Abstract
Background
Recently, vitamin D3 (1alpha, 25-dihydroxyvitamin D) has shown its capability to take part in many extraskeletal functions and its serum levels have been related to patient survival rate and malignancy of many types of neoplasms, including ovarian cancers. Catalytic iron is a free circulating form of iron that is able to generate reactive oxygen species and consequently to promote a number of cellular and tissutal dysfunctions including tumorigenesis. In fertile women an important source of catalytic iron is derived from retrograde menstruation. Epithelial secretory cells from fimbriae of fallopian tubes are greatly exposed to catalytic iron derived from menstrual reflux and so represent the site of origin for most serous ovarian cancers.
The aim of this study was to assess whether vitamin D3 can play a role in counteracting catalytic iron-induced oxidative stress in cells from fimbriae of fallopian tubes.
Methods
The cells, isolated from women undergoing isteroannessiectomy, were treated with catalytic iron 50-75-100 mM and vitamin D3 at a concentration ranging from 0.01 to 10 nM to study cell viability, radical oxygen species production, p53, pan-Ras, Ki67 and c-Myc protein expressions through Western Blot, and immunocytochemistry or immunofluorescence analysis.
Results
The pre-treatment with vitamin D3 1 nM showed its beneficial effects that consists in a significant decrease in ROS production. In addition a novel finding is represented by the demonstration that pre-treatment with vitamin D3 is also able to significantly counteract tumoral biomarkers activation, such as p53, pan-Ras, Ki67 and c-Myc, and consequently the catalytic iron-induced cellular injury.
Conclusions
This study demonstrates for the first time that vitamin D3 plays an important role in preventing catalytic iron-dependent oxidative stress in cultured fimbrial cells. These results support the hypothesis that vitamin D3 could counteract carcinogenic changes induced by catalytic iron.
Keywords: Fimbrial secretory epithelial cells, Catalytic iron, Epithelial ovarian cancer, Vitamin D3
Background
Recently, the role of 1alpha,25-dihydroxyvitamin D (VitD) has greatly expanded from its classical function of modulator of calcium metabolism and skeletal trophism into a number of extraskeletal functions such as nitric oxide production, antioxidant activity and endothelial proliferation and migration [1–3]. Along with its well-known metabolic functions, VitD has recently shown immunomodulatory and anticancer properties as well [4–7]. As a matter of fact, the importance of serum VitD level as a biomarker for cancer risk was first determined by Garland et al. in 1989 [8]. Moreover, Gorham et al. [9] confirmed the relationship between VitD and cancer, showing that an increase in the serum level of VitD to 34 ng/ml was associated with a 50 % reduction in incidence rates of colorectal cancer.
As regards ovarian cancer, it has been observed that serum concentration of VitD was lower in cancer patients than in the reference group (12.5 ± 7.75 ng/mL vs 22.4 ± 6.5 ng/mL) [10]. Moreover, low VitD serum concentration is associated with lower overall survival rate. This fact points out the importance of severe VitD deficiency as a possible cause of highly aggressive ovarian cancer [10]. In addition, VitD treatment suppressed human epithelial ovarian cancer cells migration and invasion in monolayer scratch and transwell assays, as well as the ability to colonize the omentum in an ex vivo experimental model. These findings support a role for epithelial VitD receptor (VDR) in interfering with epithelial ovarian cancer invasion [11]. A recent systematic review states that there is no consistent or strong evidence to support the claim made in numerous review articles that VitD exposure reduces the risk for ovarian cancer occurrence or mortality [12]. However, this declaration is in contrast with several human and cell-based studies which show that VitD can induce growth arrest and apoptosis either of tumor cells or of their non-neoplastic progenitors [13, 14]. In addition, it has been demonstrated that other gene targets related to DNA repair and immunomodulation, as well as other cell targets such as the stromal cells and cells of the immune system, may be regulated by VitD, thus contributing to cancer prevention [15]. The molecular mechanisms leading to cancer prevention exerted by VitD have been extensively studied in the last few years in order to identify a possible new therapeutic strategy. A large number of studies have shown that VitD has important anti-proliferative, anti-angiogenic and pro-differentiative effects in a wide range of cancers. These effects are mediated through perturbation of several important signalling pathways mediated through genomic and non-genomic mechanisms [16]. However these effects have no uniform patterns of modulation by VitD across different types of cancer cell lines. It has been hypothesized that the heterogeneous action of VitD may depend on the differentiation status of the cancer cells and VDR expression level, as well as genomic or post-translational modifications of co-activator proteins that are essential for the assembly of the transcriptionally active VDR complex [17].
Catalytic iron (Fe3+) is a free circulating iron that is not bound to transferrin or ferritin and is known to generate reactive oxygen species that may have noxious effects on cells and tissues. For example, a number of studies show that high levels of Fe3+ may promote atherosclerosis [18], endothelial dysfunction, arterial smooth muscle proliferation and ischemia/reperfusion injury [19, 20]. Blood-deriving Fe3+ can accumulate into tissues and cells where its ability to switch from its ferrous oxidation state into its ferric one reversibly makes it very dangerous since free iron can catalyze the formation of free radicals, which can damage molecular components of the cell [21]. In a chronic condition, high concentrations of heme and free iron (Fe3+) derived from lysis of red blood cells by macrophages are able to exceed the capacity of ferritin to sequester iron leading to oxidative injury. This mechanism generates oxygen-free radicals leading to numerous carcinogenic DNA mutations or loss, genetic instability, overexpression of specific oncogenes, and downregulation of tumor suppressor genes [22–24]. It has recently been demonstrated that Fe3+, derived from menstrual reflux, recently defined as “incessant menstruation” [25], is able to induce an increase in fimbrial cell viability and proliferative capacity and to activate principal oncogenes (p53, pan-Ras, Ki67 and c-Myc). So, it has been confirmed that Fe3+ is capable to induce carcinogenic changes and represents the main non-genetic risk factor for ovarian cancer [26]. For this reason, Fe3+ can be considered a putative candidate as a transforming agent from normal human fimbrial cells into cancer cells maintaining physiological conditions of the menstrual cycle through oxidative stress and consequent oncogenes activations.
