside the joint, and the portals are closed (Fig 9).
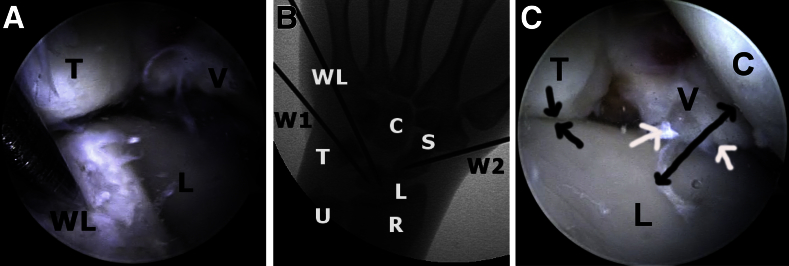
Fig 7.
Lunate reduction and fluoroscopy-guided lunotriquetral percutaneous wire transfixation (left wrist, midcarpal radial viewing portal). (A) A wire (WL) is drilled into the lunate (L) and is used as a joystick to manipulate the lunate into dorsiflexion. Additional dorsal traction on the wire aligns the lunate with the triquetrum (T). (V, volar ligaments.) (B) An image intensifier is used to drill a lunotriquetral transfixing wire (W1) while the lunate (L) and triquetrum (T) are held reduced by the lunate wire (WL). A second wire (W2) is placed across the scaphoid and will eventually be drilled to transfix the scaphoid (S) and lunate (L). (C, capitate; R, radius; U, ulna.) (C) Arthroscopic view of lunotriquetral approximation (2 arrows). One should note that the lunate (L) is now in its anatomic position, and the capitate (C) is completely covered by the lunate (double headed arrow). The volar ligaments (V) are aligned with the volar aspect of the lunate (white arrows). (T, triquetrum.)
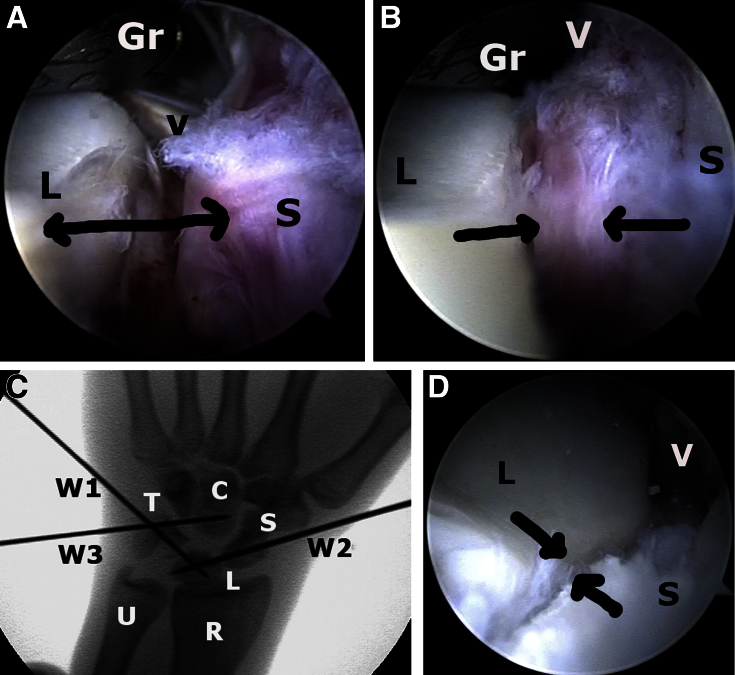
Fig 8.
Scapho-lunate reduction maneuver and fluoroscopy-guided percutaneous wire transfixation (left wrist, midcarpal radial viewing portal). (A) The scaphoid (S) and lunate (L) are displaced away from each other (arrow). The volar ligaments (V) are held with a grasper (Gr) through the midcarpal ulnar portal, and a dorsal force is applied to approximate the 2 bones. (B) The scaphoid (S) and lunate (L) are shown reduced by the grasper (Gr) through the midcarpal ulnar portal. The scapholunate ligament (arrows) is preserved and prevents bony ankylosis of the carpal bones. (V, volar ligaments.) (C) An image intensifier is used to drill a percutaneous scapholunate transfixing wire (W2) while the lunate (L) and scaphoid (S) are held reduced. A third wire (W3) is placed across the luno-capitate joint. (C, capitate; R, radius; T, triquetrum; U, ulna; W1, lunotriquetral wire.) (D) Arthroscopic view of scapholunate approximation (arrows). One should note that the lunate (L) is now in its anatomic position and aligned with the scaphoid (S). The volar ligaments (V) are aligned with the volar aspect of the lunate.