This research was planned to study the role of VitD to prevent oxidative injury induced by Fe3+ exposition in primary fimbrial cells culture, because recent studies have hypothesized that fimbrial fallopian tubes are the site where most serous ovarian cancers develop [27, 28], and the cells are subjected, to a constant carcinogenic stimulus represented by Fe3+ [26], especially in presence of low levels of serum VitD.
Methods
Samples
Thirty-six fresh fallopian tube-derived fimbriae were obtained under written consent from women during isteroannessiectomy for ovarian cancer and benign pathology without comorbidity at the II Department of Obstetrics and Gynaecology of the Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico (Milan, Italy). All subjects were in premenopause and had not received any type of hormonal or drug therapy for at least 3 months. Approval for this study was granted by the local Human Institutional Investigation Committee.
Tissue collection
Thirty-six fresh fallopian tube-derived fimbriae tissues were collected during isteroannessiectomy from 18 women and transported to laboratory in sterile falcon containing saline solution (0.9 % w/v solution of sodium chloride in distilled water, S.A.L.F, Cenate Sotto, Bergamo, Italy) supplemented with 10 % penicillin/streptomycin (Sigma, Milan, Italy). The tissue were obtained under written consent at the II Department of Obstetrics and Gynaecology of the Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico (Milan, Italy). Approval for this study was granted by the local Human Institutional Investigation Committee. All 18 women were in premenopause and had not received any type of hormonal or drug therapy for at least 3 months before isteroannessiectomy for ovarian cancer and benign pathology without comorbidity.
Primary cell preparation and culture
The isolation of epithelial secretory cells from fimbriae of fallopian tubes (FSEC) has been described in detail in a previous study [26]. Briefly, samples of fimbrial tissues were washed, minced and incubated with Dulbecco’s Modified Eagle Medium (DMEM, Sigma, Milan, Italy) supplemented with 0.1 % type A collagenase, 1 % penicillin/streptomycin and 2 mM L-Glutamine (Sigma, Milan, Italy) for 2-3 h in incubator at 37 °C in agitation and centrifuged at 600xg for 10 min at room temperature (RT). The cell population of each patient have been kept separate and used for the experiments. One experiment was performed on one population obtained from one patient. Before the experiments, the purity of cell culture was verified using a specific marker PAX8. The cells used had passage 1-5 to have a complete cell phenotype.
To study cell viability (MTT test) and ROS production 1x104 cells were plated on 24 well-plates; to perform immunohistochemistry and immunofluorescence studies 0.2x104 cells were placed in CultureSlide (BD, Bedford, MA, U.S.A.) with 4 chambers; to analyze the intracellular pathways through Western Blot analysis the cells were plated on 60 mm culture dish until confluence. Each experiment was performed on 4 to 6 cell population of FSEC to obtained 4 or 6 technical replicates using 50, 75, 100 mM of Fe3+.
Experimental protocol
Each experiment was performed on 4 to 6 FSEC using 50, 75, 100 mM of Fe3+ [26] and 1nM VitD (based on dose-response study) [2]. 1nM VitD was able to induce a maximum effect on cell viability of FSEC. This concentration was also verify in other work reported in literature [2]. This VitD concentration can ben considered physiologically and clinically attainable because in humans is comprised between 0.1 nM and 10 nM [29]. Experiments were performed using high doses of Fe3+ comparable to those observed in the content of endometriotic cysts [30]. In addition these concentrations were also observed in a previous work on fimbrial cells to be able to mimic carcinogenic changes [26]. FSEC were incubated for two hours in DMEM without red-phenol supplemented with 1 % penicillin/streptomycin, 2 mM L-Glutamine and 0.5 % FBS before and during the treatment. The stimulation with 1nM VitD was maintained alone for 6 days and replicated as pretreatment for 6 days before the stimulation with Fe3+ for other 6 days. The time of stimulation of Fe3+ was the same used in a previous work [26].
MTT test
MTT dye (Sigma-Aldrich) was used to determine cell viability. After stimulation the cells were incubated with 1 % MTT dye for 2 h at 37 °C in incubator, as previously described [2, 26].
Then, the medium was removed and the crystals were dissolved in DMSO. Cell viability was measured through a spectrometer (VICTORX3 Multilabel Plate Reader) at 570 nm with correction at 690 nm, and calculated by comparing results to control cells (100 % viable).
ROS production
The rate of superoxide anion release was used to examine the effects of VitD against the oxidative stress induced by Fe3+. The superoxide anion production was measured as superoxide dismutase-inhibitable reduction of cytochrome C, as previously described [2]. Briefly, in all samples (stimulated and untreated), 100 μL of cytochrome C was added and in another one, 100 μL of superoxide dismutase was also added for 30 min in an incubator (all substances from Sigma-Aldrich). The absorbance changes in the supernatants of the sample was measured at 550 nm in a Wallac Victor model 1421 spectrometer (PerkinElmer). The O2 was expressed as nanomoles per reduced cytochrome C per microgram of protein, using an extinction coefficient of 21000 mL/cm, after the interference absorbance subtraction [31].
Western Blot for VDR, PAX8, p53, c-Myc, Ki67 and pan-Ras
FSEC at confluence were washed three times with cold PBS 1x supplemented with 2 mM sodium orthovanadate, and then lysed in ice with Complete Tablet buffer (Roche) supplemented with 2 mM sodium orthovanadate and 50 μM MG132 (Sigma-Aldrich). Thirty-five μg of proteins from each lysate were loaded on 15 or 5 % SDS-PAGE gels and transferred to polyvinylidene fluoride membranes (PVDF, GE Healthcare Europe GmbH, Milan, Italy). They were incubated overnight at 4 °C with specific primary antibody: anti-PAX8 (1:500, Abnova, DBA ITALIA S.r.l., Milan, Italy), anti-VDR (1:200, Santa-Cruz), anti-p53 (1:500, Santa-Cruz), anti-cMyc (1:200, Millipore S.p.A., Milan, Italy), anti-Ki67 (1:500, Santa-Cruz), and anti-pan-Ras (1:500, Santa-Cruz). Protein expression was normalized and verified through ß-actin detection (1:5000; Sigma, Milan, Italy).
VDR, PAX8, c-Myc, Ki67 and pan-Ras immunocytochemistry in cellular preparation
FSEC cultured in chamber slide as described above were washed three times with cold PBS 1x supplemented with 2 mM sodium orthovanadate, and fixed using a cold fixative solution (3.7 % formaldehyde, 3 % sucrose in PBS 1X) for 20 min at RT. Then the cells were washed twice with cold PBS 1X, permeabilized with cold PBS 1X with cold 0.5 % Triton X-100 on ice at 4 °C for 20 min and then washed with PBS 1X. Then the chamber slides were incubated with 3 % hydrogen peroxide in PBS 1X for 8 min to block endogenous peroxidase activity and then maintained in a blocking solution composed of PBS 1X with 3 % albumin from bovine serum (BSA, Sigma, Milan, Italy) for 1 h at RT. The slides were subsequently incubated overnight at 4 °C with specific primary antibody: 1:150 PAX8, 1:50 VDR, 1:50 c-Myc, 1:50 Ki67 and 1:50 pan-Ras. All these antibodies were diluted in PBS 1X in a humidified chamber, and then incubated for 20 min with diluted biotinylated secondary antibody solution (Dako Italia, Milan, Italy) and then for 20 min with VECTASTAIN® ABC Reagent (Dako Italia, Milan, Italy). Finally the sections were washed, incubated with peroxidase substrate solution until desired stain intensity developed (Peroxidase/DAB, Dako Italia, Milan, Italy), rinsed in tap water, counterstained with Mayer’s hematoxylin and mounted with Bio Mount (Bio-Optika, Milan, Italy). The number of positive cells was calculated as described elsewhere [32]: briefly, 12 different areas (1 mm2) randomly selected from each section were taken, and the number of signals was determined using ImagePro 3 software (NIH, Bethesda, US). The results were expressed as a means ± SD (%).
p53 immunofluorescence in cellular preparation
After the stimulations the cells were fixed using cold buffer PAF for 20 min, washed three times with cold PBS 1X and then permeabilized with cold PBS 1X with 0.5 % Triton X-100 for 20 min at 4 °C. After this time slides were incubated in blocking solution (1 % BSA and 5 % FBS in PBS 1X) for 30 min at RT and treated with p53 specific antibody (1:50, Santa-Cruz) in PBS 1X overnight at 4 °C. The slides were then incubated with fitch-secondary antibodies (1:200, Sigma-Aldrich) in PBS 1X for 1 h in the dark, counterstained with DAPI (1 μg/ml; Sigma-Aldrich) diluted in PBS 1X for 5 min in the dark at RT and finally mounted in Vectashield (D.B.A. Italia). The number of positive cells was calculated as described by Lee et al. [32]: briefly, 12 different areas (1 mm2) randomly selected from each section were taken, and the number of signals was determined using ImagePro 3 software (NIH, Bethesda, US). The results were expressed as means ± SD (%).
Statistical analysis
Results are expressed as means ± SD of at least 4 independent experiments for each experimental protocol. One-way ANOVA followed by Bonferroni post hoc test was used for statistical analysis. The percentage values were compared through Mann-Whitney U test. P-value <0.05 was considered statistically significant.
Results
Dose-response study, cell viability and reactive oxygen species (ROS) production
The cell viability induced by stimulation of FSEC with VitD (from 0.01 to 10 nM, dissolved in ethanol), was measured in a dose-response study after 6 days by MTT test. As illustrated in Fig. 1a, the effect of VitD on cell viability by a dose-response study was examined and it was concentration-dependent with a maximum effect at 1 nM concentration after 6 days of stimulation (48.60 ± 2.93 %, P < 0.05). This concentration was used for all successive experiments. The effect of the solvent of VitD on FSEC was also tested. In addition the influence of VitD on the effects exerted by Fe3+ on cell viability of FSEC was studied. The cells were divided into two groups: one treated with different concentrations of Fe3+ for 6 days and one pre-treated with 1 nM VitD for 6 days and then stimulated with the same concentrations of Fe3+ (50-75-100 mM). Pre-treatment was also performed using ethanol alone (solvent of VitD). As reported in Fig. 1b, the pre-treatment with VitD was able to counteract the increase on cell viability induced by Fe3+ in a dose-dependent manner, and the maximum effects were observed in presence of 100 mM Fe3+ (1.033 ± 0.04 %, P < 0.05) in respect with Fe3+ alone.
Fig. 1.