Fig 9.
(A) Arthroscopic view of scapho-capitate transfixation wire (W4). Thin 1.5-mm wires are used for midcarpal transfixation to minimize articular cartilage damage. Arm countertraction is reduced to align the capitate (C) correctly. (S, scaphoid.) (B) Fluoroscopy confirms correct placement of wires to achieve a diamond-shaped percutaneous wire construct. (C, capitate; L, lunate; R, radius; S, scaphoid; T, triquetrum; U, ulna; W1, triquetro-lunate wire; W2, scapholunate wire; W3, triquetro-capitate wire; W4, scapho-capitate wire.) (C) External view of the percutaneous wires in relation to the 4 portals (asterisks). The percutaneous wires are cut short and bent over to prevent migration. (MCR, midcarpal radial portal; MCU, midcarpal ulnar portal; R, radius; U, ulna; W1, triquetro-lunate wire; W2, scapholunate wire; W3, triquetro-capitate wire; W4, scapho-capitate wire.)
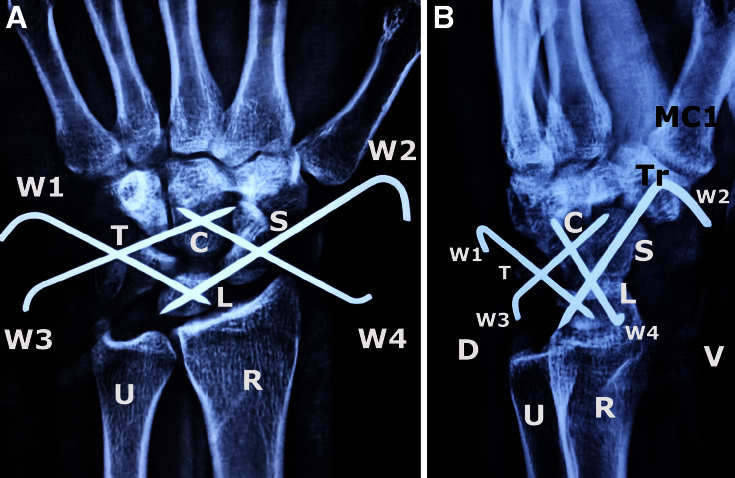
The tourniquet is deflated, and a sterile dressing is applied. A brace (Universal cock-up splint; Vissco, Mumbai, India) is used to maintain the wrist and hand in the functional position of wrist dorsiflexion. Finger movement is encouraged, and the brace is maintained for 6 weeks. Periodic radiographs are obtained to confirm maintenance of reduction (Fig 10). The wires are removed after 6 weeks, and rehabilitation is started. Range of wrist movement is begun at 6 to 7 weeks, and gradual strengthening is continued simultaneously. Activities of daily living are started at 8 weeks, and desk work is permitted after 12 weeks. Return to heavy work and sports is permitted only after 6 months of rehabilitation.
Fig 10.
(A) Anteroposterior radiograph of left wrist at 6 weeks. The carpal alignment is preserved, and none of the wires have migrated. (C, capitate; L, lunate; R, radius; S, scaphoid; T, triquetrum; Tr, trapezium; U, ulna; W1, triquetro-lunate wire; W2, scapholunate wire; W3, triquetro-capitate wire; W4, scapho-capitate wire.) (B) Lateral radiograph of left wrist at 6 weeks. The lunate (L) is in its anatomic position and well aligned to the scaphoid (S) and capitate (C). (D, dorsal; MC1, first metacarpal; R, radius; T, triquetrum; U, ulna; V, volar; W1, triquetro-lunate wire; W2, scapholunate wire; W3, triquetro-capitate wire; W4, scapho-capitate wire.)