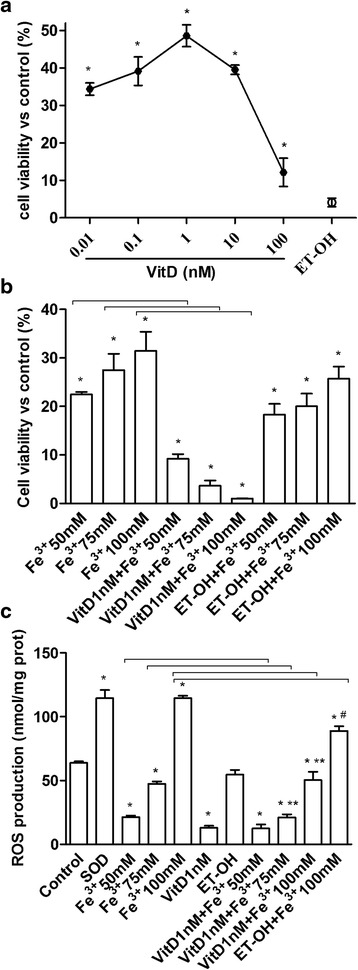
Effects of VitD on cell viability and ROS production. a, dose-response study of VitD (0.01-100 nM) on cell viability of FSEC. The results are expressed as means ± SD (%) normalized to control values of 5 technical replicates. * P < 0.05 vs control. b, MTT test performed in FSEC treated with different doses of Fe3+ (50-100 mM) alone for 6 days or pretreated with 1nM VitD for 6 days. The results are expressed as means ± SD (%) normalized to control values of 6 technical replicates. ET-OH = ethanol * P < 0.05 vs control; arrows indicate P < 0.05 between Fe3+ alone and VitD + Fe3+ c, ROS production (expressed as Cytochrome C reduced per μg of protein) in FSEC treated with different doses of Fe3+ (50-100 mM) alone for 6 days or pretreated with 1nM VitD for 6 days. The results are expressed as means ± SD of 5 technical replicates. ET-OH = ethanol. * P < 0.05 vs control; ** P < 0.05 vs VitD; # P < 0.05 vs ET-OH; arrows indicate P < 0.05 between Fe3+ alone and VitD + Fe3+
The same conditions described before were reproduced to analyze the ROS production in FSEC. In cells treated with Fe3+ we observed a significant increase in ROS production in a dose-dependent manner compared with control (Fig. 1c, P < 0.05), and the maximum effects was obtained by 100 mM Fe3+ (114.6 ± 1.84 Cytochrome C reduced per μg of protein). In FSEC treated with VitD alone a significant reduction in ROS production compared to control was observed (13.08 ± 1.53 Cytochrome C reduced per μg of protein). The pre-treatment with VitD was able to counteract the ROS production induced by Fe3+ and this effect was more evident in presence of 75 mM (21.09 ± 2.46 Cytochrome C reduced per μg of protein) and 100 mM Fe3+ (50.27 ± 6.59 Cytochrome C reduced per μg of protein) compared with Fe3+ alone (47.40 ± 1.86 and 114.6 ± 1.84 Cytochrome C reduced per μg of protein, respectively). These data confirmed previous findings on MTT test, and demonstrate the ability of VitD to prevent the effects of oxidative stress only if it used before the oxidative damage.
PAX8 and VDR receptor analysis
FSEC were tested for specific fimbrial marker PAX8 in immunocytochemistry and Western blot analysis (Figs. 2a and 3a) to verify the efficacy of cell isolation and the preservation during the stimulation with Fe3+ and VitD (as showed nuclear/perinuclear staining by immunocytochemistry). The presence of VDR receptor in FSEC were determined to demonstrate the efficacy of VitD in these cells. The presence of VDR receptor was evident in immunocytochemistry (Fig. 2b), in which 98 ± 2 % of FSEC had cytoplasmic-nuclear staining positive and this increase compared to control was also observed by Western blot analysis (Fig. 3b). Indeed the expression was augmented compared to control (about 50 %, P < 0.05) in presence of VitD alone or in samples pre-treated with VitD. These data demonstrate that VitD is able to explain its effects through VDR receptor signaling through genomic action.
Fig. 2.
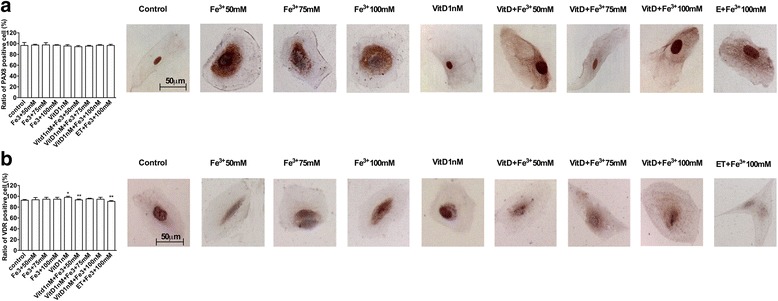
PAX-8 and VDR receptor analysis by immunocytochemistry. On the left the score of positive cells, counted in 12 different areas, and on the right the representative pictures, obtained through microscopy at original magnification of X40, are reported. A, PAX-8 staining: the ratio is reported as mean (SD) (%) of positive cells of 4 technical replicates. The scale reported in the first column on the right is to be considered valid for the same antibody. B, score of positive cells for VDR receptor is reported as mean (SD) (%) of 4 technical replicates. * P < 0.05 vs control; ** P < 0.05 vs VitD. The scale reported in the first column is to be considered valid for the same antibody
Fig. 3.
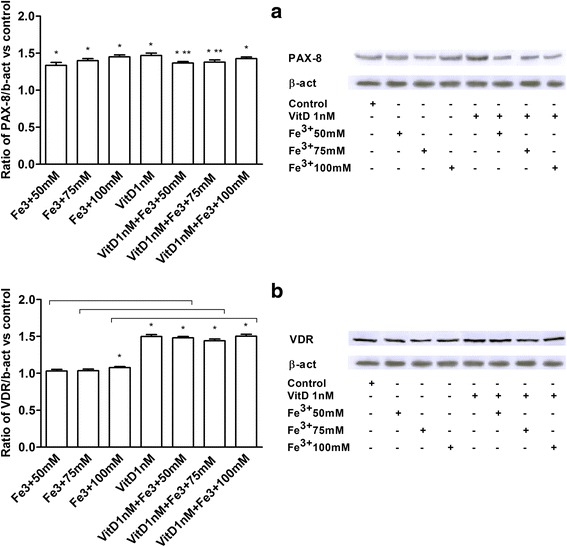
PAX-8 (a) and VDR (b) studies by Western Blot and densitometric analysis. Protein extracts has been analyzed by immunoblotting with specific antibodies against the indicated proteins. Data are expressed as means of 4 technical replicates performed on FSEC. * P < 0.05 vs control; ** P < 0.05 vs VitD; arrows indicate P < 0.05 between Fe3+ alone and VitD + Fe3+
p53, pan-Ras, Ki67, and c-Myc Analysis in FSEC
p53, pan-Ras, Ki67, and c-Myc expressions were investigated in FSEC treated with Fe3+ alone and after pre-treatment with VitD by Western blotting (Fig. 4) and immunofluorescence or immunocytochemistry (Fig. 5). The effects of VitD alone on these pathways were also tested in the same protocols (Figs. 4 and 5). In presence of Fe3+ p53, pan-Ras, Ki67, and c-Myc activations were observed in a dose-dependent manner, and the maximum effects were observed with Fe3+ 100 mM after 6 days of treatment (2.88 ± 1.06; 1.74 ± 1.03; 10.13 ± 1.23;1.28 ± 1.01 ratio of activation, respectively) compared to control values by Western blotting (Fig. 4). Similar data were also observed in immunofluorescence (p53) and immunocytochemistry experiments (pan-Ras, Ki67, c-Myc) performed in FSECs (Fig. 5). The pre-treatment with VitD for 6 days was able to counteract p53, pan-Ras, Ki67, and c-Myc activations (Figs. 4 and 5): these effects were clearer in samples treated with Fe3+ 100 mM (64 %; 42 %; 87 %; 22 % of reduction, respectively by Western Blot analysis). In addition the effects of VitD alone were also tested and didn’t reveal a significant activation of tumoral markers (P < 0.05) compared to control values.
Fig. 4.
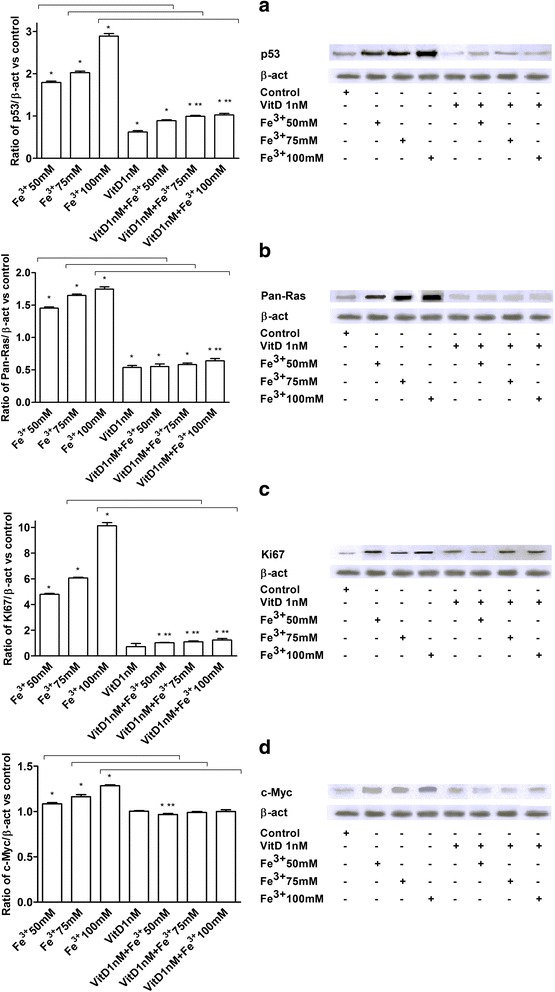
Western Blot and densitometric analysis of p53 (a), Pan-Ras (b), Ki67 (c) and c-Myc (d). Protein extracts were analyzed by immunoblotting with specific antibodies against the indicated proteins. Data are expressed as means of 5 technical replicates performed on FSEC. * P < 0.05 vs control; ** P < 0.05 vs VitD; arrows indicate P < 0.05 between Fe3+ alone and VitD + Fe3+
Fig. 5.