Discussion
Acute perilunate injuries may occasionally be missed, and a delayed presentation beyond 6 weeks results in severe fibrosis within the radiocarpal and midcarpal joints. Chronicity of these injuries is associated with a poorer prognosis; however, satisfactory results may be achieved if the carpal cartilage is preserved.4, 7, 8, 9, 10, 11, 12, 13 Various open surgical options have been described for stabilization and salvage of these injuries, and arthroscopic reduction has been performed only in acute injuries.
Arthroscopic management of a chronic perilunate injury is technically difficult because of severe derangement of the midcarpal and radiocarpal arcs. Chronicity results in scarring and fibrosis within the joints, and arthroscopic visualization and identification of pathoanatomy are challenging. Initial diagnostic evaluation of both the radiocarpal and midcarpal joints through radial and ulnar portals is crucial to identify the displacement and orientation of the carpal bones. The displaced lunate is covered with scar tissue, and a meticulous perilunate adhesiolysis is necessary to visualize and mobilize the lunate. Lunate reduction is achieved in a stepwise manner by correction of the flexion angle and approximation of the triquetro-lunate and scapholunate articulations. Fluoroscopic- and arthroscopic-guided percutaneous wire transfixation is used to stabilize the reduction, and a brace is used until soft-tissue healing is sufficient to maintain bony relations.
The described arthroscopic technique can also be used for reduction and stabilization of acute and subacute perilunate injuries. The overall advantages and pitfalls of the procedure are summarized in Table 3.
Table 3.
Advantages and Pitfalls of Technique
| Advantages |
| Arthroscopic reduction is minimally invasive and avoids the necessity for open surgical approaches. |
| Both volar and dorsal structures are well visualized. Adhesions can be identified in various zones, and effective adhesiolysis can be performed systematically in the radiocarpal, midcarpal, and perilunate regions. Additional scapho-trapezio-trapezoid fibrosis can be evaluated and cleared. |
| Correct alignment can be visualized arthroscopically, and optimal wire stabilization may be achieved. |
| Additional synovectomy and debridement of triangular fibrocartilage complex tears can be performed simultaneously. Loose cartilage and bone fragments can be cleared effectively. |
| Pitfalls |
| The procedure is technically challenging because of gross derangement of internal anatomy. Fibrosis and adhesions prevent joint distention and clear visualization. |
| The lunate is displaced volarly and is covered with scar tissue. Careful dissection along the volar and anterior lunate is necessary to prevent neurovascular complications. |
| Inadequate visualization and suboptimal technique may lead to iatrogenic cartilage damage and incorrect alignment of carpal bones. |
| Fluid extravasation into the forearm and a potential increase in compartment pressures are possible. The risk in minimized by using air as an insufflation medium for the initial diagnostic endoscopy. Fluid inflow must be minimized by using syringe inflow instead of gravity inflow or a fluid pump. Compartment pressures may be monitored if the forearm is tense and swollen excessively. |
| Percutaneous wire passage should be performed through safe zones. A tiny skin incision may be used, and blunt dissection down to bone may be used for safe wire passage. Potential neurovascular complications may occur if incorrect technique is used for wire passage. |
| Redislocation is possible if wire stabilization is insufficient. The construct shown in this technique adequately stabilizes the chronic injury. |
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Important steps of the procedure in a 2-month-old contact sport injury. The patient is positioned supine, and the left wrist is suspended using finger traps. Dorsal 3-4 and 6R portals are used for radiocarpal visualization, and adhesiolysis and excision of capsular flap tears are performed. Midcarpal radial and midcarpal ulnar portals are used to visualize the lunate and to perform perilunate adhesiolysis. Thereafter the lunate is reduced into anatomic position. A wire is drilled into the lunate and used as a joystick to manipulate it into dorsiflexion. Traction is applied on the wire to align it with the triquetrum, and a grasper is used to pull the radial aspect of the lunate into alignment with the scaphoid. Percutaneous wires are used to transfix the lunate and the midcarpal joint using fluoroscopic and arthroscopic guidance. Postoperative radiographs confirm correct alignment and maintenance of reduction.