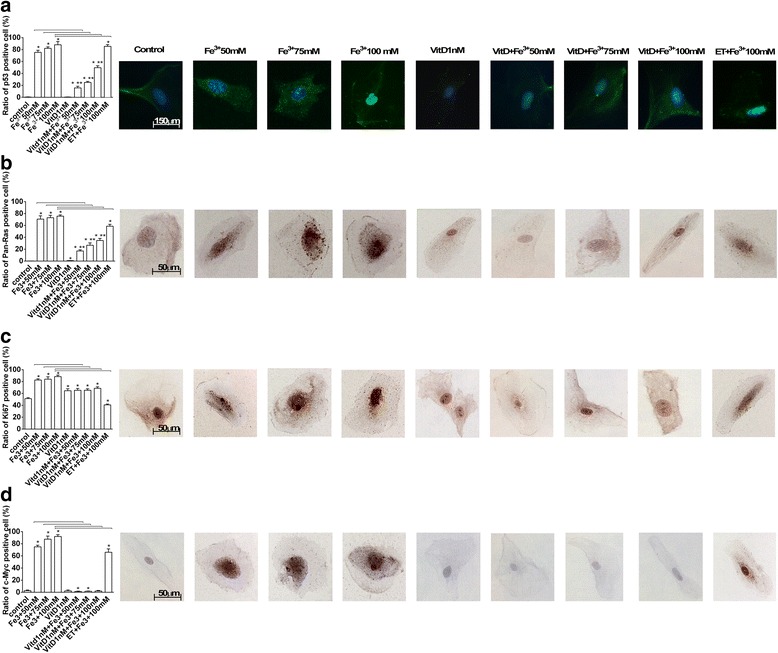
p53 (a), Pan-Ras (b), Ki67 (c) and c-Myc (d) analysis by immunofluorescence (panel A) or immunocytochemistry (panel B-D). On the left the score of positive cells, counted in 12 different areas, and on the right the representative pictures, obtained through microscopy at original magnification of X40, are reported. The ratio is reported as mean (SD) (%) of positive cells of 5 technical replicates. The scale reported in the first column on the right is to be considered valid for the same antibody. * P < 0.05 vs control; ** P < 0.05 vs VitD; arrows indicate P < 0.05 between Fe3+ alone and VitD + Fe3+
Discussion
It has been demonstrated that the site of origin of most high grade serous ovarian cancers is the fallopian tube secretory epithelial cells [33]. Recent studies hypothesized the role of retrograde menstruation-derived Fe3+ in increasing risk of ovarian cancer [25], due to a severe oxidative injury induced by iron [26, 34, 35]. Fimbria in the pouch of Douglas is exposed to generated from hemolysis of erythrocytes by pelvic macrophage during retrograde menstruation, a common physiologic event in all menstruating women [25]. In addition, Seidman [35] showed the presence of mucosal iron in fallopian tubes in advanced-grade pelvic serous carcinoma [36]. In a previous work, Lattuada et al. [26] demonstrates in FSEC the involvement of Fe3+ in carcinogenic changes using Fe3+ at highly doses [22, 30]. This study demonstrates for the first time that VitD plays an important role in preventing Fe3+-dependent oxidative stress in cultured fimbrial cells. Experiments were performed using 1 nM VitD. Experiments using Fe3+ have been preceded by a dose-response study showing that the best effect on cell viability was obtained with 1 nM VitD and the optimum range is between 0.1 and 10 nM. This is the concentration range considered physiologically and clinically attainable in humans [29]. The great decrease observed in cell viability after 100 nM VitD administration depends primarily on saturation of the intracellular pathways controlling viability. This effect is still higher than the control. The beneficial effect of VitD consists in a significant decrease of oxidative state showed by a significant decrease in ROS production in culture supernatants. However the ability of VitD to block oxidative injury has been tested only when this substance has been administered before Fe3+.
These findings support previous studies in which the relationship between low VitD serum concentration and overall survival rate of patients with ovarian cancer has been demonstrated [10]. Moreover, the important role of severe VitD deficiency in more aggressive course of ovarian cancer has been described [6, 35–37]. The effects of VitD have been observed in FSEC with a high grade of culture purity (PAX-8 positivity) along with the activation of VDR. For this reason mechanisms underlying protective effects of VitD may be hypothesized to have genomic origin.
p53, pan-Ras, Ki67 and c-Myc has been analyzed in FSEC treated with VitD alone or before Fe3+, to clarify the protective mechanism activated by VitD. A novel finding is represented by the demonstration that pre-treatment with VitD is able to significantly counteract tumoral biomarkers activation, suggesting the inhibition of epithelial cell transformation. Thus our findings indicate that VitD prevented the activation of p53, pan-Ras, Ki67, and c-Myc. On the contrary, Fe3+ alone was able to mimic in FSEC, through these tumoral biomarkers, the carcinogenic changes typical of serous ovarian cancer.
As concerns Fe3+ concentration adopted in this study, it must be considered that cellular iron homeostasis is regulated by cytosolic regulatory proteins that bound structural elements (iron-response elements) present in the messenger RNA of some major proteins such as transferrin receptor and ferritin. For this reason it is difficult to quantify the plasmatic concentration of free Fe3+. However, in this study, it has been chosen to use a Fe3+ concentration similar to that found in endometriotic cysts [30].
The importance of these data is remarkable since the Fe3+ concentration used in these experiments may induce carcinogenic changes as reported by many studies [26, 38, 39].
Conclusions
The results described herein highlight that VitD exerts protective effects against Fe3+-related oxidative stress in cultured FSEC. The discussed results could be relevant in the light of the use of serum VitD levels assessment to promote VitD supplementation or to adjust therapeutic strategies in ovarian cancer patients.
Acknowledgments
The authors thank Ms Mariangela Fortunato for her precious help with the preparation of the article.
Funding
Not applicable.
Authors’ contributions
DL and FU designed the study, wrote the manuscript and are co-first authors; FU, VM, BC and AC performed the experiments; AB and PC provided the tissue samples; FU and CM analyzed the data; CM reviewed the paper. GB designed the study and supervised the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Tissue samples were obtained after consensum format (see Methods section).
Contributor Information
Francesca Uberti, Phone: +390321660653, Email: francesca.uberti@med.uniupo.it.
Vera Morsanuto, Email: vera.morsanuto@med.uniupo.it.
Debora Lattuada, Email: UniUpo234@gmail.com.
Barbara Colciaghi, Email: UpoUni234@gmail.com.
Andrea Cochis, Email: UniUpo178@gmail.com.
Alessandro Bulfoni, Email: UpoUni794@gmail.com.
Paola Colombo, Email: upouni555@gmail.com.
Giorgio Bolis, Email: uniupo999@outlook.it.
Claudio Molinari, Email: claudio.molinari@med.uniupo.it.
References
- 1.Pittarella P, Squarzanti DF, Molinari C, et al. NO-dependent proliferation and migration induced by Vitamin D in HUVEC. J Steroid Biochem Mol Biol. 2015;149:35–42. doi: 10.1016/j.jsbmb.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 2.Uberti F, Lattuada FD, Morsanuto V, et al. Vitamin D protects human endothelial cells from oxidative stress through the autophagic and survival pathways. J Clin Endocrinol Metab. 2014;99:1367–1374. doi: 10.1210/jc.2013-2103. [DOI] [PubMed] [Google Scholar]
- 3.Molinari C, Uberti F, Grossini E, et al. 1α,25-dihydroxycholecalciferol induces nitric oxide production in cultured endothelial cells. Cell Physiol Biochem. 2011;27:661–668. doi: 10.1159/000330075. [DOI] [PubMed] [Google Scholar]
- 4.Mohr SB. A Brief History of Vitamin D and Cancer Prevention. Ann Epidemiol. 2009;19:79–83. doi: 10.1016/j.annepidem.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Attar R, Gasparri ML, Donato VD, et al. Ovarian cancer: interplay of vitamin D signaling and miRNA action. Asian Pac J Cancer Prev. 2014;15:3359–3362. doi: 10.7314/APJCP.2014.15.8.3359. [DOI] [PubMed] [Google Scholar]
- 6.Bouillon R, Eelen G, Verlinden L, et al. Vitamin D and cancer. J Steroid Biochem Mol Biol. 2006;102:156–162. doi: 10.1016/j.jsbmb.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 7.Mohapatra S, Saxena A, Gandhi G, et al. Does vitamin D mediate inhibition of epithelial ovarian cancer by modulating cytokines? Clin Transl Oncol. 2015;17(8):590–595. doi: 10.1007/s12094-015-1281-3. [DOI] [PubMed] [Google Scholar]
- 8.Garland C, Comstock G, Garland F, et al. Serum 25-hydroxyvitamin D and colon cancer: eight-year prospective study. Lancet. 1989;32:1176–1178. doi: 10.1016/S0140-6736(89)91789-3. [DOI] [PubMed] [Google Scholar]
- 9.Gorham ED, Garland CF, Garland FC, et al. Optimal vitamin D status for colorectal cancer prevention: a quantitative meta analysis. Am J Prev Med. 2007;32:210–216. doi: 10.1016/j.amepre.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Walentowicz-Sadlecka M, Grabiec M, Sadlecki P, et al. 25(OH)D3 in patients with ovarian cancer and its correlation with survival. Clin Biochem. 2012;45:1568–1572. doi: 10.1016/j.clinbiochem.2012.07.110. [DOI] [PubMed] [Google Scholar]
- 11.Lungchukiet P, Sun Y, Kasiappan R, et al. Suppression of epithelial ovarian cancer invasion into the omentum by 1α,25-dihydroxyvitamin D3 and its receptor. J Steroid Biochem Mol Biol. 2015;148:138–147. doi: 10.1016/j.jsbmb.2014.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cook LS, Neilson HK, Lorenzetti DL, et al. A systematic literature review of vitamin D and ovarian cancer. Am. J Obstet Gynecol. 2010;203:70.e1-8. doi: 10.1016/j.ajog.2010.01.062. [DOI] [PubMed]
- 13.Fleet JC. Molecular actions of vitamin D contributing to cancer prevention. Mol Aspects Med. 2008;29:388–396. doi: 10.1016/j.mam.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lombardi C, Heck JE, Cockburn M, et al. Solar UV radiation and cancer in young children. Cancer Epidemiol Biomarkers Prev. 2013;22:1118–1128. doi: 10.1158/1055-9965.EPI-12-1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis CD, Milner JA. Nutrigenomics, vitamin D and cancer prevention. J Nutrigenet Nutrigenomics. 2011;4:1–11. doi: 10.1159/000324175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deeb KK, Trump DL, Johnson CS. Vitamin D signalling pathways in cancer: potential for anticancer therapeutics. Nat Rev Cancer. 2007;7:684–700. doi: 10.1038/nrc2196. [DOI] [PubMed] [Google Scholar]
- 17.Abedin SA, Banwell CM, Colston KW, et al. Epigenetic corruption of VDR signalling in malignancy. Anticancer Res. 2006;26:2557–2566. [PubMed] [Google Scholar]
- 18.Becker BN, Himmelfarb J, Henrich WL, et al. Reassessing the cardiac risk profile in chronic hemodialysis patients: A hypothesis on the role of oxidant stress and other non-traditional cardiac risk factors. J Am Soc Nephrol. 1997;8:475–486. doi: 10.1681/ASN.V83475. [DOI] [PubMed] [Google Scholar]
- 19.Ambrosio G, Zweier JL, Jacobus WE, et al. Improvement of postischemic myocardial function and metabolism induced by administration of deferoxamine at the time of reflow: The role of iron in the pathogenesis of reperfusion injury. Circulation. 1987;76:906–915. doi: 10.1161/01.CIR.76.4.906. [DOI] [PubMed] [Google Scholar]
- 20.Van der Kraaij AM, Mostert LJ, Van Eijk HG, et al. Iron-load increases the susceptibility of rat hearts to oxygen reperfusion damage. Protection by the antioxidant (+)-cyanidanol-3 and deferoxamine. Circulation. 1988;78:442–449. doi: 10.1161/01.CIR.78.2.442. [DOI] [PubMed] [Google Scholar]