References
- 1.Mayfield J.K., Johnson R.P., Kilcoyne R.K. Carpal dislocations: Pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5:226–241. doi: 10.1016/s0363-5023(80)80007-4. [DOI] [PubMed] [Google Scholar]
- 2.Wilke B., Kakar S. Delayed avascular necrosis and fragmentation of the lunate following perilunate dislocation. Orthopedics. 2015;38:e539–e542. doi: 10.3928/01477447-20150603-92. [DOI] [PubMed] [Google Scholar]
- 3.Herzberg G., Comtet J.J., Linscheid R.L., Amadio P.C., Cooney W.P., Stalder J. Perilunate dislocations and fracture dislocations: A multicenter study. J Hand Surg Am. 1993;18:768–779. doi: 10.1016/0363-5023(93)90041-Z. [DOI] [PubMed] [Google Scholar]
- 4.Kailu L., Zhou X., Fuguo H. Chronic perilunate dislocations treated with open reduction and internal fixation: Results of medium-term follow-up. Int Orthop. 2010;34:1315–1320. doi: 10.1007/s00264-009-0926-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Komurcu M., Kürklü M., Ozturan K.E. Early and delayed treatment of dorsal transscaphoid perilunate fracture-dislocations. J Orthop Trauma. 2008;22:535–540. doi: 10.1097/BOT.0b013e318183eb23. [DOI] [PubMed] [Google Scholar]
- 6.Melone C.P., Murphy M.S., Raskin K.B. Perilunate injuries. Repair by dual dorsal and volar approaches. Hand Clin. 2000;16:439–448. [PubMed] [Google Scholar]
- 7.Kim J.P., Lee J.S., Park M.J. Arthroscopic treatment of perilunate dislocations and fracture dislocations. J Wrist Surg. 2015;4:81–87. doi: 10.1055/s-0035-1550160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu B., Chen S.L., Zhu J., Wang Z.X., Shen J. Arthroscopically assisted mini-invasive management of perilunate dislocations. J Wrist Surg. 2015;4:93–100. doi: 10.1055/s-0035-1550162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herzberg G., Burnier M., Marc A., Merlini L., Izem Y. The role of arthroscopy for treatment of perilunate injuries. J Wrist Surg. 2015;4:101–109. doi: 10.1055/s-0035-1550344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inoue G., Shionoya K. Late treatment of unreduced perilunate dislocations. J Hand Surg Br. 1999;24:221–225. doi: 10.1054/jhsb.1998.0003. [DOI] [PubMed] [Google Scholar]
- 11.Rettig M.E., Raskin K.B. Long-term assessment of proximal row carpectomy for chronic lunate dislocation. J Hand Surg Am. 1999;24:1231–1236. doi: 10.1053/jhsu.1999.1231. [DOI] [PubMed] [Google Scholar]
- 12.Siegert J.J., Frassica F.J., Amadio P.C. Treatment of chronic perilunate dislocations. J Hand Surg Am. 1988;13:206–212. doi: 10.1016/s0363-5023(88)80049-2. [DOI] [PubMed] [Google Scholar]
- 13.Green D.P., O’Brien E.T. Open reduction of carpal dislocations: Indications and operative techniques. J Hand Surg Am. 1978;3:250–265. doi: 10.1016/s0363-5023(78)80089-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Important steps of the procedure in a 2-month-old contact sport injury. The patient is positioned supine, and the left wrist is suspended using finger traps. Dorsal 3-4 and 6R portals are used for radiocarpal visualization, and adhesiolysis and excision of capsular flap tears are performed. Midcarpal radial and midcarpal ulnar portals are used to visualize the lunate and to perform perilunate adhesiolysis. Thereafter the lunate is reduced into anatomic position. A wire is drilled into the lunate and used as a joystick to manipulate it into dorsiflexion. Traction is applied on the wire to align it with the triquetrum, and a grasper is used to pull the radial aspect of the lunate into alignment with the scaphoid. Percutaneous wires are used to transfix the lunate and the midcarpal joint using fluoroscopic and arthroscopic guidance. Postoperative radiographs confirm correct alignment and maintenance of reduction.