- 21.Halliwell B, Gutteridge JM. Role of free radicals and catalytic metal ions in human disease: An overview. Methods Enzymol. 1990;186:1–85. doi: 10.1016/0076-6879(90)86093-B. [DOI] [PubMed] [Google Scholar]
- 22.Núñez MT, Tapia V, Toyokuni S, et al. Iron-induced oxidative damage in colon carcinoma (Caco-2) cells. Free Radic Res. 2001;34:57–68. doi: 10.1080/10715760100300061. [DOI] [PubMed] [Google Scholar]
- 23.Kabat GC, Rohan TE. Does excess iron play a role in breast carcinogenesis? An unresolved hypothesis. Cancer Causes Control. 2008;18:1047Y1053. doi: 10.1007/s10552-007-9058-9. [DOI] [PubMed] [Google Scholar]
- 24.Gutteridge JMC, Rowley DA, Halliwell B. Superoxide-dependent formation of hydroxyl radicals and lipid peroxidation in the presence of iron salts: detection of “catalytic” iron” and antioxidant activity in extracellular fluids. Biochem J. 1982;206:605Y609. doi: 10.1042/bj2060605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vercellini P, Crosignani P, Somigliana E, et al. The 'incessant menstruation' hypothesis: a mechanistic ovarian cancer model with implications for prevention. Hum Reprod. 2011;26:2262–2273. doi: 10.1093/humrep/der211. [DOI] [PubMed] [Google Scholar]
- 26.Lattuada D, Uberti F, Colciaghi B, et al. Fimbrial cells exposure to catalytic iron mimics carcinogenic changes. Int J Gynecol Cancer. 2015;25:389–398. doi: 10.1097/IGC.0000000000000379. [DOI] [PubMed] [Google Scholar]
- 27.Levanon K, Ng V, Piao H, et al. Primary ex vivo cultures of human fallopian tube epithelium as a model for serous ovarian carcinogenesis. Oncogene. 2010;29:1103–1113. doi: 10.1038/onc.2009.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kuhn E, Ayhan A, Shih IM, et al. Ovarian Brennan tumour: a morphologic and immunohistochemical analysis suggesting an origin from fallopian tube epithelium. Eur J Cancer. 2013;49:3839–3849. doi: 10.1016/j.ejca.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 29.Bläuer M, Sand J, Laukkarinen J. Physiological and clinically attainable concentrations of 1,25-dihydroxyvitamin D3 suppress proliferation and extracellular matrix protein expression in mouse pancreatic stellate cells. Pancreatology. 2015;15(4):366–71. doi: 10.1016/j.pan.2015.05.044. [DOI] [PubMed] [Google Scholar]
- 30.Yamaguchi K, Mandai M, Toyokuni S, et al. Contents of endometriotic cysts, especially the high concentration of free iron, are a possible cause of carcinogenesis in the cysts through the iron-induced persistent oxidative stress. Clin Cancer Res. 2008;14:32–40. doi: 10.1158/1078-0432.CCR-07-1614. [DOI] [PubMed] [Google Scholar]
- 31.Sun HY, Wang NP, Kerendi F, et al. Hypoxic postconditioning reduces cardiomyocyte loss by inhibiting ROS generation and intracellular Ca2+ overload. Am J Physiol Heart Circ Physiol. 2005;288:H1900–H1908. doi: 10.1152/ajpheart.01244.2003. [DOI] [PubMed] [Google Scholar]
- 32.Lee SH, Chung JY, Jung YS, et al. p53, secreted by K-Ras-Snail pathway, is endocytosed by K-ras-mutated cells; implication of target-specific drug delivery and early diagnostic marker. Oncogene. 2009;28:2005–2014. doi: 10.1038/onc.2009.67. [DOI] [PubMed] [Google Scholar]
- 33.Vang R, Shih MI, Kurman JR. Fallopian tube of ovarian low- and high-grade serous neoplasms. Histopathology. 2013;62:44–58. doi: 10.1111/his.12046. [DOI] [PubMed] [Google Scholar]
- 34.Dubeau L. The cell of origin of ovarian epithelial tumors and the ovarian surface epithelium dogma: does the emperor have no clothes? Gynecol Oncol. 1999;72:437–442. doi: 10.1006/gyno.1998.5275. [DOI] [PubMed] [Google Scholar]
- 35.Seidman JD. The presence of mucosal iron in the fallopian tube supports the “incessant menstruation hypothesis” for ovarian cancer. Int J Gynecol Pathol. 2013;32:454–458. doi: 10.1097/PGP.0b013e31826f5ce2. [DOI] [PubMed] [Google Scholar]
- 36.Cibula D, Gampel A, Mueck AO, et al. Hormonalcontraception and risk of cancer. Hum Reprod Update. 2010;16:631Y650. doi: 10.1093/humupd/dmq022. [DOI] [PubMed] [Google Scholar]
- 37.Lefkowitz ES, Garland CF. Sunlight, vitamin D, and ovarian cancer mortality rates in US women. Int J Epidemiol. 1994;23:1133–1136. doi: 10.1093/ije/23.6.1133. [DOI] [PubMed] [Google Scholar]
- 38.Yin L, Grandi N, Raum E, et al. Meta-analysis: Circulating vitamin D and ovarian cancer risk. Gynecol Oncol. 2011;121:369–375. doi: 10.1016/j.ygyno.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 39.Dhillon AS, Hagan S, Rath O, et al. MAP kinase signalling pathways in cancer. Oncogene. 2007;26:3279–3290. doi: 10.1038/sj.onc.1210421. [DOI] [PubMed] [Google Scholar]


